Abstract
Hepatocellular carcinoma (HCC) is the third-leading cause of cancer-related mortality worldwide. Most cases of HCC are associated with cirrhosis from various causes such as alcohol or viral hepatitis. Most patients are symptomatic as a result of cirrhosis itself or secondary to tumor extension. These tumors have an affinity for the vasculature and often invade the portal system. HCC rarely causes invasion of the inferior vena cava or the heart. We, however, present a case of HCC in a patient without cirrhosis who remained asymptomatic despite having tumor extension to the heart by way of the inferior vena cava. The mean survival in patients with intracardiac extension with or without aggressive treatment or intervention is approximately 4 months, but our patient greatly exceeded survival expectations after treatment with sorafenib.
Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide and is often associated with cirrhosis of the liver. These tumors are quite vascular. We present a case of a patient without known cirrhosis who presented with intracardiac extension of HCC inferior vena cava invasion.
CASE PRESENTATION
A 76-year-old white man with hypertension, asymptomatic carotid disease, and type II diabetes mellitus presented for routine follow-up. He was asymptomatic. His social history was negative for alcohol use, tattoos, travel, illicit drug use, blood transfusions, or chemical exposures in the past. His body mass index was 27 kg/m2. Examination disclosed no scleral icterus, ascites, organomegaly, asterixis, or spider angiomata. Complete blood counts, basic chemistries, bilirubin, albumin, and coagulation studies were normal. Table 1 notes additional studies.
Table 1.
Notable laboratory results
| Test | Result |
|---|---|
| Alkaline phosphatase, fractionated as biliary origin (IU/L) | 249 (38–126) |
| Aspartate aminotransferase (IU/L) | 51 (15–41) |
| Alanine aminotransferase (IU/L) | 42 (15–41) |
| Low-density-lipoprotein cholesterol (mg/dL) | 86 |
| Triglycerides (mg/dL) | 68 |
| Hemoglobin A1C | 6.8% |
| HIV | Negative |
| Hepatitis panel | Negative |
| Alpha-fetoprotein (ng/mL) | 4.1 |
Abdominal ultrasound revealed an 8 cm right hepatic lobe mass. A triple-phase computed tomography (CT) scan of the abdomen revealed a 12 × 8 cm hepatic mass and inferior vena cava compression, but no evidence of cirrhosis (Figure 1). Repeat CT 1 month later revealed an 11 × 13 cm mass with inferior vena cava tumor infiltration and extension to the right atrium, where a 4 × 4 cm mass consistent with tumor infiltration was noted (Figure 2). Liver biopsy noted some hepatocytes with mild fatty changes and no evidence of hemosiderosis or cirrhosis, consistent with moderately differentiated HCC. An echocardiogram showed an ejection fraction of 55% to 60% and a 2.5 × 2.5 cm fixed mass in the right atrium.
Figure 1.
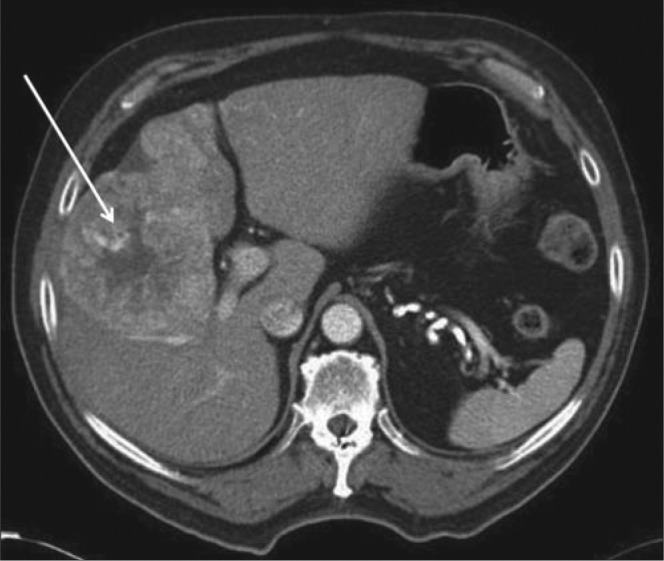
Triple-phase liver CT demonstrates a large heterogeneous mass (arrowhead) within the right hepatic lobe with peripheral arterial enhancement (increased density within the lesion) and central necrosis (decreased density and enhancement in the central aspect of the mass) suggestive of HCC.
Figure 2.
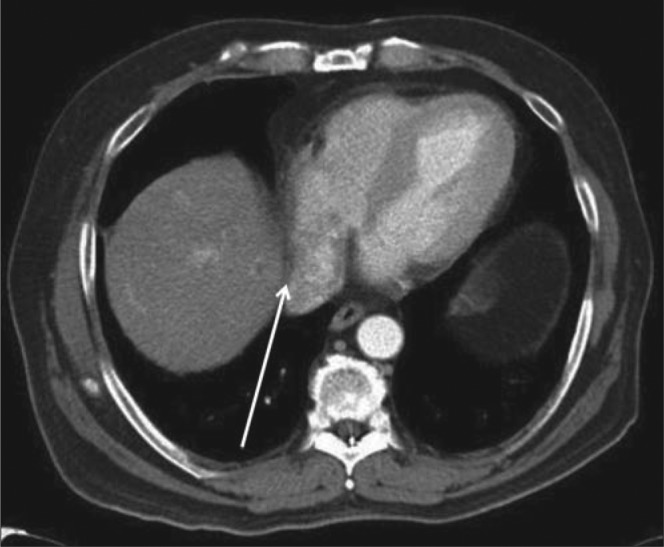
Axial CT of the abdomen demonstrating a heterogeneous enhancing filling defect within the inferior vena cava/right atrial junction (arrowhead) consistent with tumor thrombus.
The patient was started on sorafenib. He tolerated treatment well with only minimal side effects, such as hand-foot syndrome, for approximately 10 months after the diagnosis. He later developed fatigue, dyspnea, and weight loss. Repeat CT noted disease progression. He died approximately 14 months after diagnosis.
DISCUSSION
HCC has a 5-year survival of 5% in nontransplant candidates (1–3). Approximately 80% of cases worldwide are attributable to viral hepatitis (4). Nonviral factors that lead to HCC include obesity and diabetes mellitus (causing nonalcoholic fatty liver disease). Alcohol abuse and tobacco use, hemochromatosis, oral contraceptives, aflatoxin, pesticides, and cirrhosis of any cause can also cause HCC (1–3). Most HCC cases (80% to 90%) are associated with cirrhosis and are caused by viral hepatitis or alcohol abuse. Most cases of HCC in noncirrhotics are symptomatic and occur in older adults, whereas cirrhotic patients with HCC may be relatively asymptomatic (5).
HCC often metastasizes to lymph nodes, bone, and lung, but it also has a significant tendency for vascular invasion (6). Tumor extension to the portal system is quite common, but invasion of the inferior vena cava and/or heart without invasion of the portal system is rare (incidence 0.53%; 6% at autopsy) (4, 5). Local invasion is more common in cirrhotic patients (5). In the rare cases of HCC with tumor extension to the right atrium and inferior vena cava, most patients were either symptomatic, had cirrhosis, or both (4–9).
The mean survival in HCC patients with inferior vena cava or right atrium extension is 1 to 4 months regardless of treatment (4, 7). There may be a modest benefit with radiation, transarterial chemoembolization, or systemic chemotherapy with sorafenib, depending on the size of the lesions (6). Palliative cardiac surgery can be used in cases of cardiac obstruction (8, 9).
In recent years, HCC has been treated with sorafenib, an oral chemotherapeutic agent that targets several tyrosine kinase–dependent molecular pathways, such as vascular endothelial growth factor and platelet-derived growth factor-beta. These pathways allow for proliferation of HCC; therefore, sorafenib has been associated with reduced angiogenesis and increased apoptosis of tumor cells in HCC. The SHARP (Sorafenib HCC Assessment Randomized Protocol) trial randomized patients with advanced HCC who were Child-Pugh Class A and had good performance scores (Eastern Cooperative Oncology Group scores of 2 or less) to sorafenib versus placebo. There was an increase in overall survival of approximately 3 months in the sorafenib-treated group (median survival of 10.7 months in the treated group compared with 7.9 months in the placebo group) with only minimal side effects of hypertension, hand-foot syndrome, hypertension, and diarrhea (10).
To our knowledge, this is the first patient without evidence of viral hepatitis or cirrhosis to present asymptomatically with HCC and cardiac involvement. Our case is also unique in that the etiology of this patient's HCC remains largely cryptogenic. Most importantly, our patient greatly exceeded survival expectations based on currently reported survival data of patients with extensive intracardiac tumor burden (the median survival is 4 months, and our patient survived >14 months). It should be noted, however, that most of the available survival data regarding intracardiac HCC did not involve patients treated with sorafenib. Our patient's increased survival further underscores the importance of targeted chemotherapeutic agents such as sorafenib in the treatment of patients with advanced HCC.
References
- 1.Cabibbo G, Maida M, Genco C, Antonucci M, Cammà C. Causes of and prevention strategies for hepatocellular carcinoma. Semin Oncol. 2012;39(4):374–383. doi: 10.1053/j.seminoncol.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Hamed MA, Ali SA. Non-viral factors contributing to hepatocellular carcinoma. World J Hepatol. 2013;5(6):311–322. doi: 10.4254/wjh.v5.i6.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blonski W, Kotlyar DS, Forde KA. Non-viral causes of hepatocellular carcinoma. World J Gastroenterol. 2010;16(29):3603–3615. doi: 10.3748/wjg.v16.i29.3603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pandya H, Shah C, Lakhani J, Patel M. Intra-atrial tumour thrombus secondary to hepatocellular carcinoma. Australas Med J. 2013;6(6):321–324. doi: 10.4066/AMJ.2013.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demir K, Akyüz F, Poyanli A, Okten A. An asymptomatic huge hepatocellular carcinoma with intra-atrial tumor thrombus in a patient with chronic hepatitis B viral infection. Turk J Gastroenterol. 2006;17(3):203–205. [PubMed] [Google Scholar]
- 6.Sung AD, Cheng S, Moslehi J, Scully EP, Prior JM, Loscalzo J. Hepatocellular carcinoma with intracavitary cardiac involvement: a case report and review of the literature. Am J Cardiol. 2008;102(5):643–645. doi: 10.1016/j.amjcard.2008.04.042. [DOI] [PubMed] [Google Scholar]
- 7.Bhaijee F, Subramony C. Hepatocellular carcinoma with intracardiac extension. Clin Gastroenterol Hepatol. 2012;10(1):e4. doi: 10.1016/j.cgh.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Ulus T, Birdane A, Dündar E, Tünerir B. Asymptomatic course of a metastatic mass completely filling the right atrium in a patient with hepatocellular carcinoma. Turk Kardiyol Dern Ars. 2012;40(1):52–54. doi: 10.5543/tkda.2012.01753. [DOI] [PubMed] [Google Scholar]
- 9.Kan CB, Chang RY, Chen CK. Isolated right ventricular intracavitary metastasis of hepatocellular carcinoma in a 74-year-old woman. J Chin Med Assoc. 2008;71(6):318–320. doi: 10.1016/S1726-4901(08)70130-8. [DOI] [PubMed] [Google Scholar]
- 10.Llovet JM, Ricci S, Mazzaferro V, Hilgard P, Gane E, Blanc JF, de Oliveira AC, Santoro A, Raoul JL, Forner A, Schwartz M, Porta C, Zeuzem S, Bolondi L, Greten TF, Galle PR, Seitz JF, Borbath I, Häussinger D, Giannaris T, Shan M, Moscovici M, Voliotis D, Bruix J. SHARP Investigators Study Group Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–390. doi: 10.1056/NEJMoa0708857. [DOI] [PubMed] [Google Scholar]


