Abstract
Breast magnetic resonance imaging (MRI) now has an accepted place in screening younger women at high risk of breast cancer, and is increasingly used in a number of other settings including assessment of response to neo-adjuvant therapy and local staging of cancer. Although the evidence for its general use in these settings is very limited, in highly selected patients, especially where discordance with conventional measurements occurs, MRI can have a place in assessing extent of disease, both whether operable and how operable, and guiding surgery. These scenarios and future indications and alternative technologies are explored in this paper.
Keywords: Breast cancer, magnetic resonance imaging, neo-adjuvant chemotherapy
Introduction
It has been 36 years since Damadian first described the use of nuclear magnetic resonance imaging (MRI) of the breast.1 Initial images were disappointing, but intravenous contrast2 and faster sequences have changed this. MRI is now standard for screening women at high risk of breast cancer (BC).3 However other indications remain controversial and in many countries, including Australia, are not funded by government or health insurers. Key to the developing use of MRI has been the development of MRI-guided biopsy techniques.4
The American College of Radiology Breast Imaging and Reporting Data System (BI-RADS)5 provides a standardised approach to nomenclature and interpretation of breast MRI. The American College of Radiology Imaging Network (ACRIN) 6667 Trial6 and European Society of Breast Imaging7 provide standards for breast MRI equipment, protocols and reading.
The false mantra ‘breast MRI has high sensitivity but low specificity’8 is now challenged with sensitivity over 90% and specificity 97%.9 A 2012 systematic review10 evaluated the diagnostic accuracy of MRI in detecting additional lesions found a positive predictive value of 67% as did Houssami et al.11
In Australia breast MRI is currently used in screening young women at high risk of developing BC, and widely for other non-Medicare rebatable indications. This paper will explore these indications and provide cautions to help limit inappropriate use.
MRI as a Screening Tool
In 2009, the Australian Government-funded breast MRI in the diagnosis of breast cancer in asymptomatic women with a high risk of developing breast cancer when used as part of an organised surveillance program. The criteria for screening provide for an annual MRI for women under 50 with a known mutation predisposing to BC or ‘National Breast and Ovarian Cancer Centre (NBOCC) Category 3’ risk (>20% lifetime risk), plus 6 month follow-up MRI if indicated or MR-guided biopsy.
However, we have sparse data on MRI screening sensitivity, specificity, positive or negative predictive values, recall rates and interval cancer rates. Information from international studies (not from real life screening programs) suggest these parameters are at least comparable to population screening programmes of women >50 years, and although there is some evidence for down staging of tumours at presentation, any improvement in BC-specific survival data is yet to be seen.12–17
But how should we define ‘high risk’? NBOCC Category 3 includes women in whose family breast or ovarian cancer (OC) occurred in at least three relatives on one side of the family, or breast or OC in at least two relatives including one with bilateral BC, BC <40 years, OC<50 years, BC and OC in one individual, a relative with BC<45 years plus a sarcoma <45 years, male BC or if the family have Ashkenazi Jewish heritage.
Throughout the world, criteria for inclusion in MRI screening programmes18 vary depending on both model of risk used and the population it is used in. Ozanne et al.19 showed using three common models there was only 5% agreement on who was at high risk! Thus we need to develop modern validated models of risk to decide who may benefit most from MRI.
Still to be determined is also the best programme of screening within a multidisciplinary high-risk management programme – most guidelines recommend starting at 25–30 years or 10 years before the youngest relative developed BC. Current provisions only rebate MRI in women under 50, but clearly for some this arbitrary age limit may not be applicable. Some clinics suggest alternate 6 monthly MRI with mammogram.20,21
A group that merits special mention is women treated with chest irradiation at a young age. Current guidelines recommend breast MRI beginning 8–10 years after treatment, and combined with mammography has a sensitivity of 94%.22
It is also recognised that women with a prior history of some benign lesions have a significant increased BC risk – for lobular carcinoma in situ (LCIS) similar in magnitude to gene carriers. It is not known if the addition of MRI to mammographic and/or ultrasound (US) screening improves outcomes for these women, or in a selected group who are very young and with mammographically dense breasts.
MRI in Assessing Disease Extent and Guiding Surgery
Breast-conserving surgery is now offered to over 70% of Australian women (www.breastsurganz.com), however, in about 25% of cases conventional assessment (usually mammogram, US and clinical examination) under-estimates the extent of the cancer and if further surgery is necessary.23 We have recently shown (H. Ballal, D. Taylor, A. Bourke, B. Latham, P. Riley, J. Bourke, D. Dissanyake and C. Saunders C, under review) that this is more common in the presence of extensive ductal carcinoma in situ (DCIS) and multifocal disease.
There is clearly a need for more accurate techniques for defining the extent of malignancy, guiding surgery to achieve clear margins in one operation and optimising cosmetic outcome. It is unclear if MRI can improve this.24 There is little evidence pre-operative MRI reduces the risk of reoperation but it may increase unnecessary biopsies or additional imaging, and increase the likelihood of mastectomy, at least as an initial operation, although final mastectomy rate is not increased.25 MRI may also increase the likelihood of contralateral mastectomy, although this is unclear as the population of women who choose contralateral mastectomy is often similar to those who wish to have or are recommended an MRI. There is a small risk MRI may delay surgery, and increase patient anxiety, but, most importantly, there is little evidence it reduces local BC recurrence. The reasons for this are unclear, perhaps the complexity of translating a 2D image acquired prone to a 3D surgical field; or perhaps MRI just finds microscopic disease that is adequately treated with radiotherapy and systemic therapy.
More plausible perhaps is that the randomised studies to date have taken fairly unselected populations of women scheduled for breast-conserving surgery (BCS) and looked at outcomes in those having additional MRI to those not. The comparative effectiveness of MRI in BC (COMICE) trial26 and MONET trial27 are the largest of these.
COMICE concluded addition of MRI to conventional triple assessment did not reduce reoperation rate, (odds ratio 0.96, 95% CI 0.75–1.24; P = 0.77) MONET demonstrated a higher re-excision rate in the MRI group (18/53, 34%), versus the control group (6/50, 12%), P = 0.008, although the rate of conversion to mastectomy did not differ significantly. This is difficult to explain, given that baseline characteristics were comparable between groups, as was the rate of primary BCS. But median volumes of excised tissue were lower in the MRI group and the authors postulated the higher rate of re-excision was due to surgeons being inappropriately reassured by small lesion size on MRI. This suggests that the sensitivity of MRI in showing extent of in situ disease is less than standard imaging, in contrast to others28,29 where MRI better depicted the extent of than mammography.
A more recent randomised controlled trial (RCT) of 440 women, selected by young age alone25 found the MRI group had higher BCS planned and a change to mastectomy occurred in 15%, but a lower overall re-operation rate in the MRI group (5% vs. 15%) (P < 0.0001). There was no difference in overall mastectomy rate despite initial higher mastectomy rate in the MRI group.
Non-randomised studies report mixed results – one recent study of patients planned for BCS having pre-operative MRI, compared to 119 controls with no MRI 1 year earlier, found MRI changed the surgical plan to more extensive surgery in 34%. However, significantly fewer MRI patients had positive resection margins (15.8% vs. 29.3%; P < 0.01) and patients in the study group underwent significantly fewer reoperations compared with the historical control group (18.9% vs. 37.4%; P < 0.01).30
Another retrospective series at Memorial Sloan Kettering31 suggests, compared to matched controls, patients having MRI had identical rates of final negative margins although fewer in the MRI group needed re-excision (29% vs. 45%; P = 0.02). There was no significant difference in locoregional recurrence (P = 0.33) or disease-free survival (P = 0.73), however, those referred for MRI were more likely to have extremely dense breasts (28% vs. 6%; P < 0.0001) and mammographically occult cancer (24% vs. 9%; P = 0.0003) – perhaps making this a more ‘real life’ study.
A local unpublished study in Western Australia attempted to assess if the conventional assessment criteria for BCS would be altered by pre-operative MRI. In 50 women (61 cancers) apparently suitable for breast conservation on conventional assessment, MRI was undertaken with the surgeon blind to the results, and both compared to final histopathology. MRI would have correctly predicted 11 of 13 cases requiring mastectomy, 2 of 3 cases requiring re-excision and identified two contralateral cancers not seen on conventional imaging. Moreover MRI would have identified 15 of 18 patients who required more extensive surgery than predicted by conventional assessment. MRI proved most accurate in younger women and those with lobular cancer.
Evidence for MRI Effectiveness with Discrepancy in Conventional Imaging – Selected Patients
There is considerable non-randomised evidence that pre-operative MRI can be more useful in selected groups of patients. Weinstein showed in invasive lobular cancer that MRI shows disease extent more accurately than mammography (85% vs. 32%)32 and MRI changes management in up to 50% of patients.33 Mann showed MRI may decrease re-excision rate of lobular cancers (27% vs. 9%; P = 0.010), and lower final mastectomy rate (48 vs. 59%; P = 0.098).34
Very dense breasts often prove challenging, however, evidence that MRI performs better than conventional imaging in not only better defining cancers but leading to better outcomes is sparse.31
Another situation where MRI often proves useful is occult malignancy. A meta-analysis showed a 74% breast lesion detection rate for MRI with 90% sensitivity but 31% specificity.35 This may allow identification of small lesions and BCS for women who would otherwise undergo mastectomy.
Some studies suggest MRI is probably most accurate in high-grade tumours, performs better than mammography, and is thus complementary, in younger women.36,37 One author nicely describes MRI as a ‘problem solving tool’.38
Onco-Plastic Surgery
A recent but rapidly growing trend is for onco-plastic surgery, safely removing the tumour with optimisation of cosmetic outcomes. Accurately defining the size and geographical distribution of the cancer greatly assists this surgery, and although this is usually adequately done by mammogram and US, MRI may prove useful for surgical planning.
Is MRI Best for Assessing Response to Chemotherapy?
Imaging is used both during neo-adjuvant chemotherapy (NAC) to predict response and possibly allow change of therapy, and after NAC to assess if BCS is possible. International guidelines recommend MRI for these purposes, and most clinical trials mandate MRI at least twice during neo-adjuvant treatment.
Evidence suggests MRI performs better than mammography39–41 but there are no direct studies comparing it to US – which may be almost as good.42 Our own experience suggests MRI may overestimate residual tumour size due to rim enhancement, scattered nodules or fibrosis. US is not good at measuring residual DCIS which needs to be assessed carefully. MRI technology such as diffusion-weighted imaging MRI, which gives information on cell membrane integrity, may improve accuracy.43
Determining suitability for breast radiotherapy
For women with low-risk BC, partial breast irradiation provides similar local control and possibly better survival than whole breast irradiation after BCS.44 However studies to date have not mandated MRI to assess suitability for BCS.45 Using MRI as a guide for whom radiotherapy may be safely omitted is the subject of the PROSPECT trial (https://www.anzbctg.org/clinical-trials/anz1002/prospect).
For women with low-risk BC, partial breast irradiation provides similar local control and possibly better survival than whole breast irradiation after BCS.44 However studies to date have not mandated MRI to assess suitability for BCS.45 Using MRI as a guide for whom radiotherapy may be safely omitted is the subject of the PROSPECT trial (https://www.anzbctg.org/clinical-trials/anz1002/prospect).
Breast MRI in Pregnancy and Lactation
There are46 a lack of data demonstrating efficacy of MRI during pregnancy and safety concerns about gadolinium, plus difficulty positioning the pregnant patient prone. In lactating patients contrast-enhanced MRI may be performed safely, but increased background enhancement make it difficult to differentiate lactational changes from suspicious findings.47
Given that only a minute percentage of gadolinium-based contrast medium that is excreted into breast milk is absorbed by the infant's gut, available data suggest it is safe for the mother and infant to continue breast-feeding after receiving such an agent.48
Other Potential Indications
In our practice up to 30% of patients have close margins at initial BCS. MRI may prove useful to assess extent of residual disease post-op allowing mapping for further BCS. No evidence exists to compare this with careful post-operative US.
Breast MRI has been used to assess the contralateral breast for occult malignancy, in particular those with a high risk of having a genetic mutation.
The role for follow-up after BC using MRI remains unclear – for detecting local recurrence or new lesions. It seems intuitive that in women whose first cancer was occult on conventional imaging it may be a useful tool but evidence is anecdotal to date. However, in young women with a strong family history, or those who have a proven gene mutation, it would seem a reasonable follow-up option.
Use of MRI in Clinical Practice
There are no data in Australian practice about the use of MRI in local staging of cancer. A United States survey of breast surgeons49 queried routine MRI use in specific clinical scenarios and reported higher rates of MRI use in high-volume and specialised surgeons, and private practice. There was greater routine MRI use in the setting of extreme mammographic density (87.9%), strong family history of BC (73.4%), and invasive lobular carcinoma (69.4%).
More than 40% of American women will have an MRI at time of diagnosis of BC. In Australia it appears that pre-operative MRI is mostly used in the context of multidisciplinary breast teams on a case-by-case basis, to assess disease extent or response to NAC. But there is no rebate for this, thus it is either performed in public hospitals or the cost is passed on to the patient.
But there is the potential for using MRI to improve clinical outcomes for selected women diagnosed with BC. The challenge will be to prove its utility in a carefully designed clinical trial. Meanwhile we continue to accrue experience and low-level evidence (Figure1).
Figure 1.
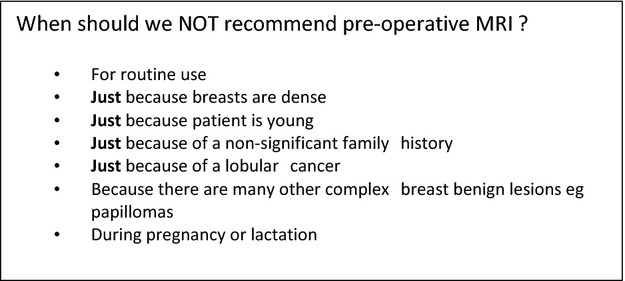
Who does not need magnetic resonance imaging (MRI).
Where to From Here?
A recent application to the Australian Medical Services Advisory Committee for MRI follow-up screening for women <50 with prior cancer was not supported. However, another application for MRI to be used to stage local cancers with discrepancy in conventional staging and to assess response to NAC is still awaiting an outcome.
Advances in Breast MRI and Development of Newer and Possibly Better Technologies
Future advances in diffusion-weighted and diffusion tensor imaging, MRI spectroscopy and Quantitative Perfusion Imaging50–53 may mean breast MRI can be performed without IV contrast injection,54 and with improved specificity and accuracy.
MRI may prove important in predicting prognosis52 and response to neo-adjuvant treatment. Contrast enhanced spectral mammography (CESM) is able to show areas of tumour neoangiogenesis. Sensitivity and specificity are significantly better than standard mammography with or without US55 and while CESM is not as sensitive as MRI, studies have shown better specificity56 and with lower cost, higher accessibility, shorter examination and reading times, fewer contra-indications and better patient tolerance than MRI.57
Conclusions
In highly selected patients, MRI as part of a multi-disciplinary work-up by an experienced team can have a place in assessing extent of disease, whether operable and how operable, and guiding surgery. This should be considered if discordance with conventional measurements occurs, perhaps especially in younger women with lobular cancer and/or increased breast density. MRI can be useful in the diagnosis of occult malignancy, in assessing response to neo-adjuvant therapy and in follow-up of very high-risk women. CESM may be an alternative, particularly for those women who cannot tolerate MRI.
Conflict of Interest
The authors declare no conflict of interest.
References
- Goldsmith M, Koutcher JA, Damadian R. NMR in cancer, XIII: application of the NMR malignancy index to human mammary tumours. Br J Cancer. 1978;38:547–54. doi: 10.1038/bjc.1978.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heywang SH, Hahn D, Schmidt H, Krischke I, Eiermann W, Bassermann R, Lissner J. MR imaging of the breast using gadolinium-DTPA. J Comput Assist Tomogr. 1986;10:199–204. doi: 10.1097/00004728-198603000-00005. [DOI] [PubMed] [Google Scholar]
- The Department of Health Australia. 2013. Department of Health Australia Breast magnetic resonance imaging (MRI) questions and answers [cited 2014 Nov 25]. Available from: http://health.gov.au/internet/main/publishing.nsf/Content/pathol-di-mri-breastmriqa.
- Heywang-Kobrunner SH, Sinnatamby R, Lebeau A, Lebrecht A, Britton PD, Schreer I Consensus Group. Interdisciplinary consensus on the uses and technique of MR-guided vacuum-assisted breast biopsy (VAB): results of a European consensus meeting. Eur J Radiol. 2009;72:289–94. doi: 10.1016/j.ejrad.2008.07.010. [DOI] [PubMed] [Google Scholar]
- Morris EA, Comstock CE, Lee CH, et al. ACR BI-RADS®. Reston, VA: American College of Radiology; 2013. Magnetic Resonance Imaging. In: ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System. [Google Scholar]
- Lehman CD, Gatsonis C, Kuhl CK, et al. MRI evaluation of the contralateral breast in women with recently diagnosed breast cancer. N Engl J Med. 2007;356:1295–303. doi: 10.1056/NEJMoa065447. [DOI] [PubMed] [Google Scholar]
- Mann RM, Kuhl CK, Kinkel K. Breast MRI: guidelines from the European Society of Breast Imaging. Eur Radiol. 2008;18:1307–18. doi: 10.1007/s00330-008-0863-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters NH, Borel RI, Zuithoff NP, Mali WP, Moons KG, Peeters PH. Meta-analysis of MR imaging in the diagnosis of breast lesions. Radiology. 2008;246:116–24. doi: 10.1148/radiol.2461061298. [DOI] [PubMed] [Google Scholar]
- Sardanelli F, Podo F, Santoro F, et al. Multicenter surveillance of women at high genetic breast cancer risk using mammography, ultrasonography, and contrast-enhanced magnetic resonance imaging (the high breast cancer risk italian 1 study): final results. Invest Radiol. 2011;46:94–105. doi: 10.1097/RLI.0b013e3181f3fcdf. [DOI] [PubMed] [Google Scholar]
- Plana MN, Carreira C, Muriel A, Chiva M, Abraira V, Emparanza JI, Bonfill X, Zamora J. Magnetic resonance imaging in the preoperative assessment of patients with primary breast cancer: systematic review of diagnostic accuracy and meta-analysis. Eur Radiol. 2012;22:26–38. doi: 10.1007/s00330-011-2238-8. [DOI] [PubMed] [Google Scholar]
- Houssami N, Ciatto S, Macaskill P, Lord SJ, Warren RM, Dixon JM, Irwig L. Accuracy and surgical impact of magnetic resonance imaging in breast cancer staging: systematic review and meta-analysis in detection of multifocal and multicentric cancer. J Clin Oncol. 2008;26:3248–58. doi: 10.1200/JCO.2007.15.2108. [DOI] [PubMed] [Google Scholar]
- Kriege M, Brekelmans CT, Boetes C, et al. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004;351:427–37. doi: 10.1056/NEJMoa031759. [DOI] [PubMed] [Google Scholar]
- Kuhl CK, Schrading S, Leutner CC, Morakkabati-Spitz N, Wardelmann E, Fimmers R, Kuhn W, Schild HH. Mammography, breast ultrasound, and magnetic resonance imaging for surveillance of women at high familial risk for breast cancer. J Clin Oncol. 2005;23:8469–76. doi: 10.1200/JCO.2004.00.4960. [DOI] [PubMed] [Google Scholar]
- Liberman L. Breast cancer screening with MRI – what are the data for patients at high risk? N Engl J Med. 2004;351:497–500. doi: 10.1056/NEJMe048117. [DOI] [PubMed] [Google Scholar]
- Leach MO, Boggis CR, Dixon AK, et al. Screening with magnetic resonance imaging and mammography of a UK population at high familial risk of breast cancer: a prospective multicentre cohort study (MARIBS) Lancet. 2005;365:1769–78. doi: 10.1016/S0140-6736(05)66481-1. [DOI] [PubMed] [Google Scholar]
- Podo F, Sardanelli F, Canese R, et al. The Italian multi-centre project on evaluation of MRI and other imaging modalities in early detection of breast cancer in subjects at high genetic risk. J Exp Clin Cancer Res. 2002;21(Suppl. 3):115–24. [PubMed] [Google Scholar]
- Stoutjesdijk MJ, Boetes C, Jager GJ, et al. Magnetic resonance imaging and mammography in women with a hereditary risk of breast cancer. J Natl Cancer Inst. 2001;93:1095–102. doi: 10.1093/jnci/93.14.1095. [DOI] [PubMed] [Google Scholar]
- Warner E, Plewes DB, Hill KA, et al. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA. 2004;292:1317–25. doi: 10.1001/jama.292.11.1317. [DOI] [PubMed] [Google Scholar]
- Ozanne EM, Drohan B, Bosinoff P, et al. Which risk model to use? Clinical implications of the ACS MRI screening guidelines. Cancer Epidemiol Biomarkers Prev. 2013;22:146–9. doi: 10.1158/1055-9965.EPI-12-0570. [DOI] [PubMed] [Google Scholar]
- Cott CJ, Lee JM, Gilmore ME, Kong CY, Lowry KP, Halpern EF, McMahon PM, Ryan PD, Gazelle GS. Cost-effectiveness of alternating magnetic resonance imaging and digital mammography screening in BRCA1 and BRCA2 gene mutation carriers. Cancer. 2013;119:1266–76. doi: 10.1002/cncr.27864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry KP, Lee JM, Kong CY, et al. Annual screening strategies in BRCA1 and BRCA2 gene mutation carriers: a comparative effectiveness analysis. Cancer. 2012;118:2021–30. doi: 10.1002/cncr.26424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng AK, Garber JE, Diller LR, Birdwell RL, Feng Y, Neuberg DS, Silver B, Fisher DC, Marcus KJ, Mauch PM. Prospective study of the efficacy of breast magnetic resonance imaging and mammographic screening in survivors of Hodgkin lymphoma. J Clin Oncol. 2013;31:2282–8. doi: 10.1200/JCO.2012.46.5732. [DOI] [PubMed] [Google Scholar]
- Lovrics PJ, Cornacchi SD, Farrokhyar F, Garnett A, Chen V, Franic S, Simunovic M. The relationship between surgical factors and margin status after breast-conservation surgery for early stage breast cancer. Am J Surg. 2009;197:740–6. doi: 10.1016/j.amjsurg.2008.03.007. [DOI] [PubMed] [Google Scholar]
- Jatoi I, Benson JR. The case against routine preoperative breast MRI. Future Oncol. 2013;9:347–53. doi: 10.2217/fon.12.186. [DOI] [PubMed] [Google Scholar]
- Gonzalez V, Sandelin K, Karlsson A, Aberg W, Lofgren L, Iliescu G, Eriksson S, Arver B. Preoperative MRI of the breast (POMB) influences primary treatment in breast cancer: a prospective, randomized, multicenter study. World J Surg. 2014;38:1685–93. doi: 10.1007/s00268-014-2605-0. [DOI] [PubMed] [Google Scholar]
- Turnbull L, Brown S, Harvey I, Olivier C, Drew P, Napp V, Hanby A, Brown J. Comparative effectiveness of MRI in breast cancer (COMICE) trial: a randomised controlled trial. Lancet. 2010;375:563–71. doi: 10.1016/S0140-6736(09)62070-5. [DOI] [PubMed] [Google Scholar]
- Peters NH, van Esser S, van den Bosch MA, et al. Preoperative MRI and surgical management in patients with nonpalpable breast cancer: the MONET – randomised controlled trial. Eur J Cancer. 2011;47:879–86. doi: 10.1016/j.ejca.2010.11.035. [DOI] [PubMed] [Google Scholar]
- Kim DY, Moon WK, Cho N, Ko ES, Yang SK, Park JS, Kim SM, Park IA, Cha JH, Lee EH. MRI of the breast for the detection and assessment of the size of ductal carcinoma in situ. Korean J Radiol. 2007;8:32–9. doi: 10.3348/kjr.2007.8.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhl CK, Schrading S, Bieling HB, Wardelmann E, Leutner CC, Koenig R, Kuhn W, Schild HH. MRI for diagnosis of pure ductal carcinoma in situ: a prospective observational study. Lancet. 2007;370:485–92. doi: 10.1016/S0140-6736(07)61232-X. [DOI] [PubMed] [Google Scholar]
- Obdeijn IM, Tilanus-Linthorst MM, Spronk S, van Deurzen CH, de Monye C, Hunink MG, Menke MB. Preoperative breast MRI can reduce the rate of tumor-positive resection margins and reoperations in patients undergoing breast-conserving surgery. Am J Roentgenol. 2013;200:304–10. doi: 10.2214/AJR.12.9185. [DOI] [PubMed] [Google Scholar]
- Sung JS, Li J, Da Costa G, Patil S, Van Zee KJ, Dershaw DD, Morris EA. Preoperative breast MRI for early-stage breast cancer: effect on surgical and long-term outcomes. Am J Roentgenol. 2014;202:1376–82. doi: 10.2214/AJR.13.11355. [DOI] [PubMed] [Google Scholar]
- Weinstein SP, Orel SG, Heller R, Reynolds C, Czerniecki B, Solin LJ, Schnall M. MR imaging of the breast in patients with invasive lobular carcinoma. Am J Roentgenol. 2001;176:399–406. doi: 10.2214/ajr.176.2.1760399. [DOI] [PubMed] [Google Scholar]
- Rodenko GN, Harms SE, Pruneda JM, Farrell RS, Jr, Evans WP, Copit DS, Krakos PA, Flamig DP. MR imaging in the management before surgery of lobular carcinoma of the breast: correlation with pathology. Am J Roentgenol. 1996;167:1415–9. doi: 10.2214/ajr.167.6.8956569. [DOI] [PubMed] [Google Scholar]
- Mann RM, Loo CE, Wobbes T, Bult P, Barentsz JO, Gilhuijs KG, Boetes C. The impact of preoperative breast MRI on the re-excision rate in invasive lobular carcinoma of the breast. Breast Cancer Res Treat. 2010;119:415–22. doi: 10.1007/s10549-009-0616-6. [DOI] [PubMed] [Google Scholar]
- de Bresser J, de Vos B, van der Ent F, Hulsewe K. Breast MRI in clinically and mammographically occult breast cancer presenting with an axillary metastasis: a systematic review. Eur J Surg Oncol. 2010;36:114–9. doi: 10.1016/j.ejso.2009.09.007. [DOI] [PubMed] [Google Scholar]
- Deurloo EE, Peterse JL, Rutgers EJ, Besnard AP, Muller SH, Gilhuijs KG. Additional breast lesions in patients eligible for breast-conserving therapy by MRI: impact on preoperative management and potential benefit of computerised analysis. Eur J Cancer. 2005;41:1393–401. doi: 10.1016/j.ejca.2005.03.017. [DOI] [PubMed] [Google Scholar]
- Pengel KE, Loo CE, Teertstra HJ, Muller SH, Wesseling J, Peterse JL, Bartelink H, Rutgers EJ, Gilhuijs KG. The impact of preoperative MRI on breast-conserving surgery of invasive cancer: a comparative cohort study. Breast Cancer Res Treat. 2009;116:161–9. doi: 10.1007/s10549-008-0182-3. [DOI] [PubMed] [Google Scholar]
- Yau EJ, Gutierrez RL, DeMartini WB, Eby PR, Peacock S, Lehman CD. The utility of breast MRI as a problem-solving tool. Breast J. 2011;17:273–80. doi: 10.1111/j.1524-4741.2011.01075.x. [DOI] [PubMed] [Google Scholar]
- Warren RM, Bobrow LG, Earl HM, Britton PD, Gopalan D, Purushotham AD, Wishart GC, Benson JR, Hollingworth W. Can breast MRI help in the management of women with breast cancer treated by neoadjuvant chemotherapy? Br J Cancer. 2004;90:1349–60. doi: 10.1038/sj.bjc.6601710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati R, Minami CA, Gornbein JA, Debruhl N, Chung D, Chang HR. Accuracy of clinical evaluation of locally advanced breast cancer in patients receiving neoadjuvant chemotherapy. Cancer. 2009;115:1194–202. doi: 10.1002/cncr.24154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Im YH, Han BK, et al. Accuracy of MRI for estimating residual tumor size after neoadjuvant chemotherapy in locally advanced breast cancer: relation to response patterns on MRI. Acta Oncol. 2007;46:996–1003. doi: 10.1080/02841860701373587. [DOI] [PubMed] [Google Scholar]
- Marinovich ML, Houssami N, Macaskill P, Sardanelli F, Irwig L, Mamounas EP, von Minckwitz G, Brennan ME, Ciatto S. Meta-analysis of magnetic resonance imaging in detecting residual breast cancer after neoadjuvant therapy. J Natl Cancer Inst. 2013;105:321–33. doi: 10.1093/jnci/djs528. [DOI] [PubMed] [Google Scholar]
- Woodhams R, Kakita S, Hata H, Iwabuchi K, Kuranami M, Gautam S, Hatabu H, Kan S, Mountford C. Identification of residual breast carcinoma following neoadjuvant chemotherapy: diffusion-weighted imaging – comparison with contrast-enhanced MR imaging and pathologic findings. Radiology. 2010;254:357–66. doi: 10.1148/radiol.2542090405. [DOI] [PubMed] [Google Scholar]
- Vaidya JS, Joseph DJ, Tobias JS, et al. Targeted intraoperative radiotherapy versus whole breast radiotherapy for breast cancer (TARGIT-A trial): an international, prospective, randomised, non-inferiority phase 3 trial. Lancet. 2010;376:91–102. doi: 10.1016/S0140-6736(10)60837-9. [DOI] [PubMed] [Google Scholar]
- Horst KC, Fero KE, Ikeda DM, Daniel BL, Dirbas FM. Defining an optimal role for breast magnetic resonance imaging when evaluating patients otherwise eligible for accelerated partial breast irradiation. Radiother Oncol. 2013;108:220–5. doi: 10.1016/j.radonc.2013.01.019. [DOI] [PubMed] [Google Scholar]
- Loibl S, von Minckwitz G, Gwyn K, et al. Breast carcinoma during pregnancy. International recommendations from an expert meeting. Cancer. 2006;106:237–46. doi: 10.1002/cncr.21610. [DOI] [PubMed] [Google Scholar]
- Vashi R, Hooley R, Butler R, Geisel J, Philpotts L. Breast imaging of the pregnant and lactating patient: imaging modalities and pregnancy-associated breast cancer. Am J Roentgenol. 2013;200:321–8. doi: 10.2214/ajr.12.9814. [DOI] [PubMed] [Google Scholar]
- American College of Radiology. 2013. ACR ACR Manual on Contrast Media version 9. ACR Committee on Drugs and Contrast Media.
- Parker A, Schroen AT, Brenin DR. MRI utilization in newly diagnosed breast cancer: a survey of practicing surgeons. Ann Surg Oncol. 2013;20:2600–6. doi: 10.1245/s10434-013-2934-5. [DOI] [PubMed] [Google Scholar]
- Baltzer PA, Renz DM, Herrmann KH, Dietzel M, Krumbein I, Gajda M, Camara O, Reichenbach JR, Kaiser WA. Diffusion-weighted imaging (DWI) in MR mammography (MRM): clinical comparison of echo planar imaging (EPI) and half-Fourier single-shot turbo spin echo (HASTE) diffusion techniques. Eur Radiol. 2009;19:1612–20. doi: 10.1007/s00330-009-1326-5. [DOI] [PubMed] [Google Scholar]
- Baltzer PA, Schafer A, Dietzel M, Grassel D, Gajda M, Camara O, Kaiser WA. Diffusion tensor magnetic resonance imaging of the breast: a pilot study. Eur Radiol. 2011;21:1–10. doi: 10.1007/s00330-010-1901-9. [DOI] [PubMed] [Google Scholar]
- Baltzer PA, Dietzel M. Breast lesions: diagnosis by using proton MR spectroscopy at 1.5 and 3.0 T – systematic review and meta-analysis. Radiology. 2013;267:735–46. doi: 10.1148/radiol.13121856. [DOI] [PubMed] [Google Scholar]
- Herrmann KH, Baltzer PA, Dietzel M, Krumbein I, Geppert C, Kaiser WA, Reichenbach JR. Resolving arterial phase and temporal enhancement characteristics in DCE MRM at high spatial resolution with TWIST acquisition. J Magn Reson Imaging. 2011;34:973–82. doi: 10.1002/jmri.22689. [DOI] [PubMed] [Google Scholar]
- Trimboli RM, Verardi N, Cartia F, Carbonaro LA, Sardanelli F. Breast cancer detection using double reading of unenhanced MRI including T1-weighted, T2-weighted STIR, and diffusion-weighted imaging: a proof of concept study. Am J Roentgenol. 2014;203:674–81. doi: 10.2214/AJR.13.11816. [DOI] [PubMed] [Google Scholar]
- Dromain C, Thibault F, Diekmann F, Fallenberg EM, Jong RA, Koomen M, Hendrick RE, Tardivon A, Toledano A. Dual-energy contrast-enhanced digital mammography: initial clinical results of a multireader, multicase study. Breast Cancer Res. 2012;14:R94. doi: 10.1186/bcr3210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jochelson MS, Dershaw DD, Sung JS, Heerdt AS, Thornton C, Moskowitz CS, Ferrara J, Morris EA. Bilateral contrast-enhanced dual-energy digital mammography: feasibility and comparison with conventional digital mammography and MR imaging in women with known breast carcinoma. Radiology. 2013;266:743–51. doi: 10.1148/radiol.12121084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitzberger FF, Fallenberg EM, Lawaczeck R, et al. Development of low-dose photon-counting contrast-enhanced tomosynthesis with spectral imaging. Radiology. 2011;259:558–64. doi: 10.1148/radiol.11101682. [DOI] [PubMed] [Google Scholar]


