Abstract
Background
The purpose of this study is to describe the mechanical durability and the clinical and radiographic outcomes of a viscoelastic total disc replacement (VTDR). The human intervertebral disc is a complex, viscoelastic structure, permitting and constraining motion in 3 axes, thus providing stability. The ideal disc replacement should be viscoelastic and deformable in all directions, and it should restore disc height and angle.
Methods
Mechanical testing was conducted to validate the durability of the VTDR, and a clinical study was conducted to evaluate safety and performance. Fifty patients with single-level, symptomatic lumbar degenerative disc disease at L4-5 or L5-S1 were enrolled in a clinical trial at 3 European sites. Patients were assessed clinically and radiographically for 2 years by the Oswestry Disability Index (ODI), a visual analog scale (VAS), and independent radiographic analyses.
Results
The VTDR showed a fatigue life in excess of 50 million cycles (50-year equivalent) and a physiologically appropriate level of stiffness, motion, geometry, and viscoelasticity. We enrolled 28 men and 22 women in the clinical study, with a mean age of 40 years. Independent quantitative radiographic assessment indicated that the VTDR restored and maintained disc height and lordosis while providing physiologic motion. Mean ODI scores decreased from 48% preoperatively to 23% at 2 years’ follow-up. Mean VAS low-back pain scores decreased from 7.1 cm to 2.9 cm. Median scores indicated that half of the patient population had ODI scores below 10% and VAS low-back pain scores below 0.95 cm at 2 years.
Conclusions
The VTDR has excellent durability and performs clinically and radiographically as intended for the treatment of symptomatic lumbar degenerative disc disease.
Clinical Relevance
The VTDR is intended to restore healthy anatomic properties and stability characteristics to the spinal segment. This study is the first to evaluate a VTDR in a 50-patient, multicenter European study.
Keywords: Lumbar, Viscoelastic Total Disc Replacement
More than 80% of people will have an episode of back pain at some time in their lives. In high-income countries, low-back pain (LBP) is the most frequent occupational health problem, with 2% to 5% of people having chronic LBP. LBP is the most frequent activity-limiting complaint and the second leading cause of sick leave worldwide.1 The global burden of LBP is estimated to exceed 2.5 million disability-adjusted life-years, representing 0.09% of the overall global disease burden.1 Total costs from back pain are estimated to exceed $100 billion annually in the United States alone, with two-thirds of the costs resulting from decreased wages and productivity.2
The vast majority of LBP patients will respond to one or more conservative therapies, such as medications, bracing, or physical therapy. However, approximately 20% of patients are unresponsive to conservative therapies and have chronic LBP develop.3–6 It is this 20% of chronic LBP patients who are ultimately responsible for 80% of the markedly accelerating expenditures for treatment of what some have termed an “epidemic” of LBP. For patients who cannot be treated successfully with conservative care, lumbar spinal arthrodesis or lumbar disc arthroplasty is a surgical option.
Published data indicate that only about 75% of fusion patients receive any clinical benefit.7–10 Only half will have major or complete relief of pain or recovery of function. Reoperation rates within 10 years are reported to be between 10% and 20%.11, 12 In addition, fusion may increase the incidence of degeneration of adjacent levels.13, 14
First-generation total disc replacement (TDR) designs incorporated the features of knee and hip implants, namely ball-and-socket joints consisting of metal and polyethylene. These TDRs are designed from a philosophical perspective of motion preservation or restoration. Although clinical trials have been initiated with a multitude of TDR designs, most available data pertain to 2 TDRs: the Charité artificial disc (DePuy Spine, Raynham, Massachusetts) and Pro-Disc-L (Synthes, West Chester, Pennsylvania).15–18 These non-inferiority trials randomized to fusion suggest that complication rates and patient-reported outcome measures are at least as good as those for fusion. The studies also show maintenance of disc space height and motion at the index level. A literature review on lumbar TDR outcomes, radiographic measures, and complications/reoperations found that TDRs produce results equivalent or superior to fusion and the procedure is likely to be less expensive in most cases; range of motion (ROM) is maintained or slightly improved, but ROM does not return to “normal” values; and the reoperation rate is probably similar to or lower than that for fusion.19
Longer-term follow-up of first-generation TDR patients, as well as analytic studies in cadaveric spines, suggests that long-term implantation of the first-generation devices places the facets under abnormal and excessive loading, creating an environment for facet degeneration and recurrence of localized pain.20–24 The Charité artificial disc has shown a propensity to impinge on 1 area of the core, and its movement is limited to only 1 or neither of its 2 articulating surfaces.25 TDRs featuring a polyethylene core have also shown deformation and failure of the core (fracture, delamination, excessive debris, and so on), whereas patients with metal-on-metal articulating TDRs have a wide dissemination of metallic particles throughout the body.26 Although the first-generation devices restore motion to the spinal segment, it is not a natural motion and, as such, has potentially negative effects, such as facet degeneration and failure to relieve pain and diminish disability, with a resultant need for revision surgery.27
The core materials used in almost all the TDRs currently in use or design are either polyethylene or metal. These metal-on-metal or metal-on-polyethylene articulations lack the viscoelasticity necessary to replicate the spring-damper function of the native disc.
The natural disc provides tri-planar motion: flexion and extension (sagittal plane); lateral bending (frontal plane); and rotation and compression (axial plane). It is viscoelastic, in that the degree of stiffness varies with the frequency of any load, and is compliant under loading, acting in the same manner as a spring-damper combination.28–30 To restore the disc function to a degenerated segment, an artificial disc should mimic the properties of the natural disc as closely as possible, including viscoelasticity.
The ideal treatment for degenerative disc disease will provide stabilization and function similar to those of a healthy segment. A TDR with a viscoelastic polymer core exhibits both viscous and elastic characteristics when undergoing deformation, providing increasing stiffness with either increasing loads or increasing loading rate. A viscoelastic total disc replacement (VTDR) has the potential to re-establish flexibility and natural resistance while creating stability within the functional spinal unit. The viscoelasticity would allow the TDR to mimic the dynamic stiffness and load sharing in the natural disc; preserve physiologic ROM in flexion, extension, lateral bending, rotation, and compression; and provide the correct spine alignment and lordosis. It may also allow restoration of the center of rotation (COR) to normal.
The aim of this study was to evaluate a VTDR in vitro and in vivo to characterize its performance and safety.
Methods
The VTDR consists of titanium alloy retaining plates, with attached end caps, bonded to a viscoelastic, silicone polycarbonate urethane core (Fig. 1). It should be noted that the investigational device tested is limited by federal (US) law to investigational use only.
Fig. 1.
Viscoelastic total disc replacement.
Mechanical study
Mechanical testing was conducted on a VTDR with a 26 × 36–mm footprint, 13-mm anterior height, and 12° angle. Dynamic mechanical tests of the VTDR were conducted to demonstrate the device's durability and characterize failure modes under different loading conditions. Some test methods were intended to represent physiologic loads, whereas others incorporated nonphysiologic loads and ROMs not typically observed in vivo to obtain functional failure of the VTDR. Compression fatigue testing was used to predict long-term in vivo performance of the VTDR. Wear testing—which is fatigue testing in flexion, extension, lateral bending, and rotation—was conducted to characterize the wear debris that may be generated by the VTDR.
All testing was conducted according to American Society for Testing and Materials (ASTM) international standards. Fatigue testing in compression and compressive shear was conducted according to ASTM F2346-05, “Standard Test Methods for Static and Dynamic Characterization of Spinal Artificial Discs.” Wear testing was conducted following the guidelines of ASTM F2423-05, “Standard Guide for Functional, Kinematic, and Wear Assessment of Total Disc Prostheses.” All fatigue tests were conducted in a 37°C saline solution environment at a testing frequency of 3 Hz or less. A previous study of the VTDR at different frequencies showed that the response of the polymer core to the applied load and the core temperature did not change significantly at frequencies between 1 and 3 Hz. Conversely, at frequencies of 4 Hz or higher, the polymer response decreased and temperature increased. The use of higher frequencies in testing of a viscoelastic device actually shields the polymer from being exposed to the command load because of the deformation delay that occurs with viscoelastic polymers at high frequencies.
Compression fatigue testing was conducted to characterize the performance of the VTDR under simulated walking loads, as well as under supra-physiologic loads needed to generate functional failures. Wear testing was conducted to characterize the performance of the VTDR under single and coupled moments in flexion, extension, rotation, and lateral bending and to characterize any wear debris generated. Three discs were tested in flexion/extension to 10 million cycles and then in coupled lateral bending and rotation to 10 million cycles, all at a loading frequency of 2 Hz. An additional 3 discs were tested in reverse order. All testing incorporated a constant axial compressive load of 1,200 N. Flexion/extension tests were conducted in load control to ± 10 Nm, lateral bending was conducted in load control at ± 12 Nm, and rotation was controlled to ± 3°. Flexion/extension and lateral bending tests were conducted under load control because load control is more physiologic; the discs are loaded during daily activities and respond to those loads with motion. Rotation tests were conducted in displacement control because load control, as specified in the ASTM standard (± 10 Nm), resulted in excessive, nonphysiologic (± 15°) motion of the VTDR. In vivo, rotation of the intervertebral discs is limited by the facets to approximately ± 3°; therefore this was believed to be the more appropriate testing option.
Solution samples were collected for each test device after each 5 million test machine cycles throughout testing. A total of 20 solution samples were analyzed, and all sample processing was conducted in a class II sterile environment. Each solution was filtered at 0.2 µm, centrifuged to collect the sediment (particles) for further analysis, and ultrasonicated to de-flocculate particles. Laser diffraction particle analysis (low angle laser light scattering) was conducted for quantitative analysis of particle size. Scanning electron microscopy with energy dispersive X-ray spectroscopy was conducted for qualitative analysis of particle shape. All particle sizes were given in equivalent spherical diameter based on a volume analysis and a number analysis.
Clinical study
The clinical trial was designed as a prospective, singlearm, longitudinal, multicenter study enrolling 50 patients. The required Independent Ethics Committee and National Competent Authority approvals were obtained before the initiation of the study at each investigational site. Patients were required to sign a study-specific informed consent form to participate, and patients were sequentially enrolled if they met prespecified entry criteria. Three investigational sites participated in the study. There was no specific advertisement-based recruitment of patients; rather, the patients were drawn from the usual patient population routinely seen by the involved investigators. Patients were clinically and radiographically assessed for safety and performance at specified intervals through 2 years, as detailed in Table 1. Inclusion and exclusion criteria are described in Table 2.
Table 1.
Clinical study follow-up intervals
| Assessment | Preoperatively | Discharge | 6 wk | 3 mo | 6 mo | 1 y | 2 y |
|---|---|---|---|---|---|---|---|
| Range | −6 mo | ± 2 wk | ± 2 wk | ± 2 wk | ± 1 mo | ± 2 mo | ± 2 mo |
Table 2.
Clinical study inclusion and exclusion criteria
| Inclusion criteria | Exclusion criteria |
|---|---|
| Symptomatic degenerative disc unresponsive to nonoperative management for a minimum of 6 mo with imaging studies (eg, radiography, CT, and MRI) verifying L4-L5 or L5-S1 structural abnormalities (eg, disc space collapse, grade 1 degenerative spondylolisthesis, desiccated disc, annular tears, or endplate morphologic changes) | Abnormal pain profile as suggested by 1 or more of the following: nonanatomic pain diagram, ODI >80, and surgeon assessment |
| Aged 20–60 y (inclusive) | ODI <30 |
| Mentally, emotionally, and physically able to understand the procedure; to comply with postoperative care instructions; and to adhere to 2-y follow-up schedule | Provocative discography with non-concordant pain at the operative level |
| Sagittal translation >5 mm at the operative level or above | |
| Symptoms associated with >1 lumbar level | |
| Evidence of grade 2 degenerative spondylolisthesis or greater, any isthmic spondylolisthesis, or arachnoiditis | |
| Radiographic findings of end-stage disc resorption and collapse, prior fracture of lower lumbar spine (eg, endplate sclerosis, endplate irregularities, bone-on-bone collapse, or peripheral rim osteophytes), or degenerative collapse of >3 levels, which—in the opinion of the investigator—prevents the patient from participating in the study | |
| Congenital or acquired structural defect (eg, scoliosis) at the operative level or above | |
| Acute disc herniation with radiculopathy | |
| Clinically significant facet arthrosis or other posterior element lysis or loss at the operative level | |
| Significant leg pain of a radicular or neurogenic claudication nature | |
| Spinal stenosis | |
| Symptoms associated with any neurologic signs | |
| Prior fusion at any lumbar level or laminectomy or discectomy at the operative level | |
| History of any invasive malignancy (except nonmelanoma skin cancer) unless treated with curative intent and there had been no clinical signs or symptoms or malignancy for at least 5 y | |
| Prior radiation to the spine | |
| Systemic disease affecting the spine, including rheumatoid arthritis, autoimmune disease, AIDS, HIV, and hepatitis | |
| Acute or chronic infection (local or systemic) | |
| Using medications or drugs known to potentially interfere with bone or soft-tissue healing (eg, steroids) | |
| Primary osteoporosis or osteopenia (DEXA T score <1.0) or metabolic bone disease | |
| Overweight as indicated by a body mass index ≥30 | |
| Pregnant or interested in becoming pregnant in the next 3 y | |
| Known or suspected allergy to titanium, polyethylene, cobalt, chromium, or molybdenum | |
| Evidence of drug or alcohol abuse | |
| Participation in another clinical trial within 8 wk of the baseline visit and for the duration of this trial | |
| Diabetic patients and patients with a history of implant rejection |
Abbreviations: CT, computed tomography; DEXA, dual-energy x-ray absorptiometry; HIV, human immunodeficiency virus; MRI, magnetic resonance imaging.
Efficacy measurements included physical evaluations, diagnostic imaging, and patient self-assessment questionnaires. Patients underwent clinical examination, including assessment of motor, sensory, and reflex evaluations, at each follow-up interval. Occurrence of patient complications was also recorded. Patient self-assessment questionnaires included assessments of patient function as measured by the Oswestry Disability Index (ODI), version 2.1; low-back and leg pain assessment as measured by a visual analog scale (VAS); and patient satisfaction. Local-language versions of the questionnaires were used as applicable.
Baseline radiographic films included neutral lateral, flexion/ extension lateral, and neutral anteroposterior (AP) views to document preoperative lumbar spine characteristics and to identify any findings that would exclude a potential patient from study participation. At discharge, plain radiographic films (neutral lateral and AP) were taken to provide information regarding technical success and device sizing, device performance, and index and adjacent disc height. At the intervals after discharge, plain radiographic films (neutral lateral and AP with flexion and extension lateral beginning at 3 months) were obtained to provide information regarding device performance through qualitative and quantitative assessments. All radiographic films were independently reviewed. Dual-energy x-ray absorptiometry was used to assess patients’ bone condition where age or family history was indicative of an increased risk of osteoporosis. Patients with a T score of less than −1.00 were excluded from the study. All 50 patients who were enrolled in the study were examined at each follow-up interval through 1 year. At 2 years, 48 of 50 patients were clinically examined.
All patients were implanted with the VTDR. During the investigation, the VTDR was available in multiple sizes. Surgeons were able to choose from VTDR devices with either a 26 × 36–mm or 28 × 38–mm footprint. In addition, depending on the footprint size, devices were available with anterior heights ranging from 14 to 19 mm and posterior heights ranging from 8 to 12 mm, and they were available with either an 8° or 12° lordotic angle.
Patients were implanted through a standard anterior, transperitoneal, or retroperitoneal approach based on the surgeon's preference. Typical of practice in Europe, no “access” surgeons were involved in any of the index-level implant procedures. The surgical procedure involved a discectomy at the index level, leaving portions of the lateral annulus. The VTDR requires no general bone resection of the intervertebral disc endplates as part of the implant technique. Minimal bone sculpting was performed as required to remove any osteophytes, and any obstructive medial, lateral, or posterior bony ridges were removed as applicable. The posterior longitudinal ligament was left intact or partially or completely transected depending on the surgeon's preference and ability to adequately open the disc space. Once the intervertebral disc space was prepared, the VTDR technique required template sizing, with 1-or 2-pass bone cuts for the retaining plate rails, and the final implant insertion was then performed under appropriate fluoroscopic imaging.
Statistical methods
All statistical analyses were performed with SAS for Windows, version 9.1 or later (SAS Institute, Cary, North Carolina). For safety evaluations, the incidence of reported adverse events was tabulated by type and time course of occurrence. All data related to performance were tabulated by type with 95% confidence intervals. Back and leg pain VAS score and ODI were tabulated by interval with means, standard deviations, medians, and change from baseline. A paired t test was used to assess significance from baseline. Other outcome parameters (categorical data) were tabulated by interval.
Results
Mechanical analysis
The VTDR survived 50 million cycles of axial compression at 2,400 N (n = 2) with no mechanical or functional failures. At 6,000 N, 3 devices completed 10 million cycles with no functional failures. Functional failures of the VTDR occurred only at supra-physiologic loads of 9,000 to 17,500 N. The dynamic stiffness remained constant throughout testing, even at the nonphysiologic loads of 6,000 and 7,000 N. This finding shows that the VTDR retains its mechanical integrity and performance throughout long-term fatigue testing.
Wear testing was completed to 30 million device cycles (10 million each of flexion/extension, lateral bending, and rotation) with no functional failures. The number-average particle diameter was 1.90 µm, with a range of 0.80 to 6.92 µm, and the weight-average particle diameter was 48.66 µm, with a range of 23 to 76 µm. The average mass of particulate per million cycles of wear testing was 1.70 mg.
Clinical analysis
Baseline demographics for enrolled patients are shown in Table 3, and intraoperative data are summarized in Table 4. Most patients were implanted at the L5-S1 level, an anticipated result because the L5-S1 level is the lumbar segment with the highest incidence of degenerative disc disease. The mean operative time was 128 minutes (2.1 hours). None of the investigational sites’ primary surgeons used an “access” co-surgeon to perform the anterior abdominal approach surgery (skin-to-spine index level) or perform the subsequent wound closure. The surgeon at 1 site usually performed a transperitoneal technique, whereas the surgeons at all other sites used a retroperitoneal technique. The length of hospital stay was common for a procedure of this type at the surgical sites in the United Kingdom and Germany. One patient had a small tear at the bifurcation of the vena cava during the approach surgery that was immediately repaired, but the tear did not result in major blood loss. The anterior abdominal approach surgical procedure and implantation of the device were well tolerated by the patients. There were no cases in which implantation of the device was aborted because of implant, instrument, or other technical or anatomic concerns. No new risks were identified with the index surgical procedure in this study compared with the risks already identified for other treatments that use a similar surgical approach.
Table 3.
Clinical study baseline demographics (overall)
| Variable | Result (N = 50) |
|---|---|
| Mean age (y) | 39.7 ± 8.3 |
| Gender | |
| Female | 22 (44.0%) |
| Male | 28 (56.0%) |
| Weight (kg) | 75.0 ± 12.3 |
| Height (m) | 1.7 ± 0.09 |
| Mean body mass index (kg/m2) | 25.3 ± 3.0 |
| Race | |
| Asian | 1 (2%) |
| White | 49 (98%) |
| Significant systemic/concurrent disease | 10 (20%) |
| Prior lumbar procedures | 1 (2%) |
| Smoking history | |
| None or none in past 10 y | 27 (54%) |
| In past 10 y but none currently | 7 (14%) |
| Currently <1 pack/day | 12 (24%) |
| Currently >1 pack/day | 4 (8%) |
| Work status | |
| Not working | 22 (44%) |
| Working full time | 21 (42%) |
| Working part time | 4 (8%) |
| Not applicable* | 3 (6%) |
| Currently receiving disability benefits | |
| No | 30 (60%) |
| Yes, back only | 20 (40%) |
| Yes, other than back | 0 (0.0%) |
| Yes, back and other reasons | 0 (0.0%) |
| Workers’ compensation in past year† | |
| Yes | 6 (12%) |
| No | 44 (88%) |
| Duration of back pain history | |
| Mean (mo) | 85.8 ± 61.0 |
| Median (mo) | 60 |
Housewife, retired, student, disabled, or wealthy.
Workers’ compensation status was determined in response to the question “Received in past year working compensation for back problems?”
Table 4.
Intraoperative data
| Variable | Result (N = 50) |
|---|---|
| Index level implanted | |
| L4-L5 | 13 (26%) |
| L5-S1 | 37 (74%) |
| Operative time: skin to skin (min) | |
| Mean | 127.6 ± 33.0 |
| Median | 120 |
| Mean estimated blood loss (mL) | |
| Mean | 206.4 ± 259.0 |
| Median | 150 |
| Mean hospital length of stay (d) | |
| Mean | 5.1 ± 1.7 |
| Median | 5 |
Clinical outcome measures
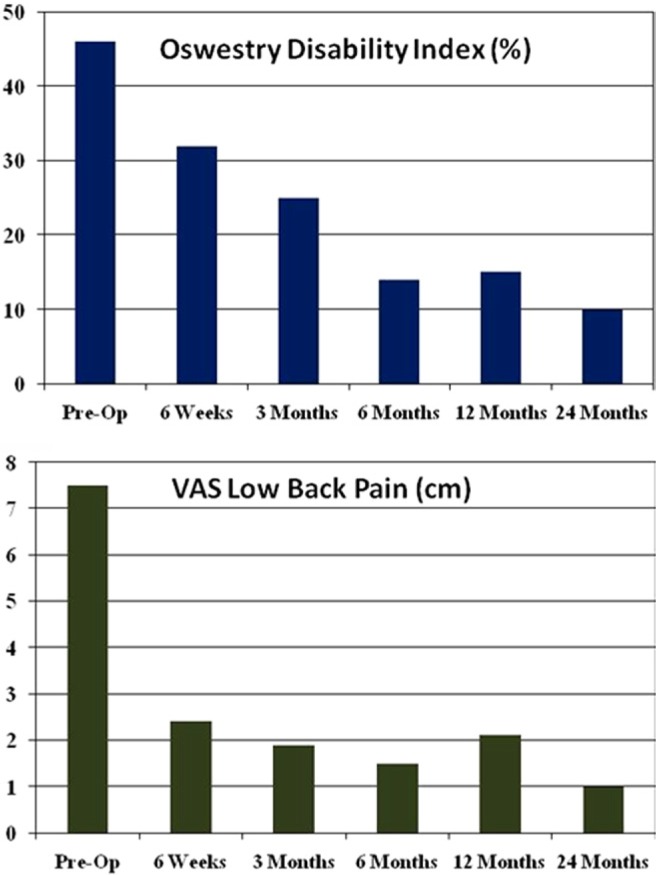
Patients in the study responded positively to the treatment as evidenced by their self-assessments of function, pain, and satisfaction. Clinical outcome scores are summarized in Fig. 2. The improvement in ODI scores from the preoperative (baseline) score was statistically significant at each postoperative interval (P < .0001). The improvement in low-back and leg pain scores versus the preoperative (baseline) score was statistically significant at each postoperative interval (P values ranged from P < .001 to P < .0001). At 6, 12, and 24 months, half of the patients had ODI scores below 14, 15, and 10, respectively (Fig. 3). At 12 and 24 months, half of the patients had VAS LBP scores below 2.1 cm and 0.95 cm, respectively (Fig. 3).
Fig. 2.
Mean ODI and VAS low back pain scores.
Fig. 3.
Median ODI and VAS low back pain scores.
Patients with the worst ODI scores and VAS LBP scores at 2 years also had confounding factors that likely affected their self-assessment of improvement, that is, adjacent-level lumbar pain that developed during the follow-up period or engaging in strenuous (noncompliant) physical activity.
Medication use decreased significantly from the preoperative value at all follow-up intervals. Preoperatively, 92% of patients were taking medications, whereas only 42%, 54%, and 40% were taking medications at 6, 12, and 24 months postoperatively (P < .0001, Wilcoxon test). Overall patient satisfaction is summarized in Table 5.
Table 5.
Patient satisfaction response
| Interval | |||
|---|---|---|---|
|
| |||
| 6 mo | 12 mo | 24 mo | |
| Question 1: Would you choose to have the same treatment for your back condition? | |||
| Definitely yes | 68% | 71.4% | 66.7% |
| Probably yes | 20% | 14.3% | 12.8% |
| Not sure | 12% | 10.2% | 15.4% |
| Probably not or definitely not | 0% | 4.1% | 5.1% |
| Question 2: Would you recommend this procedure to a family member or friend with the same back condition? | |||
| Definitely yes | 63% | 69.4% | 71.8% |
| Probably yes | 29% | 16.3% | 7.7% |
| Not sure | 8% | 12.2% | 12.8% |
| Probably not or definitely not | 0% | 2% | 7.7% |
Patient work status at 6, 12, and 24 months postoperatively is shown in Table 6. From preoperatively to 2 years’ follow-up, the percentage of patients not working decreased from 44% to 25%, and the number of patients working full or part time increased from 50% to 65%.
Table 6.
Patient work status by interval compared with baseline
| 6 mo | 12 mo | 24 mo | |
|---|---|---|---|
| Worse from baseline (95% confidence interval) | 2.1% (0.1%–11.3%) | 4.4% (0.5%–15.2%) | 7.1% (1.5%–19.5%) |
| No change or improved from baseline (95% confidence interval) | 97.9% (88.7%–100.0%) | 95.6% (84.9%–99.5%) | 92.9% (80.5%–98.5%) |
Radiographic outcome measures
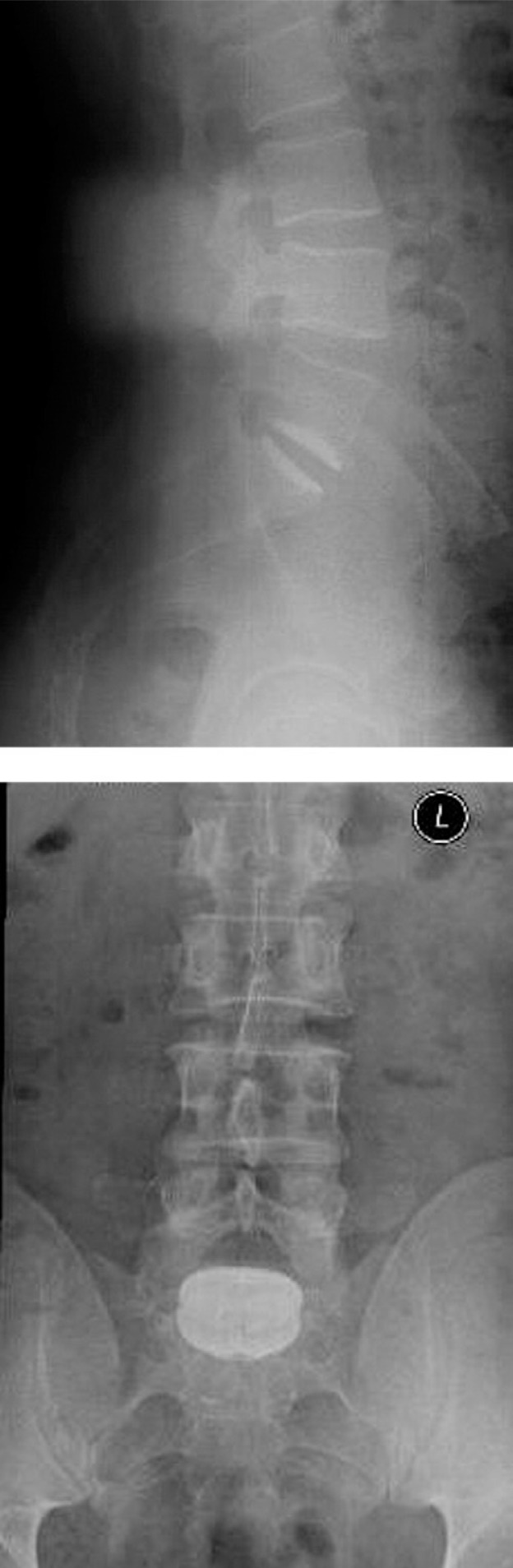
Radiographic evaluation was conducted to evaluate device performance. Device malfunctions were defined as expulsion, migration of 3 mm or greater, subsidence of 3 mm or greater, device fracture, device loosening, radiolucency, and osteophyte formation at 6 months. No cases of device expulsion or fracture occurred throughout the follow-up period. Exemplar radiographs are shown in Fig. 4.
Fig. 4.
Exemplar radiographs of a study patient.
Lumbar lordosis measurements were taken with patients in the sitting position for those initially enrolled in the study, whereas patients enrolled later had lumbar lordosis measurements taken in the standing position. The mean lumbar lordosis at 24 months’ follow-up was 41° (± 11°) for sitting patients and 57° (± 13°) for standing patients. Disc height and angle were restored and maintained throughout the 2-year follow-up period. Disc height significantly increased from 7.9 mm (± 2.1 mm) preoperatively to 12.9 mm (± 2.3 mm) at 2 years (P < .0001, paired t test), and disc angle significantly increased from 11.2° (± 6.1°) preoperatively to 16.0° (± 4.0°) at 2 years (P < .0001, paired t test). Flexion/extension ROM decreased from 8.0° (± 5.0°) preoperatively to 4.4° (± 3.1°) at 2 years. Translation was maintained over a period of 2 years, with preoperative translation of 0.6 mm (± 0.6 mm) and translation at 2 years’ follow-up of 0.5 mm (± 0.4 mm).
No device expulsion or device mechanical failures occurred. The incidence of device migration or subsidence through 2 years was minimal and comparable to, or better than, other TDRs where high-quality data are available for comparison.17, 18 The performance analysis at the 6-month endpoint determined that 1 severe radiolucency was observed, which subsequently improved and diminished in severity at subsequent interval radiographic assessments. One case of anterior migration of 3 mm or greater and one case of caudal subsidence of 3 mm or greater were reported. In the patient with an anterior migration, the disc implanted was suspected to be slightly too small based on a postoperative radiographic review. In the patient with caudal subsidence, there was no condition identified as a contributing factor to the subsidence. Continued follow-up of patients through 2 years indicated that the 2 cases with movement identified at 6 months remained but with no further increase in movement, because the devices had stabilized in their final position and required no intervention. One additional case of anterior migration of 3 mm or greater was reported beginning at 1 year, but the device's movement had stabilized at the 2-year examination and required no intervention. Independent radiographic review of this patient's radiographs indicated a slight anterolisthesis of the L5 vertebral body on S1. There was no indication that the patient's bone condition was inadequate either at index surgery or by 2 years. One patient had the device removed at approximately 15 months because of pain resulting from a caudal subsidence and confirmation of loosening at the removal surgery. In this case, borderline osteoporosis or low-grade infection may have contributed to the failure despite not being able to establish either by biopsy and blood parameters. In each of the cases of device movement, the patients’ clinical scores were improved compared with their respective preoperative clinical status.
At 2 years’ follow-up, there were 2 cases with reported moderate radiolucencies and no cases of severe radiolucencies. In the patients with some observed moderate radiolucencies, the inability to perfectly match the congruence between the VTDR device's domed plates and the vertebral endplates can produce slight mismatch at the implant-bone interface, thus resulting in clinically non-important radiolucencies.
During the 2-year follow-up, there was no osteophyte formation that resulted on bridging bone. In the patients in whom a mild, moderate, or severe osteophyte was identified at 2 years, most had pre-existing osteophytes identified at their preoperative radiographic assessment. At 2 years postoperatively, the osteophyte was scored as mild in 14 patients, moderate in 10, and severe in 9, but in these patients, some level of pre-existing osteophyte formation was identified on the preoperative radiographs for 13 mild, 7 moderate, and 6 severe cases. In addition, there was no correlation between the rating of osteophyte formation postoperatively and the patient's radiographic ROM (P > .05, Spearman correlation). The mean ROMs at each follow-up interval for patients with osteophyte ratings of none, mild, moderate, and severe are shown in Table 7. Moreover, heterotopic bone formation was not identified in this series and was not a cause of motion impairment.
Table 7.
Mean ROM for patients with each osteophyte rating by interval
| Osteophyte rating | Mean ROM | |||
|---|---|---|---|---|
|
| ||||
| Preoperatively | 6 mo | 12 mo | 24 mo | |
| None | 8.6° | 5.3° | 4.2° | 4.7° |
| Mild | 7.9° | 5.3° | 4.5° | 4.8° |
| Moderate | 5.9° | 3.9° | 3.6° | 4.1° |
| Severe | 12.2° | 5.4° | 2.9° | 3.9° |
Adverse events
Adverse events were collected to assess device safety and its impact on performance. No deaths and no unanticipated adverse events were reported in this study. All adverse events reported involve the type, scope, and frequency of medical and surgical adverse events expected in a TDR population that has undergone an open anterior lumbar surgical approach. Three patients reported retrograde ejaculation, and three patients were confirmed to have or suspected of having thromboses. The incidence of thrombosis appeared to be linked to intraoperative patient positioning at a single site. Once the patient-positioning procedure was changed, there were no further cases of thromboses at the involved site. Superficial wound infections were reported in 2 cases. One serious device-related adverse event was reported, in the patient who had the VTDR removal at approximately 15 months postoperatively because of increased LBP. It was concluded that this patient had device loosening for the reasons listed previously. One patient had a supplemental fixation at the index and superior adjacent level at 20 months postoperatively because of pain. The device was left in situ. This serious adverse event was not deemed device related but rather was considered related to non–index-level lumbar conditions. Thus, at 2 years, data for 48 of 50 patients were available for clinical analysis.
Discussion
Mechanical studies
Compression fatigue testing was used to predict longterm in vivo performance of the VTDR. At axial compressive loads in the range of average daily living loads, each cycle simulates a walking step. The average daily living load was estimated based on the loads on the lumbar spine for many activities reported by Nachemson.31 Because it is generally believed that the average person takes 1 million steps per year,32, 33 a 10 million– cycle compression fatigue test is used to predict 10 years of simulated in vivo loading. The VTDR tested in our study showed a 50-year fatigue life at twice the average daily living load. There is a lack of evidence in the literature that any other TDRs in clinical use have shown a simulated walking fatigue life of 50 years.
Hedman et al.34 estimated that the average person experiences 125,000 significant bends per year. Each cycle in flexion/extension, lateral bending, or rotation is considered to be 1 significant bend. Therefore the test that included 10 million cycles each of flexion/extension, lateral bending, and rotation produces 30 million total cycles. Each 5 million cycles is equivalent to 40 years of significant bends, 10 million cycles is equivalent to 80 years of significant bends, and so on, and 30 million cycles is equivalent to 240 years worth of significant bends. The ASTM method for wear testing combines a high lifting compressive load with maximum ROMs in flexion, extension, lateral bending, and rotation. Studies have shown that the ROM of the lumbar spine decreases with increasing compressive load.35 As a result, the ASTM method places the device under ROM and load combinations that neither the natural disc nor TDR devices would be expected to experience in vivo. For this reason, it is believed that the ASTM wear test dramatically exaggerates the functional, kinematic, and wear response of the VTDR. Even though the wear test methods were all somewhat different, the wear rate of the VTDR was more than 3 times lower than that of the ProDisc-L. The VTDR wear testing generated a larger mean particle size than those generated by first-generation TDRs. A decrease in particle size has been found to result in an increase in bioreactivity (resultant biologic proinflammatory activity). Thus smaller particles would be more likely to induce a proinflammatory response than larger particles.
For a TDR where components are bonded together, the bond may be the weakest link in the design. This study showed that the bond is durable and withstands vigorous mechanical testing under both physiologic and supra-physiologic conditions.
Clinical studies
The independent radiographic analysis data indicate that the VTDR maintains normal lumbar lordosis, restores normal disc height and angle, and provides flexion/extension ROM and translation similar to those provided by the natural disc. The mean lumbar lordosis at 2 years’ follow-up was 41° for sitting patients and 57° for standing patients. Lumbar lordosis has been found to increase from sitting to standing,36 and the range of standing lumbar lordosis in healthy patients has been reported to range from 41° to 75°.37 Disc height and angle were restored and maintained throughout the 2-year follow-up period, with a mean disc height of 12.9 mm and a mean disc angle of 15.6° at 2 years. Comparatively, lumbar disc height has been reported to range from 6 to 14 mm, and the mean lumbar disc angles for patients aged from 20 years to 50 years or older have been reported to range from 8.2° to 17.0°, with disc angle increasing with age.38 Mean flexion/extension ROM at 2 years’ follow-up was 4.2° for L4–5 implants and 4.5° for L5-S1 implants. Flexion/extension ROM at L4–5 and L5-S1 has been reported in the literature to range from 6.7° to 15.3° in cadavers39 but only from 0.8° to 3.0° in healthy volunteers with no back pain or disorders.40 Translation was maintained during the study, with translation at 2 years’ follow-up of 0.5 mm. Lumbar disc AP translation has been reported to range from 0.6 to 3.8 mm.41–43 The radiographic data for the VTDR show that it performs much like the natural healthy discs, both dimensionally and mechanically.
In studies involving first-generation ball-and-socket design discs, ROM success has been defined as motion greater than or equal to that present preoperatively. This definition does not account for patients in the instability phase of the Kirkaldy-Willis degenerative cascade.44 Patients in the dysfunction or stabilization phases may show lower amounts of motion, whereas those in the instability phase will likely show more motion preoperatively. If a TDR is implanted during the instability phase and motion increases, that would imply provision of excess motion, which may cause damage to the surrounding anatomy, such as facets. Conversely, a decrease in motion from the instability phase (preoperative) to the restoration of stability was expected in this study. ROM success should be based on restoration of the ROM of a healthy disc rather than on any increase or decrease from preoperative ROM. Our intent was to provide a TDR with stiffness equivalent to a human disc. There was no primary target for motion because this is dependent on the forces that are applied through the disc. It has been shown that motion in the Charité artificial disc in vitro25 is abnormal in type and in many cases exceeds the normal range. What has been shown in this study is that restoration of the stiffness leads to good clinical outcomes and restoration of the COR is produced,45 and thus the ROM is adequate.
In lumbar TDR clinical studies, the prevalence of TDR implantation at L5-S1 versus L4–5 is often approximately 2:1. Some investigators advocate fusing the L5-S1 segment rather than implanting a TDR because of lower reported ROMs at this level. Although the ROM has been reported to be lower in some loading modes at L5-S1 compared with L4–5,46 ROM should not be the important factor in deciding between fusion and TDR. The compressibility of the L5-S1 segment is vital in the transition to the relatively stiffer segments of the pelvis below. Thus, in the degenerative state, the resistance to compressibility is lost, leading to clinical symptoms. This study shows that restoring stability and compressibility results in excellent clinical relief of symptoms. We therefore advocate the use of VTDR in this segment over fusion wherever possible.
An interesting observation from this small sample is the relief of leg symptoms in a large number of our patients. The main entry criterion for this study was back pain, not leg pain; however, the presence of radicular symptoms (not due to prolapsed disc) was noted and scaled. The relief of radicular symptoms in these patients raises the question of the origin of radicular pain and how best to relieve it. This article supports the view that restoring the normal functional anatomy of the disc leads to relief of radicular symptoms. This is a secondary benefit of VTDR but an important one from a patient's perspective.
Although we believe that this is one of the largest studies of an elastomeric TDR, the study was limited to 50 patients at 3 investigational sites. A pivotal prospective, randomized clinical study of the VTDR is currently in progress. The results from this study, as well as potential future studies evaluating longer-term results and multilevel implantation, are necessary to confirm the results seen to date for this VTDR.
Conclusions
The VTDR showed an in vitro fatigue life equivalent to 50 years or greater. The testing showed that the VTDR allows motion around 3 axes and provides stiffness like that of the natural disc. It permits and constrains motion, providing appropriate stability while facilitating function. The VTDR provides a physiologically appropriate level of stiffness, motion, geometry, and viscoelasticity.
The study data indicate that the VTDR is safe and performs as intended for use as a total disc arthroplasty device in skeletally mature patients diagnosed with symptomatic lumbar degenerative disc disease.
References
- 1.Hoy D, March L, Brooks P, et al. Measuring the global burden of low back pain. Best Pract Res Clin Rheumatol. 2010;24:155–65. doi: 10.1016/j.berh.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences. J Bone Joint Surg Am. 2006;88(Suppl 2):21–4. doi: 10.2106/JBJS.E.01273. [DOI] [PubMed] [Google Scholar]
- 3.Von Korff M, Saunders K. The course of back pain in primary care. Spine. 1996;21:2833–7. doi: 10.1097/00007632-199612150-00004. [DOI] [PubMed] [Google Scholar]
- 4.Hurwitz EL, Morgenstern H, Kominski GF, Yu F, Chiang LM. A randomized trial of chiropractic and medical care for patients with low back pain: eighteen-month follow-up outcomes from the UCLA low back pain study. Spine. 2006;31:611–21. doi: 10.1097/01.brs.0000202559.41193.b2. [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Loeser JD, Owens DK, et al. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidencebased clinical practice guideline from the American Pain Society. Spine. 2009;34:1066–10. doi: 10.1097/BRS.0b013e3181a1390d. [DOI] [PubMed] [Google Scholar]
- 6.Furlan AD, Clarke J, Esmail R, Sinclair S, Irvin E, Bombardier C. A Critical review of reviews on the treatment of chronic low back pain. Spine. 2001;26:E155–62. doi: 10.1097/00007632-200104010-00018. [DOI] [PubMed] [Google Scholar]
- 7.Christensen FB. Lumbar spinal fusion. Outcome in relation to surgical methods, choice of implant and postoperative rehabilitation. Acta Orthop Scand. 2004;313(Suppl 75):2–43. [PubMed] [Google Scholar]
- 8.Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: influence of technique on fusion rate and clinical outcome. Spine. 2004;29:455–63. doi: 10.1097/01.brs.0000090825.94611.28. [DOI] [PubMed] [Google Scholar]
- 9.Boos N, Webb JK. Pedicle screw fixation in spinal disorders: a European view. Eur Spine J. 1997;6:2–18. doi: 10.1007/BF01676569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Turner JA, Ersek M, Herron L, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992;268:907–11. [PubMed] [Google Scholar]
- 11.Greiner-Perth R, Boehm H, Allam Y, Elsaghir H, Franke J. Reoperation rate after instrumented posterior lumbar interbody fusion: a report on 1680 cases. Spine. 2004;29:2516–20. doi: 10.1097/01.brs.0000144833.63581.c1. [DOI] [PubMed] [Google Scholar]
- 12.Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Reoperation rates following lumbar spine surgery and the influence of spinal fusion procedures. Spine. 2007;32:382–7. doi: 10.1097/01.brs.0000254104.55716.46. [DOI] [PubMed] [Google Scholar]
- 13.Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE. Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine. 2004;29:1938–44. doi: 10.1097/01.brs.0000137069.88904.03. [DOI] [PubMed] [Google Scholar]
- 14.Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine. 2008;33:1701–7. doi: 10.1097/BRS.0b013e31817bb956. [DOI] [PubMed] [Google Scholar]
- 15.Blumenthal S, McAfee PC, Guyer RD, et al. A prospective, randomized, multicenter Food and Drug Administration investigational device exemptions study of lumbar total disc replacement with the CHARITE artificial disc versus lumbar fusion: part I: evaluation of clinical outcomes. Spine. 2005;30:1565–75. doi: 10.1097/01.brs.0000170587.32676.0e. [DOI] [PubMed] [Google Scholar]
- 16.Zigler J, Delamarter R, Spivak JM, et al. Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine. 2007;32:1155–62. doi: 10.1097/BRS.0b013e318054e377. [DOI] [PubMed] [Google Scholar]
- 17.Spine Synthes. Summary of safety and effectiveness data: ProDisc-L Total Disc Replacement; 2006. FDA PMA Number P050010. [Google Scholar]
- 18.DePuy Spine, Inc., A Johnson & Johnson Company. Summary of safety and effectiveness: Charité Artificial Disc; 2004. FDA PMA Number P040006. [Google Scholar]
- 19.Guyer RD, Ohnmeiss DD, Blumenthal SL, Zigler JE. Lumbar total disc replacement: results of a comprehensive review of clinical outcomes, radiographic measures, and complications/re-operations. Presented at the International Society for the Advancement of Spine Surgery 10th Annual Symposium on Motion Preservation Technology; April 2010; New Orleans, LA. [Google Scholar]
- 20.Denozière G, Ku DN. Biomechanical comparison between fusion of two vertebrae and implantation of an artificial intervertebral disc. J Biomech. 2006;39:766–75. doi: 10.1016/j.jbiomech.2004.07.039. [DOI] [PubMed] [Google Scholar]
- 21.Park CK, Ryu KS, Jee WH. Degenerative changes of discs and facet joints in lumbar total disc replacement using ProDisc II: minimum two-year follow-up. Spine. 2008;33:1755–61. doi: 10.1097/BRS.0b013e31817b8fed. [DOI] [PubMed] [Google Scholar]
- 22.Phillips F, Diaz R, Pimenta L. The fate of the facet joints after lumbar total disc replacement: a clinical and MRI study. Spine J. 2005;5:75S–6S. [Google Scholar]
- 23.Punt IM, Visser VM, van Rhijn LW, et al. Complications and reoperations of the SB Charité lumbar disc prosthesis: experience in 75 patients. Eur Spine J. 2008;17:36–43. doi: 10.1007/s00586-007-0506-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Ooij A, Oner FC, Verbout AJ. Complications of artificial disc replacement: a report of 27 patients with the SB Charité disc. J Spinal Disord Tech. 2003;16:369–83. doi: 10.1097/00024720-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 25.O'Leary P, Nicolakis M, Lorenz MA, et al. Response of Charité total disc replacement under physiologic loads: prosthesis component motion patterns. Spine J. 2005;5:590–9. doi: 10.1016/j.spinee.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 26.Gunaratnam M, Grant MH. Cr (VI) inhibits DNA, RNA and protein syntheses in hepatocytes: involvement of glutathione reductase, reduced glutathione and DT-diaphorase. Toxicol In Vitro. 2008;22:879–86. doi: 10.1016/j.tiv.2008.01.005. [DOI] [PubMed] [Google Scholar]
- 27.Ross ER, Mirza AH, Norris HE, Khatri M. Survival and clinical outcome of SB Charite III disc replacement for back pain. J Bone Joint Surg Br. 2007;89:785–9. doi: 10.1302/0301-620X.89B6.18806. [DOI] [PubMed] [Google Scholar]
- 28.Keller TS, Spengler DM, Hansson TH. Mechanical behavior of the human lumbar spine. I. Creep analysis during static compressive loading. J Orthop Res. 1987;5:467–78. doi: 10.1002/jor.1100050402. [DOI] [PubMed] [Google Scholar]
- 29.Costi JJ, Stokes IA, Gardner-Morse MG, Iatridis JC. Frequency-dependent behavior of the intervertebral disc in response to each of six degree of freedom dynamic loading: solid phase and fluid phase contributions. Spine. 2008;33:1731–8. doi: 10.1097/BRS.0b013e31817bb116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Race A, Broom ND, Robertson P. Effect of loading rate and hydration on the mechanical properties of the disc. Spine. 2000;25:662–9. doi: 10.1097/00007632-200003150-00003. [DOI] [PubMed] [Google Scholar]
- 31.Nachemson AL. Disc pressure measurements. Spine. 1981;6:93–7. doi: 10.1097/00007632-198101000-00020. [DOI] [PubMed] [Google Scholar]
- 32.Morlock M, Schneider E, Bluhm A, et al. Duration and frequency of every day activities in total hip patients. J Biomech. 2001;34:873–81. doi: 10.1016/s0021-9290(01)00035-5. [DOI] [PubMed] [Google Scholar]
- 33.Schmalzried TP, Szuszczewicz ES, Northfield MR, et al. Quantitative assessment of walking activity after total hip or knee replacement. J Bone Joint Surg Am. 1998;80:54–9. [PubMed] [Google Scholar]
- 34.Hedman TP, Kostuik JP, Fernie GR, Hellier WG. Design of an intervertebral disc prosthesis. Spine. 1991;16:S256–60. doi: 10.1097/00007632-199106001-00016. [DOI] [PubMed] [Google Scholar]
- 35.Janevic J, Ashton-Miller JA, Schultz AB. Large compressive preloads decrease lumbar motion segment flexibility. J Orthop Res. 1991;9:228–36. doi: 10.1002/jor.1100090211. [DOI] [PubMed] [Google Scholar]
- 36.Lord MJ, Small JM, Dinsay JM, Watkins RG. Lumbar lordosis. Effects of sitting and standing. Spine. 1997;22:2571–4. doi: 10.1097/00007632-199711010-00020. [DOI] [PubMed] [Google Scholar]
- 37.Cakir B, Richter M, Kafer W, Puhl W, Schmidt R. The impact of total lumbar disc replacement on segmental and total lumbar lordosis. Clin Biomech. 2005;20:357–64. doi: 10.1016/j.clinbiomech.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 38.Eijkelkamp MF, van Donkelaar CC, Veldhuizen AG, van Horn JR, Huyghe JM, Verkerke GJ. Requirements for an artificial intervertebral disc. Int J Artif Organs. 2001;24:311–21. [PubMed] [Google Scholar]
- 39.Panjabi M, Henderson G, Abjornson C, Yue J. Multidirectional testing of one- and two-level ProDisc-L versus simulated fusions. Spine. 2007;32:1311–9. doi: 10.1097/BRS.0b013e318059af6f. [DOI] [PubMed] [Google Scholar]
- 40.Li G, Wang S, Passias P, Xia Q, Li G, Wood K. Segmental in vivo vertebral motion during functional human lumbar spine activities. Eur Spine J. 2009;18:1013–21. doi: 10.1007/s00586-009-0936-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berkson MH, Nachemson A, Schultz AB. Mechanical properties of human lumbar spine motion segments—part II: responses in compression and shear; influence of gross morphology. J Biomech Eng. 1979;101:53–75. [Google Scholar]
- 42.Posner I, White AA, Edwards WT, Hayes WC. A biomechanical analysis of the clinical stability of the lumbar and lumbosacral spine. Spine. 1982;7:374–89. doi: 10.1097/00007632-198207000-00008. [DOI] [PubMed] [Google Scholar]
- 43.Ashton-Miller JA, Schultz AB. Biomechanics of the human spine. In: Mow VC, Hayes WC, editors. Basic Orthopaedic Biomechanics. Philadelphia: Lippincott-Raven; 1997. pp. 353–93. [Google Scholar]
- 44.Kirkaldy-Willis WH, Mierau D. The three phases and three joints. In: Kirkaldy-Willis WH, Bernard TN Jr, editors. Managing Low Back Pain. 4th ed. Philadelphia: Churchill Livingstone; 1999. pp. 249–62. [Google Scholar]
- 45.Newton EM, Ross ER, Rischke B, Joellenbeck B, Hipp J, Zimmers K. An association between the center of rotation and clinical outcome in patients implanted with a viscoelastic total disc replacement. Presented at the British Association of Spine Surgeons Meeting; February 2011; Edinburgh, Scotland. [Google Scholar]
- 46.Pearcy M, Portek I, Shepherd J. Three-dimensional X-ray analysis of normal movement in the lumbar spine. Spine. 1984;9:294–7. doi: 10.1097/00007632-198404000-00013. [DOI] [PubMed] [Google Scholar]