Abstract
Visualization of the fundus is an important component of any ophthalmologic exam. Students are taught to visualize the fundus using a direct handheld ophthalmoscope. However, this device has many limitations, which may be a detriment to medical education and patient care. The invention of the non-mydriatic automatic fundus camera could significantly improve medical education. Our study examined the ability of a group of 5 medical students to visualize pathology and form a diagnosis with a traditional handheld ophthalmoscope and an automatic fundus camera. With the direct ophthalmoscope, none of the students were able to visualize the macula, a crucial aspect of the ophthalmologic exam. With the automatic fundus camera, all students were able to visualize the fundus. The latter modality also increased the proportion of students that was able to correctly diagnose the patients with diabetic retinopathy, 100% vs 40%. On average, students were also more confident in their ability to visualize basic retinal anatomy with the automatic fundus camera, 9.6/10 vs 6.4/10. Thus, incorporating the non-mydriatic automatic fundus camera into medical education, alongside the handheld ophthalmoscope, has the potential to improve both learning outcomes and patient care.
Keywords: Ophthalmoscope, Medical Education, Fundus, Physical Exam
Introduction
Since the invention of the ophthalmoscope by Helmholtz in 1851, it has become a standard item in the repertoire of nearly every medical student.1 Although the device has undergone many changes over the past 150 years, the basic principles have remained the same. Using a source of illumination and a series of reflecting surfaces, the ophthalmoscope allows the clinician to observe the fundus. This can be an enormous benefit to the clinician, as it provides significant insight into a variety of conditions. Two notable examples include cardiovascular disease and diabetes, the number one and number seven cause of death in the United States, respectively.2 While both are potentially lethal, early detection can significantly reduce complications.3 Thus, it is vital that the aspiring clinician be able to accurately and clearly view the fundus, as a matter of patient safety. The handheld direct ophthalmoscope has many useful features. It is a lightweight, portable, and relatively inexpensive means of carrying out the fundoscopic examination. Over the past century it has become an important diagnostic tool for teaching medical students and residents the fundoscopic exam. However, due to the inherent difficulty in viewing the elderly non-dilated eye, its usage and utility for medical education is limited.4 Currently, many general practitioners do not even attempt to perform a fundus exam on patients with diabetic retinopathy and instead refer directly to an ophthalmologist.4
There are other more effective methods to view the fundus. Recent technological advances have resulted in the creation of the non-mydriatic automatic fundus camera (Table 1). This tool allows the clinician to clearly observe the fundus on an electronic screen. This enables one to zoom in on the retina, measure the vessels and lesions, share the images with patients, and document the images in the patient's file for follow up. It also reduces the many risks associated with dilation, including closed angle glaucoma, allergic reactions, and transient visual impairment. All of these benefits could translate into a more effective educational experience for medical students, as well as more effective patient care. Furthermore, a recent study from Emory suggests that students prefer the automatic fundus camera to the direct ophthalmoscope for examining the fundus.4
Table 1.
Comparing the non-mydriatic camera and direct ophthalmoscope
| Equipment | Cost | Portability | Clarity and Magnification | Training and Education | Digitally capable for electronic medical record | Comfort/ Ease of Use/ Patient Safety |
| AFC-230 Non-Mydriatic camera | $15000 / unlimited use | Poor | Excellent | Excellent | Yes | Excellent |
| Direct ophthalmoscope | $150/ person | Excellent | Poor | Poor | No | Poor |
This study seeks to compare the diagnostic capability of a handheld direct ophthalmoscope to an automatic fundus camera in diagnosing retinopathy for a group of medical students. We hypothesize that the latter will be more effective. Our study expands on a similar study by having students examine patients with macular pathology,4 instead of examining normal eyes. This will provide insight and foster discussion on the possible benefits and drawbacks of incorporating a non-mydriatic automatic fundus camera into medical education clinics, alongside a traditional handheld ophthalmoscope.
Methods
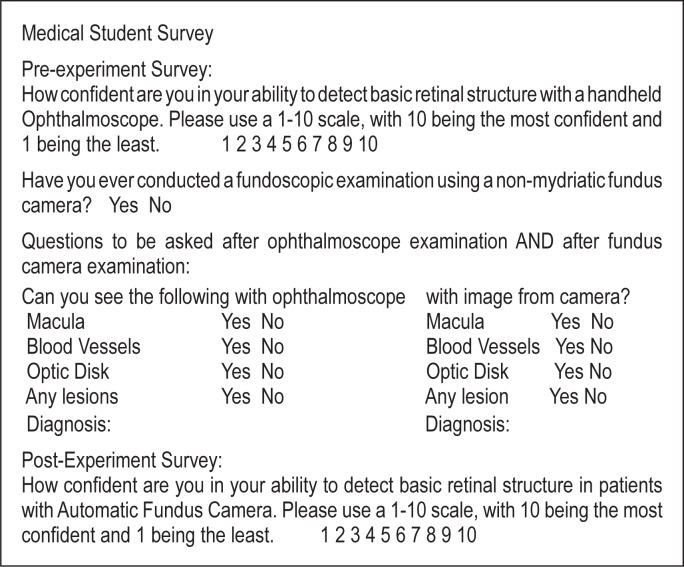
Institutional Review Board approval was obtained from the University of Hawai‘i. None of the authors had any conflict of interest. A group of five medical students from the University of Hawai‘i John A. Burns School of Medicine participated in the study. All students had previously received basic ophthalmoscope training during the first month of medical school. Immediately prior to the event, each student was given a short lecture handout on relevant retinal pathology, including common manifestations of diabetes mellitus type 2 and cardiovascular disease. Prior to examining the patients, the students were given a 15-minute introduction to direct ophthalmoscopy by a clinical associate professor in a private practice setting. This introduction demonstrated proper examination technique and reviewed the relevant anatomical structures of the eye. Each student then conducted a supervised fundoscopic examination on a fellow student without dilation in a dark room, to ensure that the exam was being correctly performed (Figure 1).
Figure 1.
Student practicing ophthalmoscope technique
Each student then conducted a fundoscopic exam using a standard direct handheld ophthalmoscope (Welch Allyn Inc., Skaneateles Falls, USA) on two undilated patients with known diabetic retinopathy. These patients had clearly observable pathology and a pupil size of 3 mm, which exceeded the minimum pupil size for the automatic fundus camera. Students were given no information on the patients' conditions beforehand. Each student examined the patients with a direct handheld ophthalmoscope, recorded his or her observations, and made a hypothesis. Students then examined the same patients using the AFC-230 Non-Mydriatic Auto Fundus Camera (Nidek Inc., Fremont, USA) (Figure 2). Again, each student recorded his or her observations and made a hypothesis.
Figure 2.
Patient receiving exam with non-mydriatic automatic fundus camera
Results
The ability of the students to visualize relevant anatomical structures with each of the two imaging modalities is listed in Table 2. Each of the 5 students examined 2 patients for a total of 10 responses. None of the students were able to visualize the macula with the direct ophthalmoscope in either patient. Students were able to view the remaining anatomical structures in 9 of 10 cases. All students were able to visualize all relevant anatomical structures with the automatic fundus camera.
Table 2.
Comparison of visualization capabilities
| Structure | Direct Handheld Ophthalmoscope (# of students able to visualize) | Nonmydriatic Automatic Fundus Camera (# of students able to visualize) |
| Macula | 0/10 | 10/10 |
| Vasculature | 9/10 | 10/10 |
| Optic Disk | 9/10 | 10/10 |
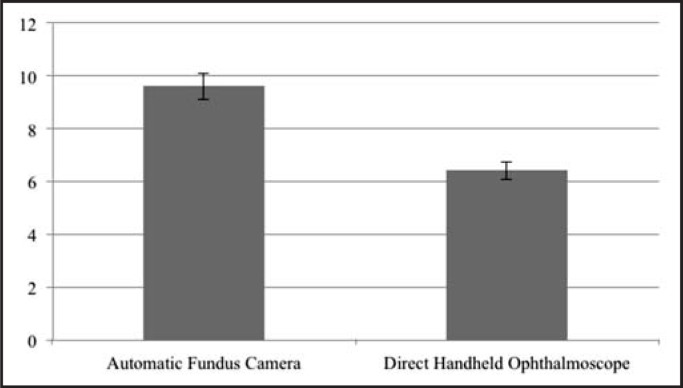
While using the direct handheld ophthalmoscope, 40% of the students accurately diagnosed the patients with diabetic retinopathy. While using the automatic fundus camera, 100% of the students accurately diagnosed the patient with diabetic retinopathy. Students were also asked to rate their confidence in visualizing basic retinal anatomy and pathology using the two modalities after conducting the exams. On a scale of 1 to 10, with 10 being the most confident, the average student response was 6.4 (range 6–7) for the direct handheld ophthalmoscope (Figure 3). The average response for the automatic fundus camera was 9.6 (range 9–10).
Figure 3.
Mean student confidence in visualizing basic anatomical structures and pathology (0–10 scale)
Discussion
The most notable discrepancy between the two imaging modalities was observed when trying to view the macula. Not a single student was able to confidently visualize the macula with the direct handheld ophthalmoscope, while all of the students were able to do so with the automatic fundus camera. This discrepancy is notable, given the numerous pathological lesions that can occur in this region of the eye. Macular pathology can be related to diabetes mellitus, as well as a variety of other conditions, such as senile macular degeneration and trauma.
Students were able to visualize the vasculature and optic disk with the handheld ophthalmoscope. However, there were multiple instances in which the crucial pathological cues, such as microaneurysms, flame shaped hemorrhages, and macular edema were missed (data not shown). Nearly all of these findings were observed by students when using the automatic fundus camera. The reason for this is evident, as the automatic fundus camera provides a stable image that can be magnified for greater clarity. Students were also significantly more confident about their diagnostic abilities when examining the patient with the automatic fundus camera. This confidence has the potential to translate into more effective patient care.
The automatic fundus camera also has many benefits from a teaching standpoint. It allows the educator to point out or confirm specific findings that may be relevant to the student's educational experience. It also allows the student and clinician to review the findings for longer periods of time or at a later time if needed. Having this new device more readily available could also reduce costs associated with diabetes mellitus type II. At this time, most diabetic patients, regardless of the extent of their disease, must be referred to an ophthalmologist at the expense of both time and money. Having automatic fundus cameras more readily available in clinics outside the ophthalmologist's office could reduce this burden.
All of these benefits suggest that the automatic fundus camera can be a useful accessory tool to help teach a proper fundoscopic examination. An ideal situation would be to use the automatic camera to take an initial picture and then let the students try to find the pathology with the handheld ophthalmoscope. This would be more effective than the current method of teaching, in which students have very little initial direction. Despite its evident utility, the automatic fundus camera is not utilized in most medical education settings. Only 40% of students in this study had ever used the device before. None of them had done so on a regular basis. One of the likely reasons for this is the cost of the device. While the device is indeed expensive, only a single device is needed at a given location. We believe that installing a single device at community health centers, outpatient clinics, and emergency rooms could provide the numerous aforementioned benefits.
Conclusion
The direct handheld ophthalmoscope is an essential part of the physical exam and an important skill for all medical students to learn. However, providing access to an automatic fundus camera, in addition to a direct ophthalmoscope, would benefit medical education and overall medical care.
Conflict of Interest
None of the authors identify a conflict of interest.
References
- 1.Keeler CR. The Ophthalmoscope in the Lifetime of Hermann von Helmholtz. Arch Ophthalmol. 2002;120:194–201. doi: 10.1001/archopht.120.2.194. [DOI] [PubMed] [Google Scholar]
- 2.Leading Causes of Death. Center for Disease Control and Prevention Web site. [April 6, 2013]. http://www.cdc.gov/nchs/fastats/lcod.htm. Updated December 30, 2013.
- 3.Black JA, Sharp SJ, Wareham NJ. Change in cardiovascular risk factors following early diagnosis of type 2 diabetes: a cohort analysis of a cluster-randomised trial. Br J Gen Pract. 2014;64:e208–e216. doi: 10.3399/bjgp14X677833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kelly LP, Garza PS, Bruce BB, Graubart EB, Newman NJ, Biousse V. Teaching Ophthalmoscopy to Medical Students (the TOTeMS Study) Am J of Ophthalmol. 2013;156:1056–1060. doi: 10.1016/j.ajo.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]