Aspiration remains the most common treatment modality for ganglions of the wrist, and there is abundant literature describing short-term clinical outcomes, such as recurrence. Studies investigating longer-term outcomes are, however, scarce and often do not report patient satisfaction. Accordingly, this retrospective, questionnaire-based study evaluated patient satisfaction and long-term recurrence rates following wrist ganglion aspiration in 41 patients.
Keywords: Aspiration, Recurrence, Satisfaction, Treatment, Wrist ganglion
Abstract
BACKGROUND:
There is a strong body of evidence addressing short-term outcomes following wrist ganglion aspiration; however, few studies have investigated long-term outcomes and patient satisfaction.
OBJECTIVE:
To evaluate patient satisfaction and the long-term rate of recurrence following wrist ganglion aspiration.
METHODS:
Charts of all patients with a wrist ganglion treated by a single surgeon from 2001 to 2011 were reviewed. Demographic and clinical data were retrieved from patient charts. Patients were contacted by telephone and asked to complete a questionnaire addressing recurrence, satisfaction and symptom improvement. Improvement was assessed using a Likert scale, with 1 indicating ‘significantly worse’ and 5 indicating ‘significantly improved’. Statistical analysis was performed using Pearson χ2, Mann-Whitney-Wilcoxon and Fisher’s exact tests.
RESULTS:
Forty-one consecutive patients were identified using hospital records; 21 (51%) consented to the telephone questionnaire. There were no differences in demographic or clinical data between patients who completed the telephone questionnaire and those who did not. The mean age at treatment was 45.3 years, mean time to follow-up was 6.3 years and 52.4% of ganglions recurred. Overall, 95% (20 of 21) of patients were satisfied with their treatment and would proceed again given the option; satisfaction was independent of recurrence. Following treatment, there was improvement in pain, function, range of motion and appearance; improvement in symptoms was independent of recurrence.
CONCLUSIONS:
Long-term recurrence of ganglions treated with aspiration appeared to be similar to the short-term rates reported in the literature. Independent of recurrence, patients remained satisfied with aspiration and reported improvement in symptoms.
Abstract
HISTORIQUE :
Les résultats à court terme de l’aspiration de ganglions sont bien étayés, mais peu d’études traitent des résultats à long terme et de la satisfaction des patients.
OBJECTIF :
Évaluer la satisfaction des patients et le taux de récurrence à long terme après l’aspiration de ganglions du poignet.
MÉTHODOLOGIE :
Les chercheurs ont examiné le dossier de tous les patients qui avaient un ganglion du poignet et avaient été traités par un même chirurgien entre 2001 et 2011. Ils ont extrait les données démographiques et cliniques de leur dossier. Ils les ont appelés et leur ont demandé de répondre à un questionnaire sur la récurrence, la satisfaction et la diminution des symptômes. Ils ont évalué cette diminution d’après l’échelle de Likert, 1 signifiant « bien pire » et 5 « bien mieux ». Ils ont procédé à l’analyse statistique à l’aide du test du chi carré de Pearson, du test de Mann-Whitney-Wilcoxon et de la méthode exacte de Fisher.
RÉSULTATS :
Les chercheurs ont repéré 41 patients consécutifs dans les dossiers hospitaliers, dont 21 (51 %) ont consenti au questionnaire téléphonique. Ils n’ont relevé aucune différence démographique ou clinique entre les patients qui avaient rempli le questionnaire téléphonique et ceux qui ne l’avaient pas rempli. Les patients avaient un âge moyen de 45,3 ans au traitement, ont été suivis en moyenne 6,3 ans, et 52,4 % des ganglions ont récidivé. Dans l’ensemble, 95 % des patients (20 sur 21) étaient satisfaits de leur traitement et se seraient fait réopérer si on le leur avait proposé. Leur satisfaction était indépendante des récurrences. Après le traitement, la douleur diminuait et la fonction, l’amplitude de mouvements et l’apparence s’amélioraient. Cette diminution des symptômes était indépendante des récurrences.
CONCLUSIONS :
La récurrence à long terme des ganglions traités par aspiration semblait similaire aux taux à court terme publiés. Qu’ils présentent ou non une récurrence, les patients étaient satisfaits de l’aspiration et signalaient une diminution des symptômes.
Ganglions are the most common benign soft tissue tumours of the hand and wrist (1). The indications for treatment include pain, stiffness, weakness and cosmetic concern. There are many potential treatment modalities but aspiration is the most common. Although there is a large body of evidence addressing short-term outcomes following aspiration, few studies have reported long-term outcomes and even fewer have reported patient satisfaction following treatment. The objective of the present study was to evaluate patient satisfaction and the long-term rate of recurrence following wrist ganglion aspiration.
METHODS
Following Ottawa Health Science Network Research Ethics Board (Ottawa, Ontario) approval, a retrospective study was initiated. Charts of all patients with a single dorsal or volar wrist ganglion treated between 2001 and 2011 were reviewed; patients with multiple ganglions were excluded. A single surgeon treated all patients. When patients desired intervention for their symptomatic ganglion, the surgeon’s practice was to treat with aspiration and not surgical excision. Ganglions were aspirated using an 18-gauge needle, and the surgeon facilitated aspiration by massaging the ganglion fluid toward the aspirating needle with a finger.
Demographic (date of birth, treatment date, sex) and clinical data (ganglion location, size, treatment, reason for seeking treatment) were retrieved from electronic patient records. Patients were contacted by telephone and asked to complete a questionnaire addressing recurrence, satisfaction and symptomatic improvement (pain, function, range of motion, appearance). Symptomatic improvement was assessed using a Likert scale from 1 to 5, with 1 indicating ‘significantly worse’ and 5 indicating ‘significantly improved’. Statistical analysis was performed using Pearson χ2, Mann-Whitney-Wilcoxon and Fisher’s exact tests.
RESULTS
A total of 41 consecutive patients, all treated with aspiration, were identified using hospital records. Of the 41 patients, 21 (51%) consented to the telephone questionnaire, 17 could not be reached due to inadequate hospital records or change in address, one was deceased and two did not consent (Figure 1). Demographic and clinical data from the 41 patients are shown in Table 1. There were no differences in demographic or clinical data between patients who completed the telephone questionnaire and those who did not.
Figure 1).
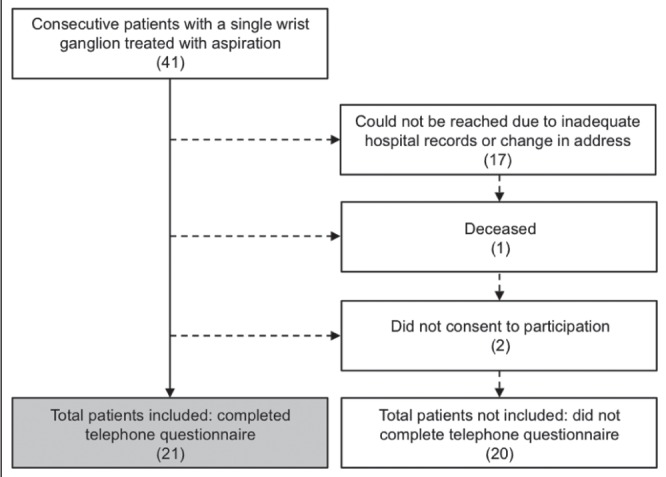
Flow diagram describing the inclusion of patients in the present study
TABLE 1.
Demographics and presenting symptoms of the study population
| Included (n=21) | Not included (n=20) | P | Total (n=41) | |
|---|---|---|---|---|
| Age at treatment, years | 45.3±4.0 | 42.4±3.7 | 0.602† | 43.9 (2.6) |
| Sex | ||||
| Female | 15 (71.4) | 13 (65.0) | 0.658* | 28 (68.3) |
| Male | 6 (28.6) | 7 (35.0) | 13 (31.7) | |
| Wrist ganglion location | ||||
| Dorsal | 13 (61.9) | 13 (65.0) | 0.837* | 26 (63.4) |
| Volar | 8 (38.1) | 7 (35.0) | 15 (36.6) | |
| Size, mL | 1.4±0.2 | 1.5±0.2 | 0.588† | 1.47 (0.1) |
| Reason for seeking treatment | ||||
| Pain | 14 (66.7) | 12 (60.0) | 0.658* | 26 (63.4) |
| Size change | 8 (38.1) | 8 (40.0) | 0.901* | 16 (39.0) |
| Cosmetic | 5 (23.8) | 6 (30.0) | 0.655* | 11 (26.8) |
| Numbness | 1 (4.8) | 3 (15.0) | 0.269* | 4 (9.8) |
| Reduced ROM | 2 (9.5) | 1 (5.0) | 0.578* | 3 (7.3) |
Data presented as mean ± standard error or n (%) unless otherwise indicated.
Pearson χ2;
Mann-Whitney-Wilcoxon. ROM Range of motion
Among the 21 patients who completed the telephone questionnaire, the mean (± SE) time to follow-up was 6.3±0.4 years. The rate of recurrence following aspiration was 52.4% (11 of 21) and no patients experienced complications. Five patients who experienced recurrence after the first aspiration progressed to undergo further aspirations, three of whom experienced complete resolution. One patient undewent multiple aspirations with continued recurrence and sought treatment with surgical excision from a different surgeon; the ganglion did not recur following excision. Overall, 95% (20 of 21) of patients were satisfied with their treatment and would proceed again given the option; satisfaction was independent of recurrence (P=0.524 [Fisher’s exact test]).
Among all patients who completed the questionnaire, there was improvement in mean pain scores (4.1±0.2 of 5.0), function (3.9±0.2 of 5.0), range of motion (3.8±0.2 of 5.0) and appearance (4.1±0.2 of 5.0); improvement in symptoms was independent of recurrence (P=0.364, P=0.685, P=0.469 and P=0.357, respectively [Mann-Whitney-Wilcoxon]).
DISCUSSION
Treatment of wrist ganglions has been reported for centuries (2). Reported outcomes typically focus on short-term clinical outcomes, such as recurrence, to define the success of interventions and most studies do not report patient satisfaction. Importantly, although a ganglion may recur following treatment, it may still be regarded a success if the patient is satisfied. Alternatively, a patient may not be satisfied – even in the context of a ganglion not recurring – if a procedure is overly invasive or produces unnecessary morbidity. The purpose of the present study was to report long-term recurrence rates for a series of patients undergoing ganglion aspiration and to collect patient perspectives on the success of the treatment.
The mean follow-up period of 6.3 years reported in the present study is relatively long compared with most other studies reporting recurrence data following aspiration of wrist ganglions (3–14). Despite the long follow-up period, the recurrence rate in the present series (52.4%) is consistent with other reported recurrence rates of shorter duration (15). Gude and Morelli (15) found an average recurrence rate for aspiration alone of 51% and recurrence with aspiration and corticosteroid injection of 52%. Two of the longest follow-ups were published by Dias et al (13), and Dias and Buch (8), who reported two cohorts of aspirated ganglions with 5.9 and 5.3 years of follow-up; the two groups had recurrence rates of 58% and 47%, respectively. In the same studies, the rates of persistence when patients were treated only with reassurance were also 58% and 47%, respectively. It appears that the rate of ganglion recurrence is relatively consistent regardless of the follow-up time period and aspiration may provide no greater recurrence benefit than no treatment.
The potential complications associated with interventions for wrist ganglion include wound infection, scar tenderness, neuroma, hypertrophic scar, neurapraxia and radial artery damage (8). All of these complications are more likely in surgical interventions but are also risks in aspiration, with infection being the most common. None of the patients in the present series experienced complications secondary to intervention. This finding reflects the relatively low rate of complications reported for wrist ganglion aspiration in the literature. Reported complication rates for aspiration range from 0% to 5% (5,8,13) and must be clearly explained to patients before intervention.
Recurrence and the absence of complications are not comprehensive measures of treatment success. Interestingly, the present study showed that independent of recurrence, patients remain satisfied with aspiration and report improvement in symptoms. Although more than one-half of the patients experienced a recurrence, all but one were satisfied with their aspiration treatment and would move forward with the treatment again if given the option.
Although not as commonly cited as recurrence, other investigators have reported on patient satisfaction. Lidder et al (16) reported a series involving 117 patients undergoing surgical excision of a wrist ganglion. Overall, 26% (31 patients) were not satisfied, with the vast majority of these patients belonging to the recurrent group (25 of 31). Of these 31 patients, 22 reported that they would not proceed with the surgery if given the choice again. Satisfaction with surgical excision more commonly exceeds 90%, with most patients remaining satisfied even if the ganglion recurs (17–19); comparable satisfaction rates have been reported in arthroscopic excisions (20,21). Importantly, Dias et al (13) found that both aspiration and surgical excision had similar rates of satisfaction (81% and 83%, respectively) but that there were differing levels of satisfaction among patients who underwent an intervention compared with those who did not. In contrast to the findings reported in the present study, Dias et al (13) also found that recurrence after any intervention was associated with greater patient dissatisfaction.
The present study had some limitations. First, the response rate was only 51%, primarily as a result of incomplete patient records and changed addresses. Nevertheless, patients who completed the telephone questionnaire were not significantly different from those who did not with regard to any recorded demographic or clinical dimension. Second, the measure of recurrence relied on a telephone questionnaire and was, thus, self-reported. However, the nature of a ganglion cyst is that it is easily palpable and the presence or absence is binary, therefore making self-reporting a relatively accurate measure. Third, the present study was a small case series; further prospective randomized trials are needed to determine the long-term recurrence and differences in satisfaction between treatment groups.
Long-term resolution of wrist ganglions following aspiration appears to be comparable with both short-term resolution rates and with spontaneous resolution without treatment. If recurrence were the only metric for success, aspiration would be of questionable benefit. However, independent of recurrence, aspiration appears to yield high satisfaction among patients. Given its low resource demands, low complication rate, high patient satisfaction and potential to avoid more invasive treatment (eg, surgical excision), aspiration should continue to be considered a first-line treatment option for the treatment of wrist ganglions.
Footnotes
DISCLOSURES: The authors have no financial disclosures or conflicts of interest to declare.
REFERENCES
- 1.Angelides A, Wallace P. The dorsal ganglia of the wrist: Its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg Am. 1976;1:228–35. doi: 10.1016/s0363-5023(76)80042-1. [DOI] [PubMed] [Google Scholar]
- 2.Clay NR, Clement DA. The treatment of dorsal wrist ganglia by radical excision. J Hand Surg Br Eur Vol. 1988;13:187–91. doi: 10.1016/0266-7681_88_90135-0. [DOI] [PubMed] [Google Scholar]
- 3.Breidahl WH, Adler RS. Ultrasound-guided injection of ganglia with corticosteroids. Skeletal Radiol. 1996;25:635–8. doi: 10.1007/s002560050150. [DOI] [PubMed] [Google Scholar]
- 4.Limpaphayom N, Wilairatana V. Randomized controlled trial between surgery and aspiration combined with methylprednisolone acetate injection plus wrist immobilization in the treatment of dorsal carpal ganglion. J Med Assoc Thail. 2004;87:1513–7. [PubMed] [Google Scholar]
- 5.Khan PS, Hayat H. Surgical excision versus aspiration combined with intralesional triamcinolone acetonide injection plus wrist immobilization therapy in the treatment of dorsal wrist ganglion; a randomized controlled trial. J Hand Microsurg. 2011;3:55–7. doi: 10.1007/s12593-011-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Korkmaz M, Ozturk H, Senarslan DA, Erdogan Y. Aspiration and methylprednisolone injection to the cavity with IV cannula needle in the treatment of volar wrist ganglia: New technique. Pakistan J Med Sci. 2013;29:5–8. doi: 10.12669/pjms.291.2655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wright TW, Cooney WP, Ilstrup DM. Anterior wrist ganglion. J Hand Surg Am. 1994;19:954–8. doi: 10.1016/0363-5023(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 8.Dias J, Buch K. Palmar wrist ganglion: Does intervention improve outcome? A prospective study of the natural history and patient-reported treatment outcomes. J Hand Surg Br Eur Ed. 2003;28:172–6. doi: 10.1016/s0266-7681(02)00365-0. [DOI] [PubMed] [Google Scholar]
- 9.Nasab SAM, Mashhadizadeh E, Sarrafan N. Comparative study between three methods of aspiration alone, aspiration plus steroid injection and aspiration plus ethanol injection for treatment of dorsal wrist ganglions. Pakistan J Med Sci. 2012;28:404–7. [Google Scholar]
- 10.Rollins K, Ollivere B, Johnston P. Predicting successful outcomes of wrist and finger ganglia. Hand Surg. 2013;18:41–4. doi: 10.1142/S021881041350007X. [DOI] [PubMed] [Google Scholar]
- 11.Stephen AB, Lyons AR, Davis TR. A prospective study of two conservative treatments for ganglia of the wrist. J Hand Surg Br Eur. 1999;24B:104–5. doi: 10.1016/s0266-7681(99)90051-7. [DOI] [PubMed] [Google Scholar]
- 12.Muddu B, Morris M, Fahmy N. The treatment of ganglia. J Bone Joint Surg. 1990;72:147. doi: 10.1302/0301-620X.72B1.2298778. [DOI] [PubMed] [Google Scholar]
- 13.Dias JJ, Dhukaram V, Kumar P. The natural history of untreated dorsal wrist ganglia and patient reported outcome 6 years after intervention. J Hand Surg Eur Vol. 2007;32:502–8. doi: 10.1016/J.JHSE.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 14.Varley G, Needoff M, Davis T, Clay R. Conservative management of wrist ganglia. J Hand Surg Br Eur. 1997;22B:636–7. doi: 10.1016/s0266-7681(97)80363-4. [DOI] [PubMed] [Google Scholar]
- 15.Gude W, Morelli V. Ganglion cysts of the wrist: Pathophysiology, clinical picture, and management. Curr Rev Musculoskelet Med. 2008;1:205–11. doi: 10.1007/s12178-008-9033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lidder S, Ranawat V, Ahrens P. Surgical excision of wrist ganglia; literature review and nine-year retrospective study of recurrence and patient satisfaction. Orthop Rev (Pavia) 2009;1:e5. doi: 10.4081/or.2009.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singhal R, Angmo N, Gupta S, Kumar V, Mehtani A. Ganglion cysts of the wrist: A prospective study of a simple outpatient management. Acta Orthop Belg. 2005;71:528–34. [PubMed] [Google Scholar]
- 18.Faithfull DK, Seeto BG. The simple wrist ganglion-more than a minor surgical procedure? Hand Surg. 2000;5:139–43. doi: 10.1142/s0218810400000235. [DOI] [PubMed] [Google Scholar]
- 19.Craik JD, Walsh SP. Patient outcomes following wrist ganglion excision surgery. J Hand Surg Eur Vol. 2012;37:673–7. doi: 10.1177/1753193411434376. [DOI] [PubMed] [Google Scholar]
- 20.Aslani H, Najafi A, Zaaferani Z. Prospective outcomes of arthroscopic treatment of dorsal wrist ganglia. Orthopedics. 2012;35:e365–70. doi: 10.3928/01477447-20120222-13. [DOI] [PubMed] [Google Scholar]
- 21.Chen AC-Y, Lee W-C, Hsu K-Y, Chan Y-S, Yuan L-J, Chang C-H. Arthroscopic ganglionectomy through an intrafocal cystic portal for wrist ganglia. Arthroscopy. 2010;26:617–22. doi: 10.1016/j.arthro.2009.08.021. [DOI] [PubMed] [Google Scholar]


