Abstract
A public health response relies upon rapid and reliable confirmation of disease by diagnostic assays. Here, we detail the design and validation of two variola virus-specific real-time PCR assays, since previous assays cross-reacted with newly identified cowpox viruses. The assay specificity must continually be reassessed as other closely related viruses are identified.
TEXT
Variola virus, a solely human pathogen, is the causative agent of smallpox, which was deemed eradicated in 1980 by the World Health Organization (WHO), leading to the cessation of routine smallpox vaccination. Although several vaccines exist, the threat of variola virus being used as a bioweapon still remains (1, 2). It would be contraindicated for certain individuals, such as the immunocompromised, to receive vaccination, due to serious vaccine adverse events that could be fatal (3, 4). Diagnosis based on clinical symptoms alone is challenging, since the symptoms of smallpox resemble those of numerous other rash-causing diseases and the majority of physicians today have never seen smallpox lesions. In the event of a release, quick and accurate clinical diagnosis would be critical to limit the spread of infection and contain a potential outbreak.
Real-time PCR has gained favor over historic diagnostic methods (5) due to its increased sensitivity, low cost, and more rapid results. This paper enumerates the design and validation of two variola virus-specific real-time PCR assays, which occurred after newly discovered orthopoxviruses identified a loss of specificity for previously authenticated variola virus-specific assays. These findings highlight the importance of continually verifying the assay's specificity to ensure a reliable diagnostic and to understand the assay's performance in identifying a high-consequence (select agent tier 1) pathogen.
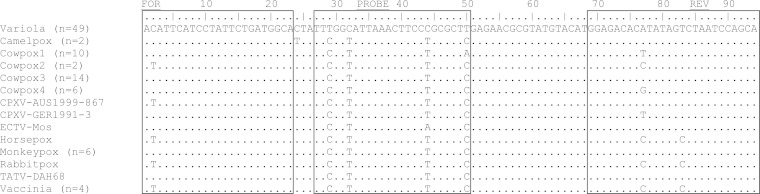
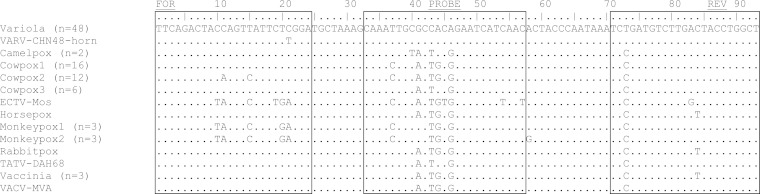
Previously validated assays directed against the E9L and A13L (A14L in variola virus) genes (see the supplemental material) of variola virus were found to cross-react with newly identified isolates of cowpox virus (6) (Table 1). The alignments of these newly identified cowpox viruses predicted cross-reaction with the E9L assay; however, the A13L assay target region resembled the cowpox virus strain used in the original validation (see Fig. S1 and S2 in the supplemental material). The original validation was done with reagents and equipment that are no longer commercially available. In order to determine whether cross-reaction would occur, wet laboratory testing was performed with newer platforms and enzymes. The reaction mixtures and cycling conditions (see Table S2 in the supplemental material) were modified slightly to replace the master mix and for use on newer platforms, either the ABI7900 or ABI7500 fast Dx (Applied Biosystems, CA). As predicted, cross-reaction occurred with the E9L assay (Table 1; see Table S2C and E). Samples were considered positive if the fluorescent signal crossed the threshold within 40 cycles. The detection of the cowpox virus strains by the A13L assay was greatly reduced compared to their detection by the E9L assay (∼10,000-fold) (Table 1). This low-level cross-reaction occurred with cowpox virus strains with sequences identical to that of the strain used in the original validation—the probe target region contains only 2 nucleotide differences, while most other non-variola orthopoxvirus sequences contain at least 3 nucleotide differences. Improvements in the efficiency of real-time PCR reagents and newer platforms may also account for this difference from the initial A13L validation (see Table S3). To fulfill the need for specific variola virus assays, the conserved region of the genome, encoding essential genes, was evaluated for regions that demonstrated specificity to variola virus through bioinformatics analysis. Potential variola virus-specific targets were identified within the A4L and A36R genes (Fig. 1 and 2). The primers and probe sequences for the A4L and A36R assays were selected from the P4b precursor protein gene (A4L from BSH75 banu) and the enveloped virus glycoprotein gene (A36R from BSH75 banu), respectively, using Primer Express (version 2.0; Applied Biosystems, CA) (Table 2). The target regions for A4L and A36R were identical in all variola virus strains except for a single nucleotide polymorphism (SNP) in the A36R gene in CHN48 horn (Fig. 2). The reaction and cycling conditions are detailed in Tables 3 and 4. Samples were considered positive if the fluorescent signal crossed the threshold within 40 cycles.
TABLE 1.
Cross-reactivity of E9L and A13L assays with newly identified cowpox virus strains
| Strain (1 ng/µl) | GenBank accession no. | Avg positive CT value in indicated assaya |
|
|---|---|---|---|
| E9L | A13L | ||
| FIN2000-MAN | HQ420893 | Neg | Neg |
| GER1980-EP4 | HQ420895 | 19.2 | 35.1 |
| GER1991-3 | DQ437593 | 18.0 | 34.2b |
| GER1998-2 | HQ420897 | 16.7 | Neg |
| Nor1994-MAN | HQ420899 | Neg | 37.3 |
The average cycle when fluorescence crossed the threshold (CT) is shown. Each sample was tested in triplicate. Neg, CT value was not produced.
GER1991-3 had a total DNA concentration of 4 ng instead of 5 ng.
FIG 1.
Sequence alignment of target regions for the A4L assay. The alignment of 99 strains was made using BioEdit Sequence Alignment Editor. Those strains within one species that were identical in the primer and probe target regions are condensed; the number in parentheses represents the number of strains included. GenBank sequence accession numbers are as follows (A4L sequences for RPXV-USA64-85A, SKPV-USA1978-WA, and VPXV-USA1985-CA are not available in GenBank): Camelpox virus (AY009089, NC_003391), Cowpox virus 1 (NC_003663, HQ420894, HQ420896, HQ420898, KC813511.1, KC813507.1, KC813494.1, KC813499.1, HQ420895.1, HQ420897.1), Cowpox virus 2 (X94355, HQ420893), Cowpox virus 3 (KC813509.1, KC813506.1, KC813504.1, KC813502.1, KC813500.1, KC813497.1, KC813498.1, KC813496.1, KC813495.1, KC813493.1, KC813492.1, KC813491.1, HQ420900.1, HQ420899.1), Cowpox virus 4 (KC813512.1, KC813510.1, KC813503.1, KC813501.1, KC813505.1, KC813508.1), Monkeypox virus (AY603973, DQ011156, DQ011157, DQ011155, NC_003310, DQ011154), Vaccinia virus (AY603355, M35027, NC_006998, AY678276). All other accession numbers can be found in Table S1 in the supplemental material. FOR, forward primer; REV, reverse primer; CPXV, cowpox virus; ECTV, ectromelia virus; TATV, taterapox virus. The probe contains 5′ 6-carboxyfluorescein (FAM).
FIG 2.
Sequence alignment of target regions for the A36R assay. The alignment of 99 strains was made using BioEdit Sequence Alignment Editor. Those strains within one species that were identical in the primer and probe target regions are condensed; the number in parentheses represents the number of strains included. GenBank sequence accession numbers are as follows (A36R sequences for RPXV-USA64-85A, SKPV-USA1978-WA and VPXV-USA1985-CA are not available in GenBank): Camelpox virus (AY009089, NC_003391), Cowpox virus 1 (HQ407377, HQ420893, HQ420895, HQ420898, X94355, KC813511.1, KC813507.1, KC813506.1, KC813504.1, KC813500.1, KC813498.1, KC813497.1, KC813495.1, KC813493.1, KC813492.1, KC813491.1), Cowpox virus 2 (NC_003663, HQ420894, HQ420896, DQ437593, HQ420897, HQ420899, HQ420900, KC813509.1, KC813502.1, KC813499.1, KC813496.1, KC813494.1), Cowpox virus 3 (KC813512.1, KC813510.1, KC813508.1, KC813505.1, KC813503.1, KC813501.1), Monkeypox virus 1 (AY603973, DQ011156, DQ011157), Monkeypox virus 2 (DQ011155, NC_003310, DQ011154), Vaccinia virus (NC_006998, M35027, AY678276). All other accession numbers can be found in Table S1 in the supplemental material. FOR, forward primer; REV, reverse primer; VARV, variola virus; ECTV, ectromelia virus; TATV, taterapox virus; VACV, vaccinia virus. The probe contains 5′ 6-carboxyfluorescein (FAM).
TABLE 2.
Sequences of the primers and probes for the A4L and A36R assaysa
| Primer or probe | Sequence for: |
|
|---|---|---|
| A4L | A36R | |
| Forward | 5′ ACATTCATCCTATTCTGATGGCA 3′ | 5′ TTCAGACTACCAGTTATTCTCGGA 3′ |
| Reverse | 5′ TGCTGGATTAGACTATATGTGTCTCC 3′ | 5′ AGCCAGGTAGTCAAGACATCAGA 3′ |
| Probe | 5′ FAM-TTTGGCATTAAACTTCCCGCGCTT-BHQ 3′ | 5′ FAM-CAAATTGCGCCACAGAATCATCAAC-BHQ 3′ |
Primer and probe sets were synthesized by the Biotechnology Core Facility (CDC, Atlanta, GA). The sequences are from BSH75 banu (GenBank accession number DQ437581). The amplicon lengths are 94 bp for A4L and 93 bp for A36R.
TABLE 3.
Master mix reaction mixture for both the A4L and the A36R assays
| Component | Amt and concn |
|---|---|
| LightCycler FastStart DNA Master HybProbe master mix (Roche Applied Science) | 2.5 μl of 10× mix |
| Forward primer | 1 μl of 25 μM stock |
| Reverse primer | 1 μl of 25 μM stock |
| Probe | 1 μl of 25 μM stock |
| Magnesium chloride | 3 μl of 25 mM stock |
| Sample DNA | 5 μl |
| Total vol | 25 μl |
TABLE 4.
Cycling conditions on the ABI7500 Fast Dx for the A4L and A36R assays
| Step | Cycling conditions (temp [°C], time, no. of cycles) for: |
|
|---|---|---|
| A4L | A36R | |
| Activate polymerase | 95, 8 min, 1 | 95, 8 min, 1 |
| Denature | 95, 5 s, 40 | 95, 5 s, 40 |
| Elongate | 60, 25 s, 40 | 60, 25 s, 40 |
Based on previous validations (see Table S4 in the supplemental material), bioinformatics analysis adeptly predicted the likelihood that a real-time PCR assay would detect a variola virus strain at a particular target region, due to low genetic variability found between variola virus strains (7). Additionally, previous validations demonstrated that real-time PCR assays remained sensitive regardless of sample type (see Table S4). Therefore, three variola virus strains of semipurified preparations were chosen for the inclusivity panel: VARV-IND64_vel5 from primary clade I, VARV-SLN68_258 from primary clade II, and VARV-CHN48_horn (primary clade I) due to the SNP (Fig. 2). To generate semipurified virus, crude virus preparations (virus-infected-cell lysates harvested at 48 or 72 h postinfection) were purified through 2 to 3 1,1,2-trichlorofluoroethane extractions followed by two sucrose cushion ultracentrifugations, as previously described (8–13). DNA was extracted using the AquaPure genomic DNA isolation kit (Bio-Rad, CA) and suspended in 50 μl of AquaPure DNA hydration buffer.
A two-step approach was employed to determine the analytical limit of detection (LOD), defined as the lowest sample concentration producing a positive threshold cycle (CT) value at least 95% of the time, for each inclusivity strain. Initially, an estimate of the analytical LOD for each variola virus strain was determined by preparing a 10-fold dilution series ranging from 500 pg to 0.05 fg of variola virus DNA per reaction. Based on the results, a narrower window of concentrations was selected to determine the analytical LOD. The lowest concentrations reproducibly detected were selected, along with the 2 log-fold-higher and -lower concentrations. A total of 20 reactions per concentration were run over 3 consecutive days by two operators for both assays to determine the analytical LOD for each strain, concentration, and assay. The analytical LOD for both assays was 50 fg, with standard deviations of 1.08 (A4L) and 1.44 (A36R) (Table 5). At the LOD concentration, the standard deviations of the observed CT values between days ranged from 0.92 to 1.15 for A4L and from 0.85 to 1.89 for A36R. The standard deviations for each operator across all days were also calculated; operator 1 had a standard deviation of 1.06 for A4L and 0.91 for A36R. Operator 2 yielded a standard deviation of 1.12 for A4L and 1.83 for A36R. These data suggest the assay to be reproducible in the hands of multiple users.
TABLE 5.
Analytical LOD determined for A4L and A36R real-time PCR assays with three variola virus strainsa
| Strain | Concn of sample | A4L |
A36R |
||
|---|---|---|---|---|---|
| No. positive/total no. of replicates | Avg positive CT value | No. positive/total no. of replicates | Avg positive CT value | ||
| CHN48 horn | 500 pg | 3/3 | 20.8 | 3/3 | 22.3 |
| CHN48 horn | 50 pg | 3/3 | 24.0 | 3/3 | 26.0 |
| CHN48 horn | 5 pg | 3/3 | 27.7 | 3/3 | 29.8 |
| CHN48 horn | 500 fg | 3/3 | 31.4 | 20/20 | 32.7 |
| CHN48 horn | 50 fg | 20/20 | 35.1 | 19/20 | 36.2 |
| CHN48 horn | 5 fg | 20/20 | 38.4 | 10/20 | 39.1 |
| CHN48 horn | 0.5 fg | 1/20 | 39.4 | 0/20 | Neg |
| CHN48 horn | 0.05 fg | 0/20 | Neg | 0/20 | Neg |
| CHN48 horn | 0.005 fg | 0/20 | Neg | — | — |
| IND64 vel5 | 500 pg | 3/3 | 19.0 | 3/3 | 20.1 |
| IND64 vel5 | 50 pg | 3/3 | 22.6 | 3/3 | 23.8 |
| IND64 vel5 | 5 pg | 3/3 | 26.3 | 3/3 | 27.9 |
| IND64 vel5 | 500 fg | 3/3 | 29.8 | 20/20 | 30.9 |
| IND64 vel5 | 50 fg | 20/20 | 33.4 | 20/20 | 34.4 |
| IND64 vel5 | 5 fg | 18/20 | 37.4 | 20/20 | 37.4 |
| IND64 vel5 | 0.5 fg | 8/20 | 39.2 | 5/20 | 38.8 |
| IND64 vel5 | 0.05 fg | 0/20 | Neg | 0/20 | Neg |
| IND64 vel5 | 0.005 fg | 0/20 | Neg | — | — |
| SLN68 258 | 500 pg | 3/3 | 21.4 | 3/3 | 23.2 |
| SLN68 258 | 50 pg | 3/3 | 25.2 | 3/3 | 26.9 |
| SLN68 258 | 5 pg | 3/3 | 28.7 | 3/3 | 30.9 |
| SLN68 258 | 500 fg | 3/3 | 32.3 | 20/20 | 33.4 |
| SLN68 258 | 50 fg | 20/20 | 35.4 | 20/20 | 36.9 |
| SLN68 258 | 5 fg | 14/20 | 39.2 | 6/20 | 39.6 |
| SLN68 258 | 0.5 fg | 0/20 | Neg | 0/20 | Neg |
| SLN68 258 | 0.05 fg | 0/20 | Neg | 0/20 | Neg |
| SLN68 258 | 0.005 fg | 0/20 | Neg | — | — |
Each sample was tested in triplicate. Neg, CT value was not produced; —, not tested.
To reduce the risk of potential false positives, an expansive exclusivity panel was defined, consisting of non-variola orthopoxviruses and non-orthopoxvirus agents that present with clinical symptoms of a rashlike illness. The origins of the viral, bacterial, clinical lesion material, and cellular isolates are documented in Table S1 in the supplemental material. Non-variola orthopoxvirus DNA was extracted using the QIAamp DNA blood minikit (Qiagen, CA) and resuspended in 50 μl of Qiagen AE elution buffer. Additionally, numerous human skin flora DNAs and human DNAs were evaluated to ensure that DNAs common in skin lesion clinical specimens (crust, swab of a lesion, touch preparation of lesion fluid, or fresh biopsy specimen) would not cross-react. Bacteria were propagated on anaerobic blood agar or 5% sheep blood agar and incubated at 35°C with or without CO2. After a 24- or 48-h incubation period, harvested colonies were suspended in 0.85% sterile saline (0.5 McFarland turbidity) and extracted using the MagNA pure nucleic acid isolation kit I (Roche Applied Science, Indianapolis, IN) on the MagNA pure compact instrument (Roche Applied Science). Both assays demonstrated high specificity; none of the 38 non-variola virus agents screened produced a signal that crossed the threshold cycle value (Table 6).
TABLE 6.
Specificity of A4L and A36R real-time PCR assays screened against non-variola orthopoxviruses, rash-causing agents, and normal skin floraa
| Speciesb | Strain | Concn of sample | Avg positive CT value for: |
|
|---|---|---|---|---|
| A4L | A36R | |||
| Camelpox virus | Somalia-1978-2379 | 500 pg | Neg | Neg |
| Cowpox virus | FIN2000-MAN | 500 pg | Neg | Neg |
| Cowpox virus | GER1980-EP4 | 500 pg | Neg | Neg |
| Cowpox virus | GER1991-3 | 500 pg | Neg | Neg |
| Cowpox virus | GER1998-2 | 500 pg | Neg | Neg |
| Cowpox virus | Nor1994-MAN | 500 pg | Neg | Neg |
| Ectromelia virus | Mos | 500 pg | Neg | Neg |
| Monkeypox virus | RCG-2003-358 | 500 pg | Neg | Neg |
| Monkeypox virus | USA-2003-044 | 500 pg | Neg | Neg |
| Raccoonpox virus | USA64-85A | 500 pg | Neg | Neg |
| Skunkpox virus | USA-1978-WA | 500 pg | Neg | Neg |
| Taterapox virus | DAH68 | 500 pg | Neg | Neg |
| Vaccinia virus | ACAM 2000 | 500 pg | Neg | Neg |
| Vaccinia virus | BRZ SERRO | 500 pg | Neg | Neg |
| Vaccinia virus | Copenhagen | 500 pg | Neg | Neg |
| Vaccinia virus | WR | 500 pg | Neg | Neg |
| Volepox virus | USA-1985-CA | 500 pg | Neg | Neg |
| Escherichia coli | 5 × 103 CFU | Neg | Neg | |
| Enterococcus faecalis | 5 × 103 CFU | Neg | Neg | |
| Herpes simplex virus type 1 | F | 5 × 106 genomes | Neg | Neg |
| Herpes simplex virus type 2 | G | 5 × 106 genomes | Neg | Neg |
| Human genomic DNA | 500 pg | Neg | Neg | |
| Klebsiella pneumoniae | 5 × 103 CFU | Neg | Neg | |
| Orf | 500 pg | Neg | Neg | |
| Peptostreptococcus anaerobius | 5 × 103 CFU | Neg | Neg | |
| Propionibacterium acnes | 5 × 103 CFU | Neg | Neg | |
| Pseudomonas aeruginosa | 5 × 103 CFU | Neg | Neg | |
| Rickettsia prowazekii | breinl | ND | Neg | Neg |
| Rickettsia sibirica | ND | Neg | Neg | |
| Staphylococcus aureus | Strain 1 | 5 × 103 CFU | Neg | Neg |
| S. aureus | Strain 2 | 5 × 103 CFU | Neg | Neg |
| Staphylococcus epidermidis | Strain 1 | 5 × 103 CFU | Neg | Neg |
| S. epidermidis | Strain 2 | 5 × 103 CFU | Neg | Neg |
| S. epidermidis | Strain 3 | 5 × 103 CFU | Neg | Neg |
| Streptococcus gallylyticus | 5 × 103 CFU | Neg | Neg | |
| Streptococcus pyogenes | 5 × 103 CFU | Neg | Neg | |
| Varicella-zoster virus | pOKA | 5 × 109 genomes | Neg | Neg |
| Varicella-zoster virus | Webster | 4 × 1010 genomes | Neg | Neg |
Each sample was tested in triplicate. ND, the concentration of DNA could not be determined, refer to BEIResources; Neg, CT value was not produced.
Bacterial strains were part of the skin flora panel, which was a gift from the CDC Bioterrorism Rapid Response and Advanced Technology Laboratory.
Since smallpox is an eradicated disease, there are no recent clinical samples available to ascertain the diagnostic assay performance within clinical material from confirmed cases. Therefore, CDC Poxvirus program clinical sample remainders, collected from patients presenting with pustular or vesicular rash illness but ruled negative for poxvirus infection by real-time PCR, were selected for diagnostic assay validation. The clinical sample specimens consisted of the following sample types: swab, swab in viral transport medium, slide, tissue, and crust. Thirty-six of these clinical sample remainders were deidentified (IRB exempt protocol number 6423) and divided into three groups of 12 to be spiked with semipurified variola virus DNA (IRB protocol number 6447) from each of the three inclusivity strains (VARV-CHN48_horn, VARV-IND64_vel5, and VARV-SLN68_258). Each group was further subdivided into three subgroups of four to be spiked with 100 pg/μl (10,000× LOD), 1 pg/μl (100× LOD), or 100 fg/μl (10× LOD). DNA was extracted using the QIAamp DSP DNA blood minikit protocol (Qiagen, CA) and screened blindly by two operators in duplicate with A4L and A36R assays on the ABI7500 fast Dx (Applied Biosystems, Foster City, CA), using the cycling conditions listed in Table 4. The A4L and A36R assays generated positive results for 35/36 (97.2%) and 34/36 (94.4%) spiked specimens, respectively, for both operators (Table 7). Specimen 4 was not detected by either operator and was spiked with the intermediate amount of VARV-IND64_vel5 DNA (1 pg/μl, 100× LOD); however, the lowest spiked concentration of VARV-IND64_vel5 was detected 100% of the time by both assays and both operators. Specimen 35 was detected by 3/4 A36R reactions and was spiked with the smallest amount of VARV-SLN68_258 DNA (0.1 pg/μl, 10× LOD). These CT values were 4.5 to 5 CT values later than those of the other three specimens spiked with 0.1 pg/μl of VARV-SLN68_258 DNA. Further PCR analysis of specimens 4 and 35 failed to yield positive results for a control assay designed to detect human DNA (data not shown), suggesting that these two clinical sample remainders were compromised, possibly containing DNA-degrading components or inhibitors to PCR. With the exception of the one negative A36R reaction for specimen 35, the operators achieved similar assay results with the spiked specimen panel (Table 7). Despite these potential compromised clinical sample remainders, both the A4L and the A36R assay remained sensitive and specific in testing spiked samples, our best measure to ensure their utility within a clinical diagnostic setting.
TABLE 7.
Sensitivities of A4L and A36R assays within clinical sample matrixesa
| Specimen | Strain | Concn of DNA (pg/μl) | Avg positive CT value for: |
|
|---|---|---|---|---|
| A4L | A36R | |||
| Control | CHN48 horn | 0.01 | 35.3 | 35.3 |
| 3 | CHN48 horn | 0.1 | 32.8 | 33.9 |
| 18 | CHN48 horn | 0.1 | 33.0 | 34.4 |
| 19 | CHN48 horn | 0.1 | 33.3 | 34.1 |
| 32 | CHN48 horn | 0.1 | 33.0 | 34.1 |
| 7 | CHN48 horn | 1 | 28.1 | 29.5 |
| 12 | CHN48 horn | 1 | 28.6 | 29.7 |
| 27 | CHN48 horn | 1 | 29.2 | 30.2 |
| 33 | CHN48 horn | 1 | 28.7 | 29.9 |
| 5 | CHN48 horn | 100 | 21.2 | 22.5 |
| 14 | CHN48 horn | 100 | 21.8 | 23.2 |
| 21 | CHN48 horn | 100 | 21.2 | 22.5 |
| 28 | CHN48 horn | 100 | 21.4 | 23.1 |
| 8 | IND64 vel5 | 0.1 | 30.2 | 31.4 |
| 13 | IND64 vel5 | 0.1 | 30.4 | 31.1 |
| 24 | IND64 vel5 | 0.1 | 31.7 | 32.6 |
| 29 | IND64 vel5 | 0.1 | 30.9 | 31.8 |
| 4 | IND64 vel5 | 1 | Neg | Neg |
| 16 | IND64 vel5 | 1 | 26.9 | 27.9 |
| 23 | IND64 vel5 | 1 | 27.1 | 27.9 |
| 36 | IND64 vel5 | 1 | 26.7 | 27.5 |
| 1 | IND64 vel5 | 100 | 19.0 | 20.1 |
| 17 | IND64 vel5 | 100 | 19.3 | 20.5 |
| 22 | IND64 vel5 | 100 | 19.3 | 20.4 |
| 30 | IND64 vel5 | 100 | 19.2 | 20.2 |
| 2 | SLN68 258 | 0.1 | 33.6 | 35.0 |
| 15 | SLN68 258 | 0.1 | 34.0 | 35.0 |
| 26 | SLN68 258 | 0.1 | 33.7 | 34.8 |
| 35 | SLN68 258 | 0.1 | 38.8 | 39.1b |
| 6 | SLN68 258 | 1 | 29.3 | 30.1 |
| 11 | SLN68 258 | 1 | 29.9 | 31.6 |
| 25 | SLN68 258 | 1 | 29.6 | 30.3 |
| 31 | SLN68 258 | 1 | 30.3 | 30.6 |
| 9 | SLN68 258 | 100 | 22.4 | 23.7 |
| 10 | SLN68 258 | 100 | 21.7 | 23.1 |
| 20 | SLN68 258 | 100 | 22.3 | 23.7 |
| 34 | SLN68 258 | 100 | 22.4 | 23.5 |
Clinical sample remainders were spiked with variola virus DNA at various concentrations as indicated. DNA was extracted and tested in duplicate by two operators. The average cycle when fluorescence crossed the threshold is shown.
One of two replicates was positive.
The newly designed diagnostic assays (A4L and A36R) underwent extensive testing with a wide-ranging exclusivity panel to ensure that cross-reactivity with the pathogens most likely to be confused with smallpox did not occur. The assays appeared extremely sensitive (LOD = 50 fg), both analytically and within spiked clinical samples. In a public health setting, these assays could provide rapid diagnosis of smallpox disease, with results taking less than 4 h from receipt of the sample. Ideally, diagnostic assays are most informative when laboratorians work closely with clinicians and epidemiologists to identify patients with the highest suspicion of smallpox. Confidence in the identification of an eradicated disease, such as smallpox, is increased when multiple assay signatures are used to identify the pathogen and are linked to clinical manifestations. In order to improve confidence in a negative assay result, the sample should be validated for the presence of human DNA and the absence of PCR inhibitors. Both assays (A4L and A36R) show great promise as variola virus-specific diagnostic assays. However, orthopoxviruses are continually being discovered or identified. In the late 2000s, the full genomic sequences of new strains of cowpox viruses from Europe became available (6). Phylogenetic analysis illustrated that these included previously unknown lineages, suggesting the need to include additional cowpox virus strains in the exclusivity panel for assay validations. Two assays previously thought to be specific for variola virus (see the supplemental material) cross-reacted, with various degrees of sensitivity, with three of the five additional strains of cowpox virus that were screened (Table 1). Since cowpox viruses actively cause disease in humans, commonly in Europe (6), this dramatically increased the potential for clinical misdiagnosis. While bioinformatics analysis predicts that the A4L and A36R assays remain specific for variola virus, it will be important to remain vigilant in reassessing the specificity as other closely related viruses are identified.
Supplementary Material
ACKNOWLEDGMENT
This research was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC.
Footnotes
Supplemental material for this article may be found at http://dx.doi.org/10.1128/JCM.03613-14.
REFERENCES
- 1.Henderson DA, Inglesby TV, Bartlett JG, Ascher MS, Eitzen E, Jahrling PB, Hauer J, Layton M, McDade J, Osterholm MT, O'Toole T, Parker G, Perl T, Russell PK, Tonat K. 1999. Smallpox as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. JAMA 281:2127–2137. doi: 10.1001/jama.281.22.2127. [DOI] [PubMed] [Google Scholar]
- 2.Riedel S. 2005. Smallpox and biological warfare: a disease revisited. Proc (Bayl Univ Med Cent) 18:13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aragon TJ, Ulrich S, Fernyak S, Rutherford GW. 2003. Risks of serious complications and death from smallpox vaccination: a systematic review of the United States experience, 1963-1968. BMC Public Health 3:26. doi: 10.1186/1471-2458-3-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bray M. 2003. Pathogenesis and potential antiviral therapy of complications of smallpox vaccination. Antivir Res 58:101–114. doi: 10.1016/S0166-3542(03)00008-1. [DOI] [PubMed] [Google Scholar]
- 5.Olson VA, Regnery RL, Damon IK. 2009. Poxviruses: laboratory diagnostic methods, p 524–528. In Specter S, Hodinka RL, Young SA, Wiedbrauk DL (ed), Clinical virology manual, 4th ed ASM Press, Washington, DC. [Google Scholar]
- 6.Carroll DS, Emerson GL, Li Y, Sammons S, Olson V, Frace M, Nakazawa Y, Czerny CP, Tryland M, Kolodziejek J, Nowotny N, Olsen-Rasmussen M, Khristova M, Govil D, Karem K, Damon IK, Meyer H. 2011. Chasing Jenner's vaccine: revisiting cowpox virus classification. PLoS One 6:e23086. doi: 10.1371/journal.pone.0023086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, Carroll DS, Gardner SN, Walsh MC, Vitalis EA, Damon IK. 2007. On the origin of smallpox: correlating variola phylogenics with historical smallpox records. Proc Natl Acad Sci U S A 104:15787–15792. doi: 10.1073/pnas.0609268104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito J, Condit R, Obijeski J. 1981. The preparation of orthopoxvirus DNA. J Virol Methods 2:175–179. doi: 10.1016/0166-0934(81)90036-7. [DOI] [PubMed] [Google Scholar]
- 9.Esposito JJ, Knight JC. 1985. Orthopoxvirus DNA: a comparison of restriction profiles and maps. Virology 143:230–251. doi: 10.1016/0042-6822(85)90111-4. [DOI] [PubMed] [Google Scholar]
- 10.Esposito JJ, Obijeski JF, Nakano JH. 1978. Orthopoxvirus DNA: strain differentiation by electrophoresis of restriction endonuclease fragmented virion DNA. Virology 89:53–66. doi: 10.1016/0042-6822(78)90039-9. [DOI] [PubMed] [Google Scholar]
- 11.Olson VA, Laue T, Laker MT, Babkin IV, Drosten C, Shchelkunov SN, Niedrig M, Damon IK, Meyer H. 2004. Real-time PCR system for detection of orthopoxviruses and simultaneous identification of smallpox virus. J Clin Microbiol 42:1940–1946. doi: 10.1128/JCM.42.5.1940-1946.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ropp SL, Jin Q, Knight JC, Massung RF, Esposito JJ. 1995. PCR strategy for identification and differentiation of small pox and other orthopoxviruses. J Clin Microbiol 33:2069–2076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sarmiento M, Haffey M, Spear PG. 1979. Membrane proteins specified by herpes simplex viruses. III. Role of glycoprotein VP7(B2) in virion infectivity. J Virol 29:1149–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.