Abstract
Background
Instrumented lumbar arthrodesis has been established as the gold standard in the care of patients with degenerative disc disease. However, spinal fusion results in the elimination of motion of the functional spinal unit and has been implicated in the development of adjacent-level degeneration. Motion-preserving devices such as the dynamic rod allow for stabilization of a pathologic motion segment above a fused segment and create a transitional zone (index level) that decreases the loads applied to the supra-adjacent normal segment.
Methods
After institutional review board approval, 28 patients were included in this prospective, consecutive, nonrandomized clinical trial. Each subject was consented for dynamic stabilization. There was no attempt at fusion at the dynamic level. The cohort underwent a posterior lateral spinal fusion with single- or 2-level transforaminal lumbar interbody fusion by use of a cage, with superior-level posterior dynamic instrumentation. Functional clinical outcomes were measured with a 100-point visual analog scale, Oswestry Disability Index, and Short Form 36 questionnaire. Radiographic measurements, fusion evaluation, complications, and screw loosening were recorded.
Results
A minimum of 24 months’ follow-up data included 22 patients. No device failure or screw breakage was identified. Postoperative range of motion averaged 2.5° at the index level, and the superior adjacent-level range of motion remained unchanged (P > .05). Disc height was preserved at all levels (P > .05). Of 180 screws, 6 (3%) showed radiographic loosening. Functional outcomes showed significant improvement in mean postoperative visual analog scale score by 24.7 points (P < .01) and Oswestry Disability Index by 27.6 points (P < .01), as well as the Short Form 36 physical (P < .01) and mental (P < .05) components from baseline to 2-year follow-up.
Conclusions
Our preliminary results at 2 years are satisfactory.
Clinical Relevance
Ultimately, further follow-up will assess the potential for this treatment to delay adjacent-level changes in the long term.
Spinal fusion has been the standard treatment for degenerative disc disease and other degenerative conditions of the spine after failure of nonoperative regimens. Successful instrumented fusions provide immediate stability after decompression and long-term maintenance of correction after reconstruction but also eliminate motion of the segment. More than 25 years ago, Ehni1 stated that “fusion generates a conflict between immediate benefit and late consequences.” With rigid fusion of the lumbar spine motion segment, the cephalad adjacent level undergoes increased loading stresses, an altered lordotic curve, and shifting of the instantaneous axis of rotation (IAR) posteriorly, which causes a nonphysiologic neo-hinge effect.2 These abnormal forces lead to a degenerative process that is well documented and may result in additional surgery.1–11
In their series of 215 lumbar fusion patients, Ghiselli et al.3 reported a predicted rate of reoperation for adjacentlevel disease of 36.1% at 10 years. Gillet4 reported a 37% incidence of adjacent segment changes at greater than 5 years in a series of 106 lumbar fusion patients. It was suggested that “preventative reinforcement” of the adjacent level may be a solution to degeneration of the transitional segment.
Dynamic stabilization is defined as a system that alters the motion and load transmission of the spinal motion segment in such a way as to favor protective physiologic motion and load through that segment without producing a fusion.2 By accomplishing this goal, the objective is not only pain relief but also prevention of damage to the adjacent intervertebral disc and surrounding tissues.5 Recent literature suggests that a window of opportunity exists in which the functional spinal unit (FSU) may be spared from the degenerative cascade if the mechanical loads upon it return to within physiologic range.2, 5,12
Any attempt to preserve motion of the FSU must maintain physiologic quality of motion as well. If an implant does not provide an IAR that is close to the normal physiologic kinematics, then failure of the system will surely result.2 The goal is to restore the IAR as close to that of a normal FSU as possible while limiting the amount of motion and controlling the loads applied to the postsurgical spinal segment. Interpedicular travel is necessary to maintain the IAR in a more physiologic position (Fig. 1).8, 13,14
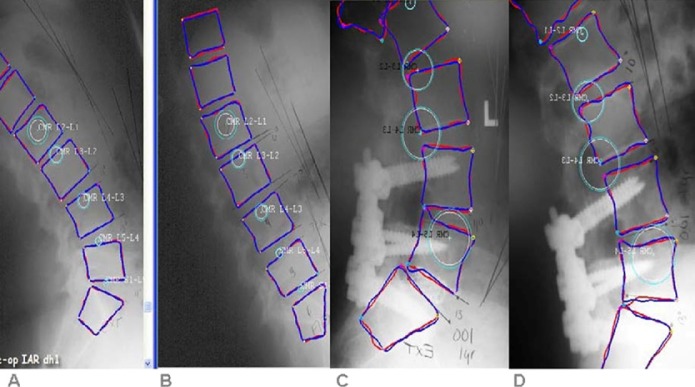
Fig. 1.
In vivo computer analysis of preoperative extension (A) and flexion (B) and postoperative extension (C) and flexion (D) dynamic films that indicates the preservation of the IAR in a more physiologic location (anterior to the posterior longitudinal ligament, albeit not entirely normal).
The dynamic rod provides a transitional zone between the healthy spine and the fused segment by decreasing the abnormal loads applied to the segment supra-adjacent to the index level. The goal of this treatment modality is to decrease adjacent-level disc degeneration and still provide good functional outcomes. This research assesses early functional outcomes and will prospectively study adjacent segment degeneration.
Methods
This study was approved by the hospital institutional review board. There were 28 patients, 17 women and 11 men, with a mean age of 43 years. There are 22 patients with complete 2-year follow-up data. All patients were diagnosed preoperatively with degenerative disc disease of the lumbar spine that resulted in significant back and leg pain for greater than 3 months for which conservative care had failed (Table 1). All patients were consented for dynamic (non-fusion) instrumentation at the index level. No attempt at any fusion was done at the index level. The transverse processes were not exposed, and the facet capsules were preserved. We did not bill the patients’ insurance for a fusion at the index level. Some of these patients had additional pathologic spinal diagnoses such as herniated nucleus pulposus, spondylolisthesis, and spinal stenosis that were recorded anecdotally and followed prospectively. These patients also had appropriate decompressions and laminectomies.
Table 1.
Patient data
| Patient No. | Levels fused | Dynamic rod (index) level | Diagnosis | Prior surgery | Complications | Follow-up completed |
|---|---|---|---|---|---|---|
| 1 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5 Spondylolisthesis at L4-5 Spondylosis at L4-5 |
Dural tear | 24 mo | |
| 2 | L5-S1 | L4-5 | DDD at L4-5 L5-S1 HNP at L5-S1 Stenosis at L5-S1 |
L5-S1 right hemilaminectomy and discectomy | Reflex sympathetic dystrophy | 12 mo |
| 3 | L4-5 | L3-4 | DDD at L4-5, L5-S1 Stenosis at L3-4, L4-5, L5-S1 |
Synovial cyst, I&D, converted to fusion | 24 mo | |
| 4 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5, L5-S1 Stenosis at L4-5 |
Segmental kyphosis at L4-5 | 12 mo | |
| 5 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5, L5-S1 |
Screw lucency at L4 | 24 mo | |
| 6 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L5-S1 Spondylolisthesis at L5-S1 Stenosis at L5-S1 |
L5 laminectomy | I&D | 24 mo |
| 7 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5, L5-S1 Stenosis at L4-5, L5-S1 |
24 mo | ||
| 8 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5 Stenosis at L4-5, L5-S1 |
I&D | 12 mo | |
| 9 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5 Stenosis at L4-5 |
24 mo | ||
| 10 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5 Stenosis at L4-5 |
12 mo | ||
| 11 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 Stenosis at L4-5 |
Radicular pain, reoperated | 24 mo | |
| 12 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 Stenosis at L2-3, L3-4, L4-5, L5-S1 Spondylolysis at L4-5 |
Screw loosening at L4 and L5 | 24 mo | |
| 13 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 Spondylolisthesis at L5-S1 |
Pseudarthrosis, screw loosening at L4 and L5, converted to fusion | 24 mo | |
| 14 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L5-S1 Stenosis at L4-5, L5-S1 |
12 mo | ||
| 15 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 Stenosis at L5-S1 |
24 mo | ||
| 16 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L4-5 |
24 mo | ||
| 17 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 | 24 mo | ||
| 18 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 HNP at L5-S1 |
Re-herniated disc at L4-5 | 24 mo | |
| 19 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 Spondylolisthesis at L5-S1 Stenosis at L4-5 |
24 mo | ||
| 20 | L4-5, L5-S1 | L3-4 | DDD at L3-4, L4-5, L5-S1 | 24 mo | ||
| 21 | L4-5, L5-S1 | L3-4 | DDD at L3-4, L4-5, L5-S1 HNP at L3-4 Stenosis at L3-4, L4-5 |
L4-5 left hemilaminectomy | 12 mo | |
| 22 | L4-5 | L3-4 | DDD at L3-4, L4-5 HNP at L3-4, L4-5 Stenosis at L2-3, L3-4, L4-5, L5-S1 |
L4-5 laminectomy | 24 mo | |
| 23 | L4-5 | L3-4 | DDD at L3-4, L4-5 Spondylolisthesis at L3-4 Stenosis at L4-5 |
24 mo | ||
| 24 | L4-5, L5-S1 | L3-4 | DDD at L3-4, L4-5, L5-S1 HNP at L3-4 Stenosis at L2-3 L3-4, L4-5 L5-S1 |
L4-5, L5-S1 laminectomy and discectomy | ||
| 25 | L3-4, L4-5, L5-S1 | L2-3 | DDD at L2-3, L3-4, L4-5, L5-S1 Stenosis at L2-3, L3-4, L4-5, L5-S1 |
L3-S1 spinal fusion | ||
| 26 | L4-5, L5-S1 | L3-4 | DDD at L3-4, L4-5, L5-S1 HNP at L4-5, L5-S1 |
L4-5, L5-S1 right hemilaminectomy and discectomy | 24 mo | |
| 27 | L4-5 | L3-4 | DDD at L3-4, L4-5 Spondylolisthesis at L4-5 |
24 mo | ||
| 28 | L5-S1 | L4-5 | DDD at L4-5, L5-S1 Spondylolisthesis at L5-S1 Spondylolysis at L4-5 |
24 mo |
The construct selected for this study is designed to fuse the caudal level(s) of lumbar degeneration and “top off” the fusion with a dynamic rod on the affected cephalad level without fusing this level. All the index “topped-off” levels were thought to need a fusion. The index level is the level that is dynamized (ie, instrumented with a dynamic dampener). The adjacent level is the one immediately above this. The adjacent level was always normal on magnetic resonance imaging and discography, and the index level was always pathologic in this study. No normal levels were instrumented. Functional and radiographic outcomes are measured to study the results on the cephalad (dynamic or index) level, not the fused levels, to report on the early incidence of adjacent-level disease for this design at 2 years postoperatively.
The patients in this study underwent a 2- or 3-level lumbar decompressive laminectomy, depending on how many levels fit the radiographic inclusion criteria for degenerative level changes. No facetectomy greater than 50% was performed. Any patient with a facetectomy greater than 50% underwent fusion and was not included in the study. In addition, a traditional single- or 2-level transforaminal lumbar interbody fusion with rigid fixation and posterior-lateral fusion were performed at the caudal level(s) of the lumbar degeneration (Fig. 2). The dynamic, or “index,” level was chosen simply as the most cephalad level of lumbar degeneration that fit the radiographic criteria of a pathologic pain generator. No degenerative changes or discogram-proven concordant pain responses were identified at the level above the index in each patient. All patients presented with a “normal” disc at the level above the index level. The pedicle screw and rod construct used in this study is the Isobar TTL (Scient'x USA, Maitland, Florida). It consists of a 5.5-mmdiameter titanium rod with an integral dampener element. The dynamic dampener component of the rod was placed at the cephalad level of the construct (ie, the L4-5 level in the single-level L5-S1 fusion cases in a patient who would have had a 2-level fusion).
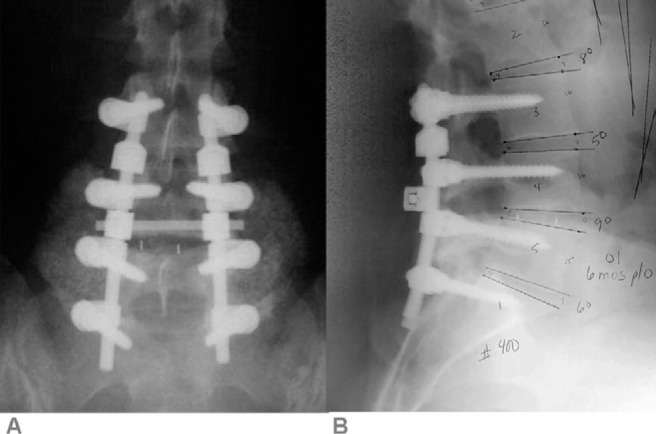
Fig. 2.
Anterior-posterior (A) and lateral (B) plain films showing an example of the posterior hybrid construct with laminectomies and interbody fusions at L4-5 and L5-S1, as well as posterior lateral fusions at these levels. The dynamic portion of the rod is placed at the cephalad (L3-4) level.
All patients presented with positive findings on discography at all levels operated on. No normal levels were instrumented, and a dynamic rod was used in lieu of a fusion at the superior level. No distinction was made between smokers and nonsmokers (Fig. 3).
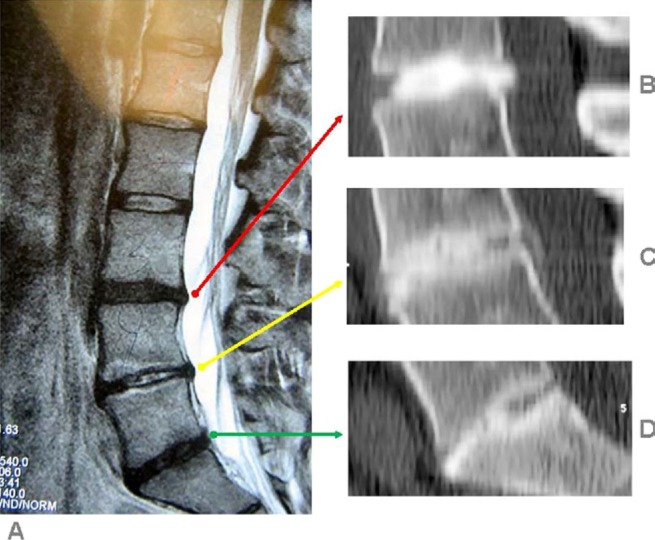
Fig. 3.
A 37-year-old woman after discectomies at L4-5 and L5-S1, with degenerative disc disease at L3-4, L4-5, and L5-S1 (A). She also had a positive discogram at L3-4 (B), L4-5 (C), and L5-S1 (D) with a normal disc at L2-3. She underwent an L4-S1 fusion with dynamic instrumentation at L3-4.
Radiographic measurements
Radiographic inclusion criteria for degenerative disc disease based on plain film changes, magnetic resonance imaging, and computed tomography were present at all levels surgically treated. All of these levels also had fully concordant pain response on discography (Fig. 4).
Fig. 4.
Left, Discogram showing pathologic morphology at both the L5-S1 and the L4-5 levels. A non-painful level with normal architecture was mandatory at the L3-4 cephalad segment. Right, Computed tomography discogram with pathologic morphology at both L4-5 and L5-S1. Both of these levels are fully concordant; the L3-4 level presents normal morphology and a negative discogram. This patient underwent an L4-5 fusion with dynamic instrumentation at L4-5.
Multiple radiographic parameters were evaluated preoperatively, and these were repeated at less than 6 weeks and 3, 6, 12, and 24 months postoperatively. The radiographic measurements include disc height ratio (Fig. 5), intervertebral angle, lumbar lordosis, vertebral translation, and mobility in flexion and extension.
Fig. 5.
Plain film radiograph showing method for measurement of disc height ratio (DHR): DHR = (a + b)/H.
The presence of radiographic fusion was evaluated by use of a 3-point scale (0, non-fusion; 1, partial or uncertain fusion; and 2, fusion) based on plain radiographs and a spiral computed tomography scan taken at 1 year postoperatively.
No preoperative dual-energy x-ray absorptiometry scans were done.
Functional outcomes
Functional outcomes were assessed with a 100-point visual analog scale (VAS), the Oswestry Disability Index (ODI), and the Short Form 36 (SF-36) global health–related quality-of-life questionnaire. These functional parameters were recorded preoperatively and at every clinical follow- up visit.
Statistical methods
The outcomes were statistically analyzed by use of paired-observation t tests with post hoc test to determine any significant changes at follow-up. The significance level (α) for all statistical tests was established a priori at .05. All mean values are reported, along with standard deviations.
Results
Functional questionnaires
ODI scores improved from preoperatively to 2 years postoperatively by 27.6 points, from 49.9 ± 15 to 22.3 ± 12.8 (P < .01). VAS scores also improved, by 24.7 points, from 60.5 ± 23.4 to 35.8 ± 30.8 (P < .01). The physical component of the SF-36 scores improved significantly by 9.8 points, from 28.8 ± 6 to 38.6 ± 12 (P < .01), and the mental component improved by 7 points, from 35.9 ± 7.3 to 42.9 ± 8.9 (P < .05).
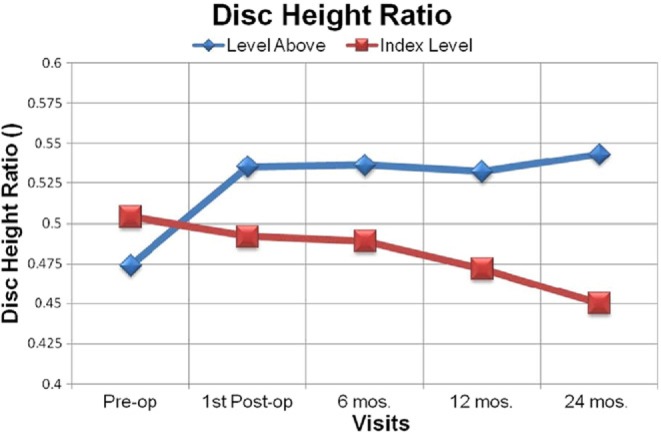
Disc height ratio
The disc height ratio 2 levels above the index level was maintained from preoperatively to the 2-year visit (P > .05). The disc height ratio at the level above the index level increased significantly by 14.6%, from 0.474 ± 0.1 to 0.543 ± 0.1 (P < .05). At the index level, the disc height ratio showed no significant change from preoperatively to 2 years postoperatively (P > .05) (Fig. 6).
Fig. 6.
Mean values for radiographic measurement of disc height ratio at each visit.
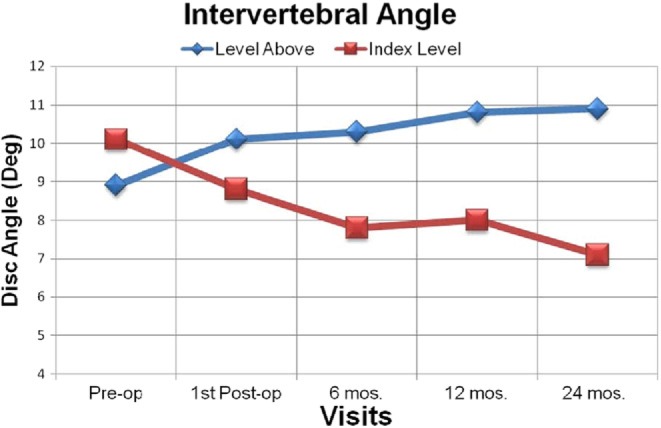
Disc angle
Two levels above the index level, the disc angle increased by 3.2°, from 6.6° ± 3.2° to 9.8° ± 3.3° (P < .01). The disc angle above the index level increased by 2°, from 8.9° ± 3.2° to 10.9° ± 2.7° (P < .05). The disc angle at the index level decreased by 3.5°, from 10.1° ± 3.8° to 6.6° ± 3.7° (P < .01) (Fig. 7).
Fig. 7.
Mean values for radiographic measurement of intervertebral angle at each visit.
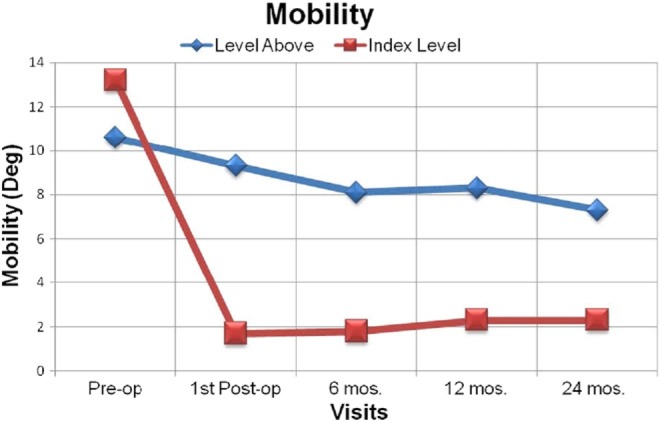
Mobility
The spinal motion segments 1 and 2 levels above the construct did not show any change in range of motion as compared with preoperative measurements (P > .05). The motion at the index level decreased from 13.2° ± 3.8° to 2.5° ± 3.6° (P < .01) and was preserved from first postoperative visit to 2-year follow-up (P > .05) (Fig. 8). This was expected because the device is designed to allow only 2° of flexion and 2° of extension, thereby shrinking the “neutral zone.”15
Fig. 8.
Mean values for radiographic measurement of angular mobility at each visit.
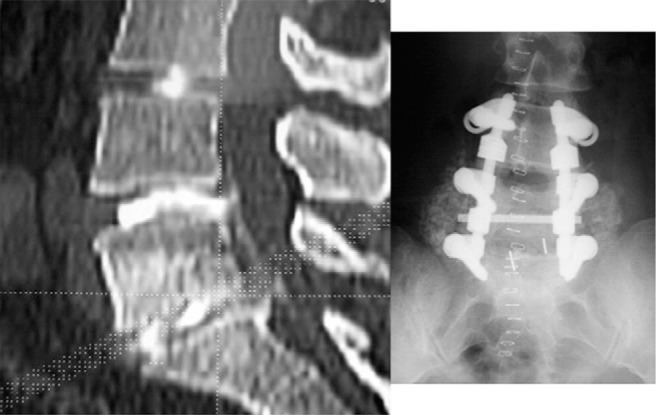
Other evaluations were recorded: lumbar lordosis, fusion, translation, and screw loosening. Overall, radiographic measurement of lumbar lordosis was preserved from preoperatively to 2 years postoperatively (50.2° ± 11° to 53.4° ± 13°) (P > .05). All patients but 1 achieved a fusion score of 2 at 1-year follow-up, with 1 case of pseudarthrosis identified at 4-year follow-up. Patient radiographs were also evaluated for translation at the index level. No statistical increase in translational deformity was identified in this series of patients. It should be noted that all radiographic measurements were calculated manually, which could make the statistical results questionable, so the measurements were confirmed by 2 independent observers to improve accuracy. All of the pedicle screws were evaluated for radiographic evidence of loosening (Fig. 9). Overall, 6 of 180 screws (3%) were determined to be loose. In 1 patient 2 screws were loose at the level above the dampener element of the rod at the L4 vertebral body and pedicle. Another patient had screws loose above (L4) and below (L5) the dampener and radiographic evidence of pseudarthrosis at the L5-S1 intervertebral disc space.
Fig. 9.
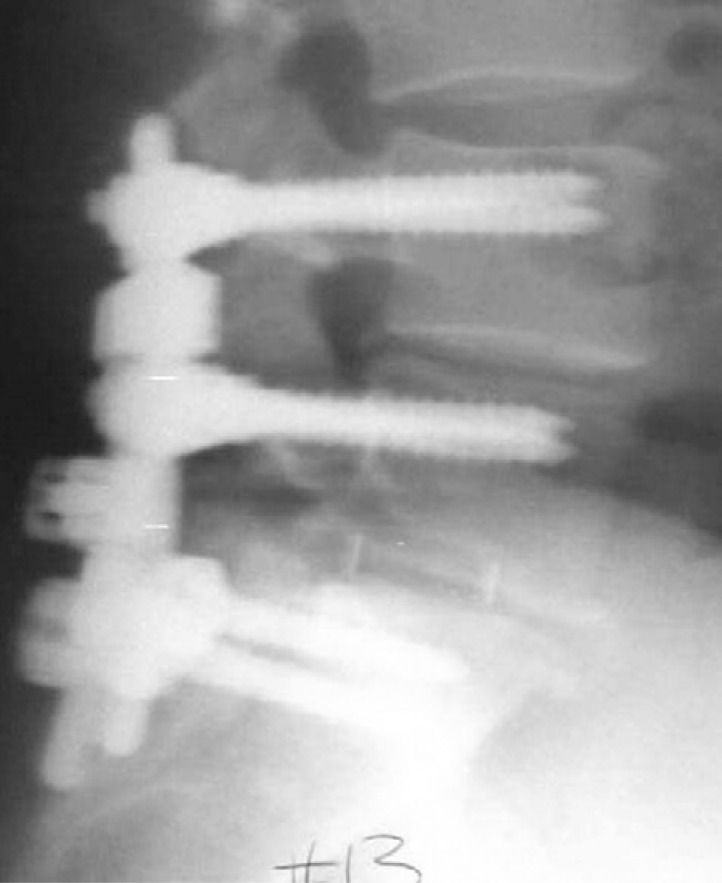
Radiographic evidence of screw loosening. The “halo” around the L4 and L5 screws in the vertebral body and pedicle should be noted. This patient also presented with a pseudarthrosis of the L5-S1 interspace at 4 years postoperatively and underwent revision to an L4-S1 fusion and repair of the pseudarthrosis.
Complications
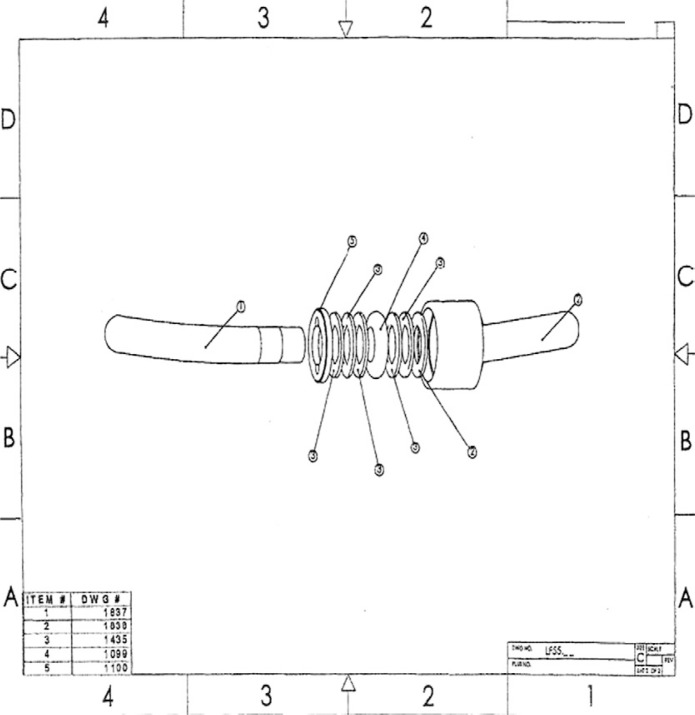
Complications that did not require reoperation included 1 case each of segmental kyphosis at the index level, reflex sympathetic dystrophy that resolved after 6 weeks of physical therapy, seroma, and a dural tear that was repaired intraoperatively (Table 1). The fourth patient who underwent surgery presented with segmental kyphosis and has had no complications from this. The surgical technique was modified so as not to create segmental kyphosis in all other patients. Four patients required further surgery for the following postoperative complications: a herniated disc at the index level, which was removed 6 weeks postoperatively, and three cases of postoperative infection, which resolved after operative debridement (Table 1). At 2 years postoperatively, no patient required revision of the dynamic rod construct, but at 4 years postoperatively, 3 patients underwent revision to a fusion (Fig. 10). One patient (patient 12) had 2-level screw loosening and a pseudarthrosis of the fusion mass, and another patient (patient 11) had unresolved radicular pain. The third patient (patient 3) had a synovial facet cyst (Fig. 11), and this was a result of medial rod placement (Table 1). Of the 3 patients who underwent revision, 2 showed no evidence of screw loosening at the time of surgery. Patients who presented with radiographic loosening and no symptoms were not treated with surgical revision.
Fig. 10.
Isobar TTL (Scient'x USA). The dampener mechanism has 0.75 mm of compression and 2° of angulation built in.
Fig. 11.
Axial computed tomography scan of synovial cyst at L3-4. The cyst was caused by medial placement of the rod. This disrupted the facet joints at the level above.
Discussion
Adjacent-level disc degeneration after a lumbar arthrodesis warrants concern about the long-term functional outcomes and stability of the spine after fusion. Recent literature suggests that the heretofore gold-standard method of treating spinal degeneration and instability must evolve.
Dynamic stabilization has been shown to be safe and effective in the treatment of lumbar degenerative disc disease through early clinical studies in Europe.6 The instrumentation design seeks to allow a predetermined range of motion to achieve symptom relief yet preserve some of the anatomic load-bearing functions of the FSU. It accomplishes this by sharing the load and motion at the index level with the superior adjacent level. This is hypothesized to decrease the incidence or severity of adjacent-level disc degeneration.16
The integral dampener element in the system used in this study results in a design-allowable 0.75 mm of maximum axial compression or distraction (interpedicular travel), as well as a maximal allowable 4° of angular motion (in flexion-extension and lateral bending). This system also includes approximately 15° of lordosis built into the rod.
The use of this technology as a hybrid system is a novel technique designed to minimize or prevent adjacent-level disc disease in the setting of lumbar fusion while providing good functional outcomes. This is a Food and Drug Administration “off-label” use of this implant. Our study shows that this operation is safe, with relatively few complications. The outcome measures, including the ODI, VAS, and SF- 36, show marked improvement in pain and functionality in these patients. These improvements are at least comparable to the historic measures seen in lumbar fusion operations with comparable follow-up.17 The radiographic data suggest preservation of the motion at the index level with no increase in the motion at the supra-adjacent segment. There does not appear to be evidence of adjacent segment disease as proven by the maintenance of disc height and range of motion at 2-year follow-up. Adjacent-level degeneration occurred in only 1 patient, and this was because of the surgeon's error of not placing the rod lateral to the superior facet joint (Fig. 11). There is a 14.6% increase in the disc height ratio at the level above the index level, which is statistically significant. This could represent very early hyperlaxity of the annular fibers, yet no increase in range of motion was found at this level. The increased disc height above the index level should be carefully assessed in future studies involving dynamic instrumentation of the spine. Discectomy was not a factor in postoperative kyphosis. Kyphosis developed in the first patient whom we operated on; this was considered iatrogenic, a result of the distraction applied between the screws to place the dynamic implant at L4-5. No correlation with “aggressive” discectomy or facetectomy in patients with increased range of motion at the adjacent level was identified. Of course, these results are early clinical measures. The ultimate objective of the current study is to evaluate the patient cohort at 10 years after surgery. Only then can the impact of dynamic stabilization on the mitigation of the incidence of adjacent-level disease be truly evaluated. Our preliminary data are encouraging, but certainly longer-term follow-up is required. The revision rate and the incidence of spontaneous fusion seem to be increasing with longer follow-up. We will report on the 5-year and 10-year outcomes for these patients.
Acknowledgments
The authors thank Deborah H. Clabeaux, RN, for assistance with this article.
References
- 1.Ehni G. The role of spine fusion. Spine. 1981;6:308–10. [Google Scholar]
- 2.Castellvi AE, Andrew SA. Scient'x IsoBar TTL dynamic rod stabilization. In: Yue JJ, Bertagnoli R, McAfee PC, editors. Motion Preservation Surgery of the Spine. 3rd ed. Philadelphia: Saunders Elsevier; 2008. pp. 483–9. [Google Scholar]
- 3.Ghiselli G, Wang JC, Bhatia NN, et al. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004;204:1497–503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Gillet P. The fate of the adjacent motion segments after lumbar fusion. J Spinal Disord Tech. 2003;16:338–45. doi: 10.1097/00024720-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Sengupta DK. Dynamic stabilization devices in the treatment of low back pain. Orthop Clin North Am. 2004;35:43–56. doi: 10.1016/S0030-5898(03)00087-7. [DOI] [PubMed] [Google Scholar]
- 6.Mulholland RC, Sengupta DK. Rationale, principles and experimental evaluation of the concept of soft stabilization. Eur Spine J. 2002;11(Suppl 2):S198–205. doi: 10.1007/s00586-002-0422-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grevitt MP, Gardner ADH, Spilsbury J, et al. The Graf stabilisation system: early results in 50 patients. Eur Spine J. 1995;4:169–75. doi: 10.1007/BF00298241. [DOI] [PubMed] [Google Scholar]
- 8.Castellvi AE, Huang H, Vestgaarden T, et al. Stress reduction in adjacent level discs via dynamic instrumentation: a finite element analysis. SAS J. 2007;1:74–81. doi: 10.1016/SASJ-2007-0004-RR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eck JC, Humphreys SC, Hodges SD. Adjacent segment degeneration after lumbar fusion: a review of clinical, biomechanical and radiologic studies. Am J Orthop. 1999;28:336–40. [PubMed] [Google Scholar]
- 10.Weinhoffer SL, Guyer RC, Herbert M, Griffith SL. Intradiscal pressure measurements above and instrumented fusion: a cadaveric study. Spine. 1995;20:526–31. doi: 10.1097/00007632-199503010-00004. [DOI] [PubMed] [Google Scholar]
- 11.Dekutoski MB, Schendel MJ, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine. 1994;19:1745–51. doi: 10.1097/00007632-199408000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Stokes IA, Iatridis JC. Mechanical conditions that accelerate intervertebral disc degeneration: overload vs. immobilization. Spine. 2004;29:2724–32. doi: 10.1097/01.brs.0000146049.52152.da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cheng BC, Cook DJ, Castellvi AE. Investigation of pedicle excursion during flexion extension bending in the human cadaveric lumbar spine. Poster presented at the Ninth Annual Global Symposium on Motion Preservation Technology (SAS9); April 28–May 1, 2009; London, England. [Google Scholar]
- 14.Cunningham B. Biomechanical animal model effectively predict the clinical situation—a critical review of testing methods and animal models utilized in the spinal motion preservation studies. Presented at the Preservation of Motion in the Spine Conference; April 1–4, 2009; Duck Key, Florida. [Google Scholar]
- 15.White AA, Panjabi M. Clinical Biomechanics of the Spine. 2nd ed. Philadelphia: Lippincott; 1990. [Google Scholar]
- 16.Kim D, Cammisa F, Fessler R. Dynamic Reconstruction of the Spine. New York: Thieme; 2006. [Google Scholar]
- 17.Glassman S, Gornet MF, Branch C, et al. MOS Short Form 36 and Oswestry Disability Index outcomes in lumbar fusion: a multicenter experience. Spine. 2006;6:21–6. doi: 10.1016/j.spinee.2005.09.004. [DOI] [PubMed] [Google Scholar]