Summary
Although short sleep duration is related to chronic conditions such as hypertension, diabetes, and obesity, the association with stroke is less well-known. Using 2006-2011 National Health Interview Surveys, we assessed the association between self-reported duration of sleep and prevalence of stroke stratifying by age and sex. Of the 154,599 participants aged 18 years or older, 29.2%, 61.8% and 9.0% reported they sleep ≤6, 7-8 and ≥9 hours per day, respectively. Corresponding age-standardized prevalence of stroke were 2.78%, 1.99% and 5.21% (P < 0.001). Logistic regression models showed a higher prevalence of stroke among those who slept ≤6 or ≥9 hours a day compared with those who slept 7-8 hours, after adjusting for sociodemographic, behavioral, and health characteristics. Further stratifying by age and sex showed that the association of duration of sleep and stroke differed among different age or sex groups. Among young adults (18-44 years), a higher prevalence of stroke was found among women with short sleep. Higher prevalence of stroke was found among middle-aged men and women reporting short or long sleep duration. Among older adults (≥65 years), higher prevalence of stroke was found only among those who slept ≥9 hours. In this national sample of adults, the association between duration of sleep and stroke varied by sex and age. Although there was an association of short sleep duration with stroke, we also observed the association of long sleep duration with stroke, especially among those aged 65 years or older.
Keywords: sleep duration, stroke, age, sex, NHIS
During the past few decades, the proportion of American adults who sleep less than 7 hours per day increased from 22%-23% in 1985 (Williams et al., 1985) to 28% in 2005-2007 (Schoenborn and Adams, 2010). In addition, earlier studies showed that short sleep duration is related to increased risk of diabetes, obesity, hypertension, coronary heart disease, and stroke (Gangwisch et al., 2005; Ayas et al., 2003; Ayas et al., 2003; Gottlieb et al., 2005; Fang et al., 2012; Sabanayagam and Shankar, 2010; Amagi et al., 2010). In 2008, stroke was the fourth leading cause of death in the United States (Miniño et al., 2011) and one of the leading causes of severe long-term disability for those who survived stroke (Go et al., 2013). Previous studies reported the association between duration of sleep and risk of stroke (Sabanayagam and Shankar, 2010; Amagi et al., 2010; Qureshi et al., 1997), but no study has explored the association of duration of sleep and prevalence of stroke among different age and sex groups.
To assess the effects of age and sex on the association between duration of sleep and stroke, we measured the association between duration of sleep and prevalence of history of stroke by using data from a large national surveillance system.
Methods
Data
The National Health Interview Survey (NHIS) is an annual multistage probability survey conducted by the National Center for Health Statistics (NCHS) at the Centers for Disease Control and Prevention (CDC) (Adams et al., 2009). The participants are a nationally representative sample of the civilian, noninstitutionalized U.S. population. The survey was conducted in person in either English or Spanish. For those who speak other languages, interpreters were available to conduct the interview. To increase the sample size for this study, we combined 6 years of survey data (2006-2011). The final response rate for the Adult Sample Person component for these 6 years of surveys ranged from 60.8% (2010) to 70.8% (2006). Detailed information on the survey design and methods can be found at the NHIS Web site (http://www.cdc.gov/nchs/nhis.htm).
Self-reported daily sleep duration was obtained through the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents reported hours of sleep in whole numbers from 1 to 24. Responses ranged from 3 to 24 hours. The National Institutes of Health recommends 7-8 hours of sleep per day for healthy adults (www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch.html). Therefore, sleep duration was categorized as short (6 or fewer hours), recommended/referent (7-8 hours), or long (9 or more hours per day). Self-reported history of stroke was defined if the respondents answered “yes” to the question, “Have you ever been told by a doctor or other health professional that you had a stroke?”
Other characteristics included sociodemographic variables: age (18-44, 45-64, and ≥65 years); sex; race/ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic other, and Hispanic); and level of education (less than high school graduate, high school graduate or equivalent, some college, and college graduate). Behavioral characteristics included smoking status (former, current, never) and alcohol intake (nondrinker [<12 drinks in entire life], former drinker [no drinks in previous year], moderate drinker [≤7 drinks per week for women or ≤14 drinks per week for men], heavy drinker [>7 drinks per week for women or > 14 drinks per week for men]). Physical activity was determined by total leisure-time aerobic physical activity based on current guidelines and was categorized as active (≥150 minutes per week of moderate-intensity equivalent leisure-time aerobic activity), insufficiently active (10-149 minutes per week of moderate-intensity equivalent leisure-time aerobic activity), and inactive (<10 minutes per week of any aerobic physical activity) (USDHHS, 2009). Health status variables included body mass index (BMI), as calculated by using self-reported weight and height (BMI, kg/m2: underweight, <18.5; normal weight, 18.5-24.9; overweight, 25-29.9; obese, ≥30) and self-reported chronic conditions, including diabetes (“Have you ever been told that you have diabetes?”), hypertension (“Have you ever had hypertension on 2 or more visits?”), and coronary heart disease (“Have you ever been told you had coronary heart disease?”, “Have you ever been told you had angina pectoris?” and “Have you ever been told you had a heart attack?”).
Data analysis
Sociodemographic, behavioral, and health condition characteristics were assessed by sleep duration group (≤6, 7-8, and ≥9 hours). Age-adjusted prevalence of history of stroke was determined for each sleep duration group. Further stratifying by age (18-44, 45-64, and ≥65 years) and sex, prevalence of history of stroke was determined for each subgroup (18-44 years-men, 45-64 years-men, ≥65 years-men, 18-44 years-women, 45-64 years-women, and ≥65 years-women).
Logistic regression models were employed to calculate the crude prevalence ratio (PR) and 95% confidence interval (CI) for the likelihood of stroke associated with short (≤6 hours) or long (≥9 hours) duration of sleep relative to a reference category of 7-8 hours. We then adjusted for age, sex, race/ethnicity, and education. Additional adjustment included behavioral characteristics (smoking status, alcohol intake, physical activity) and health conditions (overweight/obesity, diabetes, hypertension, and coronary heart disease). For each age and sex stratification group, crude and adjusted logistic regression models were conducted to assess the association between hours of sleep and history of stroke.
NHIS complex sampling design was accounted for in all analyses by using SAS-callable SUDAAN statistical software version 9.2 (Research Triangle Institute, Research Triangle Park, North Carolina) (Frane, 1989). All statistical tests were based on 2-tailed tests. Statistical significance was determined if P < 0.05. Any standard error larger than 30% relative to the estimate was considered to produce unreliable estimates.
Results
During 2006-2011, among 154,599 participants, 29.2%, 61.8%, and 9.0% of adults aged 18 years or older reported that they usually slept 6 or fewer, 7-8, and 9 or more hours per day, respectively. The characteristics of the study population for each sleep duration group are presented in Table 1. Those who slept 6 or fewer hours were more likely to be aged 45-64 years, non-Hispanic black, a current smoker, and obese than those who slept 7-8 hours. Adults who slept 9 or more hours a day were more likely to be aged 65 years or older, female, have a lower level of education, be a former drinker or never drinker, report no physical activity, and more likely to have diabetes, hypertension, and coronary heart disease than those who slept 7-8 hours.
Table 1. Prevalence (standard error) of self-reported habitual sleep duration* by characteristics of adult participants—National Health Interview Survey, 2006-2011.
| Sleep duration (hours per day) | P-value¶ | ||||
|---|---|---|---|---|---|
| ≤6 hours | 7-8 hours | ≥9 hours | |||
| Participants (N) | 154,599 | 45,121 | 95,619 | 13,859 | |
| Age (years) | 18-44 | 49.1 (0.34) | 49.7 (0.32) | 44.6 (0.62) | <0.001 |
| 45-64 | 37.7 (0.33) | 34.4 (0.25) | 25.0 (0.48) | ||
| ≥65 | 13.2 (0.22) | 16.0 (0.22) | 30.5 (0.52) | ||
| Sex | Men | 48.7 (0.28) | 48.7 (0.22) | 44.8 (0.51) | <0.001 |
| Women | 51.3 (0.28) | 51.3 (0.22) | 55.2 (0.51) | ||
| Race/ethnicity† | White | 66.8 (0.45) | 70.1 (0.35) | 69.2 (0.61) | <0.001 |
| Black | 14.9 (0.35) | 10.1 (0.22) | 13.0 (0.45) | ||
| Hispanic | 12.5 (0.28) | 14.2 (0.27) | 13.7 (0.43) | ||
| Other | 5.8 (0.16) | 5.6 (0.17) | 4.2 (0.23) | ||
| Education level | <High school | 18.5 (0.29) | 16.5 (0.24) | 27.6 (0.54) | <0.001 |
| High school | 24.9 (0.27) | 24.3 (0.24) | 29.4 (0.48) | ||
| Some college | 32.8 (0.29) | 29.3 (0.24) | 26.5 (0.47) | ||
| College graduate | 23.9 (0.37) | 30.0 (0.34) | 16.5 (0.47) | ||
| Smoking | Never | 53.5 (0.33) | 61.3 (0.26) | 52.8 (0.58) | <0.001 |
| Former | 21.3 (0.25) | 21.4 (0.21) | 24.9 (0.43) | ||
| Current | 25.2 (0.30) | 17.4 (0.20) | 22.3 (0.44) | ||
| Alcohol‡ | Never | 18.7 (0.28) | 22.2 (0.28) | 26.7 (0.55) | <0.001 |
| Former | 16.0 (0.24) | 13.2 (0.17) | 20.2 (0.43) | ||
| Moderate | 59.8 (0.34) | 59.6 (0.28) | 47.1 (0.54) | ||
| Heavy | 5.7 (0.15) | 5.0 (0.10) | 6.1 (0.28) | ||
| Physical activity§ | None | 36.7 (0.41) | 32.9 (0.40) | 45.8 (0.58) | <0.001 |
| Inadequate | 19.8 (0.27) | 20.0 (0.20) | 19.3 (0.41) | ||
| Adequate | 43.4 (0.37) | 47.2 (0.36) | 34.9 (0.56) | ||
| BMI‖ | Underweight | 1.8 (0.08) | 1.7 (0.05) | 2.9 (0.17) | <0.001 |
| Normal | 31.7 (0.31) | 37.9 (0.24) | 37.5 (0.55) | ||
| Overweight | 34.7 (0.29) | 35.6 (0.19) | 31.5 (0.52) | ||
| Obese | 32.1 (0.31) | 24.9 (0.21) | 28.1 (0.51) | ||
| Diabetes# | No | 90.3 (0.17) | 92.6 (0.12) | 86.8 (0.33) | <0.001 |
| Yes | 9.7 (0.17) | 7.4 (0.12) | 13.2 (0.33) | ||
| Hypertension# | No | 72.9 (0.31) | 77.5 (0.21) | 67.4 (0.50) | <0.001 |
| Yes | 27.1 (0.31) | 22.5 (0.21) | 32.6 (0.50) | ||
| CHD# | No | 93.0 (0.15) | 94.7 (0.10) | 88.0 (0.33) | <0.001 |
| Yes | 7.0 (0.15) | 5.3 (0.10) | 12.0 (0.33) | ||
Self-reported habitual sleep duration per day was obtained through the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents reported in 1-hour increments. The variable ranged from 3 to 24 hours and was categorized as ≤6, 7-8 and ≥9 hours per day.
P-values were 2-sided based on comparison between hours of sleep and characteristics.
Race/ethnicity categories are non-Hispanic white, non-Hispanic black, non-Hispanic other, and Hispanics.
Alcohol intake (nondrinker [<12 drinks in entire life], former drinker [no drinks in previous year], moderate drinker [≤7 drinks per week for women or ≤14 drinks per week for men], heavy drinker [>7 drinks per week for women or > 14 drinks per week for men]).
Physical activity was determined by total leisure-time aerobic physical activity based on current guidelines and categorized as active (≥150 minutes per week of moderate-intensity equivalent leisure-time aerobic activity), insufficiently active (10-149 minutes per week of moderate-intensity equivalent leisure-time aerobic activity), and inactive (<10 minutes per week of any aerobic physical activity).
Body mass index (BMI) was calculated using self-reported weight and height (BMI, kg/m2: underweight was defined as BMI<18.5, normal weight BMI=18.5-24.9, overweight BMI=25-29.9, obese BMI≥30).
Self-reported chronic conditions (diabetes, hypertension, and coronary heart disease [CHD]).
The age-adjusted prevalence estimates of self-reported history of stroke were 2.78%, 1.99%, and 5.21% for those who reported sleeping 6 or fewer, 7-8, and 9 or more hours, respectively (P < 0.001). Table 2 shows crude and adjusted prevalence ratios for the likelihood of having stroke for each sleep duration group, using 7-8 hours of sleep as the referent. Prevalence ratios were first adjusted for age, sex, race/ethnicity, and level of education (Model 1). Additional adjustment included behavioral characteristics (Model 2) and then chronic health conditions (Model 3). Overall, there was significantly increased prevalence of stroke among adults who slept 6 or fewer hours (prevalence ratio [PR] = 1.20, 95% CI = 1.11-1.29), as well as those who slept 9 or more hours (PR = 1.80, 95% CI = 1.63-1.99) compared with those who slept 7-8 hours after considering all characteristics in the final multivariable model.
Table 2. Age-adjusted prevalence* of history of stroke† and prevalence ratios‡ (95% confidence intervals) for the likelihood of stroke by habitual sleep duration§, National Health Interview Survey, 2006-2011.
| Sleep duration (hours per day) | |||
|---|---|---|---|
| ≤6 hours | 7-8 hours | ≥9 hours | |
| Participants (N) | 45,121 | 95,619 | 13,859 |
| Stroke (n) | 1,403 | 2,268 | 1,008 |
| Prevalence* (%) | 2.78 (2.63-2.95) | 1.99 (1.88-2.09) | 5.21 (4.79-5.67) |
| Crude PR | 1.37 (1.27-1.47) | 1.00 | 3.43 (3.12-3.77) |
| Adjusted PR1 | 1.36 (1.26-1.46) | 1.00 | 2.33 (2.11-2.56) |
| Adjusted PR2 | 1.29 (1.19-1.39) | 1.00 | 2.11 (1.91-2.32) |
| Adjusted PR3 | 1.20 (1.11-1.29) | 1.00 | 1.80 (1.63-1.99) |
Age-standardized prevalence estimates use the U.S. 2000 standard projected population.
Self-reported stroke was defined if the respondents answered “yes” to the question: “Have you ever been told by a doctor or other health professional that you had a stroke?”
Prevalence ratios (PR) include crude PR and adjusted PR where Adjusted PR1 adjusted for age, sex, race/ethnicity and education; Adjusted PR2 adjusted for variables from Adjusted PR model 1, plus smoking status, alcohol intake, and physical activity; and Adjusted PR3 adjusted for variables from Adjusted PR model 2, plus body mass index, hypertension, coronary heart disease, and diabetes status.
Self-reported habitual sleep duration per day was obtained through the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents reported in 1-hour increments. The variable ranged from 3 to 24 hours and was categorized as ≤6, 7-8, and ≥9 hours per day.
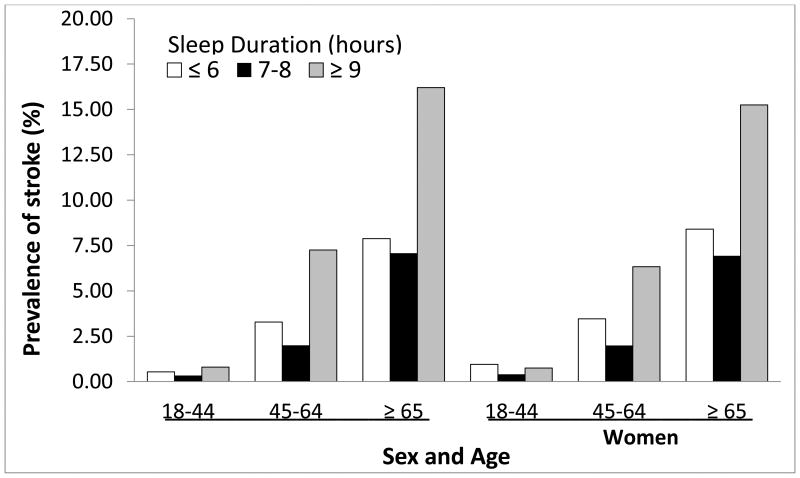
This U-shaped relationship between sleep duration and crude prevalence of history of stroke was observed for groups stratified by age and sex (Figure 1). Table 3 presents crude and adjusted prevalence ratios for stroke by sleep duration among groups stratified by age and sex. Among younger adults (18-44 years), short sleep duration was associated with stroke among women but not men. Long sleep duration was not associated with stroke among either men or women in this age group, which might be caused by the low prevalence of stroke in this group. Among middle-aged adults (45-64 years), for both men and women, we found similar associations as those overall—those who slept 6 or less or 9 or more hours showed higher prevalence of stroke after full adjustment. Among the eldest (≥65 years), 6 or fewer hours of sleep per day was not associated with a prevalence of history of stroke, although the prevalence was higher for those who slept 9 or more hours. This association was observed for both men and women.
Figure 1. Prevalence* of history of stroke‡ by sleep duration§ by sex and age groups - National Health Interview Survey, 2006-2011.
*Self-reported sleep duration per day was obtained through the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents reported in 1-hour increments. The variable ranged from 3 to 24 hours and was categorized as ≤6, 7-8, and ≥9 hours per day.
‡Self-reported history of stroke was defined if the respondents answered “yes” to the question: “Have you ever been told by a doctor or other health professional that you had a stroke?”
§Self-reported sleep duration per day was obtained through the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents reported in 1-hour increments. The variable ranged from 3 to 24 hours and was categorized as ≤6, 7-8, and ≥9 hours per day.
Table 3. Prevalence* of history of stroke† and prevalence ratios‡ (95% confidence interval) for the likelihood of stroke by habitual sleep duration§, for groups defined by age and sex, National Health Interview Survey, 2006-2011.
| Sleep duration (hours per day) | |||
|---|---|---|---|
| ≤6 hours | 7 or 8 hours | ≥9 hours | |
| Men 18-44 years | |||
| Participants | 9,813 | 20,750 | 2,134 |
| Stroke (n) | 59 | 64 | 20 |
| Prevalence (%) | 0.54 (0.40-0.73) | 0.33 (0.26-0.74) | 0.80 (0.48-1.30) |
| Crude PR | 1.61 (1.09-2.37) | 1.00 | 2.38 (1.35-4.17) |
| Adjusted PR1 | 1.48 (1.00-2.19) | 1.00 | 1.88 (1.08-3.28) |
| Adjusted PR2 | 1.41 (0.95-2.08) | 1.00 | 1.78 (1.00-3.18) |
| Adjusted PR3 | 1.11 (0.74-1.66) | 1.00 | 1.68 (0.95-2.94) |
| Men 45-64 years | |||
| Participants | 7,478 | 14,593 | 1,499 |
| Stroke (n) | 254 | 340 | 113 |
| Prevalence (%) | 3.28 (2.83-3.79) | 2.00 (1.76-2.27) | 7.25 (5.76-9.08) |
| Crude PR | 1.64 (1.35-1.99) | 1.00 | 3.63 (2.81-4.68) |
| Adjusted PR1 | 1.53 (1.26-1.86) | 1.00 | 3.10 (2.38-4.03) |
| Adjusted PR2 | 1.40 (1.14-1.72) | 1.00 | 2.55 (1.95-3.33) |
| Adjusted PR3 | 1.23 (1.01-1.52) | 1.00 | 2.06 (1.57-2.70) |
| Men ≥65 years | |||
| Participants | 2,663 | 7,486 | 2,066 |
| Stroke (n) | 217 | 546 | 321 |
| Prevalence (%) | 7.88 (6.75-9.18) | 7.08 (6.38-7.84) | 16.20 (14.33-18.26) |
| Crude PR | 1.11 (0.93-1.33) | 1.00 | 2.29 (1.96-2.67) |
| Adjusted PR1 | 1.08 (0.90-1.29) | 1.00 | 2.16 (1.85-2.52) |
| Adjusted PR2 | 1.07 (0.89-1.28) | 1.00 | 2.02 (1.73-2.36) |
| Adjusted PR3 | 1.04 (0.87-1.24) | 1.00 | 1.78 (1.52-2.08) |
| Women 18-44 years | |||
| Participants | 11,334 | 24,804 | 3,360 |
| Stroke (n) | 108 | 106 | 24 |
| Prevalence (%) | 0.95 (0.76-1.18) | 0.40 (0.32-0.50) | 0.75 (0.45-1.24) |
| Crude PR | 2.37 (1.72-3.25) | 1.00 | 1.86 (1.08-3.22) |
| Adjusted PR1 | 2.21 (1.62-3.02) | 1.00 | 1.59 (0.92-2.75) |
| Adjusted PR2 | 1.99 (1.44-2.74) | 1.00 | 1.45 (0.82-2.56) |
| Adjusted PR3 | 1.65 (1.18-2.29) | 1.00 | 1.24 (0.69-2.22) |
| Women 45-64 years | |||
| Participants | 9,072 | 17,090 | 1,971 |
| Stroke (n) | 345 | 410 | 133 |
| Prevalence (%) | 3.46 (3.09-3.86) | 1.99 (1.75-2.26) | 6.33 (4.98-8.03) |
| Crude PR | 1.74 (1.48-2.05) | 1.00 | 3.19 (2.43-4.18) |
| Adjusted PR1 | 1.54 (1.30-1.82) | 1.00 | 2.68 (2.02-3.56) |
| Adjusted PR2 | 1.39 (1.17-1.65) | 1.00 | 2.34 (1.77-3.10) |
| Adjusted PR3 | 1.24 (1.05-1.48) | 1.00 | 1.84 (1.37-2.46) |
| Women ≥65 years | |||
| Participants | 4,761 | 10,896 | 2,829 |
| Stroke (n) | 420 | 802 | 397 |
| Prevalence (%) | 8.40 (7.48-9.41) | 6.93 (6.36-7.56) | 15.25 (13.77-16.86) |
| Crude PR | 1.21 (1.05-1.40) | 1.00 | 2.20 (1.94-2.50) |
| Adjusted PR1 | 1.16 (1.01-1.34) | 1.00 | 2.08 (1.83-2.37) |
| Adjusted PR2 | 1.12 (0.97-1.29) | 1.00 | 1.91 (1.68-2.16) |
| Adjusted PR3 | 1.07 (0.92-1.23) | 1.00 | 1.68 (1.47-1.91) |
Age-standardized prevalence estimates use the U.S. 2000 standard projected population.
Self-reported stroke was defined if the respondents answered “yes” to the question: “Have you ever been told by a doctor or other health professional that you had a stroke?”
Prevalence ratios (PR) include crude PR and adjusted PR where Adjusted PR1 adjusted for age, sex, race/ethnicity and education; Adjusted PR2 adjusted for variables from Adjusted PR model 1, plus smoking status, alcohol intake, and physical activity; and Adjusted PR3 adjusted for variables from Adjusted PR model 2, plus body mass index, hypertension, coronary heart disease, and diabetes status.
Self-reported habitual sleep duration per day was obtained through the question, “On average, how many hours of sleep do you get in a 24-hour period?” Respondents reported in 1-hour increments. The variable ranged from 3 to 24 hours and was categorized as ≤6, 7-8, and ≥9 hours per day.
Discussion
The National Institutes of Health recommends 7-8 hours of sleep per day for healthy adults (www.nhlbi.nih.gov/health/health-topics/topics/sdd/howmuch.html). Yet we found that more than 29% of U.S. adults slept 6 or fewer hours and 9% reported sleeping 9 or more hours. Although the main finding of this study suggested that 6 or fewer or 9 or more hours of sleep were associated with a higher prevalence of history of stroke among adults overall, after stratifying by age and sex, similar associations were observed among middle-aged populations only. Among those aged 65 years or older, long sleep duration was associated with higher prevalence of history of stroke, whereas short sleep duration was not. Among young adults, no associations of short or long sleep duration and prevalence of history of stroke were noted among men. Among young women, however, less than 7 hours sleep was associated with prevalence of stroke.
The association of sleep duration and prevalence of stroke has been assessed in earlier studies. By using 2005 NHIS, a report showed a U-shaped association between sleep duration and cardiovascular events. This association existed for both myocardial infarction and stroke (Sabanayagam and Skanhar, 2010). Stratifying by age, sex, race/ethnicity, and obesity status, the association between sleep duration and total cardiovascular disease persisted (Sabanayagam and Skanhar, 2010). A cohort study of Japanese adults aged 40-49 years with 10 years follow-up showed that by using 7 hours sleep as reference, 6 or fewer hours of sleep was associated with total cardiovascular events, but not stroke, for men only (Amagai et al., 2010). Another study of Japanese men (aged 35-54 years) with 14 years follow-up revealed similar findings (Hamazaki et al., 2011). In a mortality follow-up study among 98,634 adults aged 40–79 years with an average of 14 years follow-up, there were 1,964 deaths from stroke. Compared with those who had reported 7 hours sleep and after adjusting for demographic, behavioral, and clinical characteristics, an increased risk of ischemic stroke death was observed among those who had reported 10 or more hours. There was no significant increased risk of death from stroke for shorter sleep durations (Ikehara et al., 2009).
The current study, which uses a nationally representative U.S. sample, was able to examine the association of sleep duration and prevalence of history of stroke by age and sex subgroups by merging 6 years of data. The study showed that short sleep duration was associated with higher prevalence of stroke only among those aged less than 65 years. However, long sleep duration was associated with higher prevalence of stroke among men and women aged 45 years or older. Among younger adults (18-44 years), short sleep duration was associated with stroke among women, but not men. However, further study is needed to determine the mechanism by age and sex.
Cross-sectional surveys, such as NHIS, cannot determine the directionality of the association. The observed association between short or long sleep durations and stroke could be caused by either short or long durations of sleep contributing to stroke or the history of stroke affecting the sleep duration. There were studies reporting that short or long durations of sleep were related to stroke. For example, short duration of sleep resulted in disturbances in endocrine and metabolic functions (Spiegel et al., 1999; Van Cauter e et al., 2007) and increased blood pressure (Kato et al., 2000; Kario et al., 2000), as observed with sleep deprivation. Short sleep duration has also been found to increase inflammatory markers an important marker for cardiovascular risk (Meier-Ewert et al., 2004). The association of long sleep duration with increased risk of stroke has been reported. The first National Health and Nutrition Examination Survey follow-up data showed that with 10 years follow-up, those who slept more than 8 hours had a 50% higher risk of stroke than those with 6-8 hours of sleep (Qureshi et al., 1997). In addition, long sleep duration may be an early symptom of chronic disease (Hamazaki et al., 2011), such as underlying sleep-disordered breathing (Patel et al., 2004) or poor sleep quality (Suzuki et al., 2009). On the other hand, a history of stroke could affect the hours of sleep from post-stroke fatigue (long duration of sleep) (Choi-Kwon and Kim, 2011; Lerdal et al., 2009) and pain, which could contribute to poor sleep quality, short duration of sleep, or insomnia (Lundström et al., 2009; Naess et al., 2010; Hermann and Bassetti, 2009). Other factors, such as sleep quality or sleep apnea, might affect the association between sleep duration and stroke (Westerlund et al., 2013).
One limitation of using NHIS data was the reliance on self-reported variables. In this study, both duration of sleep and history of stroke were reported by the participants. Early studies have shown good agreement between self-reported hours of sleep and those obtained through actigraphic monitoring (Lockley et al., 1999). An earlier study had concluded that self-reported stroke from a questionnaire can be used to assess the prevalence of stroke in epidemiological studies (Engstad et al., 2000). In addition, the study included only stroke patients who could participate in the survey; thus self-selected bias may be present. Individuals in long term care facilities, as well as those who died of stroke were not included. Furthermore, the cross-sectional design of NHIS prevented us from determining if there was a causal relationship between sleep duration and stroke.
In conclusion, self-reported stroke prevalence was higher for adults with short (≤6 hours) or long (≥9 hours) sleep durations compared with 7-8 hours, varying by age. Among those aged 65 years or older, no association between short sleep duration and prevalence of stroke was observed. Further longitudinal epidemiologic studies are needed to assess the causation between duration of sleep and stroke. The fact that the association with sleep duration varied by age suggests intervention opportunities for different age groups. In addition, there is a need for further epidemiologic research to examine the risk of stroke and other aspects of sleep (besides sleep duration), such as sleep quality or sleep disorders, as well as the risk and health effects of long duration of sleep.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Disclosures: No conflicts of interest for all authors
Author Contributorship: Jing Fang was responsible for obtaining data, analysis and drafting.
Jing Fang, Anne Wheaton, and Carma Ayala contributed the study design and participated in developing methods.
Jing Fang, Anne Wheaton, and Carma Ayala edited the manuscript.
References
- Adams PF, Barnes PM, Vickerie JL. Vital Health Stat. Vol. 10. National Center for Health Statistics; 2008. Summary health statistics for the U.S. population: National Health Interview Survey, 2007; pp. 1–104. [PubMed] [Google Scholar]
- Amagai Y, Ishikawa S, Gotoh T, Kayaba K, Nakamura Y, Kajii E. Sleep duration and incidence of cardiovascular events in a Japanese population: the Jichi Medical School cohort study. J Epidemiol. 2010;20:106–110. doi: 10.2188/jea.JE20090053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayas NT, White DP, Al-Dalaimy WK, et al. A prospective study of self- and incident diabetes in women. Diabetes Care. 2003;26:380–384. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163:205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- Choi-Kwon S, Kim JS. Poststroke fatigue: an emerging, critical issue in stroke medicine. Int J Stroke. 2011;6:328–336. doi: 10.1111/j.1747-4949.2011.00624.x. [DOI] [PubMed] [Google Scholar]
- Engstad T, Bonaa KT, Viitanen M. Validity of self-reported stroke: the Tromso Study. Stroke. 2000;31:1602–1607. doi: 10.1161/01.str.31.7.1602. [DOI] [PubMed] [Google Scholar]
- Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens. 2012;25:335–341. doi: 10.1038/ajh.2011.201. [DOI] [PubMed] [Google Scholar]
- Frane J. SUDAAN: Professional Software for Survival Data Analysis. Research Triangle Institute; Research Triangle Park, NC: 1989. [Google Scholar]
- Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield S. Inadequate sleep as a risk factor for obesity: analysis of the NHANES I. Sleep. 2005;28:1265–1272. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e6–245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb DJ, Punjabi NM, Newman AB, et al. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch Intern Med. 2005;165:863–867. doi: 10.1001/archinte.165.8.863. [DOI] [PubMed] [Google Scholar]
- Hamazaki Y, Morikawa Y, Nakamura K, et al. The effects of sleep duration on the incidence of cardiovascular events among middle-aged male workers in Japan. Scand J Work Environ Health. 2011;37:411–417. doi: 10.5271/sjweh.3168. [DOI] [PubMed] [Google Scholar]
- Hermann DM, Bassetti CL. Sleep-related breathing and sleep-wake disturbances in ischemic stroke. Neurology. 2009;73:1313–1322. doi: 10.1212/WNL.0b013e3181bd137c. [DOI] [PubMed] [Google Scholar]
- Ikehara S, Iso H, Date C, et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:295–301. doi: 10.1093/sleep/32.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kario K, Schwartz JE, Pickering TG. Changes of nocturnal blood pressure dipping status in hypertensives by nighttime dosing of adrenergic blocker, doxazosin: results from the HALT study. Hypertension. 2000;35:787–794. doi: 10.1161/01.hyp.35.3.787. [DOI] [PubMed] [Google Scholar]
- Kato M, Phillips BG, Sigurdsson G, Narkiewicz K, Pesek CA, Somers VK. Effects of sleep deprivation on neural circulatory control. Hypertension. 2000;35:1173–1175. doi: 10.1161/01.hyp.35.5.1173. [DOI] [PubMed] [Google Scholar]
- Lerdal A, Bakken LN, Kouwenhoven SE, et al. Poststroke fatigue--a review. J Pain Symptom Manage. 2009;38:928–949. doi: 10.1016/j.jpainsymman.2009.04.028. [DOI] [PubMed] [Google Scholar]
- Lockley SW, Skene DJ, Arendt J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. J Sleep Res. 1999;8:175–183. doi: 10.1046/j.1365-2869.1999.00155.x. [DOI] [PubMed] [Google Scholar]
- Lundström E, Smits A, Terént A, Borg J. Risk factors for stroke-related pain 1 year after first-ever stroke. Eur J Neurol. 2009;16:188–193. doi: 10.1111/j.1468-1331.2008.02378.x. [DOI] [PubMed] [Google Scholar]
- Meier-Ewert HK, Ridker PM, Rifai N, et al. Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol. 2004;43:678–683. doi: 10.1016/j.jacc.2003.07.050. [DOI] [PubMed] [Google Scholar]
- Miniño AM, Murphy SL, Xu J, Kochanek KD. Deaths: Final data for 2008. Natl Vital Stat Rep. 2011;59:1–126. [PubMed] [Google Scholar]
- Naess H, Lunde L, Brogger J, Waje-Andreassen U. Post-stroke pain on long-term follow-up: the Bergen stroke study. J Neurol. 2010;257:1446–1452. doi: 10.1007/s00415-010-5539-y. [DOI] [PubMed] [Google Scholar]
- Patel SR, Ayas NT, Malhotra MR, et al. Prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology. 1997;48:904–911. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- Sabanayagam C, Shankar A. Sleep duration and cardiovascular disease: results from the National Health Interview Survey. Sleep. 2010;33:1037–1042. doi: 10.1093/sleep/33.8.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenborn CA, Adams PF. Health behaviors of adults: United States, 2005-2007. Vital Health Stat 10. 2010;245:1–132. [PubMed] [Google Scholar]
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- Suzuki E, Yorifuji T, Ueshima K, et al. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: A population-based cohort study. Prev Med. 2009;19:135–141. doi: 10.1016/j.ypmed.2009.06.016. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. Physical Activity Guidelines Advisory Committee Report. Hyattsville, MD: 2008. [Google Scholar]
- Van Cauter E, Holmback U, Knutson K, et al. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007;67:2–9. doi: 10.1159/000097543. [DOI] [PubMed] [Google Scholar]
- Westerlund A, Bellocco R, Sundström J, Adami HO, Akerstedt T, Trolle Lagerros Y. Sleep characteristics and cardiovascular events in a large Swedish cohort. Eur J Epidemiol. 2013;28:463–473. doi: 10.1007/s10654-013-9802-2. [DOI] [PubMed] [Google Scholar]
- Williams GD, Dufour M, Bertolucci D. Drinking levels, knowledge, and associated characteristics, 1985 NHIS findings. Public Health Rep. 1986;101:593–598. [PMC free article] [PubMed] [Google Scholar]