Abstract
Background
Orientation is one of the most stressful times in a registered nurse's career. Little information is available regarding the efficacy of stress management approaches among new nurses. The purpose of this study was to examine outcomes of the implementation of a brief Stress Management and Resiliency Training (SMART) program within a nurse orientation program.
Methods
In this randomized controlled pilot study, self-reported measures of stress, mindfulness, anxiety, and resilience were measured at baseline and 12 weeks following the intervention. For each group, the mean change from baseline to week 12 was evaluated using the paired t test. The change from baseline was compared between groups using the 2-sample t test. Feasibility of integrating the SMART program into the nurse orientation program was also analyzed.
Results
Of the 55 participants enrolled, 40 (73%) completed the study. Mindfulness and resilience scores improved in the intervention group and declined in the control group, while stress and anxiety scores decreased in the intervention group and increased in the control group. The between-group change in each outcome, however, was not statistically significant.
Conclusions
Integrating the SMART program within the nurse orientation program is feasible. While changes between groups were not significant, trends in the results indicate that the program has the potential for efficacy. Future research with larger numbers is indicated with a revised version of the program to increase its effect size.
Keywords: Anxiety, education, mindfulness, nurses, resilience–psychological, stress–psychological
INTRODUCTION
Multiple research studies have confirmed the presence of workplace stress among nurses.1 Orientation is commonly one of the most stressful times in the career of a registered nurse (RN).2,3 Occupational stress and burnout negatively impact the health and well-being of nurses and can affect patient safety.4-8 In addition, the stressful transition from school to work can increase turnover rates of new nurses.9
Newly licensed RNs encounter several challenges as they transition into the hospital environment. They face complex settings with multiple stimuli and sources of information. In addition, they confront time pressures and challenging patients, often without adequate preparation, knowledge, time management skills, or critical thinking abilities. Thus, the transition period for the graduate nurse from orientation to staff nurse is highly stressful.2,10-12
Although the situation has not been well studied, experienced RNs who are transitioning to a new role and/or to a new institution may be susceptible to many of the same stressors experienced by new graduates.13 Transitioning RNs tend to return to the advanced beginner stage of clinical competence, the same stage as many newly licensed RNs, when they have minimal experience in the new role they are expected to perform.
Causes of Stress for Nurses
Events historically recognized to cause stress for RNs include work overload, complex patients, criticism, interpersonal relationship issues with physicians and other colleagues, lack of support from supervisors, and bureaucratic constraints.14,15 Since 2010, researchers have recognized additional stress factors, including increased complexity of patient conditions, decrease in control, role ambiguity, staffing shortages, sophisticated technology, and competition among hospitals.16,17
Adverse Effects of Stress on Nurses
Among nurses and other healthcare professionals, adverse outcomes of stress include psychosomatic disorders; poor mental health; alcoholism; drug abuse; absenteeism; tardiness; turnover; workplace injury; musculoskeletal disorders; decreased ability to provide quality care; and impairment of concentration, attention, and memory.18-22 Absenteeism and turnover related to stress can lead to inadequate staffing levels that also place patients at risk. Despite the high prevalence and adverse impact of stress among nurses, few evidence-based effective strategies exist to prevent and reduce stress in new nurses transitioning into the hospital setting and those transitioning to new roles.
Stress Management and Resiliency Training Program
An intervention that has shown promise for reducing stress and improving resiliency in a variety of populations is the Stress Management and Resiliency Training (SMART) program. The SMART program was developed at our institution by a physician in the Division of Complementary and Integrative Medicine who has extensive experience in the field of resiliency training. The program is designed to help participants understand the neuroscience and biology of stress. From that understanding, participants learn skills to develop intentional attention and reframe life experiences using the 5 core principles of gratitude, compassion, acceptance, forgiveness, and higher meaning.23-28 The present study was designed to assess feasibility and obtain preliminary estimates of efficacy of the SMART program on stress, mindfulness, anxiety, and resilience measures within a nurse orientation program at Mayo Clinic in Rochester, MN.
METHODS
Study Design and Population
This institutional review board-approved trial was designed as a randomized controlled pilot study. Participants were recruited from a group of nurses who were new to the institution or transitioning to a new unit or new role and who were undergoing new nurse orientation. Participants were randomized into either the intervention or control group through the use of a random number generator. Self-reported measures were collected from both groups at baseline and 12 weeks following the intervention. Data were collected via a secure web-based survey system.
Inclusion criteria were RNs who were enrolled in 1 of 2 designated nurse orientation classes; were willing and able to participate in all aspects of the study; and were provided with, understood, and signed the informed consent. Nurses were excluded if they reported currently or recently (within the past 6 months) experiencing a psychotic episode, a clinically significant acute psychiatric event, or a physical illness.
Intervention
The intervention group participated in a 90-minute session during which a study investigator presented a model of stress and resilience, integrating neuroscience and biology. Based on this model, mind-body approaches to managing stress were discussed, including developing intentional attention and practicing gratitude, compassion, acceptance, forgiveness, and higher meaning. Four weeks following the initial session, a 1-hour follow-up session was offered to address individual questions. Participants also received biweekly handouts on each of the topics via email. The control group received a lecture associated with the nursing orientation program that covered topics related to stress, including reality shock and work-life connectedness.
Measurement
Analyses were performed using the following measurement tools: the Perceived Stress Scale (PSS), the Mindful Attention Awareness Scale (MAAS), the Generalized Anxiety Disorder 7-item scale (GAD-7), and the Connor-Davidson Resilience Scale (CD-RISC). In addition, an investigator-developed demographic questionnaire and a program evaluation were administered. The program evaluation instrument was designed to allow the participants to provide short answer responses related to their experience with the program.
The PSS is a 14-item self-report instrument that measures the degree to which situations in one's life are appraised as stressful.29 Items are rated on a 5-point Likert scale: 0 (never), 1 (almost never), 2 (sometimes), 3 (fairly often), and 4 (very often). A higher score indicates greater stress. Examples of items include “In the last month, how often have you been upset because of something that happened unexpectedly?” and “In the last month, how often have you felt that you were effectively coping with important changes that were occurring in your life?” The PSS relates well with life event scales and has been determined to have adequate reliability in 3 different samples (α=0.84, 0.85, 0.86).29
The MAAS is a 15-item measure assessing the tendency to be aware of present-moment experiences.30 Sample statements include the following: “I could be experiencing some emotion and not be conscious of it until sometime later,” “I find it difficult to stay focused on what's happening in the present,” and “I rush through activities without being really attentive to them.” The items are answered on a Likert scale from 0 (almost always) to 6 (almost never). Higher scores indicate greater mindfulness. The MAAS has exhibited adequate reliability (α=0.80-0.87) and validity when used with a general adult population.30
The GAD-7 is a 7-item questionnaire that assesses symptoms of anxiety. Subjects are asked how often during the last 2 weeks they were bothered by each symptom.31 Response options are 0 (not at all), 1 (several days), 2 (more than half the days), and 3 (nearly every day). Examples of symptoms include “feeling nervous, anxious, or on edge,” “not being able to stop or control worrying,” and “becoming easily annoyed or irritable.” The measure has been found to have excellent internal consistency (α=0.89) and has demonstrated adequate reliability and validity in the general population.32
The CD-RISC is a 25-item scale designed to quantify resilience in a variety of populations.33 Each item is rated on a 0-4 scale with higher scores reflecting more resilience.34 Examples of items included in the scale are “I am able to adapt when changes occur,” “I can deal with whatever comes my way,” and “Past successes give me confidence in dealing with new challenges and difficulties.” The CD-RISC has been found to have external-internal consistency (α=0.89), test-retest reliability (intraclass correlation coefficient=0.87), and positive correlation with multiple related measures.35
Statistical Methods
Data were summarized using mean ± SD for continuous variables and frequency percentages for categorical variables. The primary outcomes of interest included changes in stress (PSS), mindfulness (MAAS), anxiety (GAD-7), and resilience (CD-RISC) scores. These measurements were evaluated at baseline and week 12. For each group, the mean change from baseline to week 12 was evaluated using the paired t test. To assess the efficacy of the intervention, the change from baseline to week 12 for each outcome of interest was compared between groups using the 2-sample t test. In all cases, 2-tailed P values ≤0.05 were considered statistically significant, and findings were summarized using point estimates and corresponding 95% confidence intervals. Analysis was restricted to participants who completed the study, including all follow-up assessments.
RESULTS
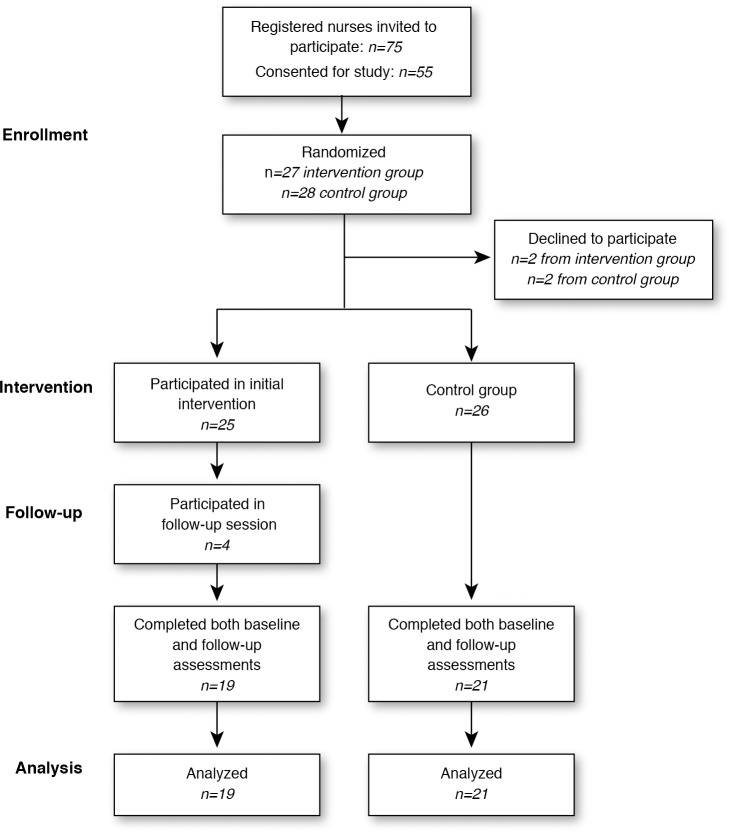
Of the 75 RN orientees invited to participate, 55 consented and were randomized—27 into the intervention arm and 28 into the control arm. Prior to the first group session, 2 participants from each group declined to participate. All 25 subjects in the intervention group participated in the first group session. Only 4 subjects were present at the follow-up session for the intervention group, mainly because of scheduling issues. Of the 51 participants enrolled, 40 completed the study (intervention group n=19, control group n=21) (Figure).
Figure.
Enrollment/retention diagram of the randomized trial testing the efficacy of a stress management program among nurses.
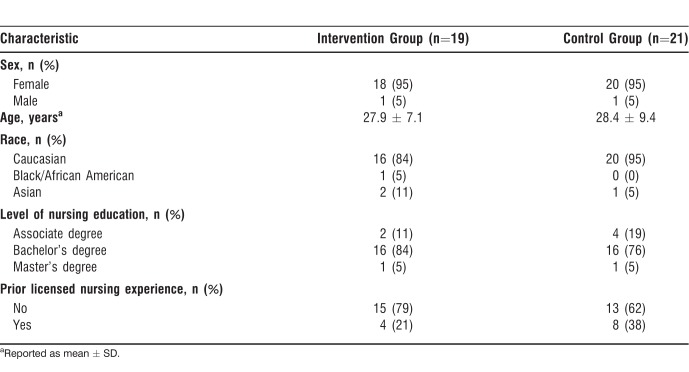
Demographics
Most participants were female (95%) and Caucasian (90%), with an average age of 28.2 years (Table 1). Additionally, most held a bachelor's degree as their highest degree in nursing (80%) and did not have previous experience as a licensed nurse (70%).
Table 1.
Baseline Characteristics of Nurses in a Stress Management Program Trial
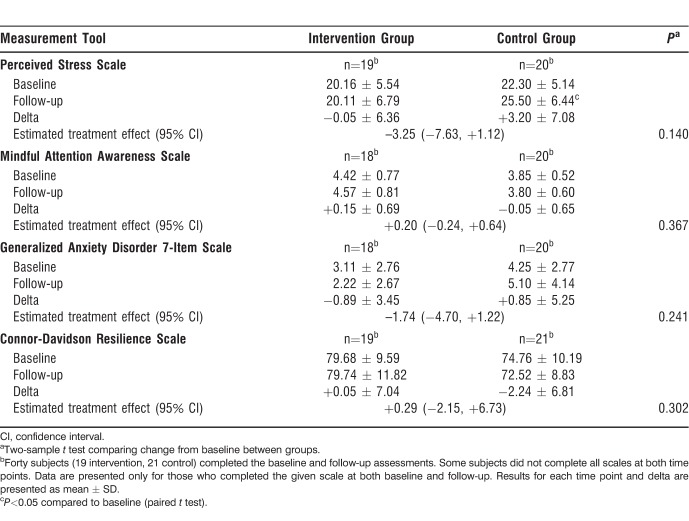
Efficacy Outcomes
The change in perceived stress (from baseline to week 12) did not differ significantly between those who received the SMART intervention vs those who did not (−0.05 ± 6.36 vs +3.20 ± 7.08 for SMART vs control, respectively, P=0.140; estimated treatment effect=−3.25; 95% confidence interval −7.63, +1.12). Changes in mindfulness, anxiety, and resilience also did not differ significantly between the groups (Table 2). The change in all 4 measures, however, was in the hypothesized direction: mindfulness and resilience levels improved for those in the intervention group and declined for those in the control group; stress and anxiety decreased for those in the intervention group and increased for those in the control group.
Table 2.
Efficacy Outcomes of a Stress Management Program Trial for Nurses
Qualitative Evaluation
Results from the program evaluation questionnaire included positive comments about the program as well as suggestions for improvement. The positive comments tended to reference the information received at the initial intervention that related to changing one's interpretation of events and practicing the SMART program principles. One participant noted, “All of the positive thinking tools have helped me the most. Sometimes in the past I would dwell on the negative and let it control my day. Now with the techniques I learned, I feel like I can take every situation and make it positive!” Another stated, “Forgiveness isn't something I think of often, so it was great to think about it once each week. I found it really helped me with personal relationships and difficult patients.” Suggestions for improvement tended to focus on the follow-up sessions. A participant noted, “The follow-up needs to have some kind of improvement. I found it difficult to keep the same kind of excitement about the program for the whole duration of the study. It would be helpful to have frequent meetings…even if it is for 10 minutes…I believe if [I had practiced it more], I would have benefited greatly.”
DISCUSSION
Our study shows the feasibility of integrating a stress management and resilience training program in a nurse orientation program. The relatively high rate of consent (73% of invited nurses) indicates interest among nurses in participating in this type of program. The study also showed trends toward efficacy of the program. The results, however, were not statistically significant.
The investigators found that enrolling participants in this study was relatively easy. However, despite the low intensity of the intervention (total time of 150 minutes), a high proportion (84%) of nurses in the intervention group were not able to participate in the follow-up session, mainly because of scheduling conflicts. The participants noted that the inability to attend the follow-up session negatively impacted their practice. A more streamlined scheduling system and protected nurse time are required to effectively implement such a program. In addition, nurse participants who voluntarily dropped out of the study indicated that it was because of an inability to make time for the program. Those who elected not to consent were feeling overwhelmed during the orientation period and thus were unable to commit to additional time, suggesting that the optimal time to offer such a program is prior to the start of the nurses' first orientation session to provide them with the skills to deal with the stress of orientation. Alternatively, a stress management and resilience training program could be offered after the initial orientation to avoid the sense of overload that some of the nurses expressed.
While the results were not statistically significant, the levels of stress, mindfulness, anxiety, and resilience all moved in a positive direction for the intervention group and in a negative direction for the control group. These results indicate a positive trend in outcomes only for those who participated in the intervention and provide a preliminary indication that the SMART program may be an effective intervention for influencing stress, mindfulness, anxiety, and resilience in new nurses. If a larger number of participants had attended the follow-up session and the intervention had been more intense, the results may have been positively influenced.
Interventions that have been tested to help nurses and other healthcare workers deal with stress can be divided into 2 categories: environmental management and individual-based approaches.36 A systematic review of the literature showed that person-directed interventions for reducing occupational stress in healthcare workers can significantly reduce stress, burnout, feelings of lack of personal accomplishment, and anxiety.37 The findings from this study preliminarily support that the SMART program, a person-directed approach to stress management, may be an effective intervention for managing nurse stress. The effectiveness of the program could be related to its emphasis on enhancing present-moment awareness and fostering positive emotions through the practices of gratitude, compassion, acceptance, forgiveness, and higher meaning. Other mindfulness-based coping intervention approaches could be considered for new nurses, such as Mindfulness-Based Stress Reduction (MBSR); however, the SMART program requires less in-person training time than MBSR, allowing easier integration into nurses' schedules.
Despite the randomized controlled design, this study has limitations. The open-label design restricted the ability to control for the Hawthorne effect. Future research could include a more credible control intervention. In addition, nurses in the control group may have worked closely with nurses in the intervention group, and that association could have led to crossover of the intervention. Although this pilot study included a small sample size, it provided valuable feasibility outcomes; however, future studies should employ a larger sample size to more effectively detect a difference between groups. The small number of participants who attended the follow-up intervention and the low intensity of the intervention may have negatively impacted the outcomes for the intervention group. Another limitation is generalizability of the results because of the lack of cultural diversity in the study sample. Diversity was restricted because of local demographics of nurses at the institution and could be improved by including other institutional sites in future studies that have a more diverse population of nurses.
CONCLUSION
Integrating the SMART program within the nurse orientation program is feasible; however, alterations to the program are warranted. The program has the potential to decrease stress and anxiety and to enhance mindfulness and resilience. For future studies, we would consider an alternative design that would include additional follow-up sessions; alternative methods for follow-up, such as teleconferences or web-based discussion; and a more effective scheduling system to allow nurses to attend all sessions. Based on this preliminary work and anecdotal comments from participants, our nursing education leadership has strongly supported offering a modified version of this stress management and resiliency training intervention to new nurses.
Footnotes
Dr Sood has a proprietary interest in a company that teaches resiliency programs. The other authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, and Interpersonal and Communication Skills.
REFERENCES
- 1.McVicar A. Workplace stress in nursing: a literature review. J Adv Nurs. 2003 Dec;44(6):633–642. doi: 10.1046/j.0309-2402.2003.02853.x. [DOI] [PubMed] [Google Scholar]
- 2.Delaney C. Walking a fine line: graduate nurses' transition experiences during orientation. J Nurs Educ. 2003 Oct;42(10):437–443. doi: 10.3928/0148-4834-20031001-05. [DOI] [PubMed] [Google Scholar]
- 3.Marshburn DM, Engelke MK, Swanson MS. Relationships of new nurses' perceptions and measured performance-based clinical competence. J Contin Educ Nurs. 2009 Sep;40(9):426–432. doi: 10.3928/00220124-20090824-02. [DOI] [PubMed] [Google Scholar]
- 4.Gelsema TI, van der Doef M, Maes S, Janssen M, Akerboom S, Verhoeven C. A longitudinal study of job stress in the nursing profession: causes and consequences. J Nurs Manag. 2006 May;14(4):289–299. doi: 10.1111/j.1365-2934.2006.00635.x. [DOI] [PubMed] [Google Scholar]
- 5.Mealer M, Burnham EL, Goode CJ, Rothbaum B, Moss M. The prevalence and impact of post-traumatic stress disorder and burnout syndrome in nurses. Depress Anxiety. 2009 Dec;26(12):1118–1126. doi: 10.1002/da.20631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berland A, Natvig GK, Gundersen D. Patient safety and job-related stress: a focus group study. Intensive Crit Care Nurs. 2008 Apr;24(2):90–97. doi: 10.1016/j.iccn.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 7.Virtanen M, Kurvinen T, Terho K, et al. Work hours, work stress, and collaboration among ward staff in relation to risk of hospital-associated infection among patients. Med Care. 2009 Mar;47(3):310–318. doi: 10.1097/MLR.0b013e3181893c64. [DOI] [PubMed] [Google Scholar]
- 8.Cimiotti JP, Aiken LH, Sloane DM, Wu ES. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012 Aug;40(6):486–490. doi: 10.1016/j.ajic.2012.02.029. Erratum in: Am J Infect Control. 2012 Sep;40(7):680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duvall JJ, Andrews DR. Using a structured review of the literature to identify key factors associated with the current nursing shortage. J Prof Nurs. 2010 Sep-Oct;26(5):309–317. doi: 10.1016/j.profnurs.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Godinez G, Schweiger J, Gruver J, Ryan P. Role transition from graduate to staff nurse: a qualitative analysis. J Nurses Staff Dev. 1999 May-Jun;15(3):97–110. doi: 10.1097/00124645-199905000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Strachota E, Normandin P, O'Brien N, Clary M, Krukow B. Reasons registered nurses leave or change employment status. J Nurs Adm. 2003 Feb;33(2):111–117. doi: 10.1097/00005110-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Oermann MH, Garvin MF. Stresses and challenges for new graduates in hospitals. Nurse Educ Today. 2002 Apr;22(3):225–230. doi: 10.1054/nedt.2001.0695. [DOI] [PubMed] [Google Scholar]
- 13.Richez M. Resilience-building strategies for nurses in transition. J Contin Educ Nurs. 2014 Feb;45(2):54–55. doi: 10.3928/00220124-20140124-12. [DOI] [PubMed] [Google Scholar]
- 14.Motowidlo SJ, Packard JS, Manning MR. Occupational stress: its causes and consequences for job performance. J Appl Psychol. 1986 Nov;71(4):618–629. [PubMed] [Google Scholar]
- 15.Dolan SL, Van Ameringen MR, Corbin S, Arsenault A. Lack of professional latitude and role problems as correlates of propensity to quit amongst nursing staff. J Adv Nurs. 1992 Dec;17(12):1455–1459. doi: 10.1111/j.1365-2648.1992.tb02817.x. [DOI] [PubMed] [Google Scholar]
- 16.Riahi S. Role stress amongst nurses at the workplace: concept analysis. J Nurs Manag. 2011 Sep;19(6):721–731. doi: 10.1111/j.1365-2834.2011.01235.x. [DOI] [PubMed] [Google Scholar]
- 17.Moustaka E, Constantinidis TC. Sources and effects of work-related stress in nursing. Health Sci J. 2010;4(4):210–216. [Google Scholar]
- 18.Dugan J, Lauer E, Bouquot Z, Dutro BK, Smith M, Widmeyer G. Stressful nurses: the effect on patient outcomes. J Nurs Care Qual. 1996 Apr;10(3):46–58. [PubMed] [Google Scholar]
- 19.O'Brien-Pallas L, Shamian J, Thomson D, et al. Work-related disability in Canadian nurses. J Nurs Scholarsh. 2004 Dec;36(4):352–357. doi: 10.1111/j.1547-5069.2004.04063.x. [DOI] [PubMed] [Google Scholar]
- 20.Allan JL, Farquharson B, Johnston DW, Jones MC, Choudhary CJ, Johnston M. Stress in telephone helpline nurses is associated with failures of concentration, attention and memory, and with more conservative referral decisions. Br J Psychol. 2014 May;105(2):200–213. doi: 10.1111/bjop.12030. [DOI] [PubMed] [Google Scholar]
- 21.Trybou J, Germonpre S, Janssens H, et al. Job-related stress and sickness absence among Belgian nurses: a prospective study. J Nurs Scholarsh. 2014 Jul;46(4):292–301. doi: 10.1111/jnu.12075. [DOI] [PubMed] [Google Scholar]
- 22.Sorour AS, El-Maksoud MM. Relationship between musculoskeletal disorders, job demands, and burnout among emergency nurses. Adv Emerg Nurs J. 2012 Jul-Sep;34(3):272–282. doi: 10.1097/TME.0b013e31826211e1. [DOI] [PubMed] [Google Scholar]
- 23.Dowd T, McCleery A. Elements of Buddhist philosophy in cognitive psychotherapy: the role of cultural specifics and universals. J Cogn Behav Psychother. 2007 Mar;7(1):67–79. [Google Scholar]
- 24.Farrow TF, Zheng Y, Wilkinson ID, et al. Investigating the functional anatomy of empathy and forgiveness. Neuroreport. 2001 Aug 8;12(11):2433–2438. doi: 10.1097/00001756-200108080-00029. [DOI] [PubMed] [Google Scholar]
- 25.Seitz RJ, Nickel J, Azari NP. Functional modularity of the medial prefrontal cortex: involvement in human empathy. Neuropsychology. 2006 Nov;20(6):743–751. doi: 10.1037/0894-4105.20.6.743. [DOI] [PubMed] [Google Scholar]
- 26.Sood A. Train Your Brain, Engage Your Heart, Transform Your Life: A Two Step Program to Enhance Attention; Decrease Stress; Cultivate Peace, Joy and Resilience; and Practice Presence with Love—A Course in Attention & Interpretation Therapy (AIT) Rochester, MN: Morning Dew Publications;; 2010. [Google Scholar]
- 27.Ochsner KN, Bunge SA, Gross JJ, Gabrieli JD. Rethinking feelings: an FMRI study of the cognitive regulation of emotion. J Cogn Neurosci. 2002 Nov 15;14(8):1215–1229. doi: 10.1162/089892902760807212. [DOI] [PubMed] [Google Scholar]
- 28.Ochsner KN, Ray RD, Cooper JC, et al. For better or for worse: neural systems supporting the cognitive down- and up-regulation of negative emotion. Neuroimage. 2004 Oct;23(2):483–499. doi: 10.1016/j.neuroimage.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983 Dec;24(4):385–396. [PubMed] [Google Scholar]
- 30.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003 Apr;84(4):822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 31.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 32.Löwe B, Decker O, Müller S, et al. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008 Mar;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 33.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003 Sep;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 34.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. 2007 Dec;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 35.Ahern NR, Kiehl EM, Sole ML, Byers J. A review of instruments measuring resilience. Issues Compr Pediatr Nurs. 2006 Apr-Jun;29(2):103–125. doi: 10.1080/01460860600677643. [DOI] [PubMed] [Google Scholar]
- 36.Mimura C, Griffiths P. The effectiveness of current approaches to workplace stress management in the nursing profession: an evidence based literature review. Occup Environ Med. 2003 Jan;60(1):10–15. doi: 10.1136/oem.60.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health. 2008 Jun;34(3):169–178. doi: 10.5271/sjweh.1240. [DOI] [PubMed] [Google Scholar]