Abstract
Current guidelines recommend that adults with atherosclerotic cardiovascular disease take low-dose aspirin or other antiplatelet medications as secondary prevention of recurrent cardiovascular events. Yet, no national level assessment of low-dose aspirin use for secondary prevention of cardiovascular disease has been reported among a community-based population. Using data from the 2012 National Health Interview Survey, we assessed low-dose aspirin use among those with atherosclerotic cardiovascular disease. We estimated the prevalence ratios of low-dose aspirin use, adjusting for sociodemographic status, health insurance, and cardiovascular risk factors. Among those with atherosclerotic cardiovascular disease (n=3,068), 76% had been instructed to take aspirin, and 88% of those were following this advice. Of those not advised, 11% took aspirin on this own. Overall, 70% were taking aspirin (including those who followed their health care provider's advice and those who were not advised but took aspirin on their own). Logistic regression models showed that women, non-Hispanic blacks and Hispanics, those aged 40–64 years, with a high school education or with some college, or with fewer cardiovascular disease risk factors were less likely to take aspirin than men, non-Hispanic whites, those aged ≥65 years, with a college education or higher, or with all four selected cardiovascular disease risk factors, respectively. Additional analyses conducted among those with coronary heart disease only (n=2,007) showed similar patterns. In conclusion, use of low-dose aspirin for secondary prevention was 70%, with high reported adherence to health care providers' advice to take low-dose aspirin (88%), and significant variability within subgroups.
Keywords: atherosclerotic cardiovascular disease, low-dose-aspirin, cardiovascular prevention, surveillance
Introduction
The effectiveness of aspirin therapy in reducing risk for myocardial infarction, ischemic stroke, and fatal coronary events among persons with preexisting atherosclerotic cardiovascular disease is well documented.1,2 Current guidelines recommend that adults with atherosclerotic cardiovascular disease take 75 to 162 mg of aspirin (low-dose aspirin) daily to prevent recurrence of cardiovascular events.3,4,5 However, data on the current use of low-dose aspirin therapy for secondary prevention of cardiovascular disease among community-dwelling adults in the U.S. is limited. Most published studies in the U.S. have focused on clinical inpatient6,7,8 and outpatient9,10,11 settings, and are related to aspirin recommendations and use at discharge or after evaluation in outpatient settings. Using data from the 2012 National Health Interview Survey (NHIS), we provide current estimates of self-reported low-dose aspirin use for secondary prevention among community-dwelling adults with atherosclerotic cardiovascular disease.
Methods
The NHIS is a multipurpose health survey conducted continuously throughout the year by the Centers for Disease Control and Prevention's (CDC), and is the principal source of information on the health of the civilian, non-institutionalized population of the United States. The NHIS has been conducted continuously since 1957, and contains four main modules: Household, Family and Sample Adult, and Sample Child. In 2012, supplemental questions on aspirin use were included in the Sample Adult questionnaire. Data from the Household, Family, and Sample Adult sections were used in this analysis. The response rate for the Sample Adult component in 2012 was 61.2%. Detailed information on the survey design and methods can be found at the NHIS Web site (http://www.cdc.gov/nchs/nhis.htm).
Low-dose aspirin use was asked of all adults aged ≥40 years. There were four questions related to low-dose aspirin use: 1) “Has a doctor or other health professional ever told you to take a low-dose aspirin each day to prevent or control heart disease?”; 2) those who answered “yes” to this question were asked, “Are you now following this advice?”; 3) those who were not following the advice were asked, “Did a doctor or other health professional advise you to stop taking a low-dose aspirin every day?”; and 4) those who had not been advised (or those who didn't know if they had been advised to take low-dose aspirin) were asked “On your own, are you now taking a low-dose aspirin each day to prevent or control heart disease?”.
Adults with atherosclerotic cardiovascular disease were defined as those who answered “yes” to any of the following four questions: “Have you ever been told by a doctor or other health professional that you had coronary heart disease?”; “Have you ever been told by a doctor or other health professional that you had angina, also called angina pectoris?”; “Have you ever been told by a doctor or other health professional that you had a heart attack (also called myocardial infarction)?”; or “Have you ever been told by a doctor or other health professional that you had a stroke?”.
Other characteristics investigated included demographic variables: age (40–64 and ≥65 years); sex; race/ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic other, and Hispanic); level of education (less than high school graduate, high school graduate, some college, and college graduate); and health insurance status (any health insurance and no health insurance). Body mass index (BMI) was calculated by using weight and height (BMI= kg/m2) and categorized as normal weight (<25), overweight (25–29.9) and obese (≥30). The four cardiovascular disease risk factors considered were diabetes (“Have you ever been told by a doctor or other health professional that you have diabetes or sugar diabetes?”, those with borderline diabetes were not considered to have diabetes), hypertension (“Were you told on two or more different visits that you had hypertension, also called high blood pressure?”), high blood cholesterol (“Have you ever been told by a doctor or other health professional that you had high cholesterol?”), and current smoking status (defined as an answer of “yes” to the question “Have you smoked at least 100 cigarettes in your entire life?” and an answer of “every day” or “some days” to the question “Do you now smoke cigarettes every day, some days or not at all?”). Other factors that could affect aspirin use included history of ulcer (“Have you ever been told by a doctor or other health professional that you had an ulcer? This could be a stomach, duodenal, or peptic ulcer.”) or arthritis (“Have you ever been told by a doctor or other health professional that you have some form of arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia?”).
Those with a history of atherosclerotic cardiovascular disease were defined as the population at risk of recurrent cardiovascular events and were eligible for low-dose aspirin use for secondary prevention based on current recommendations3. We determined the distribution of demographic characteristics and cardiovascular disease risk factors among the population at risk. We also estimated the age-standardized percentage of the population using low-dose aspirin for secondary prevention, which included those who followed a health care provider's advice and those who took low-dose aspirin on their own, using the 2000 US Census standard projected population.12 To determine whether low-dose aspirin use varied by other characteristics, we used logistic regression to calculate prevalence ratios (and 95% confidence intervals [CIs])13 of low-dose aspirin use by age, sex, race/ethnicity, levels of education, BMI, health insurance status, history of ulcer and history of arthritis. In addition, we also tested for a linear trend in the relationship between cardiovascular risk and aspirin use by substituting the number of risk factors as a continuous variable in the model.
The primary definition of atherosclerotic cardiovascular disease in this analysis includes both coronary heart disease and stroke. However, aspirin is contraindicated for those who have survived hemorrhagic strokes. The NHIS does not classify strokes as either ischemic or hemorrhagic, and therefore a second definition of atherosclerotic cardiovascular disease including only those with coronary heart disease was used in additional analyses.
Sampling weights were used to produce national estimates that are representative of the adult civilian noninstitutionalized U.S. population.14 Participants with missing data on coronary heart disease, stroke or aspirin use were excluded. The analyses were performed using SAS version 9.3 and SAS-callable SUDAAN version 10 (Research Triangle Institute, Research Triangle Park, North Carolina)15 to account for the complex sample design. All statistical tests were 2-tailed, and statistical significance was defined at P < 0.05.
Results
The 2012 NHIS Sample Adult file included 34,525 participants, of whom 3,213 had self-reported atherosclerotic cardiovascular disease. Among those ≥40 years, 3,068 provided data on their use of low-dose aspirin. Among them, 2,007 had coronary heart disease only.
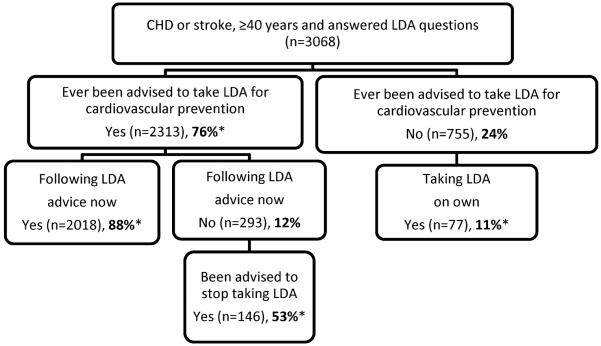
Characteristics of the population eligible for secondary prevention (those with coronary heart disease and/or stroke, as well as those with coronary heart disease only) are shown in Table 1. The distributions of demographic characteristics were generally the same, regardless of the definition of atherosclerotic cardiovascular disease. Figure 1 provides data on those with coronary heart disease or stroke, the number and percentage of respondents that provided information on low-dose aspirin behaviors. Three-quarters (76%) of adults with coronary heart disease or stroke had been advised by a health professional to take low-dose aspirin. Of these, 88% followed the advice. Among those who did not follow the advice, about half (53%) had been advised to stop taking low-dose aspirin. Among those who were not advised to take low-dose aspirin, 11% were taking it on their own. These percentages were similar for respondents with coronary heart disease only (not shown).
Table 1.
Characteristics of Adults Aged 40 and Over Eligible1 to Take Low-dose Aspirin for Secondary Prevention of Cardiovascular Disease, by Definition of Atherosclerotic Cardiovascular Disease, United States, 20122
| Variable | Coronary Heart Disease and/or Stroke (n=3,068) % (95% Confidence interval) | Coronary Heart Disease Only (n=2,007) % (95% Confidence interval) |
|---|---|---|
| Age (years) | ||
| 40–64 | 46.2% (42.8–49.8) | 46.3% (43.6–49.1) |
| >65 | 53.8% (51.5–56.1) | 53.7% (50.9–56.5) |
|
| ||
| Sex | ||
| Men | 53.9% (51.5–56.4) | 58.1% (55.0–61.1) |
| Women | 46.1% (43.6–48.5) | 41.9% (38.9–45.0) |
|
| ||
| Race/Ethnicity | ||
| Non-Hispanic White | 74.5% (72.4–76.5) | 77.2% (74.8–79.4) |
| Non-Hispanic Black | 12.4% (11.0–14.1) | 10.6% (9.1–12.3) |
| Hispanic | 8.9% (7.8–10.2) | 8.3% (7.0–9.8) |
| Other | 4.2% (3.4–5.2) | 3.9% (3.0–5.1) |
|
| ||
| Education | ||
| <High school | 25.2% (23.4–27.1) | 23.6% (21.4–25.9) |
| High school | 26.8% (24.8–28.8) | 27.1% (24.9–29.5) |
| Some college | 29.3% (27.2–31.4) | 29.5% (27.0–32.2) |
| ≥College | 18.8% (17.0–20.6) | 19.7% (17.5–22.1) |
|
| ||
| Body mass index (Kg/M2) | ||
| Normal | 27.9% (26.0–29.9) | 26.9% (24.7–29.3) |
| Overweight | 37.4% (35.3–39.6) | 37.4% (35.0–40.0) |
| Obesity | 34.6% (32.6–36.8) | 35.6% (32.9–38.4) |
|
| ||
| Have health insurance | 92.0% (90.7–93.1) | 91.7% (90.0–93.1) |
|
| ||
| Self-reported ulcer | 16.6% (15.0–18.3) | 16.5% (14.6–18.6) |
| Self-reported arthritis3 | 50.7% (48.2–53.1) | 50.8% (48.0–53.6) |
| Self-reported hypertension | 67.1% (64.9–69.2) | 66.1% (63.4–68.7) |
| Self-reported diabetes mellitus | 30.4% (28.4–32.6) | 29.8% (27.2–32.6) |
| Self-reported high blood cholesterol | 66.1% (64.0–68.1) | 67.9% (65.4–70.4) |
|
| ||
| Smoker | 19.7% (17.9–21.6) | 18.1% (16.2–20.2) |
|
| ||
| Number of risk factors4 | ||
| 0 | 10.6% (9.2–12.2) | 10.1% (8.5–11.9) |
| 1 | 25.8% (23.8–27.9) | 26.9% (24.5–29.5) |
| 2 | 36.8% (34.7–38.9) | 37.0% (34.5–39.7) |
| 3 | 23.8% (21.7–25.9) | 23.2% (20.7–25.9) |
| 4 | 3.1% (2.4–3.9) | 2.8% (2.0–3.8) |
An adult's eligibility to take low-dose aspirin is determined by either having been told by a health professional that s/he have coronary heart disease and/or stroke, or having been told by a health professional that s/he has coronary heart disease.
Data source: CDC/NCHS, National Health Interview Survey, 2012
Arthritis included arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia
Include hypertension, diabetes, high blood cholesterol and smoking
Figure 1.
National Health Interview Survey Low-dose Aspirin Questions and Associated Sample Sizes
CHD: coronary heart disease
LDA: low dose aspirin
*% was estimated based on sampling weight
The total percentage of low-dose aspirin use for secondary prevention included those following a health professional's advice to take low-dose aspirin and those taking low-dose aspirin on their own. Overall, crude percentages of low-dose aspirin use were 70% and 73% for those with coronary heart disease and/or stroke and coronary heart disease only, respectively. Table 2 shows the age-standardized percentages of low-dose aspirin use by population characteristics for those with coronary heart disease and/or stroke, as well as those with coronary heart disease only.
Table 2.
Age-Standardized Prevalence of Low-dose Aspirin Use1 Among Adults Aged 40 and Over Eligible2 to Take Low-dose Aspirin for Secondary Prevention of Cardiovascular Disease, by Definition of Atherosclerotic Cardiovascular Disease and Demographic and Health Characteristics, United States, 20123
| Coronary Heart Disease and/or Stroke n=3,068 | Coronary Heart Disease Only n=2,007 | |||
|---|---|---|---|---|
|
| ||||
| % (95% CI) | p-value4 | % (95% CI) | p-value | |
| Total | 62.2% (56.0–68.0) | 67.3% (59.9–74.0) | ||
|
| ||||
| Sex | ||||
| Men | 69.1% (60.8–76.3) | Reference | 73.1% (62.8–81.3) | Reference |
| Women | 55.3% (46.6–63.8) | <0.05 | 60.5% (50.1–70.0) | <0.05 |
|
| ||||
| Race/Ethnicity | ||||
| Non-Hispanic White | 65.5% (57.0–73.2) | Reference | 71.6% (61.2–80.2) | Reference |
| Non-Hispanic Black | 59.3% (47.2–70.3) | NS | 55.9% (38.9–71.6) | NS |
| Hispanic | 50.6% (38.6–62.6) | <0.05 | 53.9% (39.7–67.5) | <0.05 |
| Other | 60.2% (37.3–79.4) | NS | 77.6% (61.6–88.2) | NS |
|
| ||||
| Education | ||||
| <High school | 67.6% (58.4–75.6) | Reference | 68.6% (55.9–79.1) | Reference |
| High school | 56.1% (43.4–67.9) | NS | 67.9% (53.7–79.5) | NS |
| Some college | 56.0% (43.6–67.8) | NS | 61.0% (45.5–74.6) | NS |
| ≥College | 72.7% (59.3–83.0) | NS | 77.6% (63.8–87.2) | NS |
|
| ||||
| BMI | ||||
| Normal | 64.8% (52.6–75.4) | Reference | 63.4% (46.9–77.2) | Reference |
| Overweight | 65.0% (54.2–74.5) | NS | 68.5% (55.5–79.1) | NS |
| Obesity | 58.9% (49.9–67.4) | NS | 69.2% (57.3–79.0) | NS |
|
| ||||
| Insurance Status | ||||
| Yes | 62.6% (55.5–69.2) | Reference | 67.6% (59.0–75.2) | Reference |
| No | 56.2% (42.2–69.3) | NS | 57.4% (41.7–71.7) | NS |
|
| ||||
| Ulcer | ||||
| Yes | 61.9% (50.3–72.4) | Reference | 73.3% (55.4–85.2) | Reference |
| No | 62.4% (55.2–69.0) | NS | 66.2% (57.9–73.7) | NS |
|
| ||||
| Arthritis5 | ||||
| Yes | 61.2% (51.1–70.4) | Reference | 67.5% (53.8–78.8) | Reference |
| No | 62.8% (55.2–69.8) | NS | 66.9% (57.9–74.7) | NS |
|
| ||||
| Number of cardiovascular disease risk factors6 | ||||
| 0 | 37.6% (27.9–48.3) | Reference | 43.8% (27.5–61.7) | Reference |
| 1 | 53.5% (43.0–63.8) | <0.05 | 61.8% (47.7–74.1) | NS |
| 2 | 64.3% (54.1–73.3) | <0.001 | 68.7% (56.7–78.9) | <0.05 |
| 3 | 73.9% (61.7–83.2) | <0.001 | 77.4% (65.0–86.8) | <0.001 |
| 4 | 91.0% (88.4–94.6) | <0.001 | 94.0% (86.4–97.5) | <0.001 |
Including following health care provider's advice to take low-dose aspirin or independently taking low-dose aspirin
An adult's eligibility to take low-dose aspirin is determined by either having been told by a health professional that s/he have coronary heart disease and/or stroke, or having been told by a health professional that s/he has coronary heart disease.
Data source: CDC/NCHS, National Health Interview Survey, 2012
P-values are for comparisons across the categories using reference group, NS – not significant
Arthritis included arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia
Included self-reported hypertension, high blood cholesterol, diabetes and smoking
Table 3 shows that after controlling for all other demographic and risk factors, low-dose aspirin use was significantly less prevalent among those aged 40–64 years (versus ≥65 years), women (versus men), non-Hispanic black and Hispanic (versus non-Hispanic white). The linear relationship between the number of cardiovascular risk factors and low-dose aspirin use persisted after adjusting for other factors (OR=1.39 [95% CI=1.23–1.57], P<0.001 for coronary heart disease and stroke) and (OR=1.33 [95% CI=1.16–1.54], P<0.001 for coronary heart disease only). Health insurance status, level of education, BMI, and history of ulcers or arthritis were not related to low-dose aspirin use among those with coronary heart disease and/or stroke or coronary heart disease only (Table 3).
Table 3.
Adjusted Prevalence Ratio of Low-dose Aspirin Use Among Adults Aged 40 and Over Eligible1 to Take Low-dose Aspirin for Secondary Prevention of Cardiovascular Disease, by Definition of Atherosclerotic Cardiovascular Disease and Demographic and Health Characteristics, United States, 20122
| Coronary Heart Disease and/or Stroke n=3,068 Adjusted prevalence ratio (95% CI) | Coronary Heart Disease Only n=2,007 Adjusted prevalence ratio (95% CI) | |
|---|---|---|
| Age (years) | ||
| 40–64 | 0.89 (0.82–0.96) | 0.87 (0.80–0.95) |
| ≥65 | Reference | Reference |
|
| ||
| Sex | ||
| Men | Reference | Reference |
| Women | 0.91 (0.85–0.97) | 0.90 (0.84–0.98) |
|
| ||
| Race | ||
| NH-White | Reference | Reference |
| NH-Black | 0.91 (0.83–0.99) | 0.88 (0.78–0.99) |
| Hispanics | 0.83 (0.72–0.95) | 0.84 (0.72–0.97) |
| Others | 0.90 (0.78–1.05) | 1.05 (0.94–1.18) |
|
| ||
| Education | ||
| <High school | Reference | Reference |
| High school | 0.96 (0.88–1.05) | 0.97 (0.88–1.07) |
| Some college | 0.97 (0.88–1.05) | 0.99 (0.90–1.09) |
| ≥College | 1.08 (0.99–1.18) | 1.07 (0.96–1.18) |
|
| ||
| BMI | ||
| Normal | Reference | Reference |
| Overweight | 1.07 (0.99–1.16) | 1.11 (1.00–1.23) |
| Obesity | 1.07 (0.99–1.15) | 1.12 (1.01–1.23) |
|
| ||
| Have Insurance | ||
| Yes | Reference | Reference |
| No | 0.92 (0.79–1.07) | 0.87 (0.74–1.03) |
|
| ||
| Ulcer | ||
| Yes | Reference | Reference |
| No | 0.97 (0.89–1.04) | 0.97 (0.88–1.06) |
|
| ||
| Arthitis3 | ||
| Yes | Reference | Reference |
| No | 0.99 (0.92–1.06) | 1.00 (0.93–1.08) |
|
| ||
| Number of risk factors4 | ||
| 0 | Reference | Reference |
| 1 | 1.13 (0.96–1.34) | 1.09 (0.91–1.31) |
| 2 | 1.23 (1.05–1.43) | 1.19 (1.00–1.41) |
| 3 | 1.36 (1.15–1.60) | 1.26 (1.05–1.53) |
| 4 | 1.50 (1.28–1.77) | 1.42 (1.18–1.71) |
|
| ||
| Number of risk factor5 odds ratio for linear trend | 1.39 (1.23–1.57) | 1.33 (1.16–1.54 |
An adult's eligibility to take low-dose aspirin is determined by either having been told by a health professional that s/he have coronary heart disease and/or stroke, or having been told by a health professional that s/he has coronary heart disease.
Data source: CDC/NCHS, National Health Interview Survey, 20121. All covariates were in the models simultaneously
Arthritis included arthritis, rheumatoid arthritis, gout, lupus, or fibromyalgia
Tested for a linear trend in the relationship between cardiovascular risk and aspirin use by substituting the number of risk factors as a continuous variable in the model
Tested for a linear trend in the relationship between cardiovascular risk and aspirin use by substituting the number of risk factors as a continuous variable in the model
Discussion
Current guidelines recommend low-dose aspirin for cardiovascular prevention among those with a history of a previous cardiovascular event.3,4,5 Data from this report showed that 76% of adults aged≥40 years with atherosclerotic cardiovascular disease were advised to take low-dose aspirin, and 70% with known atherosclerotic cardiovascular disease were taking low-dose aspirin for secondary prevention. Demographic characteristics and the number of cardiovascular disease risk factors (which included hypertension, diabetes, high blood cholesterol and current smoking) were related to low-dose aspirin use. Those ≥65 years, men, and non-Hispanic whites were significantly more likely to take low-dose aspirin for secondary prevention than younger adults (40–64 years), women, and non-Hispanic blacks or Hispanics. A linear relationship was found between the number of cardiovascular risk factors and low-dose aspirin use.
The benefit of low-dose aspirin in reducing the likelihood of future events among those who have suffered an acute myocardial infarction and stroke has been found in multiple studies. An previous meta-analysis of randomized controlled trials among those with prior myocardial infarction (n=19,791), acute myocardial infarction (n=18,773) and prior stroke (n=11,707), examining the effectiveness of aspirin for prevention of myocardial infarction, stroke or vascular death found that aspirin reduced the risk of a fatal event by 25%, 29% and 24%, respectively.1 More recently, a meta-analysis based on randomized controlled trials found that aspirin use for secondary prevention reduced coronary heart disease and stroke risk by 20% and 19%, respectively.2 In addition to the health benefits found with the use of low-dose aspirin for secondary prevention, other studies have found the recommendations to be cost-effective and to have significant economic benefits.16 Current American Heart Association and the American College of Cardiology guidelines strongly recommend aspirin use for survivors of acute myocardial infarctions or those with coronary or other atherosclerotic vascular disease to prevent event recurrence or death.3,4,5
In this study, the prevalence of overall low-dose aspirin use for secondary prevention among adults with coronary heart disease and/or stroke was 70%, and was slightly higher among those with coronary heart disease only (73%). Other studies have found varying levels of aspirin use for secondary prevention, depending on the health care setting surveyed. A recent report from an international outpatient registry (REduction of Atherothrombosis for Continued Health [REACH]) found that about 70% of patients with established atherothrombotic disease were using aspirin9, and among those not using aspirin, 50% were using anticoagulants or other antiplatelet agents.9 A clinical database of patients who had undergone a cardiac procedure and documented coronary heart disease found “consistent use” of aspirin to be 71% in 2002.17 A recent reported based on national survey found that among office visits to primary care physicians and cardiologists where aspirin or other antiplatelet medication was eligible to adults aged ≥18 years with ischemic vascular disease, 54% had documented prescriptions for aspirin or other antiplatelet medications.18 Of note, estimates of low-dose aspirin use immediately after cardiovascular disease event have been found to be significantly higher. For example, the American Heart Association's Get With the Guidelines-Coronary Artery Disease and American College of Cardiology's Acute Coronary Treatment and Intervention Outcomes Network registry found that prescribed of recommended aspirin use at hospital discharge for acute coronary syndrome increased from 94% in 2006 to 98% in 2012.19 However, each of these reports has used data from healthcare settings, and limited information is available on the general U.S. population, highlighting the importance of this study.
An important finding from our study was the impact of the health professional's advice on low-dose aspirin use. Among those with atherosclerotic cardiovascular disease who were advised to take low-dose aspirin, nearly 90% reported following the advice. Among those who were not following the advice, about half had been advised to stop taking low-dose aspirin. In contrast, among those who were not advised to take low-dose aspirin, but were potentially eligible for it (about 24% of the eligible population), only about one in ten were taking low-dose aspirin on their own. This suggests that there is opportunity for healthcare providers to reassess the use of low-dose aspirin in patients with a history of cardiovascular disease.
Several prevalent conditions are potential contraindications for low-dose aspirin use. For those with arthritis, who are likely to utilize non-steroidal anti-inflammatory drugs for their condition, previous data have shown they may be less likely to have aspirin prescribed due to potential medication interactions.20,21 Those with a history of ulcers may also be less likely to take low-dose aspirin due to the negative gastric effects.22,23 However, our analyses found no significant differences in the percentages of low-dose aspirin use between adults with and without a history of these conditions.
There were several limitations identified in this study. First, all data were obtained by self-report, and there could be potential recall bias. This may be particularly relevant for a non-prescription medication such as aspirin, as those with a history of cardiovascular disease may have a complex medical regimen and recall of a non-prescription medication may present a challenge. In addition, the chance of recall bias increases when asking to recall whether he/she was advised to take aspirin – the patients might not recall what their doctors told them, or on purpose to deny that they were told to avoid the embracement of not doing what they were advised by their doctors. Second, the NHIS does not collect information about the type of stroke (hemorrhagic or ischemic). It is possible that the prevalence of low-dose aspirin use in the eligible population is underestimated when the eligible population includes adults who have had a hemorrhagic stroke, for which aspirin is not recommended. However, it is worth noting that additional analysis including those with coronary heart disease only had similar results. Third, we were not able to asses the use of other antiplatelet medications. Finally, NHIS does not include questions about other types of atherosclerotic cardiovascular disease, such as transient ischemic attack or peripheral vascular disease.
In this survey of community-dwelling adults, about two-thirds of the eligible populations were taking low-dose aspirin. While a portion (approximately 5%) of the population was advised to stop taking low-dose aspirin by their healthcare providers, about 24% of the eligible population had not been advised to take low-dose aspirin. When low-dose aspirin was recommended by a healthcare provider, 9 in 10 adults receiving the recommendations took low-dose aspirin. Improving aspirin use for cardiovascular prevention among those who would benefit from it is one of goals of the Million Hearts® initiative, in which clinical and community-based efforts are needed to enhance the use of aspirin for cardiovascular prevention and reduce mortality from heart disease.
Acknowledgments
Funding source: N/A
Footnotes
Publisher's Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Collaborative overview of randomized trials of antiplatelet therapy—I: Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists' Collaboration. BMJ. 1994;308:81–106. [PMC free article] [PubMed] [Google Scholar]
- 2.Antithrombotic Trialists' (ATT) Collaboration Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomized trials. Lancet. 2009;373:1849–1860. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith SC, Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, Gibbons RJ, Grundy SM, Hiratzka LF, Jones DW, Lloyd-Jones DM, Minissian M, Mosca L, Peterson ED, Sacco RL, Spertus J, Stein JH, Taubert KA. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 4.Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA, American Heart Association Stroke Council, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 5.Eikelboom JW, Hirsh J, Spencer FA, Baglin TP, Weitz JI. Antiplatelet drugs: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e89S–119S. doi: 10.1378/chest.11-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krumholz HM, Radford MJ, Ellerbeck EF, Hennen J, Meehan TP, Petrillo M, Wang Y, Jencks SF. Aspirin for secondary prevention after acute myocardial infarction in the elderly: prescribed use and outcomes. Ann Intern Med. 1996;124:292–298. doi: 10.7326/0003-4819-124-3-199602010-00002. [DOI] [PubMed] [Google Scholar]
- 7.Lewis WR, Peterson ED, Cannon CP, Super DM, LaBresh KA, Quealy K, Liang L, Fonarow GC. An organized approach to improvement in guideline adherence for acute myocardial infarction: results with the Get With The Guidelines quality improvement program. Arch Intern Med. 2008;168:1813–1819. doi: 10.1001/archinte.168.16.1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xian Y, Pan W, Peterson ED, Heidenreich PA, Cannon CP, Hernandez AF, Friedman B, Holloway RG, Fonarow GC, GWTG Steering Committee and Hospitals Are quality improvements associated with the Get With the Guidelines-Coronary Artery Disease (GWTG-CAD) program sustained over time? A longitudinal comparison of GWTG-CAD hospitals versus non-GWTG-CAD hospitals. Am Heart J. 2010;159:207–214. doi: 10.1016/j.ahj.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Cannon CP, Rhee KE, Califf RM, Boden WE, Hirsch AT, Alberts MJ, Cable G, Shao M, Ohman EM, Steg PG, Eagle KA, Bhatt DL, REACH Registry Investigators Current use of aspirin and antithrombotic agents in the United States among outpatients with atherothrombotic disease (from the REduction of Atherothrombosis for Continued Health [REACH] Registry) Am J Cardiol. 2010;105:445–452. doi: 10.1016/j.amjcard.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Soni A. Statistical Brief. Agency for Healthcare Research and Quality Medical Expenditure Survey; Rockville, MD: 2005. Aspirin Use among the Adult Noninstitutionalized Population, with and without Indicators of Heart Disease, 2005; p. 179. [Google Scholar]
- 11.CDC Recommended use of aspirin and other antiplatelet medications among adults -- National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey, United States, 2005–2008. MMWR. 2012;61(Suppl):11–18. [PubMed] [Google Scholar]
- 12.Klein RJ, Schoenborn CA. Healthy People Statistical Notes. National Center for Health Statistics; Hyattsville, MD: 2001. Age adjustment using the 2000 projected U.S. population; p. 20. [PubMed] [Google Scholar]
- 13.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171:618–623. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 14.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the National Health Interview Survey, 2006–2015. National Center for Health Statistics. Vital Health Stat. 2014;2(165) [PubMed] [Google Scholar]
- 15.Frane J. SUDAAN: Professional Software for Survival Data Analysis. Research Triangle Institute; Research Triangle Park, NC: 1989. [Google Scholar]
- 16.Ademi Z, Liew D, Hollingsworth B, Steg PG, Bhatt DL, Reid CM, REACH Registry Investigators Is it cost-effective to increase aspirin use in outpatient settings for primary or secondary prevention? Simulation data from the REACH Registry Australia Cohort. Cardiovasc Ther. 2013;31:45–52. doi: 10.1111/j.1755-5922.2011.00291.x. [DOI] [PubMed] [Google Scholar]
- 17.Newby LK, Allen LaPointe NM, Chen AY, Kramer JM, Hammill BG, DeLong ER, Muhlbaier LH, Califf RM. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation. 2006;113:203–212. doi: 10.1161/CIRCULATIONAHA.105.505636. [DOI] [PubMed] [Google Scholar]
- 18.CDC Million Hearts: Prevalence of Leading Cardiovascular Disease Risk Factors — United States, 2005–2012. MMWR. 2014;63(21):462–467. [PMC free article] [PubMed] [Google Scholar]
- 19.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Judd SE, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Mackey RH, Magid DJ, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, 3rd, Moy CS, Mussolino ME, Neumar RW, Nichol G, Pandey DK, Paynter NP, Reeves MJ, Sorlie PD, Stein J, Towfighi A, Turan TN, Virani SS, Wong ND, Woo D, Turner MB, American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.MacDonald TM, Wei L. Effect of ibuprofen on cardioprotective effect of aspirin. Lancet. 2003;361:573–574. doi: 10.1016/s0140-6736(03)12509-3. [DOI] [PubMed] [Google Scholar]
- 21.Kimmel SE, Berlin JA, Reilly M, Jaskowiak J, Kishel L, Chittams J, Strom BL. The effects of nonselective non-aspirin non-steroidal anti-inflammatory medications on the risk of nonfatal myocardial infarction and their interaction with aspirin. J Am Coll Cardiol. 2004;43:985–990. doi: 10.1016/j.jacc.2003.08.064. [DOI] [PubMed] [Google Scholar]
- 22.Weil J, Colin-Jones D, Langman M, Lawson D, Logan R, Murphy M, Rawlins M, Vessey M, Wainwright P. Prophylactic aspirin and risk of peptic ulcer bleeding. BMJ. 1995;310:827–830. doi: 10.1136/bmj.310.6983.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park K, Bavry AA. Aspirin: Its risks, benefits, and optimal use in preventing cardiovascular events. Cleveland Clinical J Med. 2013;80:318–326. doi: 10.3949/ccjm.80a.12146. [DOI] [PubMed] [Google Scholar]