Abstract
Acute myocarditis can be induced by various concomitant disease processes including infections. Most of these cases are viral in origin; however, bacterial infections are also implicated to a lesser degree. Group A streptococcus is a frequent culprit in bacterial-induced myocarditis. Its diagnosis is suspected by the presence of signs and symptoms of rheumatic fever as established by the Jones criteria. The development and refinement of current diagnostic tools has improved our ability to identify specific pathogens. It has been found that group A streptococcus may be responsible for more cases of infection-induced acute myocarditis than previously thought, and often without the clinical features of rheumatic fever. We present the case of a 43-year-old man hospitalized with chest pain that was initially diagnosed as an acute ST-elevation myocardial infarction. Further evaluation confirmed that his chief complaint was due to acute nonrheumatic streptococcal myocarditis.
Group A streptococcus (GAS) is rarely reported as a causative pathogen of acute myocarditis without clinical features suggestive of rheumatic fever. The incidence of acute myocarditis is estimated to be 1 in 10 cases per 100,000 persons, with acute viral infections accounting for most of the cases of infectious myocarditis (up to 1% to 5% of all cases). No epidemiological data estimating the incidence of GAS-induced myocarditis exist at this time. Myocardial inflammation and damage is thought to be caused by IgG binding proteins produced by GAS antigens that cross-react with cardiac myosin (1). Despite the advent of new laboratory and imaging tools, the diagnosis of acute myocarditis continues to be a challenge due to its wide variety of clinical presentations. We present the case of a 43-year-old man hospitalized with chest pain that was initially diagnosed as an acute ST-elevation myocardial infarction. Further evaluation confirmed that his chief complaint was due to acute nonrheumatic streptococcal myocarditis.
CASE PRESENTATION
A 43-year-old man presented to the hospital complaining of continuous, nonradiating, retrosternal chest pressure. The pain began at rest approximately 18 to 24 hours prior to his arrival. His pain was 6 on a scale of 1 to 10, without alleviating or aggravating factors. Additionally, the patient reported a 3-day history of sore throat, cough, fever, chills, headache, and epigastric pain. The patient had no significant risk factors for cardiovascular disease.
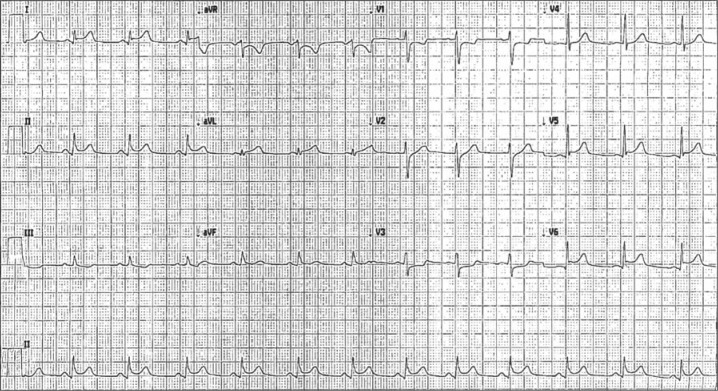
On admission, his electrocardiogram showed a sinus rhythm with a rate of 75 beats per minute and mild ST elevations in leads I, II, AVF, V4, V5, and V6 (Figure 1). Troponin I and creatine kinase-MB levels were found to be elevated at 15.8 ng/mL and 68.6 ng/mL, respectively. A repeat troponin I level was markedly increased at 45.8 ng/mL. Transthoracic echocardiogram demonstrated preserved left ventricular systolic function with an ejection fraction of 55% and no regional wall motion abnormalities. Trivial mitral regurgitation and mild left atrial dilatation were noted. Percutaneous coronary angiography revealed no evidence of obstructive coronary artery disease, and left ventriculography corroborated our echocardiogram findings.
Figure 1.
Sinus rhythm with mild ST elevations in leads I, II, AVF, V4, V5, and V6 suggesting inferolateral acute myocardial infarction.
The patient's white blood cell count was 15.9 × 109 per L and the erythrocyte sedimentation rate was 47 mm/h. The patient reported several instances of elevated oral temperature at home; the highest reading was 102°F. He was afebrile at the time of admission. A rapid streptococcal antigen test was positive. Antistreptolysin O titer (74 IU/mL) and a blood culture were negative. Treatment with amoxicillin and colchicine was initiated. The patient experienced gradual improvement in his symptoms and was discharged 3 days later with complete resolution of his chest pain.
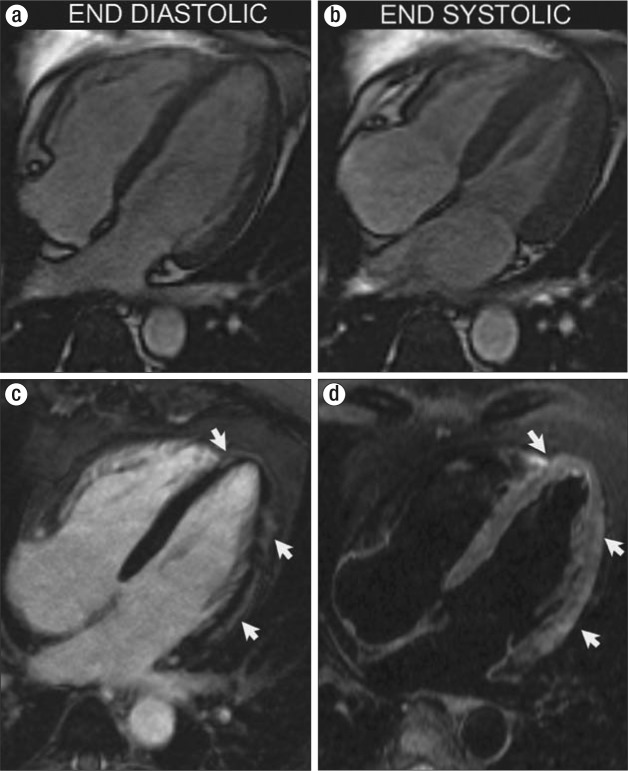
The patient had no further episodes of chest pain, and a repeat electrocardiogram showed improved tracings 7 days after discharge. Tonsillectomy was planned. Cardiac magnetic resonance imaging was performed 17 days after his discharge, showing a pattern of abnormal signal intensity (T2 hyperintensity and delay hyperenhancement) involving the subepicardial myocardium, without evidence of associated left ventricular contractile or functional abnormalities (Figure 2).
Figure 2.
Horizontal long-axis views using steady-state free precession imaging at (a) end-diastolic phase and (b) end-systolic phase demonstrate no evidence of focal or global myocardial contractile abnormalities. (c) A horizontal long-axis, contrast-enhanced inversion recovery sequence demonstrates patchy areas of myocardial enhancement following a subepicardial distribution (arrows), indicative of inflammatory tissue damage. (d) A horizontal long-axis T2-weighted black-blood image demonstrates myocardial edema matching the regions of abnormal enhancement.
DISCUSSION
Current published reports contain extensive evidence linking acute carditis (pericarditis, myocarditis, and valvulitis) with acute rheumatic fever. Acute myocarditis associated with GAS pharyngitis without rheumatic fever symptoms is rare, and its incidence has been increasingly reported since Gore and Saphir first described it in 1947 (2). The rise in reported cases is likely related to its strikingly similar clinical presentation to that of an acute myocardial infarction and the present-day availability of diagnostic tools that make the diagnosis of GAS-induced myocarditis more accurate.
Case series published by Talmon et al (3), Mokabberi et al (4), and Upadhay et al (5) provide a constellation of findings that can be useful to the clinician in making a differential diagnosis (Table 1). A diagnosis of GAS-induced myocarditis is to be suspected in young men with a chief complaint of acute chest pain without significant risk factors for premature cardiovascular disease, particularly with evidence of streptococcal pharyngitis or tonsillitis. Electrocardiogram tracings will most likely show ST-segment elevations in conjunction with elevated cardiac enzymes. Coronary arteries are typically angiographically normal. The most common transthoracic echocardiogram findings are left ventricular wall motion abnormalities, mitral regurgitation, and pericardial effusion.
Table 1.
Three reported case series of acute nonrheumatic streptococcal myocarditis
Cardiac magnetic resonance imaging appears to be the imaging modality of choice for confirmation of the diagnosis; however, it remains largely untested. Mavrogeni et al (6) described the largest series of patients evaluated with cardiac magnetic resonance imaging thus far. Unfortunately, their sample size was small (17 patients), and a correlation between cardiac enzymes and cardiac magnetic resonance imaging could not be made. Positive late gadolinium enhancement was identified in 13 patients. Reimaging 3 months later showed normal results in 14 patients.
Another important consideration is the possibility of recurrent episodes of myocarditis secondary to streptococcal infection in previously affected patients. Chikly et al (7) published a case of a 37-year-old man who presented with two separate episodes, 5 years apart from each other. Both episodes began with streptococcal pharyngitis a few days before seeking medical attention for chest pain.
References
- 1.Burova LA, Nagornev VA, Pigarevski PV, Gladilina MM, Molchanova IV, Gavrilova EA, Toltolian AA, Thern A, Schalen C. Induction of myocarditis in rabbits injected with group A streptococci. Indian J Med Res. 2004;119(Suppl):183–185. [PubMed] [Google Scholar]
- 2.Gore I, Saphir O. Myocarditis associated with acute nasopharyngitis and acute tonsillitis. Am Heart J. 1947;34(6):831–851. doi: 10.1016/0002-8703(47)90148-8. [DOI] [PubMed] [Google Scholar]
- 3.Talmon Y, Ishai R, Samet A, Sturman A, Roguin N. Acute myopericarditis complicating acute tonsillitis: beware the young male patient with tonsillitis complaining of chest pain. Ann Otol Rhinol Laryngol. 2008;117(4):295–297. doi: 10.1177/000348940811700409. [DOI] [PubMed] [Google Scholar]
- 4.Mokabberi R, Shirani J, M AH, Go BD, Schiavone W. Streptococcal pharyngitis-associated myocarditis mimicking acute STEMI. JACC Cardiovasc Imaging. 2010;3(8):892–893. doi: 10.1016/j.jcmg.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 5.Upadhay GA, Gainor JF, Stamm LM, Weinberg AN, Dec GW, Ruskin JN. Acute nonrheumatic streptococcal myocarditis: STEMI mimic in young adults. Am J Med. 2012;125(12):1230–1233. doi: 10.1016/j.amjmed.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 6.Mavrogeni S, Bratis K, Kitsiou A, Kolovou G. Streptococcal tonsillitis and acute streptococcal myocarditis: an unusual combination assessed by cardiac magnetic resonance imaging and endomyocardial biopsy. Ann Otol Rhinol Laryngol. 2012;121(9):604–608. doi: 10.1177/000348941212100907. [DOI] [PubMed] [Google Scholar]
- 7.Chikly A, Durst R, Lotan C, Chen S. Recurrent acute nonrheumatic streptococcal myocarditis mimicking STEMI in a young adult. Case Rep Cardiol. 2014;2014:964038. doi: 10.1155/2014/964038. [DOI] [PMC free article] [PubMed] [Google Scholar]