Abstract
Background
Preoperative patient education (PE) has been used by many institutions to deal with patient anxiety, pain control, and overall satisfaction. Although the literature suggests PE's effectiveness in joint reconstruction, data are missing in spinal surgery.
Methods
We retrospectively analyzed patients having elective spinal surgery who underwent PE (spine pre-care class) from October 2009 to March 2010. Of the 155 patients surveyed, 77 (49.7%) attended the class whereas 78 (50.3%) did not.
Results
Of the participants in the pre-care class, 96% were satisfied with their pain management versus 83% in the control group (P =.02). There was also a trend for better overall satisfaction in the pre-care class group (91% vs 85%; P > .05, multiple regression analysis). Elderly women tend to be less satisfied with pain management and overall treatment.
Conclusions
Implementation of PE has had a positive impact on patient satisfaction, especially in terms of pain management.
Keywords: Preoperative patient education, Decreased postoperative pain
Patient satisfaction represents a crucial aspect in the evaluation of healthcare services. Patients may choose a different physician depending on their expectations and overall satisfaction with the care provided.1 Preoperative anxiety, impaired functional status, and postoperative pain control are important aspects in the management of surgical patients and are related to a successful recovery and patient satisfaction.2
Postoperative pain management has often been described as suboptimal3; it has been reported that in only one-quarter of the 23 million procedures performed in the United States annually did the patients receive adequate pain control.4 Fear of the unknown is expected when patients are admitted for a surgical procedure, and patients may feel vulnerable and have significant perioperative anxiety.5, 6
Patient education (PE) has been used by many institutions to deal with patient anxiety, pain control, and overall satisfaction.5, 7–15 Several authors have found PE to be beneficial,5, 6, 8, 10, 13–15 whereas others found little or no significant improvement.9, 11, 16 In a study of patients undergoing surgery after lumbar disc surgery, less than half of the patients were satisfied with their preoperative PE.17 PE may help them to set realistic goals and meet their expectations. This, in turn, may positively influence surgical outcome and overall satisfaction.1, 18, 19
In the orthopedic field, PE has frequently been used in total joint replacement programs.1, 5, 6, 8–10 To our knowledge, there are no comprehensive data on the effectiveness of PE in patients undergoing spinal surgery. The purpose of this study is to report the outcomes of PE in patients having elective spinal surgery. The null hypothesis was that there is no difference in overall satisfaction and satisfaction with pain management between the PE group and the control group. We also attempted to analyze whether certain variables are correlated with the results.
Spine Pre-care Class
PE is performed at our institution through a multidisciplinary approach tailored to the needs of the spine patients. More specifically, the spine pre-care class is an educational program that was developed by a multidisciplinary team of spine surgeons, orthopedic staff nurses, physical therapists, registration department members, hospital administration, and an internal medicine physician. The goal of the class was to take the mystery out of surgery by teaching the patient and family what to expect before and during the admission to the hospital while preparing the patient for his or her surgical experience. After extensive meetings with registration and preadmission testing to coordinate the scheduling and attendance for the class, the first spine precare class took place in April 2009.
The curriculum of the pre-care class involves taking the patient through a step-by-step process of what the day of surgery will entail. This includes registration, the preoperative process, surgery, and recovery, as well as what to expect in the days after surgery. The class is taught by an experienced orthopedic registered nurse (Orthopaedic Nurse Certificate [ONC]) and lasts 1 to 1.5 hours. Basic anatomy of the spine using spine models and radiographs is presented, in an informal setting, allowing the patients to interact with the teacher. The class also implements “handson” teaching regarding postoperative equipment, such as incentive spirometry use, placement of Sequential Compresssion Device (SCD)/anti-embolism compression stockings (TED) hose, the purpose and use of drains, and the use of back braces; in addition, physical restrictions are explained.
A majority of the class time is spent on pain control, with review of both pharmacologic and nonpharmacologic methods that may be helpful with recovery. Patients are required to demonstrate proper use of the patient-controlled anesthesia while in the class, as well as how to verbally describe their level of pain. The class stresses that patients will not be “pain free” after surgery but ensures them that the nurses will work closely with the physicians in helping to control the patients’ pain.
A spine pre-care booklet, based on the curriculum tailored to spinal surgery that was discussed in the class, was designed to educate the patient and to ease his or her fears regarding the preoperative and postoperative experience. The booklet is used as a resource that is given to the patient and acts as a guide for any further questions or concerns that he or she may have at home before the scheduled spinal surgery.
Methods
The purpose of the study is to assess the patients’ perception of their pain control, regardless of spinal procedure performed. We retrospectively analyzed the data on patients who underwent the pre-care class from October 2009 to March 2010. All patients who were scheduled to undergo spinal operations throughout this time frame were offered the class. Overall, 308 patients were operated on, and 188 (61%) participated in the class; the main reason for nonparticipation was time restraints or lack of coordination between the patients and healthcare providers. A discharge phone survey was developed by the unit staff and administered to patients who underwent spinal surgery from October 2009 to March 2010 to evaluate the effectiveness of the pre-care class (Supplementary Fig. 1, online only, available at journals.elsevierhealth.com/periodicals/esas/). All patients who were discharged home throughout the study period were contacted by phone within 1 week after their discharge regardless of whether they attended the class. We surveyed 77 of 188 class participants and 78 of 120 nonparticipants; the remaining patients were either discharged to a rehabilitation facility or could not be located. Dichotomous questions were asked to evaluate patients’ satisfaction regarding pain control and overall care received while in the hospital. Those who took the class were also asked whether they believed the class was beneficial in their recovery.
Of the 155 patients who participated in the survey, 69 were men and 86 were women (55.5%). The mean age was 55 years (range, 25–84 years). Demographics are shown in Table 1. Psychiatric evaluations were not performed for these patients. They all underwent elective spinal surgery, with an admitting diagnosis of cervical spondylarthritis (21.3%) and lumbar spondylarthritis (60%) being the most prevalent. Overall, 77 of 155 patients (49.7%) had attended the pre-care educational class that was offered by the hospital, whereas 78 (50.3%) did not attend the class.
Table 1.
Demographic characteristics of participants (N = 155)
| Characteristics | No. of patients | % |
|---|---|---|
| Age | ||
| 25–34 y | 14 | 9.0 |
| 35–44 y | 27 | 17.4 |
| 45–54 y | 40 | 25.8 |
| 55–64 y | 32 | 20.6 |
| 65–74 y | 29 | 18.7 |
| 75–84 y | 12 | 7.7 |
| 85–94 y | 1 | 0.6 |
| Gender | ||
| Male | 69 | 44.5 |
| Female | 86 | 55.5 |
For statistical analysis, we used SPSS, version 18 (SPSS, Chicago, IL). Groups were compared in terms of gender and age distribution by use of a χ2 test. On the basis of the answers to the questionnaire, groups were compared to determine whether class attendance made a difference in terms of overall satisfaction and pain management satisfaction by use of multiple regression analysis. Differences were considered significant at the P = .05 level.
Results
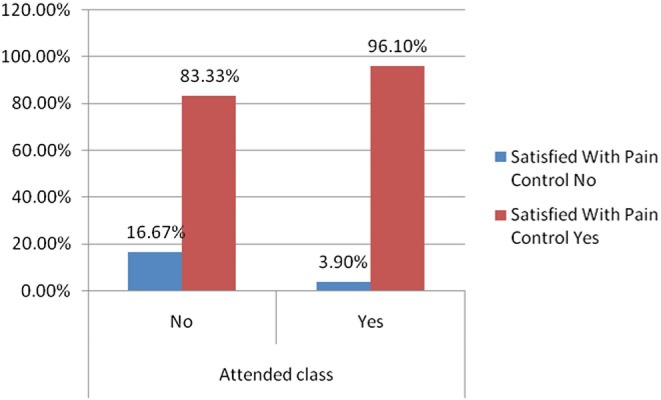
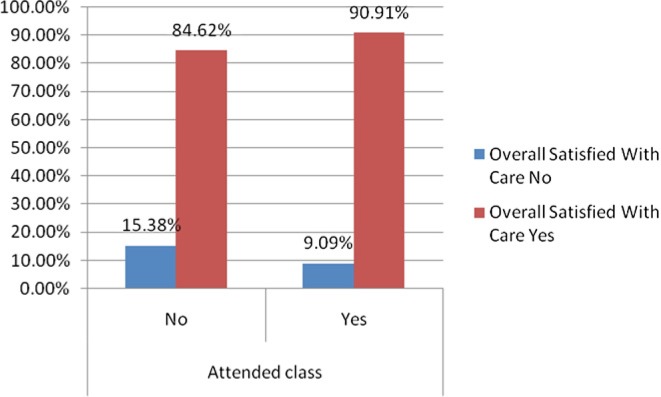
The two groups were not different in terms of their age distribution (χ2 = 9.87, P = .13) and gender distribution (χ2 = 0.78, P = .38). Patients who attended the pre-care class reported better satisfaction with pain control (96% vs 83%, Wald = 6.09, P =. 01) compared with those who did not attend (Fig. 1). There was no statistically significant difference between those who attended the pre-care class and those who did not in terms of overall satisfaction (91% vs 85%, Wald = 1.66, P = .20) (Fig. 2). As age increased, satisfaction with pain control and overall care tended to decrease (r = −0.03 and r = − 0.80, respectively). Women tended to report less satisfaction with pain control and overall care (r = − 0.01 and r = − 0.2, respectively) when compared with their male counterparts, but these results were not statistically significant.
Fig. 1.
Satisfaction with pain control.
Fig. 2.
Overall satisfaction with care.
Discussion
Preoperative PE pertains to various types of educational interventions that occur before surgery to prepare patients for the increasing physical and psychological demands during and after the operation. These provisions include health information, skill training for patients on the use of pain pumps, and provision of psychosocial support to address patients’ anxieties, needs, and concerns.7 A wide range of different approaches have been described, including group or individualized lectures, printed information such as a booklet or information sheet, audiovisual presentation, or a combination of these modalities. Timing of education also varies (before vs after admission, 1 day vs several days or weeks before the operation). PE has been implemented to help with various aspects of patient management, including length of hospitalization, preoperative anxiety, patient compliance, pain control and analgesic use, overall satisfaction, physical coping, mobility independence, and discharge preparation.2
PE has been found to be beneficial by most authorities. Previous meta-analyses have reported the effectiveness of PE. For example, Devine20 found that patients who received PE spent less time (1.5 days) in the hospital. Hathaway21 reported that PE reduced fear and anxiety. Vukomanović et al.,8 in a prospective comparative study, concluded that PE accelerated functional recovery after hip arthroplasty and recommended its use routinely. Another randomized controlled trial in the same patient population found that PE decreased preoperative anxiety and pain.10 Pulido et al.15 observed that after the implementation of an education program, there was a marked decrease in staff phone calls and improved optimal pain control. In a randomized controlled trial, coping intervention taught in PE reduced pain levels after scoliosis correction in adolescents.13 Sjöling et al.14 conducted a comparative study in patients undergoing knee arthroplasty and concluded that postoperative pain declined more rapidly for patients in the PE group, anxiety was lower, and patients were more satisfied with pain management. Various other studies support the usefulness of PE.5, 6, 12
On the other hand, there have been a few reports of little or no improvement with PE.9, 11, 16
Pain control is an essential aspect in the management of orthopedic patients, who in general have high levels of postoperative pain.22 Pain is being regarded as the fifth vital sign4 but is frequently addressed improperly.3, 4 This may cause increased morbidity and mortality rates and diminish patients’ ability to ambulate or participate in physical therapy.22, 23 Many options exist: nonsteroidal anti-inflammatory drugs, opioids, and anticonvulsants, given orally, intramuscularly, intrathecally, or in the epidural space. Frequently, patient-controlled analgesia (PCA) is used. Educating patients about PCA before surgery (eg, through practice on a dummy) and explaining to them the relationship between pain and taking pain medication and what pain relief should be expected are highly recommended.22 Patients should be involved in the decision making regarding pain control, tailored to their individual needs, desires, and circumstances; this shared decision making with their healthcare providers leads to improved health outcomes.3 Specific and realistic goals should be set preoperatively.3, 22 Patients’ expectations preoperatively frequently influence outcome and overall satisfaction.17, 19
Besides the importance of PE in improved optimal pain control, other beneficial aspects include reduction of anxiety by familiarizing the unknown,6, 24 compliance in execution of activities, discharge preparation,2 realistic expectations,1 and overall satisfaction.1, 25 In our study PE was positively correlated with patient satisfaction, especially with regard to pain management. We believe that this intervention strengthens the bond and creates a better relationship between the patient and the healthcare providers. By participating in the treatment algorithm, patients are satisfied with the tailored therapy and are educated to set reasonable expectations. We found that PE tended to be more beneficial in elderly women, although this did not reach statistical significance. This may reflect the fact that older patients frequently require repeated instructions on how to use resources (eg, PCA pumps26 and their frail health status may attenuate their anxiety and fear of adverse outcome.
To our knowledge, the only relative study reports beneficial results from coping instructions (specific coping intervention) in adolescents undergoing scoliosis correction.13 Here, we present a more comprehensive approach in a wide spectrum of elective spinal operations. We think that because of the complexity of the operations and the anatomic structures, along with the potential for catastrophic complications, PE should play a vital role in spinal surgery compared with other fields (eg, joint reconstruction).
Information provided is frequently insufficient to address patients’ questions and meet their expectations. It should not be acceptable to lead patients into complex surgery without full awareness of the procedure, postoperative course, and potential problems or complications without ways to cope or avoid adverse outcomes. Every effort should be made for a systematic, thorough, multidisciplinary preoperative preparation and education process. In line with other authors, we found that a combination of verbal instruction and provision of written pamphlets is beneficial.2
There are certain limitations of our study because it is a retrospective series. The number of subjects was also limited, and because of a high satisfaction level (>80%), the study may have been underpowered to detect discrepancies in overall satisfaction between treatment groups. The dichotomous nature of the questions being asked in our survey may also have underestimated more subtle differences. Pain ratings (on a visual analog scale [VAS]) were not compared. This was chosen for varying reasons. First, there is an inherent bias of interpreting the success of an operation with evaluation of subjective measures such as the VAS score: patients may refer to maximum pain, average pain, current pain, pain with or without medications, or positional pain; the examiner and/or the patient may be unable to document those discrepancies. Second, a mere statistical difference in VAS score may not represent a meaningful clinically significant difference.27, 28 Third, as shown by previous studies, satisfaction with provided health care may not reflect improvement in pain levels.6, 14 Satisfaction from pain management is a multifactorial issue and is being influenced by accessibility, continuity and convenience of hospital care, perceived technical quality of the center, participation in decision making, warmth of personnel, patients’ perception of a clinician's desire to provide pain relief, and so on.1
Conclusion
The implementation of our spine pre-care program has had a positive impact on patient satisfaction, especially in terms of pain management. PE represents a viable, efficient, and inexpensive intervention in patients undergoing spinal surgery.
Acknowledgments
The authors thank Mulubrhan Mogos, Nurse Research Resident, for the statistical analysis.
Appendix
Supplementary data
Note: To access the supplementary figure accompanying this report, visit the [Month] issue of SAS Journal at journals.elsevierhealth.com/periodicals/esas/.
References
- 1.Jamison RN, Ross MJ, Hoopman P, et al. Assessment of postoperative pain management: patient satisfaction and perceived helpfulness. Clin J Pain. 1997;13:229–36. doi: 10.1097/00002508-199709000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Hodgkinson B, Evans D, O'Neill S. Knowledge retention from preoperative patient information. Adelaide, Australia: The Joanna Briggs Institute for Evidence Based Nursing and Midwifery; 2000. [Google Scholar]
- 3.Gordon DB, Dahl JL, Miaskowski C, et al. American Pain Society recommendations for improving the quality of acute and cancer pain management: American Pain Society Quality of Care Task Force. Arch Intern Med. 2005;165:1574–80. doi: 10.1001/archinte.165.14.1574. [DOI] [PubMed] [Google Scholar]
- 4.Phillips DM. JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. JAMA. 2000;284:428–9. doi: 10.1001/jama.284.4.423b. [DOI] [PubMed] [Google Scholar]
- 5.Prouty A, Cooper M, Thomas P, et al. Multidisciplinary patient education for total joint replacement surgery patients. Orthop Nurs. 2006;25:257–61. doi: 10.1097/00006416-200607000-00007. quiz 262–53. [DOI] [PubMed] [Google Scholar]
- 6.Spalding NJ. Reducing anxiety by pre-operative education: make the future familiar. Occup Ther Int. 2003;10:278–93. doi: 10.1002/oti.191. [DOI] [PubMed] [Google Scholar]
- 7.Fitzpatrick E, Hyde A. Nurse-related factors in the delivery of preoperative patient education. J Clin Nurs. 2006;15:671–7. doi: 10.1111/j.1365-2702.2006.01327.x. [DOI] [PubMed] [Google Scholar]
- 8.Vukomanović A, Popović Z, Durović A, Krstić L. The effects of short-term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanit Pregl. 2008;65:291–7. doi: 10.2298/vsp0804291v. [DOI] [PubMed] [Google Scholar]
- 9.Gocen Z, Sen A, Unver B, Karatosun V, Gunal I. The effect of preoperative physiotherapy and education on the outcome of total hip replacement: a prospective randomized controlled trial. Clin Rehabil. 2004;18:353–8. doi: 10.1191/0269215504cr758oa. [DOI] [PubMed] [Google Scholar]
- 10.Giraudet-Le Quintrec JS, Coste J, Vastel L, et al. Positive effect of patient education for hip surgery: a randomized trial. Clin Orthop Relat Res. 2003:112–20. doi: 10.1097/01.blo.0000079268.91782.bc. [DOI] [PubMed] [Google Scholar]
- 11.Asilioglu K, Celik SS. The effect of preoperative education on anxiety of open cardiac surgery patients. Patient Educ Couns. 2004;53:65–70. doi: 10.1016/S0738-3991(03)00117-4. [DOI] [PubMed] [Google Scholar]
- 12.Cheung LH, Callaghan P, Chang AM. A controlled trial of psychoeducational interventions in preparing Chinese women for elective hysterectomy. Int J Nurs Stud. 2003;40:207–16. doi: 10.1016/s0020-7489(02)00080-9. [DOI] [PubMed] [Google Scholar]
- 13.LaMontagne L, Hepworth JT, Salisbury MH, Cohen F. Effects of coping instruction in reducing young adolescents’ pain after major spinal surgery. Orthop Nurs. 2003;22:398–403. doi: 10.1097/00006416-200311000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Sjöling M, Nordahl G, Olofsson N, Asplund K. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ Couns. 2003;51:169–76. doi: 10.1016/s0738-3991(02)00191-x. [DOI] [PubMed] [Google Scholar]
- 15.Pulido P, Hardwick ME, Munro M, May L, Dupies-Rosa D. Patients speak out: development of an evidence-based model for managing orthopaedic postoperative pain. Orthop Nurs. 2010;29:92–8. doi: 10.1097/NOR.0b013e3181d24399. [DOI] [PubMed] [Google Scholar]
- 16.McDonald S, Hetrick S, Green S. Pre-operative education for hip or knee replacement. Cochrane Database Syst Rev. 2004;1:CD003526. doi: 10.1002/14651858.CD003526.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Ronnberg K, Lind B, Zoega B, Halldin K, Gellerstedt M, Brisby H. Patients’ satisfaction with provided care/information and expectations on clinical outcome after lumbar disc herniation surgery. Spine (Phila Pa 1976) 2007;32:256–61. doi: 10.1097/01.brs.0000251876.98496.52. [DOI] [PubMed] [Google Scholar]
- 18.Gepstein R, Arinzon Z, Adunsky A, Folman Y. Decompression surgery for lumbar spinal stenosis in the elderly: preoperative expectations and postoperative satisfaction. Spinal Cord. 2006;44:427–31. doi: 10.1038/sj.sc.3101857. [DOI] [PubMed] [Google Scholar]
- 19.Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res. 2008;466:1154–61. doi: 10.1007/s11999-008-0194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Devine EC. Effects of psychoeducational care for adult surgical patients: a meta-analysis of 191 studies. Patient Educ Couns. 1992;19:129–42. doi: 10.1016/0738-3991(92)90193-m. [DOI] [PubMed] [Google Scholar]
- 21.Hathaway D. Effect of preoperative instruction on postoperative outcomes: a meta-analysis. Nurs Res. 1986;35:269–75. [PubMed] [Google Scholar]
- 22.Pasero C, McCaffery M. Orthopaedic postoperative pain management. J Perianesth Nurs. 2007;22:160–72. doi: 10.1016/j.jopan.2007.02.004. quiz 172–63. [DOI] [PubMed] [Google Scholar]
- 23.Morrison RS, Magaziner J, McLaughlin MA, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103:303–11. doi: 10.1016/S0304-3959(02)00458-X. [DOI] [PubMed] [Google Scholar]
- 24.Raleigh EH, Lepczyk M, Rowley C. Significant others benefit from preoperative information. J Adv Nurs. 1990;15:941–5. doi: 10.1111/j.1365-2648.1990.tb01950.x. [DOI] [PubMed] [Google Scholar]
- 25.Coslow BI, Eddy ME. Effects of preoperative ambulatory gynecological education: clinical outcomes and patient satisfaction. J Perianesth Nurs. 1998;13:4–10. doi: 10.1016/s1089-9472(98)80074-9. [DOI] [PubMed] [Google Scholar]
- 26.Egbert AM, Parks LH, Short LM, Burnett ML. Randomized trial of postoperative patient-controlled analgesia vs intramuscular narcotics in frail elderly men. Arch Intern Med. 1990;150:1897–903. [PubMed] [Google Scholar]
- 27.Glassman SD, Carreon LY. Thresholds for health-related quality of life measures: reality testing. Spine J. 2010;10:328–9. doi: 10.1016/j.spinee.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 28.Gatchel RJ, Mayer TG. Testing minimal clinically important difference: additional comments and scientific reality testing. Spine J. 2010;10:330–2. doi: 10.1016/j.spinee.2010.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]