Abstract
Purpose: This study examined the effects of a physical activity (PA) intervention for young adult cancer survivors on changes in self-efficacy, social support, and self-monitoring and determined whether changes in these social cognitive theory constructs mediated the relationship between the intervention and changes in PA.
Methods: A 12-week randomized trial compared a Facebook-based intervention (FITNET) aimed at increasing moderate-to-vigorous intensity PA to a Facebook-based self-help comparison group. Young adult cancer survivors (N=86, aged 21–39) were randomly assigned to one of the two groups. Self-report measures of PA and psychosocial variables were collected at baseline and after 12 weeks.
Results: The FITNET group reported lower self-efficacy for sticking to exercise (mean change=−0.38; 95% CI: −0.62 to −0.12; p=0.025) and social support from friends on social networking websites (mean change=−0.47; 95% CI: −1.45 to 0.65; p=0.039) relative to the self-help comparison group over time. Changes in social support from friends on social networking websites partially mediated the intervention effects on moderate-to-vigorous PA (mean indirect effect=−22.4; 95% CI: −62.0 to −2.8) in the unexpected direction. Across both groups, social support from friends and self-monitoring were positively associated with changes in moderate-to-vigorous PA.
Conclusion: The proposed mediators did not explain the positive effects of the FITNET intervention on mild PA. The lack of significant improvements in psychosocial constructs among FITNET participants may partly explain why the intervention did not increase moderate-to-vigorous PA relative to the self-help comparison group. Future PA interventions with young adult cancer survivors should examine targeting social support from friends and self-monitoring.
Keywords: : physical activity, behavioral intervention, mediation, social networking website, Facebook, psychosocial determinants
Physical activity (PA) has several benefits for cancer survivors, including improving fatigue and physical functioning and lowering diabetes and cardiovascular disease risks, for which cancer survivors are at increased risk.1–8 Among young adult cancer survivors (YACS) aged 18–39 and diagnosed as young adults, PA has been shown to improve depression, stress, and quality of life.9 Despite these benefits, most young adults diagnosed with cancer before or during young adulthood are not adhering to the American Cancer Society's PA guidelines of 150 minutes/week for cancer survivors.2,9–12 Therefore, PA interventions represent important opportunities to promote health and quality of life in YACS.13–15
YACS have expressed interest in PA interventions and preferences for online health interventions,10,16 yet limited evidence exists to guide the development of effective online PA interventions for this population. In designing PA interventions, many researchers use health behavior theories, such as social cognitive theory (SCT).17,18 SCT emphasizes that behavior is a function of a dynamic and reciprocal interaction of personal factors, behavior, and environmental influences. Self-efficacy, self-regulation, and environmental factors (e.g., social support) are key determinants of behavior described by SCT that have been targeted in several PA interventions.19–22 In the context of PA, SCT suggests that a supportive environment may enhance individuals' self-efficacy (i.e., confidence in one's ability to perform exercise and to overcome barriers to exercise in specific settings) and in turn promote self-regulation (i.e., skills for personal regulation of goal-setting, planning, and self-monitoring) to effect behavior change.
Although theory-based interventions targeting SCT constructs have effectively increased PA among cancer survivors,23–26 few studies have examined mediators of intervention effects or SCT constructs among cancer survivors.26–33 Thus, secondary analyses of intervention studies are needed to elucidate mechanisms of PA behavior change and guide future interventions. In a previous study, we used SCT to develop a 12-week social networking website (SNS)-based PA intervention for YACS who were ages 21–39. The Fostering Improvement Through Networking and Exercising Together (FITNET)34 intervention targeted self-efficacy, social support, and self-monitoring as potential mediators of PA. The FITNET intervention group significantly increased self-reported mild PA by 164 minutes/week compared to 29 minutes/week in the self-help comparison group. Both groups reported over 160 minutes/week of moderate-to-vigorous PA (MVPA), with no significant differences between the groups at 12 weeks. The goals of the current secondary analyses were to evaluate the effects of the FITNET intervention on theoretical constructs and to determine if changes in these constructs mediated the relationship between the FITNET intervention and PA behaviors. We hypothesized that changes in self-efficacy, social support, and self-monitoring would mediate intervention effects on change in PA minutes/week over time.
Methods
Participants
YACS were recruited through cancer organizations and advertisements on social media (e.g., Facebook). Eligibility criteria included: 21–39 years old at study, diagnosed with cancer (excluding non-melanoma skin cancer) while aged 18–38, ≥1 year beyond diagnosis date with no evidence of progressive disease or second cancers, completed cancer treatment (no minimum time from completion), English-speaking, no medical condition(s) precluding unsupervised exercise, exercising <150 MVPA minutes/week,2 and having internet access and an active Facebook account. In this study, we chose to exclude YACS under age 21 for two primary reasons: first, because as many 18–20 year olds are attending college and as such their needs and psychosocial development may differ from older young adults, and second, because of potential concerns about the discussion of alcohol among individuals younger than the United States' legal drinking age of 21.35 We expected that YACS aged 21–39 might have more psychosocial and developmental experiences in common with each other that could be shared through participation in the Facebook groups. All participants were screened through an online questionnaire and gave online informed consent. All study communication took place online, and all participants were from North America. Eighty-six participants completed the online baseline questionnaire and 66 (76.7%) completed the post-intervention questionnaire after 12 weeks.
Procedures
The FITNET intervention aimed to increase participants' MVPA levels to ≥150 minutes/week, as recommended for cancer survivors by the American Cancer Society,2 with a focus on walking. After completing the baseline questionnaire, participants were randomly assigned using a computer-generated random numbers list to one of two Facebook-based arms: FITNET intervention or self-help comparison. Both groups participated during the same 12-week study period, received a pedometer (Yamax Digi-Walker; Tokyo, Japan), and joined their respectively assigned Facebook group. Study methods were previously described in detail elsewhere.34 Briefly, intervention participants received 12 weekly Facebook messages with skill-building lessons (e.g., self-monitoring, enlisting social support) and links to publicly available websites. To promote self-efficacy, intervention participants additionally had access to a study website with weekly goal-setting and feedback charts on their progress. The website included a PA log feature to enhance self-monitoring. The study administrator posted weekly discussion prompts to the Facebook group wall to elicit social support (e.g., questions about participants' cancer experiences). The self-help comparison group also received 12 weekly Facebook messages with general exercise information and website links, but they did not have access to the self-monitoring website and were not prompted to interact within their Facebook group. After 12 weeks, participants completed another online questionnaire. Study procedures were approved by the Institutional Review Board of the University of North Carolina at Chapel Hill.
Measures
Demographics and health. Age at study entry, race/ethnicity, education, marital status, income, smoking behavior, cancer type, date of diagnosis, treatment types, height, and weight were collected at baseline.
Physical activity was measured using a modified version of the Godin Leisure-Time Exercise Questionnaire (GLTEQ),36 which asks participants about the frequency and average duration of vigorous, moderate, and mild (light activities such as easy walking) exercise during the previous week. The GLTEQ has demonstrated reliability and concurrent validity among various populations.37–39 PA minutes/week and three PA measures were computed—MVPA (the sum of moderate and vigorous exercise) and mild and total PA minutes/week.
Self-efficacy for PA was assessed using the Self-Efficacy and Exercise Habits Survey.40 Eleven items asked participants to “rate how confident you are that you could really motivate yourself to do things like these consistently, for at least six months (e.g., get up early, even on weekends, to exercise);” responses ranged from 1 (“I know I cannot”) to 5 (“I know I can”). All 11 items were scored to comprise two factors validated in prior work40—sticking to it (mean of 8 items) and making time (mean of 3 items)—which demonstrated good–high reliability at both baseline and post-intervention (sticking to it: α=0.90; making time: α=0.68–0.71).
Social support for exercise was assessed with items adapted from the Social Support and Exercise Survey,41 which asks about the frequency of friends' actions directed to the individual in the past month (e.g., “gave me helpful reminders to exercise”). We adapted the scale to include three subscales (5 items each) about support from family, friends (excluding friends on SNS), and friends on SNS (i.e., all communications from friends via SNS, which may have included fellow study group members if participants considered them friends). Item responses ranged from 1 (“none”) to 5 (“very often”). We computed four social support measures (family, friends, SNS friends, and total) by summing respective items. Internal consistencies were high for all measures (α=0.89–0.94). As a process measure in the post-intervention survey, participants rated social support during the past month from other members of their study group (same 5 items as above).
Self-monitoring was measured using the 10-item Exercise Goal-Setting Scale42 and two items adapted from the self-monitoring subscale of the Self-Management Scale43 (e.g., “I record my exercise activities in a written or online record”). Participants reported how much statements described themselves on a scale from 1 (“does not describe) to 5 (“describes completely”). Item scores were averaged to yield a total self-monitoring score, which demonstrated excellent internal consistency (α=0.92–0.94). The total number of goals set, PA log entries, and steps entries by intervention participants were collected from the study website as objective measures of self-monitoring.
Statistical analyses
Analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC) according to intention-to-treat principles with baseline observations carried forward for participants missing post-intervention data (n=20); we also conducted sensitivity analyses to examine consistency of these findings from analyses of study completers.44 PA data outliers (FITNET: n=3; SC: n=2) were adjusted to be one unit lower than the next highest reported measure.45,46 To compare groups on changes in SCT constructs, we conducted mixed model analyses with repeated measures to estimate outcomes at baseline and follow-up and to test for group differences in changes over time. Changes in PA were calculated using residualized change scores by regressing the post-intervention PA measure on the baseline PA measure. We similarly calculated residualized change scores for SCT constructs.
Mediation analyses examined if changes in SCT constructs mediated the FITNET intervention effects on changes in PA. We used bootstrapping methods47 and the product-of-coefficient test to evaluate significance of the mediated effect,48 a recommended approach for non-normally distributed data and small samples sizes.49,50 Using a macro by Preacher and Hayes,51 we computed a series of multiple regression models by regressing PA change on the intervention variable (total effect of intervention on PA), change scores of potential mediators on the intervention condition (α), and PA change on the intervention condition while controlling for potential mediators (β, direct effect of intervention on PA). Using 5000 bootstrap samples, indirect effects, bias-corrected estimates of the standard error, and 95% confidence intervals (CI) for the indirect effect were generated. The indirect effect was considered significant at α=0.05 when the 95% CI excluded zero. If there was no intervention effect on changes in a potential mediator, we conducted linear regression analyses with the total sample to examine whether changes in SCT constructs were associated with changes in PA. We conducted Spearman rank correlations to explore the relationship between reported self-monitoring at follow-up and objectively measured self-monitoring among intervention completers.
Results
Table 1 shows baseline sample demographics. There were no differences between the groups on baseline characteristics or baseline PA, except that FITNET intervention participants reported higher daily Facebook use (p<0.05). Adjustment for baseline Facebook use did not alter findings from unadjusted analyses, and results from complete-case analyses were consistent with intention-to-treat analyses. Thus, data are presented from unadjusted intention-to-treat analyses.
Table 1.
Baseline Characteristics of Participants in the FITNET Trial
| Characteristics | FITNET intervention (n=45) | Self-help comparison (n=41) |
|---|---|---|
| Age (years), mean (SD) | 30.8 (5.7) | 32.7 (4.2) |
| Female, % | 91.1 | 90.2 |
| Non-Hispanic White, % | 93.3 | 87.8 |
| Married or living as married, % | 46.7 | 53.7 |
| ≥College graduate, % | 80.0 | 75.6 |
| Annual income ≥$50,000, % | 55.6 | 56.1 |
| Employed full-time, % | 44.4 | 48.8 |
| Body mass index (kg/m2), mean (SD) | 28.4 (8.2) | 29.1 (8.9) |
| Cigarette use (% smokers), % | 20.0 | 29.3 |
| ≥3 hours daily internet use, % | 55.6 | 65.9 |
| Daily Facebook use,a mean (SD) | 2.6 (1.4) | 2.0 (1.0) |
| MVPA (minutes/week), mean (SD) | 109.3 (125.0) | 118.4 (126.3) |
| Mild PA (minutes/week), mean (SD) | 78.3 (91.8) | 81.0 (78.5) |
p<0.05.
FITNET, Fostering Improvement Through Networking and Exercising Together; MVPA, moderate-to-vigorous physical activity; PA, physical activity; SD, standard deviation.
Table 2 presents changes in SCT constructs. FITNET intervention participants reported lower self-efficacy for sticking to exercise over time (mean change=−0.38; p=0.005) relative to self-help comparison participants (p=0.025). Social support from SNS friends differed between groups (p=0.039), with only the self-help comparison group reporting increases in this over time (mean change=1.46; p=0.05). Other SCT constructs did not differ between groups over time. At post-intervention, there was no difference in social support from other Facebook group participants (FITNET: 8.25±4.23 vs. self-help comparison: 9.06±4.18; p=0.437).
Table 2.
Effects of FITNET Intervention on Social Cognitive Theory Constructs
| Variable and possible score range | BaselineaM (SD) | 12 weeksaM (SD) | Mean changebM (95% CI) | Time p | Group×time interactionp |
|---|---|---|---|---|---|
| Self-efficacy—sticking to it (1–5) | 0.025 | ||||
| FITNET | 3.71 (0.86) | 3.33 (0.93) | −0.38 (−0.62 to −0.12) | 0.005 | |
| SC | 3.63 (0.77) | 3.63 (0.83) | −0.01 (−0.20 to 0.20) | 0.944 | |
| Self-efficacy—making time (1–5) | 0.736 | ||||
| FITNET | 3.57 (0.94) | 3.34 (1.06) | −0.23 (−0.48 to 0.03) | 0.079 | |
| SC | 3.61 (0.95) | 3.44 (1.02) | −0.17 (−0.41 to 0.08) | 0.178 | |
| Social support—total (15–75) | 0.597 | ||||
| FITNET | 29.11 (13.12) | 29.13 (10.11) | 0.02 (−2.58 to 2.88) | 0.987 | |
| SC | 30.80 (10.70) | 31.98 (12.20) | 1.17 (−1.81 to 4.46) | 0.455 | |
| Social support—family (5–25) | 0.551 | ||||
| FITNET | 10.56 (5.30) | 10.82 (5.11) | 0.27 (−0.86 to 1.53) | 0.657 | |
| SC | 11.98 (4.92) | 11.68 (5.70) | −0.29 (−1.62 to 1.21) | 0.688 | |
| Social support—friends (5–25) | 0.808 | ||||
| FITNET | 10.18 (5.69) | 10.40 (5.37) | 0.22 (−0.90 to 1.49) | 0.712 | |
| SC | 11.00 (5.76) | 11.00 (5.64) | 0.00 (−1.35 to 1.53) | 1.000 | |
| Social support—SNS friends (5–25) | 0.039 | ||||
| FITNET | 8.38 (5.36) | 7.91 (3.98) | −0.47 (−1.45 to 0.65) | 0.397 | |
| SC | 7.83 (4.24) | 9.29 (5.13) | 1.46 (−0.002 to 3.20) | 0.050 | |
| Self-monitoring (1–5) | 0.479 | ||||
| FITNET | 2.25 (0.81) | 2.44 (0.87) | 0.19 (−0.04 to 0.43) | 0.104 | |
| SC | 2.40 (0.93) | 2.73 (1.06) | 0.33 (0.09 to 0.59) | 0.006 |
Note. Number of participants for all models: FITNET group, n=45; SC group, n=41.
Mean and SD at baseline and 12 weeks are based on raw data.
Mean changes are estimated from mixed model analyses.
FITNET, Fostering Improvement Through Networking and Exercising Together intervention group; SC, self-help comparison group; SD, standard deviation; SNS, social networking website.
Self-efficacy
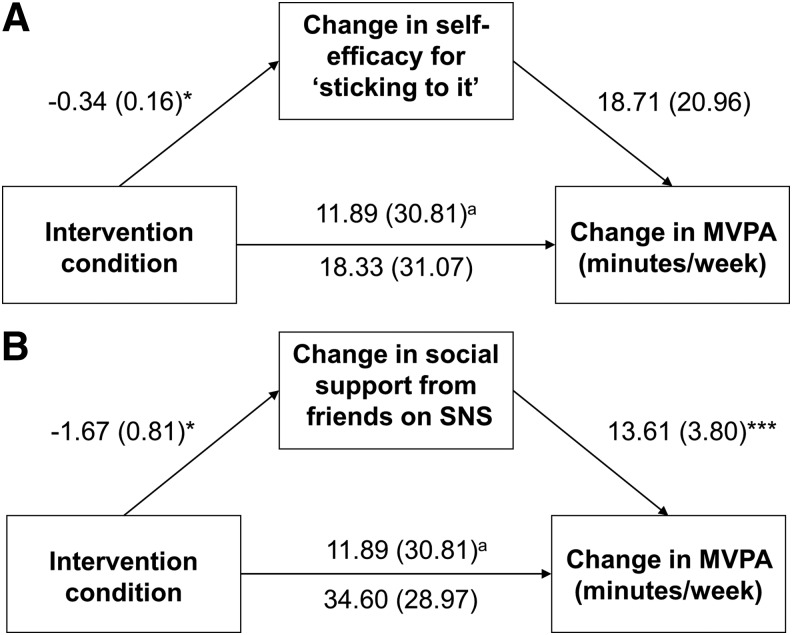
While the FITNET intervention was associated with decreased self-efficacy for “sticking to” PA (α=−0.34; standard error [SE]=0.16; p=0.031), change in self-efficacy was not associated with any PA outcomes (all p>0.05), so there was no evidence of a mediating effect (Fig. 1A). Across groups, changes in self-efficacy for “making time” were not associated with changes in MVPA or in mild or total PA (all p>0.05).
FIG. 1.
Diagrams of models testing residualized changes in psychosocial factors as mediators of the effects of the intervention condition on residualized changes in MVPA minutes per week. (A) Model depicting results of mediation analysis for change in self-efficacy for ‘sticking to it.’ (B) Model depicting results of mediation analysis for change in social support from friends on SNS. Unstandardized regression coefficients are shown with standard errors in parentheses. aCoefficient from model not including the mediator. *p≤0.05; ***p≤0.001. MVPA, moderate-to-vigorous physical activity; SNS, social networking website.
Social support
The FITNET intervention was associated with changes in social support from SNS friends (α=−1.67; SE=0.81; p=0.043), and changes in social support from SNS friends was in turn positively related to MVPA (β=13.61; SE=3.80; p=0.0006) (Fig. 1B). The estimated indirect effect (i.e., the extent to which social support from SNS accounted for the intervention effects on MVPA) indicated that changes in support from SNS friends partially mediated the FITNET intervention effects on changes in MVPA (indirect effect=−22.43; SE=14.51; 95% CI=−62.00 to −2.81). However, support from SNS friends demonstrated inconsistent mediation effects (i.e., the intervention effect on MVPA increased from 11.9 to 34.6 minutes/week when controlling for support from SNS friends).52 Social support from SNS friends was not associated with changes in either mild or total PA, indicating no mediating effects.
Across both groups, changes in MVPA were predicted by changes in total social support (β=6.21; SE=1.65; t=3.77; p=0.0003) and social support from friends (β=10.35; SE=3.68; t=2.82; p=0.006). Both changes in mild PA (β=−27.69; SE=8.12; t=−3.41; p=0.001) and changes in total PA (β=−22.41; SE=11.07; t=−2.02; p=0.046) were negatively associated with changes in family social support.
Self-monitoring
In the total sample, change in self-monitoring was positively related to change in MVPA (β=57.22; SE=19.47; t=2.94; p=0.004), but was not associated with changes in either mild or total PA. Among FITNET intervention completers, self-monitoring at 12 weeks was correlated with the number of PA log entries (rs=0.37; p=0.040), steps entries (rs=0.38; p=0.034), and goals set (rs=0.37; p=0.036) during the 12 weeks.
Discussion
This study examined relationships between a SNS-based PA intervention, changes in theoretical constructs, and changes in PA among YACS. Results did not support our hypotheses that changes in SCT constructs would mediate intervention effects on changes in PA. While the FITNET intervention produced a positive effect on mild PA, the observed increases in mild PA were not explained through the proposed mediation mechanisms. Changes in some SCT constructs were associated with changes in the amount of MVPA across groups. Social support from SNS friends was positively related to changes in MVPA. Unexpectedly, self-help comparison participants reported increased social support from SNS friends while FITNET intervention participants did not. As a result, the indirect effect of the intervention through social support from SNS friends may have attenuated increases in MVPA among FITNET intervention participants.
Social support—other than SNS support—did not mediate FITNET intervention effects on PA as anticipated. While intervention lessons taught strategies to enlist support from friends and family, the FITNET intervention was not associated with improvements in total, family, or friend social support relative to the self-help comparison group. However, our findings are consistent with other PA interventions for cancer survivors that have targeted but found no intervention effects of social support for PA.31,33 While the FITNET intervention was not related to total or friend social support, changes in these factors were related to changes in MVPA over time in the total sample as predicted by SCT.
The intervention strategies used did not appear to increase social support from friends on SNS in general; FITNET intervention participants reported no change in this social support, while self-help comparison participants reported an increase. It is possible that participants varied in their interpretation of the questions about friends on SNS to include other study group participants or friends made within their study group. However, since there was no group difference in the follow-up measure about social support from study group members, we are unable to disentangle the specific effects of study group participants over time on perceptions of social support from SNS friends.
We previously found no group differences in the number of Facebook group posts or use of Facebook group features during the 12-week program,34 suggesting that participants were equally engaged in the social components of the study. Although it is not possible to isolate the effects of specific FITNET intervention components that potentially impacted social support from SNS friends in general (e.g., reading vs. posting comments), the FITNET intervention encouraged participants to utilize Facebook features that facilitate support. For example, the study coordinator posted discussion prompts to encourage interaction within the FITNET intervention Facebook group, while self-help comparison participants engaged in unprompted group discussions. Thus, the increase in social support from SNS friends among the self-help comparison group could reflect perceived support from posts by other study participants in their Facebook group. Since we were unable to determine the relative influences of posting or reading moderator/participant comments on perceived social support and PA outcomes, the factors that contributed to enhanced social support from SNS friends in general remain unclear. As the FITNET intervention did not positively impact social support from SNS friends as anticipated, findings suggest that group interaction prompted by other study participants who share a cancer experience, rather than the study administrator, may be a superior strategy for enhancing social support among YACS.
The finding that the indirect effect of the FITNET intervention through social support from SNS friends resulted in decreased MVPA should be interpreted with caution. Although our social support measures were adapted from a validated scale, they had not been tested in the context of a SNS-delivered study and may not have been applicable to SNS friends in general. For instance, one item asked how often SNS friends “exercised with me,” yet participants may have been geographically constrained from exercising with some SNS friends. This measure may more adequately capture types of support derived through offline means (e.g., instrumental), rather than online SNS (e.g., emotional). Also, exposure to the baseline assessment and lessons on social support may have affected reinterpretation of items measuring social support from SNS friends. For instance, FITNET intervention participants may have had increased awareness about potential deficits in social support at follow-up.53
Taken together with the results on other forms of social support and across both groups, it appears that strategies to enhance social support from friends, whether in-person or on SNS, may facilitate improved PA among YACS. Indeed, YACS have acknowledged a need for interventions offering social support from other YACS and/or friends.16 Therefore, research on social support for exercise, including improved measures and intervention strategies for successfully enlisting support from a variety of sources (e.g., existing friends, cancer groups on SNS), is warranted among YACS.
In a previous study among young adults without cancer, social support influenced self-efficacy, which in turn affected PA.42 In the current study, self-efficacy did not mediate the FITNET intervention effects on PA, possibly due to an insufficient increase in social support. The FITNET intervention had a negative effect on self-efficacy for sticking to exercise relative to the self-help comparison group, which is consistent with other remotely delivered PA interventions for breast cancer survivors32,45 and adolescents in general.54 A possible explanation for our results is that participants, having overcome cancer treatment and potentially life-threatening circumstances, had higher health-related self-efficacy at baseline, and that the intervention may have given them a more accurate perception of their exercise self-efficacy. Alternatively, the decrease in self-efficacy among FITNET intervention participants may be indicative of problems with our intervention strategies, which did not increase social support or target all four factors affecting self-efficacy as outlined by SCT. A systematic review found that interventions that provided feedback on past performance resulted in the highest levels of exercise self-efficacy, while use of persuasion or barrier identification techniques resulted in decreased self-efficacy levels.55 The observed decreases in self-efficacy may reflect low adherence to the study website, which offered feedback on performance, or the use of persuasion in lessons that promoted barrier identification.
The FITNET intervention did not increase self-monitoring in the intervention group relative to the self-help comparison group. However, across groups, changes in self-monitoring were positively associated with PA increases as predicted by SCT and demonstrated in other studies.20–22 The lack of increased social support among FITNET intervention participants may partially explain why no improvements in self-efficacy or self-monitoring were found in the FITNET intervention group relative to the self-help comparison group. The lack of FITNET intervention effects on self-monitoring could be due to both groups receiving a pedometer, FITNET intervention participants more accurately reporting their self-monitoring behaviors (since they accessed the self-monitoring website), and/or self-help comparison group participants possibly over-reporting self-monitoring. Among FITNET intervention group completers, objective self-monitoring at 12 weeks was significantly associated with both the number of goals set and the number of steps entries during the 12 weeks. Without an objective measure to corroborate reported self-monitoring in the self-help comparison group, the FITNET intervention effects on self-monitoring relative to the self-help comparison group are unclear.
Our results should be interpreted with caution, as study limitations include the use of self-reported PA measures, missing data, and the relatively homogeneous sample, which limits study generalizability. While the study may have been underpowered to detect mediational effects, we used robust bootstrapping procedures appropriate for small samples.49 Data on theoretical constructs were collected simultaneously with post-intervention PA data, rather than prior to the final assessment. Additionally, the multicomponent FITNET intervention limited our ability to isolate the effects of individual components on theoretical constructs. Although use of an active self-help comparison group was useful for informing practice, mediation analyses might have more clearly elucidated intervention effects had it been compared to a true control group. Strengths of the study were that it was a longitudinal, randomized controlled trial delivered through a popular existing SNS, which matched participant communication preferences and maximized reach. It is one of the first mediation analyses of PA behavior change among YACS, an understudied group.
Conclusion
This study presents initial evidence on mediators of PA in YACS that participate in a SNS-based intervention study. Findings suggest that the lack of FITNET intervention effects on MVPA may be related to insufficient changes in SCT constructs and partial suppression of effects by social support from SNS friends. This study builds on the limited literature about mediators of PA interventions for YACS and demonstrates a theory-based evaluation of a PA intervention for YACS. Given our current findings and previous evidence, future research should examine how YACS use SNS for social support and then accordingly develop strategies for using SNS to promote healthy behaviors. In designing future PA interventions for YACS, researchers should explore how to better target SCT constructs, including social support and self-monitoring, as improvements in these potential mediators may promote PA engagement. Evaluating PA interventions in larger trials among YACS is also warranted.
Acknowledgments
This study was supported by the UNC Lineberger Cancer Control Education Program (National Cancer Institute funded; R25 CA057726), the UNC Communications for Health Applications and Interventions Core (funded through the Gillings School of Global Public Health Nutrition Obesity Research Center [National Institute of Diabetes and Digestive and Kidney Diseases funded; P30 DK56350] and Lineberger Comprehensive Cancer Center [National Cancer Institute funded; P30 CA16086]), the National Center for Research Resources (UL1RR025747), and a 2011 Society of Behavioral Medicine Distinguished Student Award for Excellence in Research. At the time of the study, the first author was supported by the UNC Cancer Health Disparities Training Program (National Cancer Institute funded; T32 CA128582).
The authors would like to acknowledge the memory of Dr. Marci Campbell, who made substantial contributions to the conception and design of the study and created a legacy that will live on. We also thank Dr. Dianne Ward and Ms. Melissa Crane for their expertise and insightful comments on a draft of this manuscript. We wish to acknowledge Dr. Carey Anders, Dr. William Wood, the community-based organizations, LIVESTRONG, and members of the LIVESTRONG Young Adult Alliance that graciously assisted with study recruitment. Finally, we are most grateful to the young adult cancer survivors who participated in the study.
Disclaimer
Parts of this manuscript were previously presented at the 2012 Annual Meeting of the International Society for Behavioral Nutrition and Physical Activity, May 23–26, 2012 in Austin, and at the 2012 and 2013 Annual Meetings of the Society of Behavioral Medicine, April 11–14, 2012 in New Orleans and March 20–23 in San Francisco, respectively.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.World Cancer Research Fund, American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. Washington, DC: American Institute for Cancer Research; 2007 [Google Scholar]
- 2.Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62(4):242–4 [DOI] [PubMed] [Google Scholar]
- 3.Ballard-Barbash R, Friedenreich CM, Courneya KS, et al. Physical activity, biomarkers, and disease outcomes in cancer survivors: a systematic review. J Natl Cancer Inst. 2012;104(11):815–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmitz KH, Holtzman J, Courneya KS, et al. Controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2005;14(7):1588–95 [DOI] [PubMed] [Google Scholar]
- 5.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee report, 2008. Washington, DC: US Department of Health and Human Services; 2008. Accessed July3, 2014 from: www.health.gov/paguidelines/Report/Default.aspx [Google Scholar]
- 6.Hewitt M, Greenfield S, Stovall E. (Eds). From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academies Press; 2006 [Google Scholar]
- 7.Curtis RE, Freedman DM, Ron E, et al. (Eds). New malignancies among cancer survivors: SEER cancer registries, 1973–2000 (NIH Pub. No. 05-5302). Bethesda, MD: National Cancer Institute; 2006 [Google Scholar]
- 8.Schmitz KH, Courneya KS, Matthews C, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42(7):1409–26 [DOI] [PubMed] [Google Scholar]
- 9.Bélanger LJ, Plotnikoff RC, Clark A, et al. Physical activity and health-related quality of life in young adult cancer survivors: a Canadian provincial survey. J Cancer Surviv. 2011;5(1):44–53 [DOI] [PubMed] [Google Scholar]
- 10.Rabin C, Politi M. Need for health behavior interventions for young adult cancer survivors. Am J Health Behav. 2010;34(1):70–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coups EJ, Ostroff JS. A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med. 2005;40(6):702–11 [DOI] [PubMed] [Google Scholar]
- 12.Bellizzi KM, Rowland JH, Jeffery DD, et al. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005;23(34):8884–93 [DOI] [PubMed] [Google Scholar]
- 13.Demark-Wahnefried W, Rock CL, Patrick K, et al. Lifestyle interventions to reduce cancer risk and improve outcomes. Am Fam Physician. 2008;77(11):1573–8 [PubMed] [Google Scholar]
- 14.Demark-Wahnefried W, Aziz NM, Rowland JH, et al. Riding the crest of the teachable moment: promoting long-term health after the diagnosis of cancer. J Clin Oncol. 2005;23(24):5814–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stull VB, Snyder DC, Demark-Wahnefried W. Lifestyle interventions in cancer survivors: designing programs that meet the needs of this vulnerable and growing population. J Nutr. 2007;137(1 Suppl):S243–8 [DOI] [PubMed] [Google Scholar]
- 16.Rabin C, Simpson N, Morrow K, et al. Intervention format and delivery preferences among young adult cancer survivors. Int J Behav Med. 2013;20(2):304–10 [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52(1):1–26 [DOI] [PubMed] [Google Scholar]
- 18.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986 [Google Scholar]
- 19.Anderson ES, Woicik JR, Winett RA, et al. Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006;25(4):510–20 [DOI] [PubMed] [Google Scholar]
- 20.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: a multivariate approach. Health Psychol. 2008;27(4):409–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lewis BA, Marcus BH, Pate RR, et al. Psychosocial mediators of physical activity behavior among adults and children. Am J Prev Med. 2002;23(2 Suppl):26–35 [DOI] [PubMed] [Google Scholar]
- 22.Rhodes RE, Pfaeffli LA. Mediators of physical activity behaviour change among adult non-clinical populations: a review update. Int J Behav Nutr Phys Act. 2010;7:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rogers LQ, Hopkins-Price P, Vicari S, et al. A randomized trial to increase physical activity in breast cancer survivors. Med Sci Sports Exerc. 2009;41(4):935–46 [DOI] [PubMed] [Google Scholar]
- 24.Demark-Wahnefried W, Clipp EC, Lipkus IM, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25(19):2709–18 [DOI] [PubMed] [Google Scholar]
- 25.Pinto BM, Ciccolo JT. Physical activity motivation and cancer survivorship. Recent Results Cancer Res. 2011;186:367–87 [DOI] [PubMed] [Google Scholar]
- 26.Pinto BM, Floyd A. Methodologic issues in exercise intervention research in oncology. Semin Oncol Nurs. 2007;23(4):297–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pinto BM, Floyd A. Theories underlying health promotion interventions among cancer survivors. Semin Oncol Nurs. 2008;24(3):153–63 [DOI] [PubMed] [Google Scholar]
- 28.Rogers LQ, Shah P, Dunnington G, et al. Social cognitive theory and physical activity during breast cancer treatment. Oncol Nurs Forum. 2005;32(4):807–15 [DOI] [PubMed] [Google Scholar]
- 29.Mosher CE, Fuemmeler BF, Sloane R, et al. Change in self-efficacy partially mediates the effects of the FRESH START intervention on cancer survivors' dietary outcomes. Psychooncology. 2008;17(10):1014–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mosher CE, Lipkus I, Sloane R, et al. Long-term outcomes of the FRESH START trial: exploring the role of self-efficacy in cancer survivors' maintenance of dietary practices and physical activity. Psychooncology. 2013;22(4):876–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rogers LQ, Markwell S, Hopkins-Price P, et al. Reduced barriers mediated physical activity maintenance among breast cancer survivors. J Sport Exercise Psychol. 2011;33(2):235–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rabin C, Pinto BM, Frierson G. Mediators of a randomized controlled physical activity intervention for breast cancer survivors. J Sport Exerc Psychol. 2006;28(3):269–84 [Google Scholar]
- 33.Taylor CLC, deMoor C, Smith MA, et al. Active for Life after Cancer: a randomized trial examining a lifestyle physical activity program for prostate cancer patients. Psychooncology. 2006;15(10):847–62 [DOI] [PubMed] [Google Scholar]
- 34.Valle CG, Tate DF, Mayer DK, et al. A randomized trial of a Facebook-based physical activity intervention for young adult cancer survivors. J Cancer Surviv. 2013;7(3):355–68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gokee-LaRose J, Gorin AA, Wing RR. Behavioral self-regulation for weight loss in young adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 2009;6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–6 [PubMed] [Google Scholar]
- 37.Jacobs DR, Ainsworth BE, Hartman TJ, et al. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25(1):81–91 [DOI] [PubMed] [Google Scholar]
- 38.Miller DJ, Freedson PS, Kline GM. Comparison of activity levels using the Caltrac accelerometer and five questionnaires. Med Sci Sports Exerc. 1994;26(3):376–82 [PubMed] [Google Scholar]
- 39.Sallis JF, Buono MJ, Roby JJ, et al. Seven-day recall and other physical activity self-reports in children and adolescents. Med Sci Sports Exerc. 1993;25(1):99–108 [DOI] [PubMed] [Google Scholar]
- 40.Sallis JF, Pinski RB, Grossman RM, et al. The development of self-efficacy scales for health-related diet and exercise behaviors. Health Educ Res. 1988;3(3):283–92 [Google Scholar]
- 41.Sallis JF, Grossman RM, Pinski RB, et al. The development of scales to measure social support for diet and exercise behaviors. Prev Med. 1987;16(6):825–36 [DOI] [PubMed] [Google Scholar]
- 42.Rovniak LS, Anderson ES, Winett RA, et al. Social cognitive determinants of physical activity in young adults: a prospective structural equation analysis. Ann Behav Med. 2002;24(2):149–56 [DOI] [PubMed] [Google Scholar]
- 43.Petosa PS. Use of social cognitive theory to explain exercise behavior among adults [dissertation]. Columbus, OH: The Ohio State University, School of Education; 1993 [Google Scholar]
- 44.White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011;342:d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vallance JK, Courneya KS, Plotnikoff RC, et al. Randomized controlled trial of the effects of print materials and step pedometers on physical activity and quality of life in breast cancer survivors. J Clin Oncol. 2007;25(17):2352–9 [DOI] [PubMed] [Google Scholar]
- 46.Tabachnick B, Fidell LS. Using multivariate statistics (3rd ed). New York: Harper Collins; 1996 [Google Scholar]
- 47.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002;7(4):422–45 [PubMed] [Google Scholar]
- 48.MacKinnon DP, Lockwood CM, Hoffman JM, et al. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cerin E, Taylor LM, Leslie E, et al. Small-scale randomized controlled trials need more powerful methods of mediational analysis than the Baron–Kenny method. J Clin Epidemiol. 2006;59(5):457–64 [DOI] [PubMed] [Google Scholar]
- 50.Cerin E, MacKinnon DP. A commentary on current practice in mediating variable analyses in behavioural nutrition and physical activity. Public Health Nutr. 2009;12(8):1182–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Res Methods. 2004;36(4):717–31 [DOI] [PubMed] [Google Scholar]
- 52.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baranowski T, Allen DD, Mâsse LC, Wilson M. Does participation in an intervention affect responses on self-report questionnaires? Health Educ Res. 2006;21(Suppl 1):i98–109 [DOI] [PubMed] [Google Scholar]
- 54.Haerens L, Cerin E, Maes L, et al. Explaining the effect of a 1-year intervention promoting physical activity in middle schools: a mediation analysis. Public Health Nutr. 2008;11(5):501–12 [DOI] [PubMed] [Google Scholar]
- 55.Ashford S, Edmunds J, French DP. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br J Health Psychol. 2010;15(Pt 2):265–88 [DOI] [PubMed] [Google Scholar]