Abstract
Tritrichomonas foetus is a very intriguing trichomonad protozoan with respect to its varied choice of residence in the different host species. It is an obligate parasite of the reproductive and the gastrointestinal tract of bovine and feline host respectively, leading to trichomonosis. Bovine trichomonosis is a sexually transmitted disease whereas feline trichomonosis is a disease with a purported fecal-oral route of spread. Further, the trichomonad is a commensal in the nasal passages, stomach, cecum and colon of swine host. Advances have been exponential in understanding the trichomonad biology and specifically feline trichomonosis since late 1990s and early 2000s when T. foetus was soundly determined to be a causative agent of chronic diarrhea in the domestic cat. It is a challenging task, even for a skilled investigator not to mention the busy clinical veterinarian, to keep up with the vast volume of information. Here we comprehensively reviewed the trichomonad biology, clinical manifestations, pathogenesis, host immunity, world map of distribution, risk factors, diagnosis and treatment. Risk factors associated with T. foetus-positive status in the domestic cat include young age, purebred, history of diarrhea, co-infections with other enteral pathogens. In addition, molecular similarity of bovine and feline isolates of T. foetus in DNA sequence was concisely discussed. The data presented serve as an information source for veterinarians, and investigators who are interested in biology of T. foetus and feline trichomonosis.
Table of contents
Introduction
Molecular studies
Survival of trophozoites in the environment and possible transmission route
Clinical signs associated with gastrointestinal tract infection
Infection in the urogenital tract
Pathogenesis
Host immunity
- Epidemiology
-
8.1.Geographic distribution
-
8.2.Risk factors
-
8.2.1.Age
-
8.2.2.Breed
-
8.2.3.History of diarrhea
-
8.2.4.Co-infection with other enteric protozoa
-
8.2.5.Others
-
8.2.1.
-
8.1.
Diagnosis
Treatment
Conclusions
List of abbreviations
Competing interests
Authors’ contributions
Authors’ information
Acknowledgments
References
1. Introduction
The genus Tritrichomonas belongs to the family Trichomonadidae. Among a few species of veterinary importance in the genus is Tritrichomonas foetus. Tritrichomonas foetus is fascinating both biologically and in its clinical manifestations in addition to being occasionally diagnosed in immunocompromised human beings [1]. It resides in the urogenital tract of cattle and causes bovine trichomonosis, a sexually transmitted disease with no approved treatment, throughout many geographic regions worldwide (bovine isolate) [2]. The same trichomonad species was soundly confirmed in 2003 to be the causative agent of chronic diarrhea in the domestic cat (feline isolate) [3,4] although the discovery of protozoan in these animals was made decades ago, as early as in 1928 [5]. Similar to other trichomonads such as human parasite Trichomonas vaginalis, T. foetus has only trophozoite stage although a pseudocyst stage is described [6-9]. Trophozoites reproduce asexually by longitudinal binary fission; no sexual reproduction has been ever discovered. They are pear- or spindle-shaped with three anterior flagella and one posterior flagellum. An undulating membrane extends along the whole length of the body and emerges as the posterior flagellum. The axostyle extends to the length of the cell and usually projects posteriorly. The size approximates 10-25 μm in length and 3-15 μm in width (Figure 1).
Figure 1.
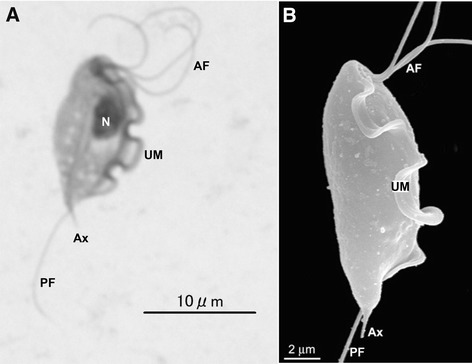
Tritrichomonas foetus trophozoites. A: Giemsa-stain. B: scanning electron microscopy. AF: anterior flagella; Ax: axostyle; N: nucleus; PF: posterior flagellum; UM: undulating membrane. A and B: reproduced from Figure 1 of Doi et al. ([80]) and Figure 1b of Midlej et al. [81], respectively, with permission.
Tritrichomonas foetus has been a topic of review, especially on the clinical aspects of feline trichomonosis [10-15]. The major purpose of the current manuscript is to comprehensively review trichomonad biology, geographic distributions with compiling a world map of distribution, risk factors, host immunity and pathogenesis of the feline isolate. Of course it would not be complete without briefly going over clinical signs, diagnosis, treatment and prognosis of feline trichomonosis.
2. Molecular studies
Feline isolates found in the gastrointestinal (GI) tract of the domestic cat and bovine isolates in the urogenital tract of cattle are morphologically indistinguishable. An identity of 100% has been found within each of both feline and bovine isolates among more than 5000 base pair (bp) at 11 loci by DNA sequencing [16-19]. Nevertheless, there are minor, but consistent differences among these loci, ranging from 0.3% of internal transcribed spacer (ITS) and cysteine protease (CP) 7 and 8 to 1.9% of CP6 gene [16-19] (see Table 1 for details of each locus). Lately, 0.7% difference were found among eight protease inhibitors covering a total of 4674 bp, with individual sequence length ranging from 297 to 1145 bp by a transcriptomical approach. Further, CP8 and CP7 were the most transcribed gene in bovine and feline isolate, respectively [20]. Based on the molecular sequence differences along with disparity of experimental cross-infections and divergence in pathogenicity Walden et al. proposed a new name for the feline isolate. They named it T. blagburni, a new trichomonad species [21]. However, these authors did not show a clear separation of feline from bovine isolate, a requirement for naming a new species. The new nomenclature, if holding up, still waits to be accepted, which may take a while, especially among veterinarians. Nevertheless, comparative transcriptomics revealed near identical functional category distribution of expressed genes with no indication of molecular level divergence, which strongly suggested feline and bovine isolates were taxonomically two isolates of one species [20]. It is not our intension, nor the scope of this manuscript deals with such a debate on taxonomical status of the pathogen causing chronic diarrhea in the domestic cat. Consequently, the name of T. foetus is kept in the current review as well as in the title referring the feline isolate unless otherwise stated in order to be consistent with literature and to avoid confusion among readers.
Table 1.
Genetic similarity in percentage (%) between feline isolates and bovine isolates of Tritrichomonas foetus
| Bovine isolates* | Refs | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Feline isolates # | ITS (2) | ITS-2 (10) | EF-1α (10) | CP8 (2) | CP1 (8) | CP2 (8) | CP4 (8) | CP5 (8) | CP6 (8) | CP7 (8) | CP8 (8) | CP9 (8) | MDH1 (8) | ITS1 + 2 (8) | |
| ITS (4, 327) | 99.7 | [17] | |||||||||||||
| ITS-2 (4, 368) | 99.7 | [16] | |||||||||||||
| EF-1α (4, 783) | 99.4 | [16] | |||||||||||||
| CP8 (4, 663) | 99.7 | [19] | |||||||||||||
| CP1 (7, 503) | 99.4 | [18] | |||||||||||||
| CP2 (7, 669) | 96.7 | [18] | |||||||||||||
| CP4 (7, 273) | 99.3 | [18] | |||||||||||||
| CP5 (7, 361) | 99.2 | [18] | |||||||||||||
| CP6 (7, 318) | 98.1 | [18] | |||||||||||||
| CP7 (7, 373) | 99.7 | [18] | |||||||||||||
| CP8 (7, 907) | 99.4 | [18] | |||||||||||||
| CP9 (7, 289) | 99.3 | [18] | |||||||||||||
| MDH1 (7, 562) | 99.6 | [18] | |||||||||||||
| ITS1 + 2 (7, 297) | 99.7 | [18] | |||||||||||||
CP, cysteine protease; MDH, malate dehydrogenase; ITS, internal transcribed spacer; EL, elongation factor.
*number of cattle isolates.
#first number - number of cat isolates; second number - length of sequence in base pair (bp).
In addition it is worth briefly describing another trichomonad, T. suis. The latter localizes at the nasal passages, stomach, cecum and colon of the domestic pig, and is morphologically indistinguishable from T. foetus. No differences have been found between T. suis and T. foetus bovine isolates at the molecular level such as random amplified polymorphic DNA (RAPD) [22-24], restriction fragment length polymorphism (RFLP) [24], and ITS-1 - 5.8S-rRNA - ITS-2 sequences [25,26]. Consequently they have been suggested synonyms, i.e. the same species [24,27]. Further sequence analysis of more than 5000 bp at 11 loci reveals 100% identity in all loci except elongation factor (EL)-1α and CP8 with 99.4% and 99.7%, respectively (Table 2). Together these molecular data confirm that T. suis and T. foetus bovine isolate are the same species, which makes T. foetus even more fascinating.
Table 2.
Genetic similarity in percentage (%) between Tritrichomonas suis and bovine isolates of T. foetus
| Bovine isolates of T. foetus * | Refs. | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T. suis # | ITS-2 (10) | EF-1α (10) | CP8 (2) | CP1 (8) | CP2 (8) | CP4 (8) | CP5 (8) | CP6 (8) | CP7 (8) | CP8 (8) | CP9 (8) | MDH1 (8) | ITS1 + 2 (8) | |
| ITS-2 (4, 368) | 100.0 | [16] | ||||||||||||
| EF-1α (4, 783) | 99.4 | [16] | ||||||||||||
| CP8 (4, 663) | 99.7 | [19] | ||||||||||||
| CP1 (4, 503) | 100.0 | [18] | ||||||||||||
| CP2 (4, 669) | 100.0 | [18] | ||||||||||||
| CP4 (4, 273) | 100.0 | [18] | ||||||||||||
| CP5 (4, 361) | 100.0 | [18] | ||||||||||||
| CP6 (4, 318) | 100.0 | [18] | ||||||||||||
| CP7 (4, 373) | 100.0 | [18] | ||||||||||||
| CP8 (4, 907) | 100.0 (3); 99.9 (1) | [18] | ||||||||||||
| CP9 (4, 289) | 100.0 | [18] | ||||||||||||
| MDH1 (4, 562) | 100.0 | [18] | ||||||||||||
| ITS1 + 2 (4, 297) | 100.0 | [18] | ||||||||||||
CP, cysteine protease; MDH, malate dehydrogenase; ITS, internal transcribed spacer.
*number of cattle isolates.
#first number - number of cat isolates; second number - length of sequence in base pair (bp).
3. Survival of trophozoites in the environment and possible transmission route
Tritrichomonas foetus like many other trichomonad protozoa has only trophozoites stage. Under the experimental conditions four pathogen-free and four Cryptosporidium sp. infected cats were inoculated via orogastric intubation with 2 × 106 axenic T. foetus. All cats were persistently carrying the protozoan for the entire study period of over 200 days and experienced diarrhea that was self-resolved in seven weeks [28]. It is plausible that trophozoites are transmitted by a fecal-oral route from an infected cat to an uninfected one. By doing so trophozoites have to overcome challenges they face and survive in: 1) the environment they encounter during the period between being discharged from one host and being ingested by the next; and 2) the hostile gastric niche of the new host after ingestion and before moving down to the intestine. A few studies have been done on these areas.
In an experiment that normally formed cat feces that were first mixed with saline in a 1:1 ratio, resulting in no form, loose, puddles or piles, were spiked with 10-fold serially diluted trophozoites (2 × 102 – 2 × 105/gram feces) and stored at room temperature (23-25 °C) for various length periods of time. An accumulative rate of more than 80% of positive culture for feces stored for 6 and 24 h was obtained in both InPouch™ and in Modified Diamond’s Medium (MDM) [29]. It would be more relevant to find out how long the organisms would survive in diarrheic feces, which is currently unavailable. In another experiment cat food was spiked, the pathogens were cultivable for five consecutive days when MDM was used [30]. Similarly T. foetus trophozoites survived more than 3 h in feline urine and sauced cat food, 2 h on ground cat food although only half an hour in tap or distilled water [31]. These data collectively suggest that transmission is not solely limited to close contact between cats. Contamination of food and water by the trichomonads, although less likely in the latter, may be an important route for transmission. Further, garden slugs common in Sydney, Australia were fed cat foods spiked with 106 T. foetus feline isolate trophozoites per gram. One hundred percent and 83% of the Leopard slugs and the Yellow cellar slugs shed viable T. foetus in their feces, respectively, which was cultivable in MDM. Therefore slugs may facilitate the transmission of T. foetus among cats [30] as a vector. It is also plausible that these slugs may serve as transport hosts upon accidental ingestion by cats, which needs to be confirmed.
4. Clinical signs associated with gastrointestinal tract infection
Gastrointestinal disease has been demonstrated in cats experimentally infected with T. foetus, an organism not considered part of the normal feline microbiome [3,28,32]. It is possible to isolate T. foetus from a healthy cat as subclinical shedding does occur [33]. Infection can be demonstrated as early as 2 to 7 days after orogastric inoculation [28]. In experimental infection, T. foetus is limited to the ileum, cecum and colon [28]. Clinical signs vary from subclinical to intractable large bowel diarrhea [3]. Typical clinical signs in natural infections are chronic or intermittent large bowel diarrhea reported in about 61% to 64% of infected cats, with many cats having no reported diarrhea in the 6 months preceding diagnosis [34,35]. The feces has been described as yellow-green in color and malodorous with typical signs of colitis including fresh blood, mucous, fecal incontinence, tenesmus and flatulence [3,36]. The consistency of the feces has been described most commonly as semi-formed to cow pat [28]. An objective fecal scoring system has been used in studies: a scale of 1 to 5 based on consistency, with a score of 1 representing watery feces and a score of 5 is dry and firm feces. Trichomonad infected cats fecal score have been described to range from 3 to 5 [33]. Up to as many as 20% of infected cats have reported systemic signs including anorexia, depression, vomiting and weight loss with a case report describing a kitten as pyrexic and experimental infections reporting vomiting and fever [34,36,37]. In a study examining experimental infection (n = 8), only two cats demonstrated clinical signs of disease, fecal blood and mucous at nine days post-infection (dpi), and fever with vomiting 21 dpi [32]. Interestingly, motile trichomonads were observed in intestinal content culture in only three of the eight cats infected, none of which showed clinical signs. Mortality is extremely rare and only reported in kittens. The first report of mortality was in the study that first described natural and experimental trichomonosis in kittens in 1928 with a feline isolate [5]. All nine kittens diagnosed with naturally acquired infection, and five of the six experimentally infected kittens, wasted and died within five to ten days and four to nine days of diagnosis respectively [5]. The second report that documents mortality was a prevalence study examining T. foetus infection in cats with diarrhea in a shelter colony in Italy [38]. One 7-month old kitten housed in this shelter with confirmed T. foetus infection succumbed to suspected septic shock despite having started ronidazole therapy two days prior [38].
Clinical signs are reported to persist for 5 to 24 months (median 9 months) from the time of diagnosis [33]. More than half of the cats that go into clinical remission will have PCR evidence of trichomonad infection (asymptomatic carrier), and many of these cats will relapse for a short duration, often with worse diarrhea [33]. Not surprisingly, the number of other cats in the same household will negatively impact the time from diagnosis to resolution of clinical signs [33]. Infection with T. foetus is not unlikely in single-cat households even in cats that have lived in isolation for years, as they can acquire the infection in the early stages of their lives [34]. Trichomonad infections can occur as co-infections, most notably Giardia species and coccidia [3,34,35,39]. More severe diarrhea has been reported in four cats experimentally infected with T. foetus and Cryptosporidium species, despite the latter organism having a tropism for the small intestines [28]. In surveys of naturally acquired trichomonad infections the severity of diarrhea has not reported to be worsened by co-infection with enteric parasites [35].
5. Infection in the urogenital tract
In addition to the GI tract T. foetus is also found in the urogenital tract of the domestic cat at least once. Dahlgren et al. reported the first case of T. foetus in the uterus of a cat with pyometra [40]. In this case wet mounts made directly from the fluid collected from the surgically removed uterus revealed microscopically numerous motile flagellated protozoa. They were 13–17 × 5–7 μm in size with undulating membrane, suggesting T. foetus. Further, PCR detected an expected size band product of 343 bp in length using primers PRF3 and PRF4. The PCR product was sequenced and the sequence was 100% identical to T. foetus feline isolate sequences, which confirmed the identity of the protozoan causing feline pyometra as T. foetus [40]. T. foetus was also found in the feces of three other cats in the same household, one of which had chronic diarrhea [40]. These authors were unable to conclude that the infection was sexually transmitted even though the female mated repeatedly with T. foetus-positive male with chronic diarrhea [40].
In a comprehensive study Gray et al. used parallel samples collected in USA from both the urogenital tract as a result of ovariohysterectomy or castration and feces of purebred cats [41]. Direct microscopy, Immunohistochemical analysis and PCR were used to test each sample for the presence of T. foetus among the two sets of samples. Tritrichomonas foetus infections were detected by PCR in 25% (15/61) cats and 67% catteries (22/33). Nevertheless, T. foetus was never detected in the urogenital tract of any cats, including the 15 T. foetus-positive cats in feces. These authors concluded that no evidence of urogenital tract colonization by T. foetus was detected and that urogenital tract infection with T. foetus very unlikely plays an important role in overall disease transmission [41]. Collectively this data demonstrates that infection of the urogenital tract by T. foetus does occur and may cause pyometra, but it is a rare event especially among the healthy cats presenting to clinics for ovariohysterectomy or castration.
6. Pathogenesis
In the above mentioned experiment, four pathogen-free and four Cryptosporidium sp. infected cats were inoculated with axenic T. foetus. All cats experienced self-resolved diarrhea for weeks. Tritrichomonas foetus was isolated from the ileum, cecum, and colon during necropsy. It was further shown that protozoa and its surface-located antigen were detected on surface epithelia and within superficial detritus of the cecal and colonic mucosa (Figure 2) [28]. Similarly in naturally infected cats the parasites were generally present in close proximity to the mucosal surface and less frequently in the lumen of colonic crypts. Mild-to-moderate lymphoplasmacytic and neutrophilic colitis, crypt epithelial cell hypertrophy, hyperplasia and increased mitotic activity, loss of goblet cells were associated with the presence of trichomonads in colon [42]. Consequently in both experimental and natural infections the predilection sites for T. foetus trophozoites are the epithelial surface and crypts of cecum and colon.
Figure 2.
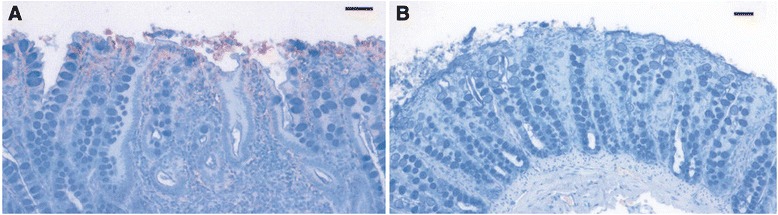
Tritrichomonas foetus antigens in colonic mucosal biopsy specimens. Immunolabeled trichomonads (red stained organisms) in panel A are located on surface enterocytes and within superficial mucus and detritus of the cecal mucosa. Panel B is a negative control omitting primary antibody. Bar = 100 μm. Reproduced with permission [28].
Burgess et al. found that T. foetus bovine isolate was highly cytotoxic to Hela cells, a human cervical cell line, and early bovine lymphosarcoma (BL-3) but displayed low levels of cytotoxicity against Vero cells [43]. The latter are African green monkey kidney cells [43]. This isolate also adheres to bovine vaginal epithelial cells (BVECs) in an in vitro assay. The adhesion process was first initiated by the posterior flagellum followed by the body. IgG1 antibodies inhibited adherence, whereas IgG2 did not [44]. Furthermore, purified lipophosphoglycan (LPG) of T. foetus bovine isolate inhibited the binding of T. foetus to BVECs by competing with the protozoa in specific receptor – ligand interactions [45]. Adhesion of T. foetus resulted in extensive damage of BVEC monolayers [45]. This cytopathic effect was the results of apoptosis induced by T. foetus. A painstaking research pinpointed that CP8 of 30 kDa was the major player in T. foetus inducing BVEC apoptosis [46]. Collectively the data from multiple research groups demonstrate that T. foetus bovine isolate causes cell death of BVECs by means of apoptosis, in which CPs such as CP8 plays a pivotal role. It is not clear whether the same occurs in vivo in infected cows and heifers, which waits to be confirmed.
In an in vitro analysis Tolbert et al. demonstrated that feline T. foetus trophozoites adhere to monolayers of the porcine intestinal epithelial cell line (IPEC)-J2 cells [47] (Figure 3). The reason for using a porcine jejunal cell line was the unavailability of epithelial cell line of feline origin. It is worthy of noting that T. suis, a synonym of T. foetus resides in the GI tract of pigs without causing clinical signs as mentioned in the section of molecular studies. So IPEC-J2 may represent the second best in vitro model. These authors showed that adhesion was via specific receptor – ligand interaction, required viable trichomonad cells and was independent of cytoskeletal activity of the trophozoites [47]. Lately the same authors elegantly demonstrated that feline T. foetus trophozoites progressively destroyed IPEC-J2 cell monolayer via apoptosis. The protozoan promoted a direct contact – dependent activation of intestinal epithelial cell apoptosis signaling. This pathologic effect depended upon T. foetus – cell associated cysteine proteases [48]. Effect of bovine T. foetus on epithelial cultured cells was investigated using clonal populations of the protozoan. Five clonal populations destroyed epithelial monolayers at different degrees, ranging from 25% to 55% despite similar cytoadhesion levels and whole-cell protease activity. They also showed various degrees of contact – dependent and contact – independent cytotoxicity. Contact – independent cytotoxicity was strictly related to the degree of enzyme activation of an extracellular protease [49]. Furthermore, it was shown that extracellular proteinases such as CP8 of T. foetus bovine isolate cleaved C3b (the bigger fragment of two C3 component in the original paper designed as C3a) to small fragments, which could play a role in evasion of complement killing in vivo as a result of preventing completion of complement activation cascade [50].
Figure 3.
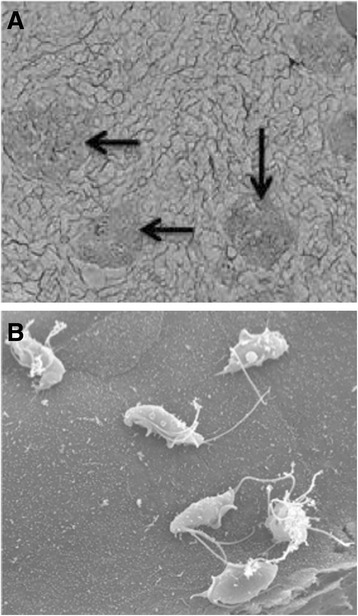
Scanning electron microscopy of Tritrichomonas foetus adhesion to porcine intestinal epithelial cell (IPEC)-J2 monolayers. A. Aggregates of trophozoites adhering to IPEC-J2 monolayers (arrows). B. Six trophoziotes adhering to a single IPEC-J2 cell. Reproduced with permission [47].
Taken together, the pathogenesis of T. foetus on the intestinal epithelial cells is both contact – dependent and contact – independent. In the former, cytopathic effect is mainly via apoptosis induced by cell-associated proteases, whereas extracellular proteases are the major players in contact – independent cytotoxicity. Extracellular proteases may also play a role in evading complement killing. Consequently proteases are a major player although other uncharacterized molecules may also contribute to pathogenesis of this intriguing trichomonad. Consistent with the notion, 483 and 445 bovine and feline isolates of T. foetus transcripts were determined to be proteases by a transcriptomical approach. Among these 389 and 346 were CP, respectively [20].
7. Host immunity
There is significant paucity of literature on immunity of feline hosts to microbial infections in general and to T. foetus infections in the GI tract in specific. The latter is understandable provided that the trichomonad has been ascribed to be causative agents only in last 15 or so years. In general IgA is a pivotal player in mucosal secretion of cat’s GI tract [51,52]. Consequently IgA profile in the GI tract among different age groups of various breeds is crucial to understand host immunity against and susceptibility to microbial infections. Unfortunately this information is very scarce at present. It was found very low concentrations of hyperimmune serum (up to 1:640 dilution, the highest available title in the experiments) promoted significant enhancement of killing of T. foetus bovine isolate by the alternative pathway of bovine complement [53]. Nevertheless, extracellular proteinases such as CP8 of T. foetus bovine isolate cleaved C3b to small inactive fragments, which may counteract this host defense system [50].
8. Epidemiology
8.1. Geographic distribution
Although T. foetus was reported in nine kittens with diarrhea as early as 1928 [5] its status as an etiological pathogen of chronic diarrhea of the domestic cat was only confirmed very recently. Gookin et al. established an association between diarrhea and T. foetus infections in the domestic cat in the USA [3]. They further determined that this trichomonad was the etiological agent of feline trichomonal diarrhea using rRNA gene sequence analysis; restriction enzyme digest mapping; and light, transmission, and scanning electron microscopy [4].
Tritrichomonas foetus has been diagnosed in the domestic cat in many geographic regions. To the best of our knowledge its geographic distribution has covered four continents including Europe (Austria, Finland, France, Germany, Greece, Italy, Netherland, Norway, Poland, Spain, Sweden, Switzerland, and UK), North America (Canada and USA), Australia/Oceania (Australia and New Zealand), and Asia (Japan and South Korea) (Figure 4). In some regions only case reports were available, whereas in others survey data were generated (Table 3). Many of the survey data were collected from diarrheic cats, show cat, cats in catteries, or cats presenting to veterinarians and veterinary clinics. Consequently there is a bias associated with such samples, i.e., a bias resulting in higher positive rate than cross-sectional samples that would have been collected from pet owners under the most scenarios. For instance in New Zealand, 22 samples of show cats revealed a positive rate of 82%. In USA diarrheic cats had positive rate as low as 6% in one study [54], and as high as 40% in another [55]. Figure 4 shows the different geographic regions of the world where surveys have been conducted and/or cases have been reported.
Figure 4.
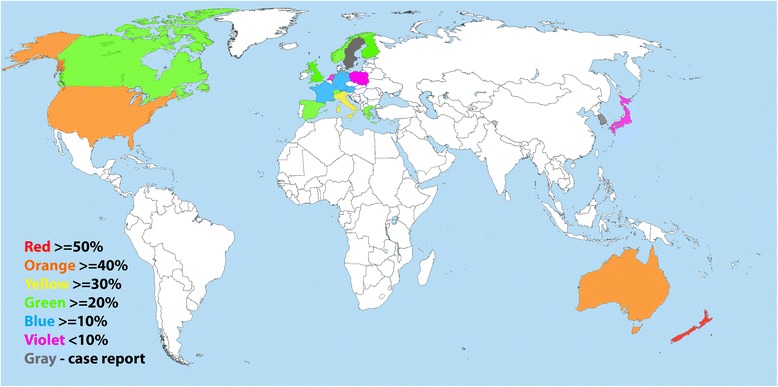
Geographical distribution of surveys for and case report of Tritrichomonas foetus detected positive cats worldwide. The prevalence of T. foetus infection of each regional study is reported although is not representative of the true prevalence of the entire country. Highest rate is used in countries with more than one regional report on prevalence.
Table 3.
Cases and prevalence of feline trichomonosis throughout the world
| Country | Year | Sources (cat examined) | Diagnosis | Case report | Prevalence (%) | Refs |
|---|---|---|---|---|---|---|
| Australia | Vet Clinic | M;C;PCR;S | 16 | [63] | ||
| Australia | 2006-2010 | Vet Clinic | M: PCR | 13 | [82] | |
| 2008-2009 | Cattery (59) | PCR | 42.4 | |||
| Australia | 2006-2007 | Cattery (82) | C;PCR | 0 | [83] | |
| Shelter (52) | 0 | |||||
| Austria & Germany | Fecal samples (31) | PCR,S | 19.4 | [84] | ||
| Austria | 1997-2008 | Necropsy (96); Organ samples (6) | chromogenic in situ hybridization; PCR; S | 2.9 | [71] | |
| Canada | Cats with chronical diarrhea (1) | PCR | 1 | [85] | ||
| Canada | 2011-2012 | Cat Clinic (140) | C;PCR | 0.7 | [61] | |
| Cat show (55) | 23.6 | |||||
| Humane Society (46) | 0 | |||||
| European Union – 15 countries | 2009-2010 | Diarrheic cats (1840) | PCR,S | 9.0 | [59,86] | |
| Finland | 2008-2010 | Diagnostic samples (60) | PCR | 28.3 | [87] | |
| France | 2009-2010 | Cat show (140) | C;S | 14.3 | [58] | |
| Germany | Diarrheic cats (3) | M, PCR, S | 3 | [88] | ||
| Germany | 2008 | Cat shows (230) | C;PCR;S | 15.7 | [35] | |
| Greece | Fecal samples (30) | PCR | 20.0 | [89] | ||
| Italy | 2008-2010 | Pet (181), sheltered cats (54), stray cats (28) | C | 0 | [90] | |
| Italy | Healthy pets (146) | PCR | 2.1 | [65] | ||
| Italy | 2006 | Rescued Cats (74) | M;C;PCR | 32.4 | [38] | |
| Japan | 2008 | Animal Hospitals (147) | C;PCR;S | 8.8 | [80] | |
| Netherland | 2006 | Diarrheic cats (53) | PCR | 2 | [91] | |
| Cattery (47) | 4 | |||||
| pet (54) | 0 | |||||
| New Zealand | 2006 | Cat shows (22) | C;PCR | 81.8 | [64] | |
| Norway | 2006 | Vet Clinic | M; PCR;S | 3 | [40] | |
| Norway | 2009 | Cat show (52) | C; PCR;S | 21.2 | [62] | |
| Poland | Vet Clinics (135) | C;PCR | 7.3 | [92] | ||
| South Korea | 2008 | Vet Clinic | M;C;PCR | 2 | [93] | |
| Spain | Cattery (20) | M;C;PCR | 25.0 | [94] | ||
| Sweden | Diarrheic cats (1) | 1 | [95] | |||
| Switzerland | 2007 | Diarrheic cats (45) | C;PCR;S | 24.4 | [96] | |
| Switzerland | 2007-2008 | Vet Clinic (105) | C;PCR | 25.7 | [97] | |
| UK | 2004 | Diarrheic cats (1) | M; PCR | 1 | [36] | |
| UK | 2006 | Diarrheic cats (111) | PCR | 14.4 | [57] | |
| UK | 2010 - 2012 | Diarrheic cats (1882) | PCR | 18.8 | [66] | |
| UK | Vet Clinic (163) | PCR | 20.0 | [98] | ||
| USA | Diarrheic cats (26) | M;C;PCR | 26 | [33] | ||
| USA | Diarrheic cats (32) | M;C | 32 | [3] | ||
| USA | Diarrheic cats (1) | M;C;PCR | 1 | [75] | ||
| USA | Diarrheic cats (4) | C; PCR | 4 | [74] | ||
| USA | Diarrheic cats (4) | C; PCR | 4 | [78] | ||
| USA | 2006-2009 | Vet Clinic (104) | PCR | 104 | [34] | |
| USA | Diarrheic cat (7) | M;C;PCR | 7 | [42] | ||
| USA | nondiarrheic cats (53) | C;PCR | 0.0 | [54] | ||
| Diarrheic cats (170) | 5.9 | |||||
| USA | Fecal samples (173) | C;PCR | 9.8 | [39] | ||
| USA | Catteries (61) | M; PCR | 24.6 | [41] | ||
| USA | 2001 | Cat show (117) | M;C;PCR | 30.8 | [60] | |
| USA | 2009-2012 | Diarrheic cats (68) | PCR | 39.7 | [55] |
C: Culture; M: Microscopy; PCR: polymerase chain reaction; S: Sequencing.
8.2. Risk factors
Odds ratio (OR) is commonly used to quantitatively gauge risk factors. An OR is a measure of association between an exposure and an outcome [56]. In this section OR will be used either directly taken from the original publications or calculated by us if data allow to do so. Risk factors discussed in the section include age and breed of the animals, a history of diarrhea, co-infection with other enteral protozoa and housing conditions etc.
8.2.1. Age
An association between age of infected cats and T. foetus infections has been probed in many studies, of which several were showed in Table 4. A common notion is that cats of one year old or younger are more susceptible to T. foetus. However, data presented in Table 4 did not show a clear picture at all. OR for cats ≤ 1 year old generated from data collected from France and UK were 2.5 (P = 0.057) and 13.4 (P < 0.01), respectively [57,58]. Further, Galian et al. reported a positive association between age and T. foetus prevalence among 1391 fecal samples submitted to a diagnostic laboratory originated from 15 countries in the European Union [59]. They found 10.4%, 5.5%, 2.5%, 3.5% and 0% T. foetus-positive cats among age groups ≤1 year old, 2-7, 8-11, 12-15 and ≥15 years old, respectively [59]. However, data from Germany yielded a contradicted picture with younger cats marginally less susceptible with OR 0.9 (P < 0.05) [35]. Also no association was found from data collected from Canada, Norway, and USA [60-62] (Table 4). Collectively data from multiple countries do not consistently support a notion that T. foetus infections occur more often in the domestic cat of one year old or younger.
Table 4.
Risk factors related to feline infections by Tritrichomonas foetus ¶
| Country | Age in month | Sex-male | Purebred | Housing | History of diarrhea in past 6 months | Food | Refs |
|---|---|---|---|---|---|---|---|
| Canada | <6 – 0.6 (0.1–3.4) | 2.0 (0.5–7.9) | 26.3 (3.8–1142.2)** | >5 cats per house – 4.6 (1.3–20.8)** | Another cat – 4.4 (1.3–16.2)** | Fed a raw food diet – 5.4 (1.5–19.6)** | [61] |
| Self – 1.7 (0.4–6.4) | |||||||
| France | <12 – #2.5(0.6-10.2)+ | NC | NC | NC | NC | [58] | |
| Germany | ≤12 – 0.9 (0.7-1.0)* | NC | Norwegian Forest – 25.9 (7.6-87.7)*** | NC | Another cat – 3.2 (1.2–9.9)** | NC | [35] |
| Self – 3.2 (1.1- 8.7)* | |||||||
| Norway | NC | NC | NC | NC (P = 0.1) | [62] | ||
| UK | 6-12 (29.4%); >12 (15.2%)*** | Pedigree (37.8%); | [66] | ||||
| Non-pedigree (6.0%)*** | |||||||
| UK | ≤12, #13.4(1.7-107.7)** | NC | # > 999.9 | [57] | |||
| Siamese and Bengal #7.3 (2.1-25.9)** | |||||||
| USA | Infected mean 8 vs non- infected mean 64.8*** | Abyssinians, Siamese and Bengal** | [54] | ||||
| USA | #> 999.9** | [41] | |||||
| USA | NC | NC | Self – 3.5 (1.1-11.3)* | [60] |
¶Odds ratio is given; 95% confidence interval is in bracket. Blank cells: no data available.
#:Calculated by the authors of current manuscript according to [56]; P value from the original paper.
*P < 0.05; **P < 0.01; ***P < 0.001; + P = 0.057.
NC: No correlation was detected.
A metadata analysis on OR of cat of one year old or younger was performed by the current authors on available data in publications, which all happened to originate from various European countries (Table 5). The cats in this age group had an OR of 2.1 (1.7-2.6) than older animals. Therefore, young age is a risk factor for T. foetus infection.
Table 5.
Data included in metadata analysis of odds ratio of young cats with Tritrichonomas foetus infections
8.2.2. Breed
There are many different pure breed and crossbreeds of the domestic cat throughout the world. Some breeds are more popular than the others in certain geographic regions. Many veterinarians have observed that purebreds present more often to clinics than crossbreds due to T. foetus infections. Among six sets of data all except one found this is true (Table 4). The only exception might be due to a small sample size. In this case, 20 T. foetus-positive samples were found in 140 show cats [58]. Purebreds have a much higher OR to be T. foetus positive than non-purebreds, which range from 26.3 in Canada [61] to >999.9 in UK [57]. Further analysis showed that a few breeds with a higher OR, such as 7.3 for Siamese and Bengal in UK [57], and 25.9 for Norwegian Forest in Germany [35]. Abyssinians, Siamese and Bengal were found more likely to be T. foetus positive in a survey carried out in USA [54]. Collectively purebred is a risk factor for T. foetus infections in general, and Abyssinians, Siamese, Bengal and Norwegian Forest in specific. Nevertheless, it is worthy of mentioning that some studies sampled purebred cats from cat breeding centers with a densely housed population. Under this scenario increased incidence of infection might be due to the reliance on close and direct contact among animals.
8.2.3. History of diarrhea
History of diarrhea can be the T. foetus positive cat itself, or the other cats sharing the same household in the past, say 6 months. In the former, two studies showed OR 3.2 (P < 0.05) in Germany [35] and 3.5 (P < 0.05) in USA [60]. Third study in Canada showed an OR 1.7 without statistical significance [61]. For the latter, two investigations resulted in ORs of 4.4 (P < 0.01) in Canada [61] and 3.2 in Germany (P < 0.01) [35]. Therefore, history of diarrhea in the past six months, no matter whether it is the presenting cat itself or its playmates, rendered a cat a threefold higher chance of having a T. foetus-positive status.
8.2.4. Co-infection with other enteric protozoa
Enteral protozoa of the domestic cat include, but are not limited to, T. foetus, Giardia duodenalis, Cryptosporidium spp. Toxoplasma gondii, Isospora spp. and Sarcocystis spp. Co-infection of these is not unusual. For example, five of 16 T. foetus positive cats were Giardia sp. positive in Australia [63]; five of 18 T. foetus positive cats were Giardia sp. positive in New Zealand [64]; ten, six and one of 36 T. foetus positive cats were Giardia sp., Isospora sp., and Cryptosporidium sp. positive, respectively, three were co-infected by all except Cryptosporidium sp. in a survey carried out in Germany [35]. In a survey of 146 fecal samples in Italy, co-infections were not found although 15, 11, 3, and 3 were positive for T. gondii, G. duodenalis, Cryptosporidium sp. and T. foetus, respectively [65]. A detail analysis of enteropathogen co-infection in UK cats with diarrhea was carried out. There was greater co-occurrence than random of G. duodenalis with either T. foetus or Cryptosporidium sp. respectively. Further a greater three-way co-occurrence existed among these three enteral protozoa [66]. These data collectively show that these enteral protozoa render greater risk for the domestic cat to be infected with T. foetus even though they may locate at different niches than T. foetus.
8.2.5. Others
A few other factors have been analyzed for and found their association with T. foetus-positive status occasionally. One is sex. Among seven studies only one demonstrated being a male kitten is a great risk factor (P < 0.01) [41]. Another one is housing with more than one other cat. One of four surveys showed sharing house with more than five cats had an OR 4.6 (P < 0.01) [61]. The third one is food, one of three investigations resulted in an OR 5.4 for feeding raw food diet (P < 0.01) [61]. What causes this disparity is beyond the scope of this manuscript. Plausible reasons include small sample sizes and confounding factors.
9. Diagnosis
Tritrichomonas foetus infection should be suspected in a cat with recent (<6 months) clinical signs of chronic large bowel diarrhea, with highest risk in densely housed young, purebred, show cats [3,60]. There are no differences in the signalment between Giardia sp. and T. foetus infected cats and co-infections are common enough (12%) to warrant testing for T. foetus despite the diagnosis of other enteric protozoal infection, although Giardia sp. is a small bowel parasite and the clinical signs should distinguish the infections. There have been no hematological or biochemical abnormalities reported in the literature. Diagnosis of a trichomonad infection is made by either the demonstration of the trophozoite on a saline diluted direct fecal smear (14.7% sensitivity), culture by inoculating MDM (26.4% sensitivity) or the commercially available InPouch™ TF medium (InPouch TF; BioMed Diagnostics, Inc, White City, OR USA) (58.8% sensitivity) or the extraction of DNA in feces and the amplification of T. foetus rDNA by the use of PCR [13,60]. Fecal samples include either a voided stool or collected by manual extraction with the aid of fecal loops or by a colon flush technique. The technique of colon flush is demonstrated in a video clip the North Carolina (NC) State University, College of Veterinary Medicine (CVM) website (Colon Flush Technique [67]). Fecal wet preparation is viewed under 40 × magnification. The motile characteristic of T. foetus differ from Giardia sp. in that it has a forward motility in contrast to a falling leaf motility of Giardia sp. as demonstrated in a video clip from the NC State University CVM website (T. foetus vs. Giardia [68]). Failing to distinguish the two trophozoites on microscopy, Giardia sp. can be confirmed by fecal enzyme-linked immunosorbent assay for Giardia-specific antigen [60]. In cases where T. foetus is suspected despite negative microscopy or fecal culture, when a faster turn-around time than culture is required, or for confirmation of an organism visible on microscopy, T. foetus cannot precisely be distinguished microscopically from Pentatrichomonas hominis, a commensal trichomonad, a commercially available PCR assay is available targeting part of the 18 s ribosomal RNA (rRNA). Submission of samples should be diarrheic and free from litter as formed stool rarely tests positive even if a subclinical shedder (NC State University CVM, Submission of Samples for T. foetus PCR Testing [69]). The sample, roughly the size of a lima bean should be submitted in a sterile tube and the remainder of the volume filled with isopropyl alcohol, without the need for refrigeration. Unfortunately PCR cannot prove the absence of infection.
Chronic experimentally induced infection with T. foetus is limited to the colon, cecum and ileum [28]. The distribution of T. foetus organisms within the colon is not homogenous and histopathological diagnosis on samples procured by necropsy, surgery or endoscopy in cats with naturally acquired infection had a sensitivity of 56% [42]. The probability of diagnosing T. foetus infection on histopathology is increased with the number of samples submitted. Thus examination of multiple samples will increase the likelihood of diagnosis with a minimum of 6 colon samples required to have a ≥95% confidence of detecting T. foetus on at least one sample [42]. A species (sequence) specific fluorescent antibody in situ hybridization (FISH) probe has been developed for the detection of T. foetus on formalin fixed samples allowing confirmation of location and molecular identification of a trichomonad [70]. A study examined an chromogenic in situ hybridization (CISH) technique using T. foetus and P. hominis probes on formalin archived small and large intestinal samples collected from young (4 weeks to 2 years of age) cats with diarrhea [71]. This technique is apparently more reliable than FISH technique as mammalian red blood cells, roughly the same size as trichomonads, auto-fluoresce. Four of the 102 samples were found to be positive, with three testing positive for the T. foetus probe and one with the P. hominis probe.
10. Treatment
The natural course of diarrhea in cats infected with T. foetus is waxing and waning, giving the false impression that therapy may be effective, but often relapsing after discontinuation of treatment [3]. Trichomonads rely on hydrogenosomal fermentation of pyruvate making them susceptibility to 5-nitroimidazole antibiotics, such as metronidazole, tinidazole and ronidazole [72]. Therapeutics reported in the literature include: paromomycin, fenbendazole, furazolidone, nitazoxanide, metronidazole, tinidazole and ronidazole [3,28]. One of the earliest reported descriptions of treatment was paromomycin, an aminoglycoside used to treat Trichomonas vaginalis, a human protozoal infection of the genital tract, at the same dose used to treat cryptosporidiosis in cats [3]. In the 25 cats studied, evaluated 3 days to 6 months after treatment, only three had normal stool without T. foetus isolated from their stool. Forty percent of the cats in the study continued to have diarrhea after treatment, of which 9 had positive fecal smears, and in the 12 cats that had normal stools, 22% of those cats tested (n = 9) had positive fecal smears. Three of the cats in the study were kittens and 2 of them suffered side-effects including acute renal failure, deafness and cataracts. These kittens were included in a case series of 4 kittens that suffered severe side-effects (acute renal failure, deafness and cataracts) after treatment with oral paromomycin [73]. Paromomycin has also been tested in vitro using a 24-h sensitivity assay and the results showed no effect at minimum lethal concentrations (MLC) ≤ 80 μg/mL [74]. Eleven of the original 25 cats were subsequently treated with fenbendazole and then 2-weeks later by furazolidone [3]. There was a decrease in the number of cats having diarrhea, although the stool was described as semi-formed in 9 of the cats with confirmed shedding trichomonads for the following 10-months. Furazolidone has shown equal 24-hour susceptibilities of T. foetus cultures to that of metronidazole and ronidazole at MLC of 0.625 to 2.5 μg/mL [74]. In experimentally infected cats, nitazoxanide, a nitrothiazole benzamide compound, with broad-spectrum antiprotozoal activity, decreased the number of trichomonads shed in the feces but failed to eliminate the T. foetus infection, although it did eliminate the cryptosporidial infection in those cats that were co-infected. Reported side-effects of nausea and foul-smelling dark diarrhea make it even less attractive as a therapeutic.
Nitroimidazoles (metronidazole, tinidazole and ronidazole) have been investigated both in vitro and in vivo in experimentally induced infections [74-76]. Metronidazole did not show any inhibitory effect in vitro at concentrations ≤10 μg/mL in contrast to tinidazole and ronidazole which had an inhibitory effect at MLC of ≥0.1 μg/mL [75]. Kather et al. demonstrated in vitro results that contradict these findings, as both metronidazole (1.25 to 2.5 μg/mL) and ronidazole (0.625 to 2.5 μg/mL) had a 24-h kill effect on T. foetus isolates, although ronidazole had lower 24-h MLC for some isolates [74]. Time-kill assays, which evaluate the degree of growth inhibition and survival during 24-h incubation demonstrated a significant difference in the survival kinetics of T. foetus in culture incubated with metronidazole as compared to ronidazole, with ronidazole being more effective [74]. Tinidazole has been investigated twice in vitro with reported MLC of ≥0.1 μg/mL and ≥10 μg/mL [75,76]. The disparity may be ascribable to different strains used in the two experiments.
The efficacy of metronidazole in vitro has not been translated to an in vivo efficacy, although transient improvement in clinical signs do occur independent of elimination of the T. foetus infection, the reasons proposed include alteration in bacterial microflora, elimination of Giardia co-infection or immunomodulatory effect [33,74]. Interestingly, treatment of infected cats with antibiotics that kill natural microbiota will increase shedding of T. foetus, as the organism is dependent on host bacteria for acquisition of micronutrients [75]. Tinidazole cleared experimentally induced T. foetus infection within 3-days, but the trichomonads were detected within 6 to 8 weeks after discontinuation of the treatment [76]. The poor in vivo efficacy may be related to its increased absorption and reduced concentration within the intestines. Ronidazole has been investigated in experimentally infected cats and shedding discontinued within 3-days of initiating therapy at 10 mg/kg, dosed orally every 12 h, although relapse was detected but the cultured organisms retrieved from the feces remained susceptible to ronidazole in vitro [75]. Relapses were reported in cats receiving a dose of 30 mg/kg twice daily but not in cats receiving 50 mg/kg twice daily. One reason for better efficacy of ronidazole as compared to other nitroimidazoles may be due to improved trapping of the activated compounds within the intestine [75].
Nitroimidazole resistant trichomonads are hydrogenosomal pyruvate:ferredoxin oxidoreductase deficient, and compensate by increased glycolysis and alternative cytosolic pathways. Ronidazole resistance is defined as aerobic MLC ≥100 μg/mL and is both inherent and acquired [77]. Resistant strains of T. foetus to ronidazole have been documented in cats with confirmed treatment failure after excluding the possibility of reinfection or urogenital nidus, and is related to the cross resistance of the organism to all nitroimidazole drugs [77].
Ronidazole is not registered for human or veterinary use and informed consent is necessary prior to use in cats and should only be prescribed in confirmed cases. The current recommended dose is 30 mg/kg, once daily for 14-days [75]. Relapse is common and cats with resolved clinical signs can continue to carry the organism and thus vigilant and prolonged post-treatment monitoring is indicated. No adverse effects were reported in the original study that examined ronidazole as a treatment for T. foetus at doses as high as 50 mg/kg, twice daily and hematology and biochemistry results remained within reference range and did not change as compared to pretreatment values [75]. Subsequent to this, four cases of neurological toxicity in cats treated with ronidazole in the range of 30 to 50 mg/kg were reported. The clinical signs included, having a blank stare, “slow motion” movements, agitation, facial tremors, trembling of the extremities, unable to jump or walk stairs and hyperesthesia which started three to nine days after initiating ronidazole, lasting one to four weeks in duration [78]. A lower dose of ronidazole, 10-30 mg/kg once daily, for 14 days, together with a probiotic (Pro-Kolin Enterogenic, Protexin, Probiotics International) was compared to a placebo control and ronidazole at the same dose, frequency and duration in age matched cats diagnosed with T. foetus-associated diarrhea [79]. No side-effects were noted with relapse reported in both groups but cats that received the probiotic with the ronidazole were less likely to relapse.
11. Conclusions
Feline trichomonosis is caused by T. foetus. The etiology was determined merely one and half a decades ago. The current manuscript comprehensively reviews the trichomonad biology and the disease itself. The authors hope this will provides individuals who are interesting in the topic with one source for updated information.
16. Acknowledgments
The authors are very grateful to Dr A Lee Willingham of RUSVM for his critical review of the manuscript. Drs. Esteban Soto and Edyta Bajak of RUSVM translated literature published in Spanish and Polish, respectively. The cost for publication is provided by an intramural grant of RUSVM One Health Center for Zoonoses and Tropical Veterinary Medicine.
12. Abbreviations
- bp
base pair
- BL
bovine lymphosarcoma
- BVEC
Bovine vaginal epithelial cells
- CISH
Chromogenic in situ hybridization
- CP
Cysteine protease
- CVM
College of Veterinary Medicine
- dpi
days post infection
- EL
Elongation factor
- FISH
Fluorescent antibody in situ hybridization
- GI
Gastrointestinal
- IPEC
Porcine intestinal epithelial cell
- ITS
Internal transcribed spacer
- LPG
Lipophosphoglycan
- MDH
malate dehydrogenase
- MDM
Modified Diamond’s Medium
- MLC
Minimum lethal concentration
- NC
North Carolina
- OR
Odds ratio
- RAPD
Random amplified polymorphic DNA
- RFLP
Restriction fragment length polymorphism
- RUSVM
Ross University School of Veterinary Medicine
Footnotes
13. Competing interests
The authors declare that they have no competing interests.
14. Authors’ contributions
CY conceived the manuscript, and wrote all sections except the ones by LSK who was responsible for clinical signs associated with gastrointestinal tract infection, diagnosis and treatment. Both authors read and approved the final manuscript.
15. Authors’ information
CY is an Associate Professor of Parasitology at Ross University School of Veterinary Medicine (RUSVM). CY has studied T. foetus for more than five years and published five refereed paper on the subject and 45 refereed manuscripts on other topics. CY had headed the Parasitology section of Wyoming State Veterinary Laboratory (WSVL) between 2008 and 2013, where about 8000 T. foetus testing was annually performed. LSK is an European Specialist in Internal Medicine and an Assistant Professor of Internal Medicine at RUSVM. LSK has 15 years of clinical experience working with companion animals including cats as a veterinarian and has frequently diagnosed and treated feline trichomonosis.
Contributor Information
Chaoqun Yao, Email: chyao@rossvet.edu.kn.
Liza S Köster, Email: lkoster@rossvet.edu.kn.
17. References
- 1.Yao C. Opportunistic human infections caused by Tritrichomonas species: a mini-review. Clin Microbiol Newsl. 2012;34:127–131. doi: 10.1016/j.clinmicnews.2012.07.004. [DOI] [Google Scholar]
- 2.Yao C. Diagnosis of Tritrichomonas foetus-infected bulls, an ultimate approach to eradicate bovine trichomoniasis in US cattle? J Med Microbiol. 2013;62:1–9. doi: 10.1099/jmm.0.047365-0. [DOI] [PubMed] [Google Scholar]
- 3.Gookin JL, Breitschwerdt EB, Levy MG, Gager RB, Benrud JG. Diarrhea associated with trichomonosis in cats. J Am Vet Med Assoc. 1999;215:1450–1454. [PubMed] [Google Scholar]
- 4.Levy MG, Gookin JL, Poore M, Birkenheuer AJ, Dykstra MJ, Litaker RW. Tritrichomonas foetus and not Pentatrichomonas hominis is the etiologic agent of feline trichomonal diarrhea. J Parasitol. 2003;89:99–104. doi: 10.1645/0022-3395(2003)089[0099:TFANPH]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Kessel JF. Trichomoniasis in kittens. Trans R Soc Trop Med Hyg. 1928;22:61–80. doi: 10.1016/S0035-9203(28)90155-8. [DOI] [Google Scholar]
- 6.Benchimol M. Trichomonads under Microscopy. Microsc Microanal. 2004;10:528–550. doi: 10.1017/S1431927604040905. [DOI] [PubMed] [Google Scholar]
- 7.Lipman NS, Lampen N, Nguyen HT. Identification of pseudocysts of Tritrichomonas muris in Armenian hamsters and their transmission to mice. Lab Anim Sci. 1999;49:313–315. [PubMed] [Google Scholar]
- 8.Mariante RM, Lopes LC, Benchimol M. Tritrichomonas foetus pseudocysts adhere to vaginal epithelial cells in a contact-dependent manner. Parasitol Res. 2004;92:303–312. doi: 10.1007/s00436-003-1026-z. [DOI] [PubMed] [Google Scholar]
- 9.Pereira-Neves A, Ribeiro KC, Benchimol M. Pseudocysts in trichomonads–new insights. Protist. 2003;154:313–329. doi: 10.1078/143446103322454095. [DOI] [PubMed] [Google Scholar]
- 10.Gruffydd-Jones T, Addie D, Belak S, Boucraut-Baralon C, Egberink H, Frymus T, Hartmann K, Hosie MJ, Lloret A, Lutz H, Marsilio F, Möstl K, Pennisi MG, Radford AD, Thiry E, Truyen U, Horzinek MC. Tritrichomoniasis in cats: ABCD guidelines on prevention and management. J Feline Med Surg. 2013;15:647–649. doi: 10.1177/1098612X13489231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lappin MR. Enteric protozoal diseases. Vet Clin North Am Small Anim Pract. 2005;35:81–88. doi: 10.1016/j.cvsm.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Levy MG, Gookin JL, Poore MF, Litaker RW, Dykstra M. Information on parasitic gastrointestinal tract infections in cats. J Am Vet Med Assoc. 2001;218:194–195. [PubMed] [Google Scholar]
- 13.Manning K. Update on the diagnosis and management of Tritrichomonas foetus infections in cats. Top Companion Anim Med. 2010;25:145–148. doi: 10.1053/j.tcam.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 14.Payne PA, Artzer M. The biology and control of Giardia spp and Tritrichomonas foetus. Vet Clin North Am Small Anim Pract. 2009;39:993–1007. doi: 10.1016/j.cvsm.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 15.Tolbert MK, Gookin J. Tritrichomonas foetus: a new agent of feline diarrhea. Compend Contin Educ Vet. 2009;31:374–381. [PubMed] [Google Scholar]
- 16.Reinmann K, Muller N, Kuhnert P, Campero CM, Leitsch D, Hess M, Henning K, Fort M, Muller J, Gottstein B, Frey CF. Tritrichomonas foetus isolates from cats and cattle show minor genetic differences in unrelated loci ITS-2 and EF-1alpha. Vet Parasitol. 2012;185:138–144. doi: 10.1016/j.vetpar.2011.09.032. [DOI] [PubMed] [Google Scholar]
- 17.Slapeta J, Craig S, McDonell D, Emery D. Tritrichomonas foetus from domestic cats and cattle are genetically distinct. Exp Parasitol. 2010;126:209–213. doi: 10.1016/j.exppara.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 18.Slapeta J, Muller N, Stack CM, Walker G, Lew-Tabor A, Tachezy J, Frey CF. Comparative analysis of Tritrichomonas foetus (Riedmuller, 1928) cat genotype, T. foetus (Riedmuller, 1928) cattle genotype and Tritrichomonas suis (Davaine, 1875) at 10 DNA loci. Int J Parasitol. 2012;42:1143–1149. doi: 10.1016/j.ijpara.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 19.Sun Z, Stack C, Slapeta J. Sequence differences in the diagnostic region of the cysteine protease 8 gene of Tritrichomonas foetus parasites of cats and cattle. Vet Parasitol. 2012;186:445–449. doi: 10.1016/j.vetpar.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Morin-Adeline V, Lomas R, O’Meally D, Stack C, Conesa A, Sapeta J. Comparative transcriptomics reveals striking similarities between the bovine and feline isolates of Tritrichomonas foetus: consequences for in silico drug-target identification. BMC Genomics. 2014;15:955. doi: 10.1186/1471-2164-15-955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Walden HS, Dykstra C, Dillon A, Rodning S, Givens D, Bird R, Newton J, Lindsay D. A new species of Tritrichomonas (Sarcomastigophora: Trichomonida) from the domestic cat (Felis catus) Parasitol Res. 2013;112:2227–2235. doi: 10.1007/s00436-013-3381-8. [DOI] [PubMed] [Google Scholar]
- 22.Felleisen RS. Comparative genetic analysis of tritrichomonadid protozoa by the random amplified polymorphic DNA technique. Parasitol Res. 1998;84:153–156. doi: 10.1007/s004360050374. [DOI] [PubMed] [Google Scholar]
- 23.Hampl V, Pavlicek A, Flegr J. Construction and bootstrap analysis of DNA fingerprinting-based phylogenetic trees with the freeware program FreeTree: application to trichomonad parasites. Int J Syst Evol Microbiol. 2001;51:731–735. doi: 10.1099/00207713-51-3-731. [DOI] [PubMed] [Google Scholar]
- 24.Tachezy J, Tachezy R, Hampl V, Sedinova M, Vanacova S, Vrlik M, Van Ranst M, Flegr J, Kuldaa J. Cattle pathogen Tritrichomonas foetus (Riedmuller, 1928) and pig commensal Tritrichomonas suis (Gruby & Delafond, 1843) belong to the same species. J Eukaryot Microbiol. 2002;49:154–163. doi: 10.1111/j.1550-7408.2002.tb00360.x. [DOI] [PubMed] [Google Scholar]
- 25.Kleina P, Bettim-Bandinelli J, Bonatto SL, Benchimol M, Bogo MR. Molecular phylogeny of Trichomonadidae family inferred from ITS-1, 5.8S rRNA and ITS-2 sequences. Int J Parasitol. 2004;34:963–970. doi: 10.1016/j.ijpara.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Walker RL, Hayes DC, Sawyer SJ, Nordhausen RW, Van Hoosear KA, BonDurant RH. Comparison of the 5.8S rRNA gene and internal transcribed spacer regions of trichomonadid protozoa recovered from the bovine preputial cavity. J Vet Diagn Invest. 2003;15:14–20. doi: 10.1177/104063870301500104. [DOI] [PubMed] [Google Scholar]
- 27.Lun ZR, Chen XG, Zhu XQ, Li XR, Xie MQ. Are Tritrichomonas foetus and Tritrichomonas suis synonyms? Trends Parasitol. 2005;21:122–125. doi: 10.1016/j.pt.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 28.Gookin JL, Levy MG, Law JM, Papich MG, Poore MF, Breitschwerdt EB. Experimental infection of cats with Tritrichomonas foetus. Am J Vet Res. 2001;62:1690–1697. doi: 10.2460/ajvr.2001.62.1690. [DOI] [PubMed] [Google Scholar]
- 29.Hale S, Norris JM, Slapeta J. Prolonged resilience of Tritrichomonas foetus in cat faeces at ambient temperature. Vet Parasitol. 2009;166:60–65. doi: 10.1016/j.vetpar.2009.07.032. [DOI] [PubMed] [Google Scholar]
- 30.Van der Saag M, McDonell D, Slapeta J. Cat genotype Tritrichomonas foetus survives passage through the alimentary tract of two common slug species. Vet Parasitol. 2011;177:262–266. doi: 10.1016/j.vetpar.2010.11.054. [DOI] [PubMed] [Google Scholar]
- 31.Rosypal AC, Ripley A, Stockdale Walden HD, Blagburn BL, Grant DC, Lindsay DS. Survival of a feline isolate of Tritrichomonas foetus in water, cat urine, cat food and cat litter. Vet Parasitol. 2012;185:279–281. doi: 10.1016/j.vetpar.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Stockdale HD, Dillon AR, Newton JC, Bird RC, Bondurant RH, Deinnocentes P, Barney S, Bulter J, Land T, Spencer JA, Lindsay DS, Blagburn BL. Experimental infection of cats (Felis catus) with Tritrichomonas foetus isolated from cattle. Vet Parasitol. 2008;154:156–161. doi: 10.1016/j.vetpar.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 33.Foster DM, Gookin JL, Poore MF, Stebbins ME, Levy MG. Outcome of cats with diarrhea and Tritrichomonas foetus infection. J Am Vet Med Assoc. 2004;225:888–892. doi: 10.2460/javma.2004.225.888. [DOI] [PubMed] [Google Scholar]
- 34.Xenoulis PG, Lopinski DJ, Read SA, Suchodolski JS, Steiner JM. Intestinal Tritrichomonas foetus infection in cats: a retrospective study of 104 cases. J Feline Med Surg. 2013;15:1098–1103. doi: 10.1177/1098612X13495024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kuehner KA, Marks SL, Kass PH, Sauter-Louis C, Grahn RA, Barutzki D, Hartmann K. Tritrichomonas foetus infection in purebred cats in Germany: prevalence of clinical signs and the role of co-infection with other enteroparasites. J Feline Med Surg. 2011;13:251–258. doi: 10.1016/j.jfms.2010.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mardell EJ, Sparkes AH. Chronic diarrhoea associated with Tritrichomonas foetus infection in a British cat. Vet Rec. 2006;158:765–766. doi: 10.1136/vr.158.22.765. [DOI] [PubMed] [Google Scholar]
- 37.Stockdale H, Rodning S, Givens M, Carpenter D, Lenz S, Spencer J, Dykstra C, Lindsay D, Blagburn B. Experimental infection of cattle with a feline isolate of Tritrichomonas foetus. J Parasitol. 2007;93:1429–1434. doi: 10.1645/GE-1305.1. [DOI] [PubMed] [Google Scholar]
- 38.Holliday M, Deni D, Gunn-Moore DA. Tritrichomonas foetus infection in cats with diarrhoea in a rescue colony in Italy. J Feline Med Surg. 2009;11:131–134. doi: 10.1016/j.jfms.2008.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stockdale HD, Givens MD, Dykstra CC, Blagburn BL. Tritrichomonas foetus infections in surveyed pet cats. Vet Parasitol. 2009;160:13–17. doi: 10.1016/j.vetpar.2008.10.091. [DOI] [PubMed] [Google Scholar]
- 40.Dahlgren SS, Gjerde B, Pettersen HY. First record of natural Tritrichomonas foetus infection of the feline uterus. J Small Anim Pract. 2007;48:654–657. doi: 10.1111/j.1748-5827.2007.00405.x. [DOI] [PubMed] [Google Scholar]
- 41.Gray SG, Hunter SA, Stone MR, Gookin JL. Assessment of reproductive tract disease in cats at risk for Tritrichomonas foetus infection. Am J Vet Res. 2010;71:76–81. doi: 10.2460/ajvr.71.1.76. [DOI] [PubMed] [Google Scholar]
- 42.Yaeger MJ, Gookin JL. Histologic features associated with tritrichomonas foetus-induced colitis in domestic cats. Vet Pathol. 2005;42:797–804. doi: 10.1354/vp.42-6-797. [DOI] [PubMed] [Google Scholar]
- 43.Burgess DE, Knoblock KF, Daugherty T, Robertson NP. Cytotoxic and hemolytic effects of Tritrichomonas foetus on mammalian cells. Infect Immun. 1990;58:3627–3632. doi: 10.1128/iai.58.11.3627-3632.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Corbeil LB, Hodgson JL, Jones DW, Corbeil RR, Widders PR, Stephens LR. Adherence of Tritrichomonas foetus to bovine vaginal epithelial cells. Infect Immun. 1989;57:2158–2165. doi: 10.1128/iai.57.7.2158-2165.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singh BN, Lucas JJ, Beach DH, Shin ST, Gilbert RO. Adhesion of Tritrichomonas foetus to bovine vaginal epithelial cells. Infect Immun. 1999;67:3847–3854. doi: 10.1128/iai.67.8.3847-3854.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Singh BN, Lucas JJ, Hayes GR, Kumar I, Beach DH, Frajblat M, Gilbert RO, Sommer U, Costello CE. Tritrichomonas foetus induces apoptotic cell death in bovine vaginal epithelial cells. Infect Immun. 2004;72:4151–4158. doi: 10.1128/IAI.72.7.4151-4158.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tolbert MK, Stauffer SH, Gookin JL. Feline Tritrichomonas foetus adhere to intestinal epithelium by receptor-ligand-dependent mechanisms. Vet Parasitol. 2013;192:75–82. doi: 10.1016/j.vetpar.2012.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tolbert MK, Stauffer SH, Brand MD, Gookin JL. Cysteine protease activity of feline Tritrichomonas foetus promotes adhesion-dependent cytotoxicity to intestinal epithelial cells. Infect Immun. 2014;82:2851–2859. doi: 10.1128/IAI.01671-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Da Rocha-Azevedo B, De Melo-Braga MB, Silva-Filho FC E. Intra-strain clonal phenotypic variation of Tritrichomonas foetus is related to the cytotoxicity exerted by the parasite to cultured cells. Parasitol Res. 2005;95:106–112. doi: 10.1007/s00436-004-1251-0. [DOI] [PubMed] [Google Scholar]
- 50.Kania SA, Reed SL, Thomford JW, BonDurant RH, Hirata K, Corbeil RR, North MJ, Corbeil LB. Degradation of bovine complement C3 by trichomonad extracellular proteinase. Vet Immunol Immunopathol. 2001;78:83–96. doi: 10.1016/S0165-2427(00)00256-7. [DOI] [PubMed] [Google Scholar]
- 51.Allenspach K. Clinical immunology and immunopathology of the canine and feline intestine. Vet Clin North Am Small Anim Pract. 2011;41:345–360. doi: 10.1016/j.cvsm.2011.01.004. [DOI] [PubMed] [Google Scholar]
- 52.Stokes C, Waly N. Mucosal defence along the gastrointestinal tract of cats and dogs. Vet Res. 2006;37:281–293. doi: 10.1051/vetres:2006015. [DOI] [PubMed] [Google Scholar]
- 53.Aydintug MK, Leid RW, Widders PR. Antibody enhances killing of Tritrichomonas foetus by the alternative bovine complement pathway. Infect Immun. 1990;58:944–948. doi: 10.1128/iai.58.4.944-948.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Queen EV, Marks SL, Farver TB. Prevalence of selected bacterial and parasitic agents in feces from diarrheic and healthy control cats from Northern California. J Vet Intern Med. 2012;26:54–60. doi: 10.1111/j.1939-1676.2011.00843.x. [DOI] [PubMed] [Google Scholar]
- 55.Polak KC, Levy JK, Crawford PC, Leutenegger CM, Moriello KA. Infectious diseases in large-scale cat hoarding investigations. Vet J. 2014;201:189–195. doi: 10.1016/j.tvjl.2014.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Szumilas M. Explaining Odds Ratios. J Can Acad Child Adolesc Psychiatry. 2010;19:227–229. doi: 10.1007/s00787-010-0087-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gunn-Moore DA, McCann TM, Reed N, Simpson KE, Tennant B. Prevalence of Tritrichomonas foetus infection in cats with diarrhoea in the UK. J Feline Med Surg. 2007;9:214–218. doi: 10.1016/j.jfms.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Profizi C, Cian A, Meloni D, Hugonnard M, Lambert V, Groud K, Gagnon AC, Viscogliosi E, Zenner L. Prevalence of Tritrichomonas foetus infections in French catteries. Vet Parasitol. 2013;196:50–55. doi: 10.1016/j.vetpar.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 59.Galián M, Heusinger A, Gentil M, Müller E (2011) Tritrichomonas fetus in cats. Argos - Informativo Veterinario 134:44-45.
- 60.Gookin JL, Stebbins ME, Hunt E, Burlone K, Fulton M, Hochel R, Talaat M, Poore M, Levy MG. Prevalence of and risk factors for feline Tritrichomonas foetus and giardia infection. J Clin Microbiol. 2004;42:2707–2710. doi: 10.1128/JCM.42.6.2707-2710.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hosein A, Kruth SA, Pearl DL, Richardson D, Maggs JC, Peach HA, Peregrine AS. Isolation of Tritrichomonas foetus from cats sampled at a cat clinic, cat shows and a humane society in southern Ontario. J Feline Med Surg. 2013;15:706–711. doi: 10.1177/1098612X13475617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tysnes K, Gjerde B, Nodtvedt A, Skancke E. A cross-sectional study of Tritrichomonas foetus infection among healthy cats at shows in Norway. Acta Vet Scand. 2011;53:39. doi: 10.1186/1751-0147-53-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bissett SA, Gowan RA, O’Brien CR, Stone MR, Gookin JL. Feline diarrhoea associated with Tritrichomonas cf. foetus and Giardia co-infection in an Australian cattery. Aust Vet J. 2008;86:440–443. doi: 10.1111/j.1751-0813.2008.00356.x. [DOI] [PubMed] [Google Scholar]
- 64.Kingsbury DD, Marks SL, Cave NJ, Grahn RA. Identification of Tritrichomonas foetus and Giardia spp. infection in pedigree show cats in New Zealand. N Z Vet J. 2010;58:6–10. doi: 10.1080/00480169.2010.65054. [DOI] [PubMed] [Google Scholar]
- 65.Mancianti F, Nardoni S, Mugnaini L, Zambernardi L, Guerrini A, Gazzola V, Papini RA. A retrospective molecular study of select intestinal protozoa in healthy pet cats from Italy. J Feline Med Surg. 2015;17:163–167. doi: 10.1177/1098612X14533549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Paris J, Wills S, Balzer H-J, Shaw D, Gunn-Moore D. Enteropathogen co-infection in UK cats with diarrhoea. BMC Vet Res. 2014;10:13. doi: 10.1186/1746-6148-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Colon Flush Technique [http://www.youtube.com/watch?v=JMfZ9M80V8E] Accessed 15 Jan 2015
- 68.T. foetus vs. Giardia [http://www.youtube.com/watch?v=aF06jlbcF8E] Accessed 15 Jan 2015
- 69.NC State University CVM, Submission of Samples for T. foetus PCR Testing [http://www.JodyGookin.com]. Accessed 15 Jan 2015
- 70.Gookin JL, Stone MR, Yaeger MJ, Meyerholz DK, Moisan P. Fluorescence in situ hybridization for identification of Tritrichomonas foetus in formalin-fixed and paraffin-embedded histological specimens of intestinal trichomoniasis. Vet Parasitol. 2010;172:139–143. doi: 10.1016/j.vetpar.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 71.Mostegl MM, Wetscher A, Richter B, Nedorost N, Dinhopl N, Weissenbock H. Detection of Tritrichomonas foetus and Pentatrichomonas hominis in intestinal tissue specimens of cats by chromogenic in situ hybridization. Vet Parasitol. 2012;183:209–214. doi: 10.1016/j.vetpar.2011.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kulda J. Trichomonads, hydrogenosomes and drug resistance. Int J Parasitol. 1999;29:199–212. doi: 10.1016/S0020-7519(98)00155-6. [DOI] [PubMed] [Google Scholar]
- 73.Gookin JL, Riviere JE, Gilger BC, Papich MG. Acute renal failure in four cats treated with paromomycin. J Am Vet Med Assoc. 1999;215:1821–1823. [PubMed] [Google Scholar]
- 74.Kather EJ, Marks SL, Kass PH. Determination of the in vitro susceptibility of feline Tritrichomonas foetus to 5 antimicrobial agents. J Vet Intern Med. 2007;21:966–970. doi: 10.1111/j.1939-1676.2007.tb03050.x. [DOI] [PubMed] [Google Scholar]
- 75.Gookin JL, Copple CN, Papich MG, Poore MF, Stauffer SH, Birkenheuer AJ, Twedt DC, Levy MG. Efficacy of ronidazole for treatment of feline Tritrichomonas foetus infection. J Vet Intern Med. 2006;20:536–543. doi: 10.1111/j.1939-1676.2006.tb02893.x. [DOI] [PubMed] [Google Scholar]
- 76.Gookin JL, Stauffer SH, Coccaro MR, Poore MF, Levy MG, Papich MG. Efficacy of tinidazole for treatment of cats experimentally infected with Tritrichomonas foetus. Am J Vet Res. 2007;68:1085–1088. doi: 10.2460/ajvr.68.10.1085. [DOI] [PubMed] [Google Scholar]
- 77.Gookin JL, Stauffer SH, Dybas D, Cannon DH. Documentation of in vivo and in vitro aerobic resistance of feline Tritrichomonas foetus isolates to ronidazole. J Vet Intern Med. 2010;24:1003–1007. doi: 10.1111/j.1939-1676.2010.0534.x. [DOI] [PubMed] [Google Scholar]
- 78.Rosado TW, Specht A, Marks SL. Neurotoxicosis in 4 cats receiving ronidazole. J Vet Intern Med. 2007;21:328–331. doi: 10.1111/j.1939-1676.2007.tb02968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lalor SL, Gunn-Moore DA. Effects of concurrent ronidazole and probiotic therapy in cats with Tritrichomonas foetus-associated diarrhoea. J Feline Med Surg. 2012;14:650–658. doi: 10.1177/1098612X12455302. [DOI] [Google Scholar]
- 80.Doi J, Hirota J, Morita A, Fukushima K, Kamijyo H, Ohta H, Yamasaki M, Takahashi T, Katakura K, Oku Y. Intestinal Tritrichomonas suis (=T. foetus) infection in Japanese cats. J Vet Med Sci. 2012;74:413–417. doi: 10.1292/jvms.11-0171. [DOI] [PubMed] [Google Scholar]
- 81.Midlej V, Pereira-Neves A, Kist LW, Bogo MR, Benchimol M. Ultrastructural features of Tritrichomonas mobilensis and comparison with Tritrichomonas foetus. Vet Parasitol. 2011;182:171–180. doi: 10.1016/j.vetpar.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 82.Bell ET, Gowan RA, Lingard AE, McCoy RJ, Slapeta J, Malik R. Naturally occurring Tritrichomonas foetus infections in Australian cats: 38 cases. J Feline Med Surg. 2010;12:889–898. doi: 10.1016/j.jfms.2010.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bissett SA, Stone ML, Malik R, Norris JM, O’Brien C, Mansfield CS, Nicholls JM, Griffin A, Gookin JL. Observed occurrence of Tritrichomonas foetus and other enteric parasites in Australian cattery and shelter cats. J Feline Med Surg. 2009;11:803–807. doi: 10.1016/j.jfms.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Steiner JM, Xenoulis PG, Read SA, Suchodolski JS, Globokar M, Huisinga E, Thuere S. Identification of Tritrichomonas foetus DNA in feces from cats with diarrhea from Germany and Austria. J Vet Intern Med. 2007;21:649. [Google Scholar]
- 85.Pham D. Chronic intermittent diarrhea in a 14-month-old Abyssinian cat. Can Vet J. 2009;50:85–87. [PMC free article] [PubMed] [Google Scholar]
- 86.Galián M, Gentil M, Heusinger A, Müller E (2011) Tritrichomonas foetus as a cause of diarrhoea in cats. Tierärztliche Umschau Parasiten-Spezial 1:5-8
- 87.Castrén L, Vainio-Siukola K, Laaksonen I, Saari S. Tritrichomonas foetus as a cause of feline chronic large bowel diarrhoea. Suomen Eläinlääkärilehti. 2011;117:371–378. [Google Scholar]
- 88.Schrey C, Mundhenk L, Grubers A, Henning K, Frey C. Tritrichomonas foetus as a cause of diarrhoea in three cats. Kleintierpraxis. 2009;54:93–96. [Google Scholar]
- 89.Xenoulis PG, Saridomichelakis MN, Read SA, Suchodolski JS, Steiner JM. Detection of Tritrichomonas foetus in cats in Greece. J Feline Med Surg. 2010;12:831–833. doi: 10.1016/j.jfms.2010.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mugnaini L, Papini R, Gorini G, Passantino A, Merildi V, Mancianti F. Pattern and predictive factors of endoparasitism in cats in Central Italy. Rev Med Vet. 2012;163:89–94. [Google Scholar]
- 91.van Doorn DC, de Bruin MJ, Jorritsma RA, Ploeger HW, Schoormans A. Prevalence of Tritrichomonas foetus among Dutch cats. Tijdschr Diergeneeskd. 2009;134:698–700. [PubMed] [Google Scholar]
- 92.Hensinger T. Trichomonas foetus. A pathogen responsible for diarrhoea in cats. Weterynaria w Praktyce. 2009;6:80–81. [Google Scholar]
- 93.Lim S, Park SI, Ahn KS, Oh DS, Ryu JS, Shin SS. First report of feline intestinal trichomoniasis caused by Tritrichomonas foetus in Korea. Korean J Parasitol. 2010;48:247–251. doi: 10.3347/kjp.2010.48.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Miro G, Hernandez L, Montoya A, Arranz-Solis D, Dado D, Rojo-Montejo S, Mendoza-Ibarra JA, Ortega-Mora LM, Pedraza-Diaz S. First description of naturally acquired Tritrichomonas foetus infection in a Persian cattery in Spain. Parasitol Res. 2011;109:1151–1154. doi: 10.1007/s00436-011-2359-7. [DOI] [PubMed] [Google Scholar]
- 95.Forshell U, Osterman-Lind E. Chronic diarrhoea caused by Tritrichomonas foetus in the cat. Svensk Veterinärtidning. 2010;62:19–21. [Google Scholar]
- 96.Frey CF, Schild M, Hemphill A, Stunzi P, Muller N, Gottstein B, Burgener IA. Intestinal Tritrichomonas foetus infection in cats in Switzerland detected by in vitro cultivation and PCR. Parasitol Res. 2009;104:783–788. doi: 10.1007/s00436-008-1255-2. [DOI] [PubMed] [Google Scholar]
- 97.Burgener IA, Frey CF, Kook PH, Gottstein B. Tritrichomonas foetus: a new intestinal parasite in Swiss cats. Schweiz Arch Tierheilkd. 2010;151:383–389. doi: 10.1024/0036-7281.151.8.383. [DOI] [PubMed] [Google Scholar]
- 98.Gunn-Moore D, Tennant B. Tritrichomonas foetus diarrhoea in cats. Vet Rec. 2007;160:850–851. doi: 10.1136/vr.160.24.850-b. [DOI] [PubMed] [Google Scholar]


