Abstract
Acute and chronic lateral ankle instability are common in high-demand patient populations. If not managed appropriately, patients may experience recurrent instability, chronic pain, osteochondral lesions of the talus, premature osteoarthritis, and other significant long-term disability. Certain populations, including young athletes, military personnel and those involved in frequent running, jumping, and cutting motions, are at increased risk. Proposed risk factors include prior ankle sprain, elevated body weight or body mass index, female gender, neuromuscular deficits, postural imbalance, foot/ankle malalignment, and exposure to at-risk athletic activity. Prompt, accurate diagnosis is crucial, and evidence-based, functional rehabilitation regimens have a proven track record in returning active patients to work and sport. When patients fail to improve with physical therapy and external bracing, multiple surgical techniques have been described with reliable results, including both anatomic and non-anatomic reconstructive methods. Anatomic repair of the lateral ligamentous complex remains the gold standard for recurrent ankle instability, and it effectively restores native ankle anatomy and joint kinematics while preserving physiologic ankle and subtalar motion. Further preventative measures may minimize the risk of ankle instability in athletic cohorts, including prophylactic bracing and combined neuromuscular and proprioceptive training programs. These interventions have demonstrated benefit in patients at heightened risk for lateral ankle sprain and allow active cohorts to return to full activity without adversely affecting athletic performance.
Keywords: Ankle instability, Athlete, Treatment, Epidemiology, Prevention, Lateral, Sprain
Core tip: Competitive athletes and high-demand military servicemembers are at significant risk for lateral ankle instability during at-risk activity, particularly in the presence of certain modifiable and non-modifiable risk factors. In conjunction with semirigid ankle bracing, functional rehabilitation protocols emphasizing neuromuscular coordination, peroneal strengthening, and proprioceptive training are effective for the majority of patients with acute ankle sprain. However, with chronic lateral ankle instability unresponsive to conservative measures, anatomic ligamentous repair or reconstruction reliably restores active patients to full athletic function. Prophylactic bracing and targeted physical therapy may also be considered in selected, high-risk cohorts.
INTRODUCTION
Acute and chronic ankle instability are common within athletic patient populations. Ankle sprain is a term often applied to a broad spectrum of traumatic soft tissue injuries about the ankle and hindfoot. However, the injury discussed in this review specifically addresses ligamentous instability about the talocrural joint[1]. Ankle instability has classically been organized into three categories: lateral, medial, and syndesmotic ligament injuries. These injuries are often seen in conjunction with other concomitant trauma, particularly involving the talar dome articular surface and peroneal tendons. Lateral ankle sprains, specifically those involving the anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL), and posterior talofibular ligament, account for over 85% of all ankle sprains[2]. Conversely, syndesmotic sprains (i.e., “high ankle sprains”) and medial ankle ligamentous injuries encompass up to 15% of all ankle sprains, although these injuries are far less thoroughly evaluated in the literature[3,4].
Acute ankle sprain has been reported to be the most common injury sustained by athletes, accounting for up to 40% of sports injuries[5-8]. Annually, an estimated two million acute ankle sprains occur each year in the United States, resulting in nearly 1.2 million healthcare-related visits and an annual aggregate health-care cost of up to $2 billion[9-11]. Ankle instability, when undertreated, may also result in chronic pain, muscular weakness, recurrent instability, and degenerative arthritis[2,12]. Significant time lost at work or further disability has been reported to occur in up to 60% of patients[9,13,14].
The purpose of this review is to summarize the relevant contemporary literature regarding acute and chronic lateral ankle instability and identify epidemiological risk factors for subsequent injury within an active patient population. Additionally, we will discuss the management and prevention of these common athletic injuries within the context of this higher-demand cohort.
EPIDEMIOLOGY
The incidence rates of ankle sprain may vary depending on patient demographics and method of surveillance, and several authors have reported between 2 to 7 individuals affected per 1000 in the general population each year[9,12,15]. Acute ankle sprain has also been identified as the most common injury sustained by United States military personnel[4,8], as well as young athletes[4,12,15,16]. In 2007, Fong et al[6] performed a systematic review of sports injuries sustained from 1977 to 2005, and ankle sprain was the major ankle injury in 33 of 43 sports.
With frequent, heavy load-bearing activity, rigorous physical demands, and unpredictable terrain, the incidence rates of ankle sprain among military servicemembers are an order of magnitude greater than that reported in the civilian population. Prior studies have underscored this epidemiological trend, with reported rates of ankle sprain ranging from 35 to 58 per 1000 person-years within the active duty United States military population[4]. Paratroopers may represent an even higher risk demographic. In this patient subset, ankle sprain accounts for 9%-33% of all parachute-related injuries and the incidence rate is estimated between 1 and 4.5 per 1000 jumps[17-19].
RISK FACTORS
Multiple studies have identified specific risk factors for ankle sprain in athletic cohorts, which are classically categorized as intrinsic or extrinsic factors[4,11,20,21]. Intrinsic risk factors may include age, gender, height, weight, body mass index (BMI), previous injury, aerobic fitness, limb dominance, flexibility, limb girth, muscle strength, proprioception, reaction time, postural stability, anatomical alignment, foot morphology, and inadequate rehabilitation. Extrinsic risk factors may include specific sport or at-risk activity, level of competition, shoe type, playing surface, and the use of external restraints such as ankle tape and/or braces[9,22]. Recently, injury epidemiologists have demonstrated a renewed focus on identifying modifiable and non-modifiable risk factors that tend to be associated with this common injury[4,20-23] (Table 1). Understanding variables within this framework may be useful in identifying high-risk populations. Furthermore, the targeting of modifiable risk factors may yield opportunities for further injury prevention[22].
Table 1.
Risk factors for ankle sprain among athletic populations
| Non-modifiable risk factors | Modifiable risk factors |
| Sex | Weight |
| Age | Body mass index |
| Height | Bracing/taping |
| Race | Footwear |
| Foot/ankle anatomy | Neuromuscular control |
| Extremity alignment | Postural stability |
| Previous ankle sprain | Muscle strength |
| Generalized Joint Laxity | Exposure to sport |
| Player position | |
| Playing surface | |
| Skill level |
Prior ankle instability
A history of previous ankle sprain appears to be an independent risk factor for recurrent acute ankle sprain. The index ankle sprain results in damage to the lateral ligaments responsible for stability of the tibiotalar joint and contributes to subsequent functional limitations. The initial inflammatory response from an acute ankle sprain also leads to scar formation, which is more prone to failure than uninjured native tissue, with a 60% reduction in energy absorbing capacity[24]. Tyler et al[25] reported that among high school football players, overweight athletes with a history of previous ankle sprain were 19 times more likely to sustain a noncontact ankle sprain than was a normal-weight player without a history of previous ankle sprain. Even with less severe primary ankle sprains, re-injury may still occur in athletes and military recruits involved in basic training type activities[8,26-28]. This increased risk may also be attributable to insufficient rehabilitation and earlier perceived healing of less severe injuries, despite persistent proprioceptive deficits[28].
Neuromuscular control
Neuromuscular control and postural stability are likely important factors affecting an athlete’s risk for ankle instability. The relationship between neuromuscular control and ankle sprain was first described by Freeman et al[29] in 1965. Subsequent investigations of athletes sustaining acute ankle sprains have extensively evaluated the proprioceptive deficit following the primary injury, and its resultant impairment of postural balance, ankle stability, and strength[30,31]. McGuine et al[32] reported that high school basketball players who sustained acute ankle instability events, demonstrated considerably greater postural sway on stabilometry, than their peers who did not sustain acute ankle sprains.
Other studies utilizing clinical assessments of postural stability have reported similar results, which underscores the likelihood of a neuromuscular predisposition for injury in certain athletes[33]. Muscle fatigue and loss of pre-injury strength may exacerbate neuromuscular impairment, resulting in the subsequent development of ankle instability[34]. Changes in ligament morphology and disruption of afferent nervous networks have been described in the setting of acute ankle sprain and may significantly affect postural stability; however, their contribution to the development of chronic instability is less well understood and requires further study[35-37].
Sex
While female gender has been previously associated with higher incidence rates of ankle sprain, studies evaluating gender disparity in acute ankle instability incidence have yielded mixed results. A study of military cadets at the United States Military Academy revealed an incidence rate for ankle sprain among female cadets of 96.4 per 1000 person-years in contrast to an incidence rate of 52.7 per 1000 person-years among male cadets (Incidence Rate Ratio 1.83)[4]. When examining the subset of intercollegiate athletes, no difference was detected by gender after controlling for athletic exposure and individual sport[4]. Beynnon et al[38] reported an incidence rate of ankle sprain of 1.6 per 1000 person-days for male college athletes, compared to 2.2 per 1000 person-days for female college athletes, although the reported disparity did not achieve statistical significance. Hosea et al[39] also reported a 25% greater risk for sustaining less severe (Grade I) ankle sprains for female high school and college basketball players, than their male counterparts. They did not; however, find a statistically different incidence of more severe ankle sprains among the same population. A recent military study revealed that among active duty servicemembers, females sustained ankle sprains with an incidence rate 21% higher than male military personnel[4].
With increasing female participation in athletic activities, studies comparing the incidence of musculoskeletal injury between the sexes have become important in identifying potential disparities between male and female athletes. The cause of differences in injury frequency is likely multifactorial, with hypothesized explanations including differences in hormones, ligamentous laxity, neuromuscular control, lower extremity limb alignment and anatomy, and both the level type of athletic participation[9,22,40]. Based on the available literature, there may be a higher incidence rate of lateral ankle sprain in females. However, fundamental differences in exposure to, as well as the level of, at-risk activity may confound this apparent difference, highlighting the need for further rigorous study.
Anthropomorphic measures
With increasing weight and body mass index, an increasing mass moment of inertia acting at the talocrural joint potentially increases the risk for acute ankle sprain. Tyler et al[25] reported that among high school football players with a BMI greater than 25 sustained ankle sprains significantly more frequently than those with a normal BMI. Waterman et al[3] described a similar association among male United States Military Academy cadets, with an increased incidence of ankle instability in cadets with a higher mean weight and BMI than sex-matched, uninjured cohorts. Conversely, other investigations have not found weight and BMI to be independent risk factors for ankle sprain[38,41]. Despite the varying results found in the literature, certain athletes and player positions may be at higher risk for ankle sprain.
At-risk activity or sport
Specific activity type resulting in ankle sprain also appears to vary by age, with young active patients involved in both competitive and recreational athletics occurring most often[4]. Activities that involve frequent running, jumping and cutting type movements place athletes at higher risk for ankle instability. Analysis of the National Electronic Injury Surveillance System for all ankle sprains presenting to emergency departments over a five-year period revealed that 49.3% of ankle sprains were caused by participation in sports, with basketball (41.1%), football (9.3%), and soccer (7.9%) accounting for over half of all ankle sprains sustained during athletic activity[9].
A more extensive investigation of the epidemiology of ankle sprains revealed that incidence rates vary depending on the unit of measurement utilized[6]. When evaluating for incidence per 1000 person-hours, rugby had the highest incidence (4.20), followed by soccer (2.52). Conversely, when reporting incidence more accurately in terms of athletic exposure, lacrosse had the highest incidence rate (2.56) of sprains per 1000 person-exposures, followed by basketball (1.90). Waterman et al[4] found a similar relationship with men’s rugby (1.53), men’s lacrosse (1.34) and basketball (women’s, 1.14 and men’s, 1.67),resulting in the highest incidences of ankle sprain per 1000 person-years among intercollegiate athletes.
Level of competition
Level of competition is another modifiable risk factor for ankle sprain that has been reported in the literature. Level of competition is a term commonly used to define both the intensity of competition as well as the skill level of participants (i.e., recreational, intramural, intercollegiate, or professional). However, these two components both represent distinct risk factors that should be separately evaluated[9]. There is a higher risk of ankle sprain with increasing level of intensity of competition, with approximately 55%-66% of injuries sustained during games, as opposed training or practice type activities[42-45]. Increases in pace of play and propensity for risk-taking activity likely account for this difference[9]. However, the impact of athlete skill level on the incidence of ankle sprain is less clear. Previous investigations suggest that college athletes are at seven times the risk for ankle sprain than their intramural counterparts, when analyzing the incidence of injury per 1000 person-years[4]. When controlling for the amount of athlete-exposures; however, no statistically significant difference was found between these cohorts. Additionally, Beynnon et al[46] reported that the risk of first-time ankle injury is similar for high school and college-level athletes. Other authors have similarly reported increased risk among intercollegiate athletes[39], while others have demonstrated a decreased risk among higher-skill level soccer players than their lower-skill level counterparts[43,47]. Other variables likely contribute to such differences seen between the different skill level cohorts, such as more match exposure and higher collective numbers of athlete-exposures[42], higher match-to-training ratio[48], and a lower warm-up or stretching period[48-50].
ACUTE ANKLE SPRAIN TREATMENT
Early recognition and evidence-based management of these common injuries are of great importance, and the consequences of missed or undertreated ankle instability is well documented with chronic instability resulting in as many as 60% of patients[2,9,13,14,16,51]. An initial assessment should always include a thorough history and physical examination, with consideration for radiographic evaluation. The Ottawa Ankle Rules are one commonly utilized method for the identification or exclusion of ankle fracture or other osseous trauma, and weight-bearing images are recommended if possible. Additionally, stress radiographs, including the talar tilt and anterior drawer tests, are often useful in evaluating for ligamentous laxity in patients with chronic ankle instability, but are not recommended in the acute setting[52-55].
The most common treatment methods described for severe, grade III acute ankle sprains are a brief period of rigid immobilization (e.g., < 10 d), functional management with transition to a semi-rigid external restraint, and delayed surgical repair in select, high-demand patients. Rigid immobilization in a cast is typically reserved for lower demand patients and should be employed for a period of no more than 3 wk, followed by sustained course of physical therapy for muscle strengthening and proprioceptive retraining[54,56-59]. Functional management of the acute ankle sprain entails early mobilization, weight bearing with an external restraint such as a brace, non-steroidal anti-inflammatory medication, and other anti-edema measures (rest, ice, compression, elevation). Following the acute phase, a physical therapy regimen may be utilized to focus on muscle strengthening, ankle range of motion, and proprioceptive or postural training (Figure 1). Proprioceptive therapy, such as with a Biomechanical Ankle Platform System, is crucial in regaining and to re-establish positional control vis-à-vis inversion ankle stress[60]. Similarly, external restraints and orthotics not only confer mechanical stability, but also likely provide some degree of short-term proprioceptive feedback in order to accelerate the recovery process[56-62].
Figure 1.

Clinical image demonstrating proprioceptive training during physical therapy.
Karlsson et al[63] reported that early functional treatment could significantly reduce the time required to return to work or preinjury sport. Furthermore, van Os et al[64] published a thorough review demonstrating that functional treatment with concomitant supervised physical therapy could yield superior recovery results when compared with functional treatment alone, specifically with regard to persistent swelling and time for return to work. Multiple authors have also reported significant reduction in recurrent ankle injury, attributable to proprioceptive training as part of a rehabilitation protocol[63-69].
Ardèvol et al[56] published results from a randomized controlled trial comparing cast immobilization with functional management in an athletic cohort. They found that patients managed with a functional protocol were able return to sporting activity sooner, and had fewer symptoms at three and six months following injury. Although they did not find a statistically significant difference in reinjury rates between the two groups, they did report less ligamentous laxity radiographically in the cohort managed with a functional protocol. In 2002, Kerkhoffs et al[57] performed a meta-analysis of randomized controlled trials comparing rigid immobilization and functional management of acute lateral ankle sprains. They reported a higher return to sport percentage in patients managed with functional protocols. They also reported faster return to work, better range of motion and a lower prevalence of persistent swelling and ligamentous laxity at intermediate follow-up, when compared to patients treated with rigid immobilization[54,57].
Surgical management of acute lateral ankle ligamentous injuries remains controversial; however, the majority of treating providers recommend a thorough three to six month course of nonoperative treatment before consideration of surgical management. In 2003, Pijnenburg et al[60] published their findings of a randomized prospective trial comparing functional treatment with primary surgical repair using the technique described by Prins[61], for patients with acute lateral ankle ligamentous injuries. The authors reported superiority with regard to pain, instability, and recurrent ankle sprains in patients treated with ligament repair. However, these authors advised caution in extrapolating their findings to the general population. They cited higher cost, higher risk of complications, and comparable results with delayed repair when comparing initial functional non-operative management of patients with acute ankle sprains[60].
Conversely, Tiling et al[70] performed a thorough review of 24 trials comparing surgical and functional management of ankle sprains and concluded that no significant difference was found between the two treatment strategies. More recently, in 2010, Pihlajamäki et al[71] reported the results of their prospective randomized trial, in an active Finnish patient population. These authors compared functional management to suture repair of ruptured ligaments within 1 wk of injury for acute grade III lateral ankle ligaments. They concluded that surgical repair and functional treatment of these injuries resulted in equivalent results with respect to recovery to preinjury activity level. Although surgery did appear to decrease the incidence of lateral ligament reinjury in their study population, the found that osteoarthritis was observed significantly more frequently in the surgical group[71].
CHRONIC ANKLE INSTABILITY TREATMENT
Patients with chronic ankle instability can be further stratified into two categories, which are not necessarily mutually exclusive. Mechanical instability is identifiable on physical examination and stress radiographs, whereas functional instability reflects subjective, patient-reported complaints of the ankle instability with or without clinical laxity[54,72,73]. Surgery is generally reserved for patients with chronic ankle stability that have failed to improve with a thorough course of conservative management and physical therapy. Similar to that for acute ankle sprain, nonoperative measures for chronic instability emphasize peroneal strengthening, proprioceptive training, lateral heel wedges, and strapping or bracing[52]. Patients with functional instability without demonstrable mechanical instability are more likely to benefit from these non-operative measures[54,73].
Modern surgical techniques for chronic lateral ankle instability can be divided into two broad categories: anatomic ligament repair (Figure 2) and non-anatomic reconstruction (Figure 3). Anatomic repair can be performed with or without augmentation and/or tenodesis, while non-anatomic reconstruction is typically performed with tenodesis[54,74]. The goal of anatomic ligament repair is restore native ankle anatomy, stability, and joint kinematics, while preserving functional ankle and subtalar motion. This can be accomplished with the use of local tissue, free tendon graft, or both. While this type of repair is a technically simpler surgery than non-anatomic reconstruction procedures, its success is dependent on the condition of the injured tissues, and may sometimes require augmentation[74-78].
Figure 2.
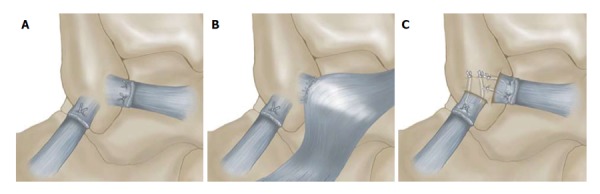
Anatomic repair of the lateral ligamentous complex[54]. Illustration demonstrating anatomic repair of chronic lateral ankle instability. A: Broström anatomic repair, demonstrating midsubstance imbrication and suture of the ruptured ligament ends; B: Gould modification augmented with the mobilized lateral portion of the extensor retinaculum; C: Karlsson modification, which involves anchoring the proximal ligament ends through drill holes.
Figure 3.
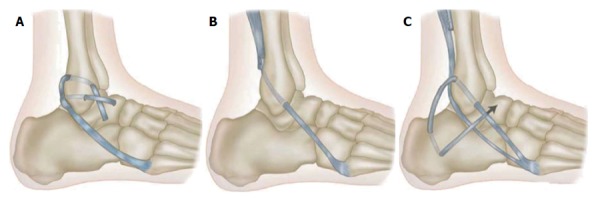
Selected techniques for non-anatomic lateral ligament reconstruction[54]. Tenodesis reconstruction for chronic lateral ankle instability. A: Watson-Jones procedure; B: Evans procedure; C: Chrisman-Snook procedure.
Non-anatomic reconstructions utilize tenodesis fixation to stabilize the ankle with the repair of the native ligaments. While multiple configurations have been described, most techniques involve rerouting of the peroneus brevis around the lateral ankle, and include the Watson-Jones, Evans, and Chrisman-Snook procedures (Figure 3)[74,79-82]. Long-term outcomes of non-anatomic reconstructions are hindered by alterations in ankle and hindfoot kinematics and often, resultant loss of subtalar motion[83-90]. Although initial reports were promising, comparison studies with longer follow-up generally favor anatomic repair over non-anatomic tenodesis reconstructions. Between 2000-2001, Krips et al[87,88] published a series of comparison studies, including more than 300 patients, with up to 30 years of follow-up data. These authors ultimately concluded that long-term, non-anatomic tenodesis lead to decreased function, increased pain, limited range of motion, instability, increased need for revision procedures, and greater degrees of osteoarthritis compared to anatomic reconstructions.
Since its first description in a series of 60 patients in 1966, the Broström technique has as evolved into the foundation for anatomic lateral ankle ligament repairs, with imbrication of ruptured ATFL and/or CFL[54,91]. In 1980, Gould et al[92] described the augmentation of the Broström repair with the inferior extensor retinaculum secured to the fibula following ligament repair. In 1988, Karlsson et al[93] reported that the ATFL and CFL were often found to be elongated and scarred, rather than disrupted. Based on this observation, these authors recommended imbrication of the attenuated ligaments followed by reinsertion into the fibula in their anatomic position with drill holes. Variations of anatomic repairs of the lateral ankle ligaments have a long track record in the literature, yielding good to excellent results in 85% of patients[54,74,86-88,94]. The use of a periosteal flap from the fibula, as well as autologous free tendon graft and allograft augments, has also been well described with favorable results[75,76,78]. Furthermore, sustained excellent patient outcomes have been reported by Bell et al[95] at greater than 20-year follow-up, and this procedure has demonstrable success in high-demand athletes[96].
Anatomic tenodesis procedures have recently been the subject of multiple investigations and have demonstrated promising results[54,74,87,88,97]. The goal of this type of a repair is to augment an anatomical lateral ankle ligament repair, without sacrificing anatomy or kinematics in the reconstruction. In 1995, Colville et al[77], described introduced a reconstruction using a split peroneus brevis tendon to augment the repair of the ATFL and CFL in a small series, with encouraging clinical outcomes. Although long term data is not yet available, multiple authors have demonstrated maintenance of mechanical stability after these procedures while preserving the normal range of motion of the ankle and subtalar joints[74,77,87,88]. Graft position and ankle position during graft tensioning are likely critical for the success of this type of reconstruction and may become more relevant in light of the declining, long-term results of standard non-anatomic tenodesis[98,99].
In 1996, Hennrikus et al[86] prospectively compared the modified Broström with the Chrisman-Snook procedure in 40 patients. Both demonstrated improvement in more than 80% of patients, although those who underwent a modified Broström procedure had a lower rate of complications and a higher Sefton[100] outcomes scores. The authors concluded that the modified Broström procedure was superior to the Chrisman-Snook procedure for chronic lateral ankle instability. Subsequently, meta-analyses by de Vries et al[89,90] have evaluated the available randomized trials comparing the surgical procedures commonly performed. The authors were not unable to reach a conclusion regarding the best surgical option for management of chronic ankle instability, given the lack of statistical significance and poor methodological quality of the randomized controlled trials performed to date. Rigorous research is still needed to determine the most effective surgical strategy for treating this important problem.
The role of ankle arthroscopy in lateral ligament reconstruction is not yet well defined. In 1955, Bosien et al[101] cited a 6.5% incidence of osteochondral fractures of the talus with ankle sprains, and more recent studies have investigated the presence of articular abnormalities with both acute ankle sprain and chronic instability[102]. In 1999, Komenda et al[103] examined arthroscopically 54 consecutive patients with lateral ankle instability before ligament stabilization and noted frequent intra-articular pathology, including a 25% incidence of articular chondral injury. These authors concluded that articular cartilage injuries are common in patients with lateral ankle instability and can be successfully addressed with ankle arthroscopy in addition to open ligament stabilization. The indications for arthroscopy before lateral ligamentous repair remain ill defined, but these reports and others suggest that it is important to rule out associated injuries in patients with painful unstable ankles.
Advancements in MRI technology and its ready availability in many healthcare settings may be helpful in identifying associated osteochondral lesions of the talus and peroneal tendon pathology. Its use may be valuable in determining the utility of concomitant arthroscopy, particularly in the presence of mechanical symptoms, chronic ankle pain, or other focal findings on physical examination.
Bony malalignment can play an important role in the etiology and treatment of ankle instability. Specifically, hindfoot varus, first ray plantarflexion, or midfoot cavus can predispose patients to chronic lateral ankle instability and contribute to early operative failure if not addressed with a corrective procedure at the time of surgery. Concomitant calcaneal osteotomy for cavovarus deformity has been advocated for patients with varus hindfoot deformity in conjunction with lateral ligamentous surgery[74,104,105]. Csizy et al[104] published a series of six patients with ankle instability and a varus calcaneus treated successfully with a Dwyer-type osteotomy and ligament reconstruction. Fortin et al[105] reported 13 patients with combined cavovarus foot deformity and ankle instability, half of whom required ankle fusion due to advanced degenerative changes. The remaining patients were effectively treated with calcaneal osteotomy and dorsiflexion osteotomy of the first metatarsal, depending on the rigidity of the deformity.
A high index of suspicion for ankle and hindfoot malalignment, associated peroneal tendon pathology and generalized ligamentous laxity are each of great importance when evaluating the patient with and planning surgery for ankle instability[74]. Concomitant osteoarticular injuries are an increasingly identified component of ankle pain associated with ankle instability[52,101,103]. It is crucial that these common defects, as well as other periarticular pathology be recognized when ankle instability is diagnosed and treated.
PREVENTATIVE MEASURES
There are multiple practical measures that may be utilized to mitigate modifiable risk factors and reduce the risk of ankle sprain in athletic patient populations. Weight loss with BMI optimization, as well as activity appropriate footwear and external restraints are among recommendations that may be considered. Several interventions have demonstrated success in achieving these goals without significant effects on quality of life or impeding athletic performance. By increasing passive restraints to ankle inversion and enhancing postural stability, prophylactic bracing in high-risk athletes has demonstrated success reducing the risk of primary and recurrent ankle sprain by up to 50%[41,106,107]. In one prospective randomized trial, Sitler et al[41] demonstrated a threefold increased risk for ankle sprain among unbraced basketball players when compared to braced athletes over a two-year time period at the United States Military Academy. Among paratroopers, a recent systematic review revealed that the external parachute ankle brace reduced all ankle injuries, including ankle sprain, by approximately half while saving between 0.6 and 3.4 million dollars in direct and indirect costs[19].
Neuromuscular training programs have also demonstrated success in reducing the risk of ankle sprain. In a meta-analysis, McKeon et al[37] reported that targeted balance control training resulted in a 20% to 60% relative risk reduction for lateral ankle sprain, particularly in athletes with having sustained prior ankle sprains. More effective screening of high-risk athletes and better objective measures for diagnosis, prophylactic interventions have to potential to benefit a larger number of athletes, reducing the overall incidence of ankle sprain and its potential burden on healthcare systems.
CONCLUSION
Acute and chronic ankle stability are a common source of disability in athletes and other high-demand patient populations, and may result in significant long-term sequelae, particularly with osteochondral lesions of the talus or peroneal tendon pathology. With enhanced screening based on known epidemiological risk factors, functional rehabilitation programs and prophylactic bracing may mitigate further lateral ankle instability with further physical activity. Anatomic surgical repair or reconstruction may be considered after failure of nonoperative measures, with high rates of return to full function in active patient cohorts.
ACKNOWLEDGMENTS
We would like to thank MAJ Justin D Orr, MD for his clinical images. The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of Defense or the United States government. The authors are employees of the United States nment.
Footnotes
P- Reviewer: Paschalis V, Vosoughi AR S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
Conflict-of-interest: I declare that I have no conflicts of interest in the authorship or publication of this contribution.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: December 31, 2013
First decision: January 20, 2014
Article in press: December 31, 2014
References
- 1.Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37:280–285. doi: 10.1016/s1067-2516(98)80063-x. [DOI] [PubMed] [Google Scholar]
- 2.Ferran NA, Maffulli N. Epidemiology of sprains of the lateral ankle ligament complex. Foot Ankle Clin. 2006;11:659–662. doi: 10.1016/j.fcl.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Waterman BR, Belmont PJ, Cameron KL, Svoboda SJ, Alitz CJ, Owens BD. Risk factors for syndesmotic and medial ankle sprain: role of sex, sport, and level of competition. Am J Sports Med. 2011;39:992–998. doi: 10.1177/0363546510391462. [DOI] [PubMed] [Google Scholar]
- 4.Waterman BR, Belmont PJ, Cameron KL, Deberardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38:797–803. doi: 10.1177/0363546509350757. [DOI] [PubMed] [Google Scholar]
- 5.DiGiovanni BF, Partal G, Baumhauer JF. Acute ankle injury and chronic lateral instability in the athlete. Clin Sports Med. 2004;23:1–19, v. doi: 10.1016/S0278-5919(03)00095-4. [DOI] [PubMed] [Google Scholar]
- 6.Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 7.Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311–319. [PMC free article] [PubMed] [Google Scholar]
- 8.Milgrom C, Shlamkovitch N, Finestone A, Eldad A, Laor A, Danon YL, Lavie O, Wosk J, Simkin A. Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle. 1991;12:26–30. doi: 10.1177/107110079101200105. [DOI] [PubMed] [Google Scholar]
- 9.Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 10.Cordova ML, Sefton JM, Hubbard TJ. Mechanical joint laxity associated with chronic ankle instability: a systematic review. Sports Health. 2010;2:452–459. doi: 10.1177/1941738110382392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bridgman SA, Clement D, Downing A, Walley G, Phair I, Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England, and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20:508–510. doi: 10.1136/emj.20.6.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. 1984;(183):160–168. [PubMed] [Google Scholar]
- 13.Gerber JP, Williams GN, Scoville CR, Arciero RA, Taylor DC. Persistent disability associated with ankle sprains: a prospective examination of an athletic population. Foot Ankle Int. 1998;19:653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 14.Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hølmer P, Søndergaard L, Konradsen L, Nielsen PT, Jørgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15:72–74. doi: 10.1177/107110079401500204. [DOI] [PubMed] [Google Scholar]
- 16.Cameron KL, Owens BD, DeBerardino TM. Incidence of ankle sprains among active-duty members of the United States Armed Services from 1998 through 2006. J Athl Train. 2010;45:29–38. doi: 10.4085/1062-6050-45.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lillywhite LP. Analysis of extrinsic factor associated with 379 injuries occurring during 34,236 military parachute descents. J R Army Med Corps. 1991;137:115–121. doi: 10.1136/jramc-137-03-02. [DOI] [PubMed] [Google Scholar]
- 18.Knapik JJ, Spiess A, Swedler DI, Grier TL, Darakjy SS, Jones BH. Systematic review of the parachute ankle brace: injury risk reduction and cost effectiveness. Am J Prev Med. 2010;38:S182–S188. doi: 10.1016/j.amepre.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 19.Luippold RS, Sulsky SI, Amoroso PJ. Effectiveness of an external ankle brace in reducing parachuting-related ankle injuries. Inj Prev. 2011;17:58–61. doi: 10.1136/ip.2009.025981. [DOI] [PubMed] [Google Scholar]
- 20.Beynnon BD, Murphy DF, Alosa DM. Predictive Factors for Lateral Ankle Sprains: A Literature Review. J Athl Train. 2002;37:376–380. [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy DF, Connolly DA, Beynnon BD. Risk factors for lower extremity injury: a review of the literature. Br J Sports Med. 2003;37:13–29. doi: 10.1136/bjsm.37.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cameron KL. Commentary: Time for a paradigm shift in conceptualizing risk factors in sports injury research. J Athl Train. 2010;45:58–60. doi: 10.4085/1062-6050-45.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Williams JG. Aetiologic classification of injuries in sportsmen. Br J Sports Med. 1971;5:228–230. [Google Scholar]
- 24.Frank C, Amiel D, Woo SL, Akeson W. Normal ligament properties and ligament healing. Clin Orthop Relat Res. 1985;(196):15–25. [PubMed] [Google Scholar]
- 25.Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34:471–475. doi: 10.1177/0363546505280429. [DOI] [PubMed] [Google Scholar]
- 26.Ekstrand J, Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15:267–270. doi: 10.1249/00005768-198315030-00014. [DOI] [PubMed] [Google Scholar]
- 27.McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malliaropoulos N, Ntessalen M, Papacostas E, Longo UG, Maffulli N. Reinjury after acute lateral ankle sprains in elite track and field athletes. Am J Sports Med. 2009;37:1755–1761. doi: 10.1177/0363546509338107. [DOI] [PubMed] [Google Scholar]
- 29.Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- 30.Leanderson J, Eriksson E, Nilsson C, Wykman A. Proprioception in classical ballet dancers. A prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am J Sports Med. 1996;24:370–374. doi: 10.1177/036354659602400320. [DOI] [PubMed] [Google Scholar]
- 31.Perrin PP, Béné MC, Perrin CA, Durupt D. Ankle trauma significantly impairs posture control--a study in basketball players and controls. Int J Sports Med. 1997;18:387–392. doi: 10.1055/s-2007-972651. [DOI] [PubMed] [Google Scholar]
- 32.McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Trojian TH, McKeag DB. Single leg balance test to identify risk of ankle sprains. Br J Sports Med. 2006;40:610–663; discussion 613. doi: 10.1136/bjsm.2005.024356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mohammadi F, Roozdar A. Effects of fatigue due to contraction of evertor muscles on the ankle joint position sense in male soccer players. Am J Sports Med. 2010;38:824–828. doi: 10.1177/0363546509354056. [DOI] [PubMed] [Google Scholar]
- 35.Stecco C, Macchi V, Porzionato A, Morra A, Parenti A, Stecco A, Delmas V, De Caro R. The ankle retinacula: morphological evidence of the proprioceptive role of the fascial system. Cells Tissues Organs. 2010;192:200–210. doi: 10.1159/000290225. [DOI] [PubMed] [Google Scholar]
- 36.Riemann BL. Is There a Link Between Chronic Ankle Instability and Postural Instability? J Athl Train. 2002;37:386–393. [PMC free article] [PubMed] [Google Scholar]
- 37.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train. 2008;43:305–315. doi: 10.4085/1062-6050-43.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beynnon BD, Renström PA, Alosa DM, Baumhauer JF, Vacek PM. Ankle ligament injury risk factors: a prospective study of college athletes. J Orthop Res. 2001;19:213–220. doi: 10.1016/S0736-0266(00)90004-4. [DOI] [PubMed] [Google Scholar]
- 39.Hosea TM, Carey CC, Harrer MF. The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop Relat Res. 2000;(372):45–49. doi: 10.1097/00003086-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Gwinn DE, Wilckens JH, McDevitt ER, Ross G, Kao TC. The relative incidence of anterior cruciate ligament injury in men and women at the United States Naval Academy. Am J Sports Med. 2000;28:98–102. doi: 10.1177/03635465000280012901. [DOI] [PubMed] [Google Scholar]
- 41.Sitler M, Ryan J, Wheeler B, McBride J, Arciero R, Anderson J, Horodyski M. The efficacy of a semirigid ankle stabilizer to reduce acute ankle injuries in basketball. A randomized clinical study at West Point. Am J Sports Med. 1994;22:454–461. doi: 10.1177/036354659402200404. [DOI] [PubMed] [Google Scholar]
- 42.Arnason A, Gudmundsson A, Dahl HA, Jóhannsson E. Soccer injuries in Iceland. Scand J Med Sci Sports. 1996;6:40–45. doi: 10.1111/j.1600-0838.1996.tb00069.x. [DOI] [PubMed] [Google Scholar]
- 43.Chomiak J, Junge A, Peterson L, Dvorak J. Severe injuries in football players. Influencing factors. Am J Sports Med. 2000;28:S58–S68. doi: 10.1177/28.suppl_5.s-58. [DOI] [PubMed] [Google Scholar]
- 44.Kujala UM, Taimela S, Antti-Poika I, Orava S, Tuominen R, Myllynen P. Acute injuries in soccer, ice hockey, volleyball, basketball, judo, and karate: analysis of national registry data. BMJ. 1995;311:1465–1468. doi: 10.1136/bmj.311.7018.1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sullivan JA, Gross RH, Grana WA, Garcia-Moral CA. Evaluation of injuries in youth soccer. Am J Sports Med. 1980;8:325–327. doi: 10.1177/036354658000800505. [DOI] [PubMed] [Google Scholar]
- 46.Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33:1485–1491. doi: 10.1177/0363546505275490. [DOI] [PubMed] [Google Scholar]
- 47.Peterson L, Junge A, Chomiak J, Graf-Baumann T, Dvorak J. Incidence of football injuries and complaints in different age groups and skill-level groups. Am J Sports Med. 2000;28:S51–S57. doi: 10.1177/28.suppl_5.s-51. [DOI] [PubMed] [Google Scholar]
- 48.Dvorak J, Junge A, Chomiak J, Graf-Baumann T, Peterson L, Rösch D, Hodgson R. Risk factor analysis for injuries in football players. Possibilities for a prevention program. Am J Sports Med. 2000;28:S69–S74. doi: 10.1177/28.suppl_5.s-69. [DOI] [PubMed] [Google Scholar]
- 49.Olsen OE, Myklebust G, Engebretsen L, Holme I, Bahr R. Exercises to prevent lower limb injuries in youth sports: cluster randomised controlled trial. BMJ. 2005;330:449. doi: 10.1136/bmj.38330.632801.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ekstrand J, Gillquist J, Möller M, Oberg B, Liljedahl SO. Incidence of soccer injuries and their relation to training and team success. Am J Sports Med. 1983;11:63–67. doi: 10.1177/036354658301100203. [DOI] [PubMed] [Google Scholar]
- 51.Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- 52.Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69:17–26. [PubMed] [Google Scholar]
- 53.Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Reardon M, Stewart JP, Maloney J. Decision rules for the use of radiography in acute ankle injuries. Refinement and prospective validation. JAMA. 1993;269:1127–1132. doi: 10.1001/jama.269.9.1127. [DOI] [PubMed] [Google Scholar]
- 54.Maffulli N, Ferran NA. Management of acute and chronic ankle instability. J Am Acad Orthop Surg. 2008;16:608–615. doi: 10.5435/00124635-200810000-00006. [DOI] [PubMed] [Google Scholar]
- 55.Frost SC, Amendola A. Is stress radiography necessary in the diagnosis of acute or chronic ankle instability? Clin J Sport Med. 1999;9:40–45. doi: 10.1097/00042752-199901000-00008. [DOI] [PubMed] [Google Scholar]
- 56.Ardèvol J, Bolíbar I, Belda V, Argilaga S. Treatment of complete rupture of the lateral ligaments of the ankle: a randomized clinical trial comparing cast immobilization with functional treatment. Knee Surg Sports Traumatol Arthrosc. 2002;10:371–377. doi: 10.1007/s00167-002-0308-9. [DOI] [PubMed] [Google Scholar]
- 57.Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly K, Struijs PA, van Dijk CN. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;(3):CD003762. doi: 10.1002/14651858.CD003762. [DOI] [PubMed] [Google Scholar]
- 58.Kerkhoffs GM, Struijs PA, Marti RK, Blankevoort L, Assendelft WJ, van Dijk CN. Functional treatments for acute ruptures of the lateral ankle ligament: a systematic review. Acta Orthop Scand. 2003;74:69–77. doi: 10.1080/00016470310013699. [DOI] [PubMed] [Google Scholar]
- 59.Mattacola CG, Dwyer MK. Rehabilitation of the Ankle After Acute Sprain or Chronic Instability. J Athl Train. 2002;37:413–429. [PMC free article] [PubMed] [Google Scholar]
- 60.Pijnenburg AC, Bogaard K, Krips R, Marti RK, Bossuyt PM, van Dijk CN. Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomised, prospective trial. J Bone Joint Surg Br. 2003;85:525–530. doi: 10.1302/0301-620x.85b4.13928. [DOI] [PubMed] [Google Scholar]
- 61.Prins JG. Diagnosis and treatment of injury to the lateral ligament of the ankle. A comparative clinical study. Acta Chir Scand Suppl. 1978;486:3–149. [PubMed] [Google Scholar]
- 62.Polzer H, Kanz KG, Prall WC, Haasters F, Ockert B, Mutschler W, Grote S. Diagnosis and treatment of acute ankle injuries: development of an evidence-based algorithm. Orthop Rev (Pavia) 2012;4:e5. doi: 10.4081/or.2012.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Karlsson J, Eriksson BI, Swärd L. Early functional treatment for acute ligament injuries of the ankle joint. Scand J Med Sci Sports. 1996;6:341–345. doi: 10.1111/j.1600-0838.1996.tb00104.x. [DOI] [PubMed] [Google Scholar]
- 64.van Os AG, Bierma-Zeinstra SM, Verhagen AP, de Bie RA, Luijsterburg PA, Koes BW. Comparison of conventional treatment and supervised rehabilitation for treatment of acute lateral ankle sprains: a systematic review of the literature. J Orthop Sports Phys Ther. 2005;35:95–105. doi: 10.2519/jospt.2005.35.2.95. [DOI] [PubMed] [Google Scholar]
- 65.Drez D, Young JC, Waldman D, Shackleton R, Parker W. Nonoperative treatment of double lateral ligament tears of the ankle. Am J Sports Med. 1982;10:197–200. doi: 10.1177/036354658201000401. [DOI] [PubMed] [Google Scholar]
- 66.Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14:465–471. doi: 10.1177/036354658601400606. [DOI] [PubMed] [Google Scholar]
- 67.Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999;9:104–109. doi: 10.1111/j.1600-0838.1999.tb00217.x. [DOI] [PubMed] [Google Scholar]
- 68.Hupperets MD, Verhagen EA, van Mechelen W. Effect of sensorimotor training on morphological, neurophysiological and functional characteristics of the ankle: a critical review. Sports Med. 2009;39:591–605. doi: 10.2165/00007256-200939070-00005. [DOI] [PubMed] [Google Scholar]
- 69.Mohammadi F. Comparison of 3 preventive methods to reduce the recurrence of ankle inversion sprains in male soccer players. Am J Sports Med. 2007;35:922–926. doi: 10.1177/0363546507299259. [DOI] [PubMed] [Google Scholar]
- 70.Tiling T, Bonk A, Höher J, Klein J. [Acute injury to the lateral ligament of the ankle joint in the athlete] Chirurg. 1994;65:920–933. [PubMed] [Google Scholar]
- 71.Pihlajamäki H, Hietaniemi K, Paavola M, Visuri T, Mattila VM. Surgical versus functional treatment for acute ruptures of the lateral ligament complex of the ankle in young men: a randomized controlled trial. J Bone Joint Surg Am. 2010;92:2367–2374. doi: 10.2106/JBJS.I.01176. [DOI] [PubMed] [Google Scholar]
- 72.DiGiovanni CW, Brodsky A. Current concepts: lateral ankle instability. Foot Ankle Int. 2006;27:854–866. doi: 10.1177/107110070602701019. [DOI] [PubMed] [Google Scholar]
- 73.Ajis A, Maffulli N. Conservative management of chronic ankle instability. Foot Ankle Clin. 2006;11:531–537. doi: 10.1016/j.fcl.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 74.Colville MR. Surgical treatment of the unstable ankle. J Am Acad Orthop Surg. 1998;6:368–377. doi: 10.5435/00124635-199811000-00005. [DOI] [PubMed] [Google Scholar]
- 75.Okazaki K, Miyagi S, Tokunaga J. Anatomic reconstruction of the lateral ligament of the ankle using a periosteal flap from the fibula. Tech Foot Ankle Surg. 2005;4:98–103. [Google Scholar]
- 76.Rudert M, Wülker N, Wirth CJ. Reconstruction of the lateral ligaments of the ankle using a regional periosteal flap. J Bone Joint Surg Br. 1997;79:446–451. doi: 10.1302/0301-620x.79b3.7183. [DOI] [PubMed] [Google Scholar]
- 77.Colville MR, Grondel RJ. Anatomic reconstruction of the lateral ankle ligaments using a split peroneus brevis tendon graft. Am J Sports Med. 1995;23:210–213. doi: 10.1177/036354659502300214. [DOI] [PubMed] [Google Scholar]
- 78.Paterson R, Cohen B, Taylor D, Bourne A, Black J. Reconstruction of the lateral ligaments of the ankle using semi-tendinosis graft. Foot Ankle Int. 2000;21:413–419. doi: 10.1177/107110070002100510. [DOI] [PubMed] [Google Scholar]
- 79.Watson-Jones R. Recurrent forward dislocation of the ankle joint. J Bone Joint Surg Br. 1952;134:519. [Google Scholar]
- 80.Evans DL. Recurrent instability of the ankle; a method of surgical treatment. Proc R Soc Med. 1953;46:343–344. doi: 10.1177/003591575304600507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chrisman OD, Snook GA. Reconstruction of lateral ligament tears of the ankle. An experimental study and clinical evaluation of seven patients treated by a new modification of the Elmslie procedure. J Bone Joint Surg Am. 1969;51:904–912. [PubMed] [Google Scholar]
- 82.Krips R, Brandsson S, Swensson C, van Dijk CN, Karlsson J. Anatomical reconstruction and Evans tenodesis of the lateral ligaments of the ankle. Clinical and radiological findings after follow-up for 15 to 30 years. J Bone Joint Surg Br. 2002;84:232–236. doi: 10.1302/0301-620x.84b2.12143. [DOI] [PubMed] [Google Scholar]
- 83.Bahr R, Pena F, Shine J, Lew WD, Tyrdal S, Engebretsen L. Biomechanics of ankle ligament reconstruction. An in vitro comparison of the Broström repair, Watson-Jones reconstruction, and a new anatomic reconstruction technique. Am J Sports Med. 1997;25:424–432. doi: 10.1177/036354659702500402. [DOI] [PubMed] [Google Scholar]
- 84.Korkala O, Tanskanen P, Mäkijärvi J, Sorvali T, Ylikoski M, Haapala J. Long-term results of the Evans procedure for lateral instability of the ankle. J Bone Joint Surg Br. 1991;73:96–99. doi: 10.1302/0301-620X.73B1.1991787. [DOI] [PubMed] [Google Scholar]
- 85.Korkala O, Sorvali T, Niskanen R, Haapala J, Tanskanen P, Kuokkanen H. Twenty-year results of the Evans operation for lateral instability of the ankle. Clin Orthop Relat Res. 2002;(405):195–198. doi: 10.1097/00003086-200212000-00025. [DOI] [PubMed] [Google Scholar]
- 86.Hennrikus WL, Mapes RC, Lyons PM, Lapoint JM. Outcomes of the Chrisman-Snook and modified-Broström procedures for chronic lateral ankle instability. A prospective, randomized comparison. Am J Sports Med. 1996;24:400–404. doi: 10.1177/036354659602400402. [DOI] [PubMed] [Google Scholar]
- 87.Krips R, van Dijk CN, Halasi T, Lehtonen H, Moyen B, Lanzetta A, Farkas T, Karlsson J. Anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: a 2- to 10-year follow-up, multicenter study. Knee Surg Sports Traumatol Arthrosc. 2000;8:173–179. doi: 10.1007/s001670050210. [DOI] [PubMed] [Google Scholar]
- 88.Krips R, van Dijk CN, Halasi PT, Lehtonen H, Corradini C, Moyen B, Karlsson J. Long-term outcome of anatomical reconstruction versus tenodesis for the treatment of chronic anterolateral instability of the ankle joint: a multicenter study. Foot Ankle Int. 2001;22:415–421. doi: 10.1177/107110070102200510. [DOI] [PubMed] [Google Scholar]
- 89.de Vries JS, Krips R, Sierevelt IN, Blankevoort L. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2006;(4):CD004124. doi: 10.1002/14651858.CD004124.pub2. [DOI] [PubMed] [Google Scholar]
- 90.de Vries JS, Krips R, Sierevelt IN, Blankevoort L, van Dijk CN. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;(8):CD004124. doi: 10.1002/14651858.CD004124.pub3. [DOI] [PubMed] [Google Scholar]
- 91.Broström L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551–565. [PubMed] [Google Scholar]
- 92.Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84–89. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- 93.Karlsson J, Bergsten T, Lansinger O, Peterson L. Reconstruction of the lateral ligaments of the ankle for chronic lateral instability. J Bone Joint Surg Am. 1988;70:581–588. [PubMed] [Google Scholar]
- 94.Hamilton WG, Thompson FM, Snow SW. The modified Brostrom procedure for lateral ankle instability. Foot Ankle. 1993;14:1–7. doi: 10.1177/107110079301400101. [DOI] [PubMed] [Google Scholar]
- 95.Bell SJ, Mologne TS, Sitler DF, Cox JS. Twenty-six-year results after Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2006;34:975–978. doi: 10.1177/0363546505282616. [DOI] [PubMed] [Google Scholar]
- 96.Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009;37:488–494. doi: 10.1177/0363546508327541. [DOI] [PubMed] [Google Scholar]
- 97.Colville MR, Marder RA, Zarins B. Reconstruction of the lateral ankle ligaments. A biomechanical analysis. Am J Sports Med. 1992;20:594–600. doi: 10.1177/036354659202000518. [DOI] [PubMed] [Google Scholar]
- 98.Sammarco GJ, Idusuyi OB. Reconstruction of the lateral ankle ligaments using a split peroneus brevis tendon graft. Foot Ankle Int. 1999;20:97–103. doi: 10.1177/107110079902000205. [DOI] [PubMed] [Google Scholar]
- 99.Acevedo JI, Myerson MS. Modification of the Chrisman-Snook technique. Foot Ankle Int. 2000;21:154–155. doi: 10.1177/107110070002100211. [DOI] [PubMed] [Google Scholar]
- 100.Sefton GK, George J, Fitton JM, McMullen H. Reconstruction of the anterior talofibular ligament for the treatment of the unstable ankle. J Bone Joint Surg Br. 1979;61-B:352–354. doi: 10.1302/0301-620X.61B3.113415. [DOI] [PubMed] [Google Scholar]
- 101.Bosien WR, Staples OS, Russell SW. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37-A:1237–1243. [PubMed] [Google Scholar]
- 102.Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005;33:686–692. doi: 10.1177/0363546504270566. [DOI] [PubMed] [Google Scholar]
- 103.Komenda GA, Ferkel RD. Arthroscopic findings associated with the unstable ankle. Foot Ankle Int. 1999;20:708–713. doi: 10.1177/107110079902001106. [DOI] [PubMed] [Google Scholar]
- 104.Csizy M, Hintermann B. [Dwyer osteotomy with or without lateral stabilization in calcaneus varus with lateral ligament insufficiency of the upper ankle joint] Sportverletz Sportschaden. 1996;10:100–102. doi: 10.1055/s-2007-993410. [DOI] [PubMed] [Google Scholar]
- 105.Fortin PT, Guettler J, Manoli A. Idiopathic cavovarus and lateral ankle instability: recognition and treatment implications relating to ankle arthritis. Foot Ankle Int. 2002;23:1031–1037. doi: 10.1177/107110070202301111. [DOI] [PubMed] [Google Scholar]
- 106.Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005;(2):CD000450. doi: 10.1002/14651858.CD000450.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Frey C, Feder KS, Sleight J. Prophylactic ankle brace use in high school volleyball players: a prospective study. Foot Ankle Int. 2010;31:296–300. doi: 10.3113/FAI.2010.0296. [DOI] [PubMed] [Google Scholar]


