Abstract
Three cases of inoperable secondary spontaneous pneumothorax were diagnosed in patients with chronic obstructive pulmonary disease. Two cases initially underwent bronchial occlusion with endobronchial Watanabe spigot (EWS), while one underwent talc poudrage with pleuroscopy. As air leaks were not stopped completely in all cases with the initial procedures, we performed additional interventional treatments: pleuroscopic talc poudrage in cases when bronchial occlusion was performed first; and bronchial occlusion with EWS for a case that initially underwent talc pleurodesis. The air leaks ceased in all cases without complication. We successfully removed chest tubes 2–10 days after secondary procedure, which was 10–23 days after the first procedure. The combination of talc pleurodesis and bronchial occlusion with EWS, when a single, initial interventional treatment fails, can be considered in cases of intractable, inoperable secondary pneumothorax.
Keywords: Chronic obstructive pulmonary disease, endobronchial Watanabe spigot, pleuroscopy, secondary spontaneous pneumothorax, talc poudrage
Introduction
Secondary spontaneous pneumothorax (SSP) in patients with underlying diseases such as chronic obstructive pulmonary disease (COPD) can be life threatening. While surgery is recommended to manage SSP [1], we sometimes encounter cases that are considered inoperable because of low pulmonary function. For these cases, interventional treatments such as thoracoscopic talc poudrage [2] and bronchial occlusion with endobronchial Watanabe spigots (EWS) [3] have been reported as effective. However, performing bronchial occlusion or talc pleurodesis alone can be ineffective. For such intractable SSP cases, we recently performed additional secondary treatments: pleuroscopic talc poudrage in cases after initial bronchial occlusion; and bronchial occlusion with EWS for cases after initial talc pleurodesis. We herein report three cases of intractable, inoperable SSP with severe COPD that were successfully managed with secondary interventional treatment.
Case Reports
Case 1
A 77-year-old man with COPD complaining of severe dyspnea was transferred to our institution. Chest radiograph showed pneumothorax in the right lower lung field (Fig. 1A). A chest tube was immediately inserted and attached to a water seal drainage system. Although suction at −15 cmH2O was commenced, the lung did not fully re-expand. The patient was deemed inoperable because of low pulmonary function with a forced expiratory volume in 1 sec (FEV1) of 1010 mL prior to pneumothorax. As the air leaks persisted, pleuroscopy was performed (Fig. 2A) for talc pleurodesis on day 14. Under direct visualization, 2 g of sterile talc (Steritalc®; Novatech, La Ciotat, France) was insufflated using a catheter (SG-201C; Olympus, Tokyo, Japan) and talc atomizer (Richard Wolf, Knittlingen, Germany) through a pleuroscope (LTF-260; Olympus) (Fig. 2B, C) as previously described [4]. After talc pleurodesis followed by suction at −15 cmH2O, the right lung was re-expanded (Fig. 1B), but the air leaks persisted. Bronchoscopy was then performed on day 27. Balloon test to block each bronchus using a balloon catheter (B5/B7-2C; Olympus) was unable to show any changes in the air leak. Subsequently, we performed bronchography using Iopamidol (Hikari Pharmaceutical, Tokyo, Japan) as contrast, and confirmed the leak to the pleural space through the right B1a under fluoroscopy. Next, we occluded the right B1a using a small EWS (S-EWS) (Novatech, La Ciotat, France) and a medium EWS (M-EWS) (Fig. 2D, E). The chest tube was connected to −15 cmH2O of suction, and the air leaks ceased on day 34 and the chest tube was removed on day 37. There were no complications for procedures. Chest radiograph taken 1 month after chest tube removal showed complete lung re-expansion (Fig. 1C). Spigots did not migrate and were not removed. The patient has maintained his general condition for over 1 year.
Figure 1.

Chest radiographs for case 1. Chest radiograph on admission showed pneumothorax in the right lower lung field (arrowheads) (A). After talc poudrage, the right lung was re-expanded (B). Chest radiograph taken 1 month after chest tube removal followed by bronchial occlusion with endobronchial Watanabe spigot (EWS) to the right B1a (arrows) showed complete lung re-expansion (C).
Figure 2.
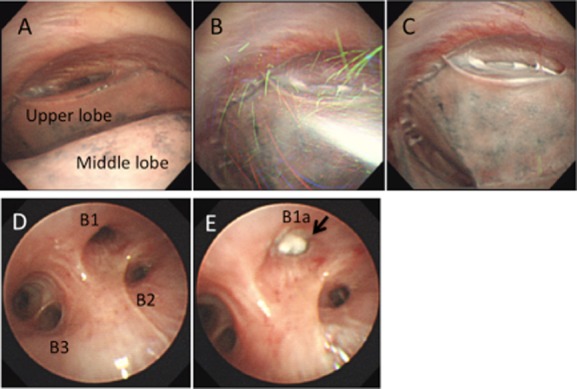
Endoscopic images for case 1. Pleuroscopy before talc poudrage revealed the right upper lobe was adhered to the chest wall (A). Talc was insufflated pleuroscopically under visualization (B). At the end of the procedure, talc was well distributed on the pleura (C). Bronchoscopic image of the right upper bronchus (D). Right B1a was occluded with endobronchial Watanabe spigot (EWS) (arrow) (E).
Case 2
A 62-year-old man with severe COPD was referred to the emergency department of our institution because of right tension pneumothorax. The patient was considered inoperable by thoracic surgeons. As the air leaks persisted under −15 cmH2O of suction, bronchoscopy was performed on day 38. Balloon test at the right B1 and B3 markedly reduced the air leak, and subsequently, bronchography confirmed these affected bronchi. We then occluded the right B1a with an M-EWS, B1b with an S-EWS, B3a with an S-EWS, and B3b with an M-EWS. After bronchial occlusion, air leaks were reduced, but still persisted confirmed by water seal drainage. Next, we performed pleuroscopy on day 51 and administered 2 g of sterile talc visually through a catheter. Immediately after talc insufflation, the patient complained of chest pain requiring 50 mg of diclofenac. Suction at −20 cmH2O was commenced and the air leaks ceased on day 54. The chest tube was then removed on day 57. Spigots were fixed and have not migrated. Recurrence has not occurred for over 2 years.
Case 3
A 64-year-old man having severe COPD with an FEV1 of 740 mL developed left pneumothorax. As air leaks persisted despite repetitive pleurodesis by blood patch, he was referred to our institution on day 38. The patient was deemed inoperable because of his low pulmonary function. As the air leaks persisted under −15 cmH2O of suction, we first performed bronchoscopy on day 51. Balloon test revealed the air leak decreased after blocking the left B3b, B3c, and B4b, and bronchography confirmed these affected bronchi. We occluded the left B3c with a large EWS (L-EWS), B3b with two M-EWS, and B4b with an L-EWS. The air leaks were markedly reduced, but still persisted under −15 cmH2O of suction. Therefore, on day 59, we performed talc poudrage with 2 g of sterile talc using a catheter under pleuroscopy, which caused chest pain requiring 15 mg of pentazocine. With suction at −20 cmH2O after pleuroscopy, the air leaks stopped on day 60, and the chest tube was removed on day 61. Eleven days after chest tube removal, the patient developed pneumonia in the left upper lobe, which was considered related to EWS placement. As pneumonia was easily treated with oral antibiotics and the spigots did not migrate, we did not remove them. Pneumothorax has not recurred for over 1 year.
Discussion
For the management of inoperable SSP, interventional treatments are reported as effective 1–3. However, when the first treatment fails, we have to consider whether to wait until air leaks cease by tube thoracostomy and suction only, or to perform subsequent procedures. For the present cases, we added secondary procedures to the initial treatment, which were successful in all cases. We consider effective treatment was possible using two approaches; bronchial occlusion internally and talc pleurodesis externally. Thus, after a single interventional treatment fails, the combination of talc pleurodesis and bronchial occlusion with EWS is considered promising for intractable, inoperable SSP.
Similar to endobronchial valves [5], EWS is a bronchial blocker that is placed under bronchoscopy. Cases showing complete stoppage of air leaks only by bronchial occlusion remain approximately 40–50% [3], [5] because of collateral ventilation. To achieve optimal results for bronchial occlusion, we determine the affected bronchi by bronchography in addition to balloon test [3]. However, in cases when bronchial occlusion is ineffective despite using dedicated methods, pleurodesis using talc, for example, should be considered as an additional procedure to overcome collateral ventilation.
For talc poudrage, we previously reported a catheter technique with pleuroscopy under local anesthesia to insufflate talc visually from a single port [4]. This technique was acceptable even in elderly patients or those with relatively low performance status. Many patients with intractable SSP have poor general condition and this method should be considered for treatment. Two of the presented cases complained of chest pain requiring analgesics after undergoing talc poudrage. Pleural anesthesia using lidocaine [6] can be used to prevent pain.
Acknowledgments
The authors are indebted to Mr. Jason Tonge for his English review of this article.
Disclosure Statements
No conflict of interest declared.
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
References
- MacDuff A, Arnold A. Harvey J. Management of spontaneous pneumorhorax: British Thoracic Society pleural disease guideline 2010. Thorax. 2010;65(Suppl. 2):ii18–ii31. doi: 10.1136/thx.2010.136986. [DOI] [PubMed] [Google Scholar]
- Lee P, Yap WS, Pek WY. An audit of medical thoracoscopy and talc poudrage for pneumothorax prevention in advanced COPD. Chest. 2004;125:1315–1320. doi: 10.1378/chest.125.4.1315. [DOI] [PubMed] [Google Scholar]
- Watanabe Y, Matsuo K, Tamaoki A. Bronchial occlusion with endobronchial Watanabe spigot. J. Bronchol. 2003;10:264–267. [Google Scholar]
- Ishida A, Nakamura M, Miyazawa T. Novel approach for talc pleurodesis by dedicated catheter through flexi-rigid thoracoscope under local anesthesia. Interact. Cardiovasc. Thorac. Surg. 2011;12:667–670. doi: 10.1510/icvts.2010.263137. [DOI] [PubMed] [Google Scholar]
- Travaline JM, McKenna RJ, Jr, De Giacomo T. Treatment of persistent pulmonary air leaks using endobronchial valves. Chest. 2009;136:355–360. doi: 10.1378/chest.08-2389. [DOI] [PubMed] [Google Scholar]
- Lee P. Colt HG. A spray catheter technique for pleural anesthesia: a novel method for pain control before talc poudrage. Anesth. Analg. 2007;104:198–200. doi: 10.1213/01.ane.0000249046.02025.ef. [DOI] [PubMed] [Google Scholar]


