Abstract
We analyzed georeferenced data on mobility and HIV infection from the 2009 Demographic and Health Survey of Lesotho. We found ~50% of the population traveled in the preceding year. By constructing gender-specific mobility maps we discovered travel is highest in the urban areas bordering South Africa, and in the mountainous interior of the country. For both genders, increased mobility was associated with increased levels of “recent” sexual behavior. Notably, mobility was only associated with an increased risk of HIV infection for men who travelled frequently. We discuss the implications of our results for designing effective treatment programs and HIV interventions.
Introduction
Studies in Kenya, Tanzania, Burkina Faso, Zimbabwe, South Africa and Cameroon have shown an association between increased mobility and increased levels of sexual behavior [1-3], increased risk of HIV infection [4, 5], or both [6-10]. These studies indicate population mobility may have a significant effect on HIV transmission in these countries. Moreover a recent study has shown the importance of travel in the early spread of the HIV epidemic in Sub-Saharan Africa [11]. Notably, the potential impact of mobility on HIV transmission in countries where the HIV prevalence is extremely high has not yet been investigated. Here we assess the potential impact of mobility on the high-prevalence HIV epidemic in Lesotho, where 27% of women and 18% of men are infected with HIV [12]. In Lesotho there is a high level of circular migration as many men and women have to travel for employment. Some travel within the country to work in agriculture and the textile industry [13], others travel between Lesotho and South Africa for employment as domestic and mine workers [13, 14]. To evaluate the impact of mobility we analyzed linked demographic, behavioral and HIV infection data from the 2009 Demographic and Health Survey (DHS) of Lesotho [15]. We analyzed the DHS data in order to: (i) quantitatively assess the mobility of the population, (ii) identify the demographic and behavioral characteristics of individuals who travel, (iii) determine if there are geographic patterns in mobility, and (iv) determine whether there is an association between mobility and increased levels of sexual behavior and/or risk of HIV infection.
Many of the previous epidemiological studies investigating the effect of mobility and migration on HIV epidemics have been based on small sample sizes and/or used poorly designed questionnaires to collect data on risk behaviors [9, 16, 17]. In contrast in our study we analyzed data collected from ~45,000 individuals living in ~9,000 households. It has been suggested that concurrency is under reported in DHS surveys in Sub-Saharan Africa due to problems with the questionnaire design [18, 19]. However, we note the questionnaire was changed for the 2009 Lesotho DHS and the levels of reported concurrency are high [19].
Methods
We used georeferenced demographic, behavioral, and HIV testing data that had been collected in the 2009 DHS in Lesotho. In this data set an individual's HIV test results are linked to their demographic and behavioral data. The response rate for the DHS in Lesotho, unlike in many other African countries where DHS are conducted [20], was very high: 98% for women, 95% for men. Participation in HIV testing was also high: 94% for women, 88% for men. Data were weighted to ensure they were representative of the population [21]. A detailed description of the DHS data can be found elsewhere [12].
We quantified population mobility by stratifying the population into three travel categories according to the number of trips taken in the preceding year: (i) no travel, (ii) one to four trips, and (iii) five or more trips. A trip was defined as being away from home for at least one night. We defined individuals who had made five or more trips in the preceding year as frequent travelers. We compared demographic and behavioral characteristics of individuals in these three travel categories.
We constructed mobility maps, using the georeferenced DHS data, to determine if there are geographic patterns in mobility. The maps show: (i) the percentage of individuals (living at a specific geographic location) who traveled in the preceding year, and (ii) where the frequent travelers live. We constructed gender-specific maps. The maps were constructed using Kriging [22-24] which was implemented using the R package geoR [25].
To determine whether mobility was associated with increased risk behavior and/or increased risk of HIV infection we used logistic regression. For both genders, risk behavior was defined in terms of: (i) the number of sex partners reported in the preceding year and in the respondents lifetime, (ii) concurrency (defined as two or more sexual partnerships that overlapped in time) and (iii) condom usage (defined as using a condom for the last sex act). For men we analyzed a further measure of risk behavior, whether they had ever paid for sex. In separate analyses the measures of risk behavior and HIV infection were used as response variables; analyses were gender-specific. Mobility (adjusting for age, education level, marital and employment status) was assessed as an explanatory variable.
Results
Demographic statistics, stratified by gender and travel category (i.e., number of trips taken in the last year) are given in Table 1. It can be seen that the population of Lesotho is highly mobile: 30% of women and 32% of men made one to four trips in the preceding year, 18% of women and 21% of men made five or more. For a high percentage of individuals who travelled (37% women and 39% men), one or more of their trips lasted for at least a month. Men and women who travelled were slightly older than those who did not travel. They were also more likely to be married, employed, live in urban areas and have a higher level of education. The age of sexual debut was not significantly different between those who travelled and those who did not. Notably, individuals who travelled reported having had a greater number of sex partners in the preceding year than those who did not; those who were frequent travelers (i.e., made five or more trips in the last year) reported the highest numbers. A greater percentage of men who travelled reported paying for sex; however the numbers are low, only ~8% of men who travelled frequently reported paying for sex.
Table 1.
Summary statistics and adjusted odds ratios (aOR) of HIV infection and sexual risk behavior.
| Women | Men | |||||||
|---|---|---|---|---|---|---|---|---|
| Number of overnight trips in the past year | Number of overnight trips in the past year | |||||||
| Demographic summary statistics | 0 | l to 4 | 5 or more | 0 | l to 4 | 5 or more | ||
| Fraction of total population | n/N | (%) | 1992/3849 (51.8%) | 1158/3849 (30.1%) | 699/3849 (18.2%) | 1467/3075 (47.7%) | 971/3075 (31.6%) | 638/3075 (20.7%) |
| Age | Median | (IQR) | 25(19-35) | 28 (21-36)* | 28 (21-36)* | 26 (19-38) | 25 (19-34) | 29 (22-38)* |
| Age of sexual debut | Median | (IQR) | 17(16-19) | 18 (16-20) | 18 (16-20) | 17 (15-20) | 17(15-19) | 17(15-20) |
| Live in urban areas | n/N | (%) | 595/1992 (29.9%) | 336/1158 (29.0%) | 297/699 (42.5%)* | 342/1467 (23.3%) | 243/971 (25.0%) | 217/638 (34.0%)* |
| Employed | n/N | (%) | 626/1992 (31.4%) | 495/1158(42.7%)* | 350/699 (50.1%)* | 872/1467 (59.4%) | 602/971 (62.0%) | 470/638 (73.7%)* |
| Ever married | n/N | (%) | 1241/1992 (62.3%) | 815/1158 (70.4%)* | 466/699 (66.7%)* | 654/1467 (44.6%) | 436/971 (44.9%) | 375/638 (58.8%)* |
| Secondary or higher education | n/N | (%) | 965/1992 (48.4%) | 599/1158 (51.7%) | 413/699 (59.1%)* | 481/1467 (32.8%) | 366/971 (37.7%)* | 297/638(46.6%)* |
| Number of sex partners in last year | Mean | (SD) | 0.74 (0.55) | 0.87 (0.54)* | 0.91 (0.56)* | 0.93 (1.17) | 1.08 (0.80)* | 1.26 (0.93)* |
| Odds ratios of HIV infection and sexual risk behavior | ||||||||
| HIV infected | n/N | (%) | 484/1941 (24.9%) | 302/1202 (25.1%) | 211/706 (29.9%) | 230/1445 (15.9%) | 171/982 (17.4%) | 142/648 (21.9%) |
| aOR (95% CI) | 1 (REF) | 0.91 (0.76-1.09) | 1.13 (0.92-1.39) | 1 (REF) | 1.17 (0.93-1.48) | 1.31 (1.01-1.68)* | ||
| 2 or more sex partners in last year | n/N | (%) | 90/1910 (4.7%) | 99/1193(8.3%) | 70/703 (10.0%) | 236/1415 (16.7%) | 239/974 (24.5%) | 199/642 (31.0%) |
| aOR (95% CI) | 1 (REF) | 1.64 (1.22-2.21)* | 1.97 (1.41-2.73) * | 1 (REF) | 1.58 (1.29-1.94)* | 2.00 (1.60-2.50)* | ||
| 4 or more lifetime sex partners | n/N | (%) | 240/1585 (15.1%) | 159/1059 (15.0%) | 119/616 (19.3%) | 564/1147 (49.2%) | 468/824 (56.8%) | 354/576 (61.5%) |
| aOR (95% CI) | 1 (REF) | 0.97 (0.77-1.21) | 1.20 (0.93-1.54) | 1 (REF) | 1.41 (1.18-1.70)* | 1.46 (1.19-1.82)* | ||
| Concurrent partnership in last year | n/N | (%) | 72/1333 (5.4%) | 88/921(9.6%) | 64/556 (11.5%) | 184/995 (18.5%) | 180/765 (23.5%) | 169/557 (30.3%) |
| aOR (95% CI) | 1 (REF) | 1.79 (1.29-2.49)* | 1.92 (1.33-2.77)* | 1 (REF) | 1.33 (1.05-1.68)* | 1.76 (1.38-2.25)* | ||
| Ever paid for sex | n/N | (%) | 56/945 (5.9%) | 52/734 (7.1%) | 44/541 (8.1%) | |||
| aOR (95% CI) | 1 (REF) | 1.29 (0.87-1.93) | 1.32 (0.86-2.02) | |||||
The summary statistics for those that travel one to four, or five or more time, are compared to those that do not travel. Significance is shown with stars. On average, those who travel frequently are slightly older. The mobile population is more likely to live in urban areas, be employed and have a higher level of education. The mean number of sex partners increases with mobility. Odds ratios are calculated adjusting for age, employment status, marital status and education. Stars denote the significance according to the following P-values:
*P <0.001
*0.001≤P<0.01
0.01≤P<0.05.
Mobile women and men have a greater odds ratio of having two or more sex partners and having concurrent partnerships than those who did not travel. Concurrent partnerships are calculated amongst those who had sex in the last 12 months. Mobile men have greater odds of reporting four or more lifetime sex partners. Men who made five or more trips have greater odds of being HIV infected than those who did not travel.
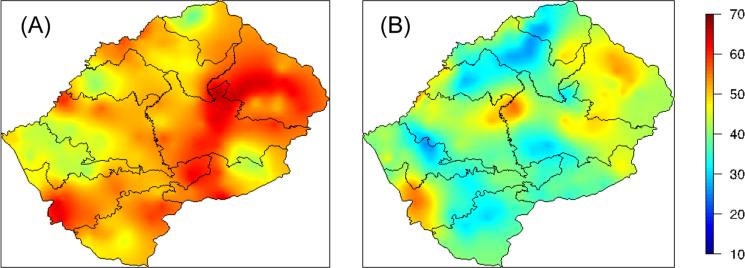
The mobility maps (for men) are shown in Figure 1. Figure 1A shows the percentage of men (living at a specific geographic location) who travelled in the preceding year; Figure 1B shows where the frequent travelers live. Figure 1A shows that the level of mobility is high throughout the country, but geographic patterns are apparent. In some parts of the country ~40% of men traveled (green data), whereas in other parts ~70% of men traveled (red data). The highest concentration of frequent travellers (shown by the red data) is in several of the urban areas that border South Africa, and also in the mountainous interior of the country (Figure 1B). For a map of the mountainous areas and urban centers in Lesotho see reference [23]. The mobility maps for women are similar to those for men; results not shown.
Figure 1.
Mobility maps for men in Lesotho. The maps are constructed using the 2009 Demographic Health Survey data from Lesotho and plotted using kriging: (A) shows the percentage of men (living at a specific geographic location) who travel; men who travel are defined as those who made one or more trips in the last year, and (B) shows the percentage of men (amongst those who traveled last year) who were frequent travellers and who live at that specific geographic location; frequent travelers are defined as those who made five or more trips in the last year.
Adjusted odds ratios from the logistic regression analyses are presented in Table 1. We found men and women who travelled (regardless of the number of trips they made) were more likely to have had multiple partners in the preceding year (i.e., recent partners) than those who did not travel; odds increased with the frequency of travel. Men and women who made five or more trips were almost twice as likely to have two or more recent partners than those who did not travel. In addition, men and women who travelled (regardless of the number of trips they made) were more likely to have concurrent partners than those who did not travel; odds increased with frequency of travel. Further, men who travelled (regardless of the number of trips they made) were more likely to have a greater number of lifetime sex partners, than men who did not travel. However, no association was found between travel and the number of lifetime partners for women; and no association was found, for either gender, between mobility and condom usage. Men who travelled, regardless of the number of trips they made, were not more likely to have paid for sex than men who did not travel.
Notably, only men who travelled frequently (i.e., made five or more trips in the past year) had an increased risk of HIV infection: they were 1.31 (CI: 1.01-1.68) times more likely to be infected than men who did not travel, Table 1. Men who travelled infrequently (i.e., made one to four trips in the preceding year), and women who traveled (regardless of the number of trips) did not have an increased risk of HIV infection in comparison with individuals who did not travel.
Discussion
Previous epidemiological studies that have looked for associations between mobility and increased levels of sexual behavior and/or risk of HIV infection have focused on specific “risk groups” living in particular locations [2, 4-8, 10]. In contrast, we have focused on an entire population and (by using georeferenced data) evaluated mobility within a large-scale geographic context. By constructing mobility maps we have discovered that, although the entire population of Lesotho is very mobile, there is an observable geographic pattern. We have found two “types” of areas where a very high proportion of the population travel: (i) Maseru (the capital of Lesotho) and smaller urban areas that border South Africa, and (ii) the remote, mountainous interior of the country. Notably, this geographic pattern holds for both men and women. Unfortunately, the DHS did not collect data that enabled us to determine where, or why, individuals traveled. It is possible that the destinations individuals travelled to may differ for those who live in urban areas versus those who live in the mountains. Our results suggest that travel (for both genders) may be necessary for employment, as we found that those who travelled were more likely to be employed than those who did not travel. Notably, in the mountainous areas there are few employment opportunities. Future studies of migration would be improved by collecting detailed data to determine where individuals travel and why they travel.
Our results show, as suggested by social scientists [16], that the effect of mobility and circular migration on HIV epidemics is complex and dynamic. For both men and women we found that increased mobility was associated with increased levels of “recent” sexual behavior (i.e., in the preceding year). However it was only for men that we found an association between increased mobility and increased numbers of lifetime sex partners. Notably, it was only for men who were frequent travelers that we found an association between increased mobility and an increased risk of HIV infection. Whether, or not, mobility increases an individuals’ risk of infection depends upon multiple interacting factors: e.g., the baseline risk of infection, the magnitude of increase in risk behavior, and the travel destination. There is a need to develop a greater understanding of the causal pathways through which migration can increase vulnerability to HIV [16]. There is also a need to develop complex transmission models that can be used to gain insights into the dynamic effect of mobility and migration on sexual networks and HIV epidemics [26, 27].
Our results have significant implications for the design of effective treatment programs and interventions for reducing HIV transmission in Lesotho. As many individuals travel it may be very difficult to ensure high adherence to treatment [28]. Our mobility maps can be used to identify the geographic regions where attaining high levels of adherence may be the most challenging. We recommend that treatment programs in Lesotho should collect travel data from patients and use these data as a basis for developing strategies to enhance adherence. It is generally assumed that implementing interventions in one geographic region will reduce transmission in that region. However this may not be the case in Lesotho where the highly mobile population can link many “localized” HIV epidemics both within the country and in the bordering provinces of South Africa. For example, miners who live in Lesotho may become infected in South Africa and then infect their partners when they return home. Under these conditions it is essential to design interventions that are specifically targeted to migrant workers, and frequent travelers. Our mobility maps can be used to identify where there is the greatest need for such interventions. Taken together our results imply that in Lesotho and in other countries (such as Zimbabwe, Cameroon and Kenya) that have high levels of mobility and circular migration, it may be more difficult to control HIV epidemics than currently appears.
Acknowledgements
We thank Dr. Brian Coburn and Justin Okano for their comments and discussion whilst preparing this manuscript. This work was supported by NIH grant R01AI041935 and funding from the Semel Institute of Neuroscience and Human Behavior, and the David Geffen School of Medicine at UCLA.
References
- 1.Brockerhoff M, Biddlecom AE. Migration, sexual behavior and the risk of HIV in Kenya. International Migration Review. 1999:833–856. [Google Scholar]
- 2.Khan MR, Patnaik P, Brown L, Nagot N, Salouka S, Weir SS. Mobility and HIV-related sexual behavior in Burkina Faso. AIDS Behav. 2007;12:202–212. doi: 10.1007/s10461-007-9314-8. [DOI] [PubMed] [Google Scholar]
- 3.Cassels S, Manhart L, Jenness SM, Morris M. Short-term mobility and increased partnership concurrency among men in Zimbabwe. PLoS ONE. 2013;8:e66342. doi: 10.1371/journal.pone.0066342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mmbaga EJ, Leyna GH, Hussain A, Mnyika KS, Sam NE, Klepp K-I. The role of in-migrants in the increasing rural HIV-1 epidemic: results from a village population survey in the Kilimanjaro region of Tanzania. International Journal of Infectious Diseases. 2008;12:519–525. doi: 10.1016/j.ijid.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Kwena ZA, Camlin CS, Shisanya CA, Mwanzo I, Bukusi EA. Short-Term Mobility and the Risk of HIV Infection among Married Couples in the Fishing Communities along Lake Victoria, Kenya. PLoS ONE. 2013;8:e54523. doi: 10.1371/journal.pone.0054523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kishamawe C, Vissers DCJ, Urassa M, Isingo R, Mwaluko G, Borsboom GJJM, Voeten HACM, Zaba B, Habbema JDF, de Vlas SJ. Mobility and HIV in Tanzanian couples: both mobile persons and their partners show increased risk. AIDS. 2006;20:601–608. doi: 10.1097/01.aids.0000210615.83330.b2. [DOI] [PubMed] [Google Scholar]
- 7.Lydié N, Robinson NJ, Ferry B, Akam E, De Loenzien M, Abega S. Study Group on Heterogeneity of HIV Epidemics in African Cities: Mobility, sexual behavior, and HIV infection in an urban population in Cameroon. J Acquir Immune Defic Syndr. 2004;35:67–74. doi: 10.1097/00126334-200401010-00010. [DOI] [PubMed] [Google Scholar]
- 8.Camlin CS, Hosegood V, Newell M-L, McGrath N, Bärnighausen T, Snow RC. Gender, migration and HIV in rural KwaZulu-Natal, South Africa. PLoS ONE. 2010;5:e11539. doi: 10.1371/journal.pone.0011539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weine SM, Kashuba AB. Labor migration and HIV risk: a systematic review of the literature. AIDS Behav. 2012;16:1605–1621. doi: 10.1007/s10461-012-0183-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lurie MN, Williams BG, Zuma K, Mkaya-Mwamburi D, Garnett GP, Sturm AW, Sweat MD, Gittelsohn J, Karim SSA. The impact of migration on HIV-1 transmission in South Africa: a study of migrant and nonmigrant men and their partners. Sexually transmitted diseases. 2003;30:149–156. doi: 10.1097/00007435-200302000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Faria NR, Rambaut A, Suchard MA, Baele G, Bedford T, Ward MJ, Tatem AJ, Sousa JD, Arinaminpathy N, Pepin J, Posada D, Peeters M, Pybus OG, Lemey P. The early spread and epidemic ignition of HIV-1 in human populations. Science. 2014;346:56–61. doi: 10.1126/science.1256739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coburn BJ, Okano JT, Blower S. Current drivers and geographic patterns of HIV in Lesotho: implications for treatment and prevention in Sub-Saharan Africa. BMC Medicine. 2013;11:1–1. doi: 10.1186/1741-7015-11-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.International Organization for Migration (IOM) Briefing Note on HIV and Labour Migration in Lesotho. 2006:1–15. [Google Scholar]
- 14.International Organization for Migration (IOM) HIV/AIDS, Population Mobility and Migration in Southern Africa. 2005:1–81. [Google Scholar]
- 15.Ministry of Health and Social Welfare (Lesotho) ICF Macro: Lesotho Demographic and Health Survey. 2009;2010:1–452. [Google Scholar]
- 16.Deane KD, Parkhurst JO, Johnston D. Linking migration, mobility and HIV. Tropical Medicine & International Health. 2010;15:1458–1463. doi: 10.1111/j.1365-3156.2010.02647.x. [DOI] [PubMed] [Google Scholar]
- 17.Nnko S, Boerma JT, Urassa M, Mwaluko G, Zaba B. Secretive females or swaggering males? Social Science & Medicine. 2004;59:299–310. doi: 10.1016/j.socscimed.2003.10.031. [DOI] [PubMed] [Google Scholar]
- 18.Morris M, Leslie-Cook A, Nelson SJ. Evaluating concurrent partnership data from the 2005-2008 demographic and health surveys (DHS). XVIII International AIDS Conference [Google Scholar]
- 19.Epstein H, Morris M. Concurrent partnerships and HIV: an inconvenient truth. Journal of the International AIDS Society. 2011;14:13. doi: 10.1186/1758-2652-14-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mishra V, Hong R, Khan S, Gu Y. Evaluating HIV estimates from national population- based surveys for bias resulting from non-reponse. Calverton. 2008:1–167. [Google Scholar]
- 21.Rutstein SO, Rojas G. Guide to DHS Statistics. OCR Macro; Calverton, Maryland: 2006. pp. 1–168. [Google Scholar]
- 22.Diggle PJ, Ribeiro PJ., Jr . Model Based Geostatistics. Springer; New York: 2007. [Google Scholar]
- 23.Coburn BJ, Blower S. Mapping HIV epidemics in sub-Saharan Africa with use of GPS data. The Lancet Global Health. 2014;1:e251–e253. doi: 10.1016/S2214-109X(13)70084-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krige DG. A statistical approach to some basic mine valuation problems on the Witwatersrand. Journal of Chemical, Metallurgical, and Mining Society of South Africa. 1951 [Google Scholar]
- 25.Ribeiro PJ, Jr, Diggle PJ. geoR: a package for geostatistical analysis. 2001 [Google Scholar]
- 26.Wilson DP, Kahn J, Blower SM. Predicting the epidemiological impact of antiretroviral allocation strategies in KwaZulu-Natal: The effect of the urban–rural divide. Proceedings of the National Academy of Sciences. 2006;103:14228–14233. doi: 10.1073/pnas.0509689103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andrews JR, Wood R, Bekker L-G, Middelkoop K, Walensky RP. Projecting the benefits of antiretroviral therapy for HIV prevention: the impact of population mobility and linkage to care. J Infect Dis. 2012;206:543–551. doi: 10.1093/infdis/jis401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bygrave H, Kranzer K, Hilderbrand K, Whittall J, Jouquet G, Goemaere E, Vlahakis N, Triviño L, Makakole L, Ford N. Trends in loss to follow-up among migrant workers on antiretroviral therapy in a community cohort in Lesotho. PLoS ONE. 2010;5:e13198. doi: 10.1371/journal.pone.0013198. [DOI] [PMC free article] [PubMed] [Google Scholar]