Abstract
BACKGROUND:
Excess sitting is emerging as a novel risk factor for cardiovascular disease, diabetes, mental illness, and all-cause mortality. Physical activity, distinct from sitting, is associated with better sleep and lower risk for OSA, yet relationships among sitting behaviors and sleep/OSA remain unknown. We examined whether total sitting time and sitting while viewing television were associated with sleep duration and quality, OSA risk, and sleepiness.
METHODS:
The 2013 National Sleep Foundation Sleep in America Poll was a cross-sectional study of 1,000 adults aged 23 to 60 years. Total sitting time, time watching television while sitting, sleep duration and quality, OSA risk, and daytime sleepiness were assessed.
RESULTS:
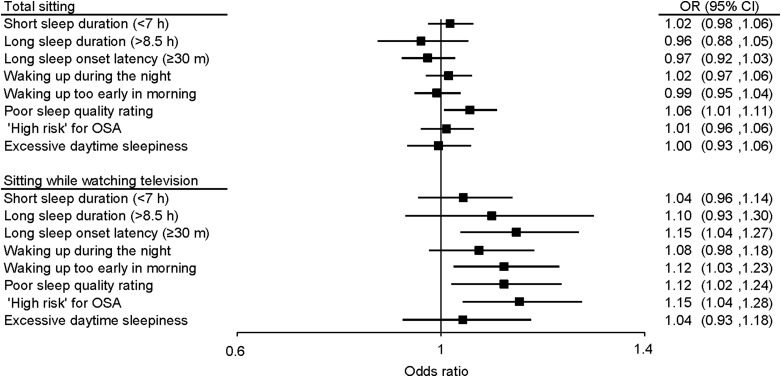
After adjusting for confounding factors (including BMI and physical activity), each additional hour per day of total sitting was associated with greater odds of poor sleep quality (OR [95% CI] = 1.06 [1.01, 1.11]) but not with other sleep metrics (including sleep duration), OSA risk, or daytime sleepiness. For television viewing while sitting, each additional hour per day was associated with greater odds of long sleep onset latency (≥ 30 min) (OR = 1.15 [1.04, 1.27]), waking up too early in the morning (OR = 1.12 [1.03, 1.23]), poor sleep quality (OR = 1.12 [1.02, 1.24]), and “high risk” for OSA (OR = 1.15 [1.04, 1.28]). Based upon an interaction analysis, regular physical activity was protective against OSA risk associated with television viewing (P = .04).
CONCLUSIONS:
Excess sitting was associated with relatively poor sleep quality. Sitting while watching television was associated with relatively poor sleep quality and OSA risk and may be an important risk factor for sleep disturbance and apnea risk.
Sedentary behavior is defined as sitting/reclining with low energy expenditure.1 Sedentary behavior is emerging as a novel risk factor for most chronic diseases, including cardiovascular disease, diabetes, and some cancers.2‐4 The detrimental consequences of sedentary behavior (eg, sitting) are largely independent of the robust benefit physical activity has on these same health outcomes.5 Laboratory (both animal and human) and prospective cohort studies demonstrate that simply spending more time in a sitting posture, compared with standing, correlates with less favorable cardiometabolic risk biomarkers, higher incidence of cardiovascular disease, and higher mortality rates.6‐8 Reducing sitting time is now considered an important preventive health measure.5 The context of sitting behaviors also appears important for health outcomes. Television viewing—the predominant leisure-time sitting behavior9—is consistently more strongly linked to adverse health outcomes than total sitting time.4
Poor sleep quality, short and long sleep duration, and OSA are also considered important determinants of cardiovascular disease, diabetes, and all-cause mortality.10‐15 Improving sleep quality, optimizing sleep duration, and treating OSA have emerged as important public health priorities.16 Pharmacologic and nonpharmacologic treatments for poor sleep and OSA are widely used. Regular physical activity, one such nonpharmacologic approach, improves sleep quality17‐19 and is a relatively simple, inexpensive, and safe alternative to medicine for long-term treatment of poor sleep.20‐22 Physical activity also reduces OSA symptom severity independent of weight loss23 and provides additional benefit when combined with weight loss.24
To our knowledge, no studies in adults have explored the relationship between sitting, sleep disturbance, and/or OSA. Furthermore, the differential influence of total time spent sitting vs context-specific forms of sitting (eg, television viewing) also remain unexplored. If a relationship exists, it is not clear whether this relationship is independent of confounding factors such as weight or physical activity. Therefore, the purpose of this study was to examine the relationship between sitting behaviors (both total sitting and television viewing) and sleep duration, sleep quality, OSA risk, and sleepiness in a large American sample participating in the National Sleep Foundation’s 2013 Sleep in America poll. Furthermore, we explored whether weight and/or physical activity were protective against the negative associations between excess sitting and sleep quality, sleep duration, and OSA risk.
Materials and Methods
Poll Content
The poll content was developed by a task force of independent scientists and clinicians. Members were invited based on their expertise in sleep science/medicine and/or exercise science. Poll items were derived from several sources, including validated questionnaires (used either in part or in their entirety) and items developed specifically for the poll. A complete listing of questions used for the poll can be found at www.sleepfoundation.org/2013poll. The National Sleep Foundation did not solicit or accept any corporate support for this poll.
Procedures
Telephone interviews were conducted by professional interviewing staff of WBA Research using a computer-assisted telephone interviewing system to provide a script prompt and tabulate responses. The telephone sample used random digit dialing of listed and cell phone telephone numbers. The web sample was obtained using an online e-Rewards panel of Americans meeting study requirements. Upon completion, interviews were edited, coded, and keypunched. All surveys were conducted with the respondents. Data were collected from October 19 to November 12, 2012. Institutional review board approval is not required to conduct or publish results of a poll conducted by a nonprofit independent organization when no identifying information is included.
Sample
The sample used was composed of individuals currently living in the United States. Surveys were collected from 1,000 individuals, 23 to 60 years of age. The sample was stratified by age and US geographic region. Sample size for stratification on these factors was derived from 2010 US census data. Maximum sampling error for the entire sample was ± 3.1% (at the 95% confidence level).
Measures
Sitting Behavior:
Total sitting time was assessed with a single item from the International Physical Activity Questionnaire.25 A single-item measure of “sitting while watching television” was also included. Additional context-specific sitting time questions were also asked, including using a computer, reading, socializing with friends/family, traveling in motor vehicle/public transport, doing hobbies, and something else (fill-in) to reduce overreporting in the television viewing item. All sitting time questions were reported in hours and minutes per day and were assessed in reference to the past week.
Sleep Quality and Duration Measures:
Sleep quality metrics were assessed in reference to the past 2 weeks and were selected from a core set of questions used annually in Sleep in America polls. Sleep duration was assessed in hours and minutes “on average worknights or weeknights…not including naps.” For analysis, sleep duration values were collapsed to short sleep duration (< 7 h/night, yes/no) and long sleep duration (> 8.5 h, yes/no). Sleep onset latency was assessed in “minutes, on most worknights or weeknights…to fall asleep” and collapsed to indicate presence of long sleep onset latency (≥ 30 min, yes/no). “Waking up during the night” and “waking up too early in the morning” were modified from the Insomnia Severity Index26 using four-item Likert-type questions with “every night or almost every night,” “a few nights a week,” “rarely,” and “never” response options. Responses of “every night or almost every night” and “a few nights a week” were combined for these items to indicate a sleep complaint. Overall sleep quality was measured with one four-item Likert-type question from the Pittsburgh Sleep Quality Index,27 with “very good,” “fairly good,” “fairly bad,” and “very bad” response options. For analysis, responses were collapsed to good (fairly good/very good) vs poor (fairly bad/very bad) sleep quality.
Risk for OSA:
OSA risk was assessed with a validated four-item questionnaire, which assesses four risk factors for OSA, including snoring, tiredness during daytime, observed apnea, and reported high BP (STOP). This measure has been shown to have acceptable sensitivity (74.3%) and specificity (53.3%) for mild or more severe OSA.28
Daytime Sleepiness:
Daytime sleepiness was assessed with an abbreviated version of the Epworth Sleepiness Scale.29 This scale tabulates self-reported likelihood estimates of falling asleep during eight everyday sedentary activities; for the 2013 Sleep in America poll, all items were used except “sitting, inactive in a public place (eg, in a theater or a meeting)” to avoid collinearity with the sitting time questions. Response options for each activity ranged from 0 (would never doze) to 3 (high chance of dozing), and individual items were summed for a total score. “Excessive daytime sleepiness” was indicated by scores > 10.
Demographic and Study Covariates:
Demographic characteristics of interest included age (continuous), sex, ethnicity (Hispanic/Latino vs not Hispanic/Latino), race (white, black, Asian, biracial, other), work status (full- or part-time vs not working), educational status (bachelor degree or more vs other), marital status (married/partnered vs other), US geographic region (Northeast, Midwest, South, West), and web (n = 500) vs telephone (n = 500) poll administration. BMI was included continuously (in kg/m2 from weight [kg] and height [m]) as a covariate in all models and explored as an effect modifier categorically (BMI ≥ 30 kg/m2 vs < 30 kg/m2). Finally, physical activity status was assessed with a single-item endorsement of physical activities performed for at least 10 min at a time in the past 7 days as either “none,” “light,” “moderate,” or “vigorous.” Individuals endorsing moderate or vigorous activities were considered physically active for these analyses.
Analysis
We calculated descriptive statistics to represent the sample, including means, SDs, frequencies, and percentages. Multiple logistic regression analysis (SAS Enterprise Guide 5.1; SAS Institute Inc) was used to identify predictors of sleep duration, sleep quality, OSA risk, and daytime sleepiness. Interaction analyses tested whether weight or physical activity status modified sitting time associations with sleep, OSA, and daytime sleepiness variables. Sitting time (total and while viewing television) were entered as continuous variables into all models to retain maximal statistical power; thus, OR estimates can be interpreted as additional risk per 1 h/d difference in sitting time. Inferential testing was conducted at a P < .05 significance level.
Results
Demographic Information
Table 1 provides sample demographics for the 2013 Sleep in America poll. In total, 1,000 respondents were surveyed; however, we excluded 157 cases from analyses because of one or more missing covariate, exposure, or outcome variable (N = 843). The sample could be generally characterized as middle-aged, non-Hispanic white, working, college-educated, married/partnered, overweight individuals. Obese individuals (26.0%) reported similar total sitting (6.6 ± 3.7 h/d vs 6.2 ± 3.5 h/d) but more television viewing (2.4 ± 2.0 h/d vs 2.0 ± 1.6 h/d, P = .0007) than normal/overweight individuals. Physically active individuals reported less total sitting (5.9 ± 3.4 h/d vs 6.6 ± 3.7 h/d) and television viewing (1.8 ± 1.4 h/d vs 2.4 ± 1.9 h/d) than physically inactive individuals (P values < .0001).
TABLE 1 ] .
Descriptive Results From the 2013 National Sleep Foundation Sleep in America Poll (N = 843)
| Variables | Measure |
| Demographic variables | |
| Age, mean (SD) | 42.14 (11.08) |
| Female sex | 426 (50.53) |
| Hispanic/Latino ethnicity | 45 (5.34) |
| Race | |
| White | 680 (80.67) |
| Black | 74 (8.77) |
| Asian | 38 (4.51) |
| Other | 51 (6.05) |
| Currently working, full/part time | 660 (78.29) |
| Bachelor’s degree or more | 482 (57.18) |
| Married/partnered | 560 (66.43) |
| BMI, mean (SD) | 27.31 (5.75) |
| Physically active | 376 (44.60) |
| Exposure variables, mean (SD) | |
| Total sitting time, h/d | 6.28 (3.55) |
| Sitting while watching television, h/d | 2.13 (1.73) |
| Outcome variables | |
| Short sleep duration, < 7 h | 333 (39.50) |
| Long sleep duration, > 8.5 h | 44 (5.22) |
| Long sleep onset latency, ≥ 30 min | 176 (20.88) |
| Waking up during the night | 557 (66.07) |
| Waking up too early in morning | 288 (34.37) |
| Poor sleep quality rating | 199 (23.61) |
| High risk for OSA | 219 (25.89) |
| Excessive daytime sleepiness | 125 (14.48) |
Data are presented as No. (%) unless otherwise indicated.
Logistic Regression Analyses: Total Sitting and Television Viewing
Figure 1 summarizes the logistic regression analyses results for total sitting time and sitting while watching television. For total sitting, the only significant association was with poor sleep quality; each additional hour of total sitting was associated with greater odds of poor sleep quality. By contrast, watching television sitting was associated with long sleep onset latency, waking too early in the morning, and poor sleep quality. Television viewing was also associated with greater odds of high risk status for OSA. However, television viewing was not associated with excessive daytime sleepiness.
Figure 1 –
ORs for sleep duration/quality, high risk status for OSA, and excessive sleepiness per a 1-h/d difference in total sitting time and sitting while watching television. Models are adjusted for age, sex, ethnicity, race, work status, educational status, geographic region, web vs telephone administration, BMI, and physical activity status.
Effect Modification of BMI and Physical Activity Status
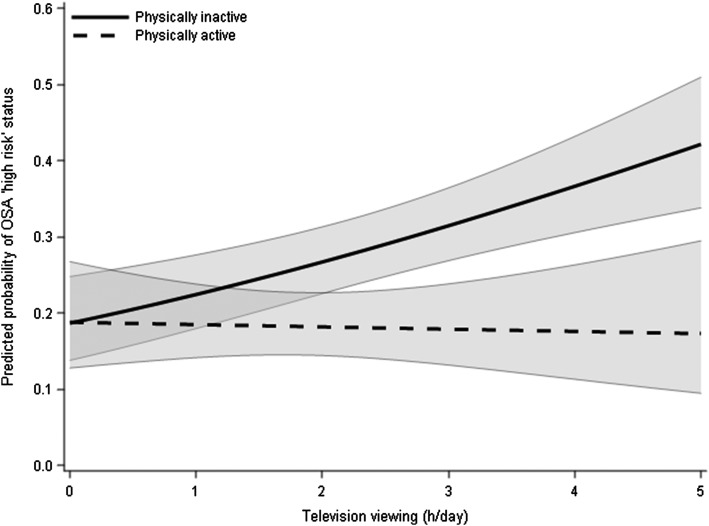
BMI was not a significant effect modifier in any of the logistic regression models. This suggests similar sitting time associations with sleep outcomes among normal/overweight and obese individuals. Physical activity status was a significant effect modifier for the association between television viewing and high risk status for OSA (coefficient [SE] = −0.29 [0.12]; P = .04). The relationship between television viewing and OSA risk was not as strong among physically active individuals as it was among physically inactive individuals (Fig 2).
Figure 2 –
Associations of television viewing while sitting and high-risk status for OSA (defined by 2+ risk factors from the STOP questionnaire) by physical activity status. P for interaction = .04. 95% CIs are displayed in gray. Predicted probabilities set at mean BMI (27.3 ± 5.6 kg/m2).
Discussion
This study’s primary finding was that sitting while watching television was associated with sleep disturbance and increased OSA risk. This relationship was present despite controlling for BMI and physical activity status. By contrast, with the exception of overall sleep quality, self-reported total sitting time did not independently predict sleep duration or quality, OSA risk, or daytime sleepiness. Finally, physically active individuals did not exhibit the same detrimental association between television viewing and OSA risk that was observed for physically inactive individuals. The detrimental association between television viewing and OSA risk was similar among normal/overweight and obese individuals.
Whereas mechanism(s) underlying the association between sitting and OSA remain unknown, this study may provide a clue. Postural changes from sitting to standing (with only slight increases in energy expenditure) can produce improved lipoprotein lipase oxidation,8 postural muscle activation,30 and more efficient lower body fluid dynamics.31 The data presented here suggest that being physically active decreases the linkage between television viewing, poor sleep, and OSA. One could posit that these effects are analogous to the protective benefits of physical activity against other risks (eg, obesity, smoking). Such a hypothesis warrants further investigation.
The consistent detrimental associations of relatively poor sleep and OSA with sitting while watching television, but not with total sitting time, were consistent with other studies showing relatively greater risks of television viewing than total sitting on other health outcomes.4 We do not have a clear explanation for these patterns. One possibility might be greater measurement error associated with estimating total daily sitting time compared with the time spent watching television. Alternatively, one could speculate the sleep disruption and OSA risks associated with television viewing are due to the proximity of television viewing to sleep. This assumes, of course, that the majority of television viewing occurs in the evening prior to bedtime. An association of simple changes in fluid dynamics with sleep might be more evident following evening sitting. Another potential factor involves television viewing’s additional contribution to light exposure. Blue light exposure in the evening provokes a delay in sleep phase; consequently, electronic devices, such as televisions, prior to bed may suppress melatonin secretion and delay sleep onset.32 Finally, television show content can increase autonomic activation, provoke anxiety,33 and/or disrupt facilitative sleep conditioning.34 Each of these factors may disturb sleep when occurring close to bedtime and could potentially have additive effects that may all be contributing to the findings presented here.
Strengths of the current study include its use of a large multiregional sample. The conclusions are less likely to include incorporation bias, thereby strengthening our conclusions and the robustness of the relationships observed. Second, by including television viewing as a unique exposure, separate from total sitting time, context-specific forms of sitting (ie, television viewing) could be examined. Finally, information concerning body mass and physical activity status allowed us to limit confounding effects. Physical activity level acted as an intermediate variable modifying the relationships we found. The ability to covary such variables strengthens our findings concerning sitting time as a novel and independent risk factor. It is possible, however, that additional confounding effects exist.
This study also includes a number of limitations. First, the cross-sectional nature of this study limits causal inferences. It is not clear whether excess sitting and television viewing occurred before, after, or during the onset of relatively poor sleep and OSA risk. However, if the opposite causal direction were true, given the effect sedentary behavior has on a host of health outcomes, it would suggest an additional mechanism by which poor sleep and OSA risk may lead to poor health.
A second limitation in this poll was the administration of self-reported measures of both sitting and sleep. Objective measures of posture (ie, inclinometers) and movement (ie, accelerometers) are available and are regularly used to identify sedentary behaviors; however, it was not feasible to deploy these sensors given our large sample, nor could these sensors provide the contextual nature of sitting behaviors (eg, television viewing) that a self-report measure can provide. Although reported sitting time estimates in this study were more similar to other population-based studies using accelerometers35 and diaries9 to estimate total sitting and television viewing than previous population-based self-report studies,36 recall-based measures of sitting behaviors are likely prone to error.
Finally, we did not query the specific timing of sitting behaviors relative to bedtime. Sitting time increases throughout the day,37 and it is possible that excess sitting close to bedtime may have more harmful effects on sleep. Future studies should examine the association of timing of sitting with sleep. Being physically active rather than sitting near bedtime might be associated with reduction in some risks. A recent study from the 2013 Sleep in America poll found that physical activity completed within 4 h of bed was not harmful, and may be beneficial, for sleep.38 It is not clear whether a beneficial effect of exercise in the evening would be due to increased physical activity, a reduction in time spent sitting, or some combination.
Overall, this investigation represents a first step in understanding the relationship between sitting and sleep and can serve to generate hypotheses for future research. Sitting time and television viewing appear to be novel and important risk factors for sleep quality and OSA risk. To further elucidate this relationship, future research can objectively assess time sitting and specific sleep parameters. Prospective investigations measuring sitting behavior, timing, and temporal sequence relative to bedtime remain important directions to advance our understanding.
Acknowledgments
Author contributions: All authors are accountable for the accuracy and integrity of the manuscript. M. P. B. was responsible for study conception, data analysis, and drafting the manuscript. M. P. B. and C. E. K. contributed to interpretation of the data; and M. P. B., C. E. K., S. D. Y., B. P., M. T. d. M., and M. H. contributed to the development of the primary survey, study design, critically revising the manuscript for important intellectual content, and providing final approval of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The National Sleep Foundation created general reports and summaries of the findings and contributed to survey development. The National Institutes of Health had no role in this manuscript beyond funding.
Footnotes
This work was presented at the International Congress on Physical Activity and Public Health, April 10, 2014, Rio de Janeiro, Brazil.
FUNDING/SUPPORT: This study was funded by the National Sleep Foundation and by the National Institutes of Health [Grants K23HL118318 to Dr Kline and R01HL095799 to Dr Youngstedt].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35(6):725-740. [DOI] [PubMed] [Google Scholar]
- 2.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41(5):998-1005. [DOI] [PubMed] [Google Scholar]
- 3.Warren TY, Barry V, Hooker SP, Sui X, Church TS, Blair SN. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42(5):879-885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thorp AA, Owen N, Neuhaus M, Dunstan DW. Sedentary behaviors and subsequent health outcomes in adults a systematic review of longitudinal studies, 1996-2011. Am J Prev Med. 2011;41(2):207-215. [DOI] [PubMed] [Google Scholar]
- 5.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010;38(3):105-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katzmarzyk PT. Standing and mortality in a prospective cohort of Canadian adults. Med Sci Sports Exerc. 2014;46(5):940-946. [DOI] [PubMed] [Google Scholar]
- 7.Dunstan DW, Kingwell BA, Larsen R, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):976-983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551(pt 2):673-682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Labor, Bureau of Labor Statistics. American Time Use Survey - 2012 Results. Washington, DC: US Department of Labor; 2012 [Google Scholar]
- 10.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration as a risk factor for diabetes incidence in a large US sample. Sleep. 2007;30(12):1667-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165(8):863-867. [DOI] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Redline S, Nieto FJ, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009-1014. [DOI] [PubMed] [Google Scholar]
- 13.Campos-Rodriguez F, Martinez-Garcia MA, de la Cruz-Moron I, Almeida-Gonzalez C, Catalan-Serra P, Montserrat JM. Cardiovascular mortality in women with obstructive sleep apnea with or without continuous positive airway pressure treatment: a cohort study. Ann Intern Med. 2012;156(2):115-122. [DOI] [PubMed] [Google Scholar]
- 14.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perry GS, Patil SP, Presley-Cantrell LR. Raising awareness of sleep as a healthy behavior. Prev Chronic Dis. 2013;10:E133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King AC, Pruitt LA, Woo S, et al. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J Gerontol A Biol Sci Med Sci. 2008;63(9):997-1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buman MP, King AC. Exercise as a treatment to enhance sleep. Am J Lifestyle Med. 2010;4(6):500-514. [Google Scholar]
- 19.Youngstedt SD, O’Connor PJ, Dishman RK. The effects of acute exercise on sleep: a quantitative synthesis. Sleep. 1997;20(3):203-214. [DOI] [PubMed] [Google Scholar]
- 20.Mallon L, Broman J-E, Hetta J. Is usage of hypnotics associated with mortality? Sleep Med. 2009;10(3):279-286. [DOI] [PubMed] [Google Scholar]
- 21.Kripke DF, Langer RD, Kline LE. Hypnotics’ association with mortality or cancer: a matched cohort study. BMJ Open. 2012;2(1):e000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Youngstedt SD. Effects of exercise on sleep. Clin Sports Med. 2005;24(2):355-365. [DOI] [PubMed] [Google Scholar]
- 23.Kline CE, Crowley EP, Ewing GB, et al. The effect of exercise training on obstructive sleep apnea and sleep quality: a randomized controlled trial. Sleep. 2011;34(12):1631-1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iftikhar IH, Kline CE, Youngstedt SD. Effects of exercise training on sleep apnea: a meta-analysis. Lung. 2014;192(1):175-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hagströmer M, Oja P, Sjöström M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9(6):755-762. [DOI] [PubMed] [Google Scholar]
- 26.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. [DOI] [PubMed] [Google Scholar]
- 28.Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108(5):812-821. [DOI] [PubMed] [Google Scholar]
- 29.Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15(4):376-381. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton MT, Healy GN, Dunstan DW, Zderic TW, Owen N. Too little exercise and too much sitting: inactivity physiology and the need for new recommendations on sedentary behavior. Curr Cardiovasc Risk Rep. 2008;2(4):292-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mirrakhimov AE. Physical exercise related improvement in obstructive sleep apnea. Look for the rostral fluid shift. Med Hypotheses. 2013;80(2):125-128. [DOI] [PubMed] [Google Scholar]
- 32.Bues M, Pross A, Stefani O, et al. LED-backlit computer screens influence our biological clock and keep us more awake. J Soc Inf Disp. 2012;20(5):266-272. [Google Scholar]
- 33.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14(1):9-15. [DOI] [PubMed] [Google Scholar]
- 34.Bootzin RR, Epstein DR. Understanding and treating insomnia. Annu Rev Clin Psychol. 2011;7:435-458. [DOI] [PubMed] [Google Scholar]
- 35.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol. 2008;167(7):875-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bauman A, Ainsworth BE, Sallis JF, et al. ; IPS Group. The descriptive epidemiology of sitting. A 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41(2):228-235. [DOI] [PubMed] [Google Scholar]
- 37.Reid N, Eakin E, Henwood T, et al. Objectively measured activity patterns among adults in residential aged care. Int J Environ Res Public Health. 2013;10(12):6783-6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buman MP, Phillips BA, Youngstedt SD, Kline CE, Hirshkowitz M. Does nighttime exercise really disturb sleep? Results from the 2013 National Sleep Foundation Sleep in America Poll. Sleep Med. 2014;15(7):755-761. [DOI] [PubMed] [Google Scholar]