Abstract
Background
Rhabdomyolysis is a complex medical condition involving the rapid dissolution of damaged or injured skeletal muscle.
Methods
This review focuses on the epidemiology, pathophysiology, causes, presentation, diagnosis, complications, management, and anesthetic considerations related to rhabdomyolysis.
Results
Any form of muscle damage––and by extension any entity that causes muscle damage––can initiate rhabdomyolysis. One of the most important treatment goals when rhabdomyolysis is suspected is avoiding acute kidney injury.
Conclusion
All clinicians should be aware of common causes, diagnosis, and treatment options.
Keywords: Rhabdomyolysis
INTRODUCTION
Rhabdomyolysis is a complex medical condition involving the rapid dissolution of damaged or injured skeletal muscle. This disruption of skeletal muscle integrity leads to the direct release of intracellular muscle components, including myoglobin, creatine kinase (CK), aldolase, and lactate dehydrogenase, as well as electrolytes, into the bloodstream and extracellular space. Rhabdomyolysis ranges from an asymptomatic illness with elevation in the CK level to a life-threatening condition associated with extreme elevations in CK, electrolyte imbalances, acute renal failure (ARF), and disseminated intravascular coagulation.1 Although rhabdomyolysis is most often caused by direct traumatic injury, the condition can also be the result of drugs, toxins, infections, muscle ischemia, electrolyte and metabolic disorders, genetic disorders, exertion or prolonged bed rest, and temperature-induced states such as neuroleptic malignant syndrome (NMS) and malignant hyperthermia (MH).2 Massive necrosis, manifested as limb weakness, myalgia, swelling, and commonly gross pigmenturia without hematuria, is the common denominator of both traumatic and nontraumatic rhabdomyolysis.3
The earliest known description of this condition appears in the Old Testament's Book of Numbers that records a plague suffered by the Jews during their exodus from Egypt after consuming large amounts of quail.4 The plague is widely assumed to be a reference to the signs and symptoms of myolysis, a long-observed outcome in the Mediterranean after the intake of quail.5,6 Myolysis seemingly occurs because of the poisonous hemlock that quail consume during the spring migration.7,8 In modern times, one of the first medical descriptions of rhabdomyolysis is in German medical literature from the early 1900s, where it is termed Meyer-Betz disease.9 Bywaters and Beall are often credited with the first account of the pathophysiologic mechanisms of the syndrome and the accurate depiction of the link between rhabdomyolysis and ARF.10,11
Clinically, rhabdomyolysis is exhibited by a triad of symptoms: myalgia, weakness, and myoglobinuria, manifested as the classically described tea-colored urine. However, this rigid depiction of symptoms can be misleading as the triad is only observed in <10% of patients, and >50% of patients do not complain of muscle pain or weakness, with the initial presenting symptom being discolored urine.2 An elevated CK level is the most sensitive laboratory test for evaluating an injury to muscle that has the potential to cause rhabdomyolysis (assuming no concurrent cardiac or brain injury).1 Attempts to correlate the elevation in CK level with the severity of muscle damage and/or renal failure have had mixed results, although significant muscle injury is likely at CK levels >5,000 IU/L.1,9 Treatment for rhabdomyolysis, at least initially, is mainly supportive, centering on the management of the ABCs (airway, breathing, circulation) and measures to preserve renal function, including vigorous rehydration.
EPIDEMIOLOGY
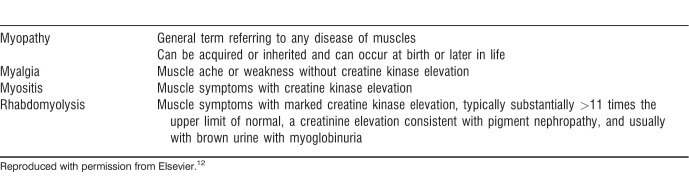
Historically, the incidence of myopathic events and rhabdomyolysis has been challenging to evaluate in clinical research because of a lack of formal clinical definitions. In 2002, the American College of Cardiology (ACC), American Heart Association (AHA), and National Heart, Lung, and Blood Institute (NHLBI) jointly released the Clinical Advisory on the Use and Safety of Statins in an attempt to resolve this issue.12 Their recommended definitions are presented in Table 1.
Table 1.
Definitions of Muscle Toxicity and Rhabdomyolysis by Clinical Advisory
Because ARF is the most significant and acutely life-threatening complication of rhabdomyolysis, it is important to look at the link between the two. An estimated 10%-40% of patients with rhabdomyolysis develop ARF, and up to 15% of all cases of ARF can be attributed to rhabdomyolysis.13 Previous studies have suggested that the percentage of children with rhabdomyolysis who develop ARF may be even higher, as much as 42%-50%.14,15 However, because of varying clinical scenarios, settings, and the confounding variables introduced by comorbid conditions, more precise estimates have been difficult to obtain.
PATHOPHYSIOLOGY
While the etiology of a specific case of rhabdomyolysis is often known, the exact pathways by which the various insults that can cause this syndrome ultimately lead to muscle injury and necrosis are less clear. Much clearer is the picture of the final common events shared by the diverse etiologies of rhabdomyolysis. Irrespective of the initial insult, the final steps leading to rhabdomyolysis involve either direct myocyte injury or a failure of the energy supply within the muscle cells.16
During normal muscle physiology at rest, ion channels (including Na+/K+ pumps and Na+/Ca2+ exchangers) located on the plasma membrane (sarcolemma) maintain low intracellular Na+ and Ca2+ concentrations and high K+ concentrations within the muscle fiber. Muscle depolarization results in an influx of Ca2+ from the reserves stored in the sarcoplasmic reticulum into the cytoplasm (sarcoplasm), causing the muscle cells to contract through actin-myosin cross-linking. All of these processes are dependent on the availability of sufficient energy in the form of adenosine triphosphate (ATP). Therefore, any insult that damages the ion channels through direct myocyte injury or reduces the availability of ATP for energy will cause a disruption in the proper balance of intracellular electrolyte concentrations.
When muscle injury or ATP depletion occurs, the result is an excessive intracellular influx of Na+ and Ca2+. An increase in intracellular Na+ draws water into the cell and disrupts the integrity of the intracellular space. The prolonged presence of high Ca2+ levels intracellularly leads to a sustained myofibrillar contraction that further depletes ATP.16 Also, the elevation in Ca2+ activates Ca2+-dependent proteases and phospholipases, promoting lysis of the cellular membrane and further damage to the ion channels.1 The end result of these alterations within the muscle cell milieu is an inflammatory, self-sustaining myolytic cascade that causes necrosis of the muscle fibers and releases the muscle contents into the extracellular space and the bloodstream.10 Figure 1 illustrates this process, showing how a wide array of insults can ultimately coalesce upon a final common effector pathway to initiate the rhabdomyolysis cascade.
Figure 1.
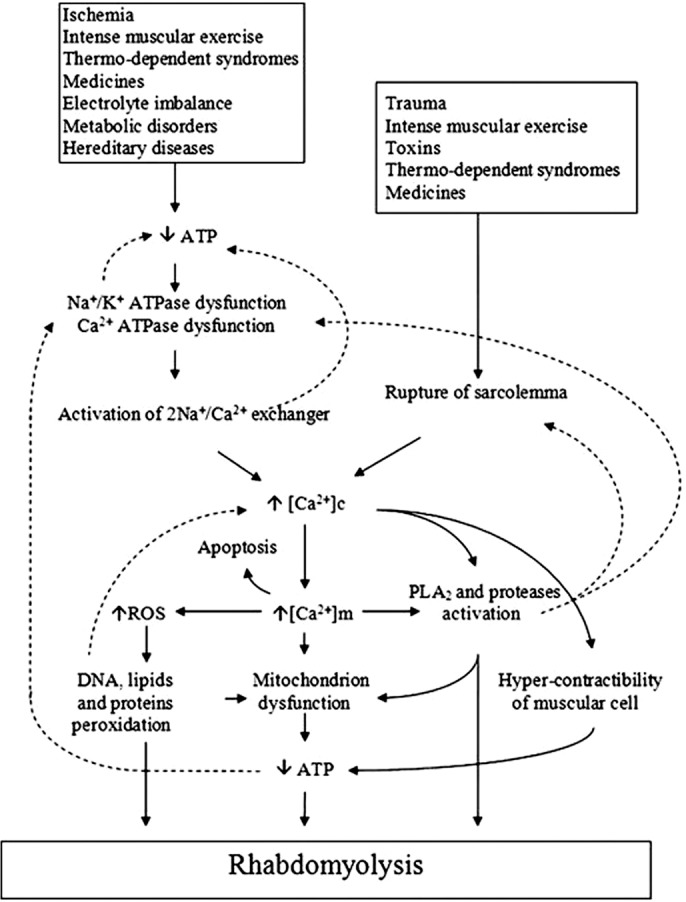
Mechanisms of rhabdomyolysis. Reproduced with permission from Elsevier.17 ATP, adenosine triphosphate; ATPase, adenosine triphosphatase; DNA, deoxyribonucleic acid; PLA, polylactic acid; ROS, reactive oxygen species.
CAUSES
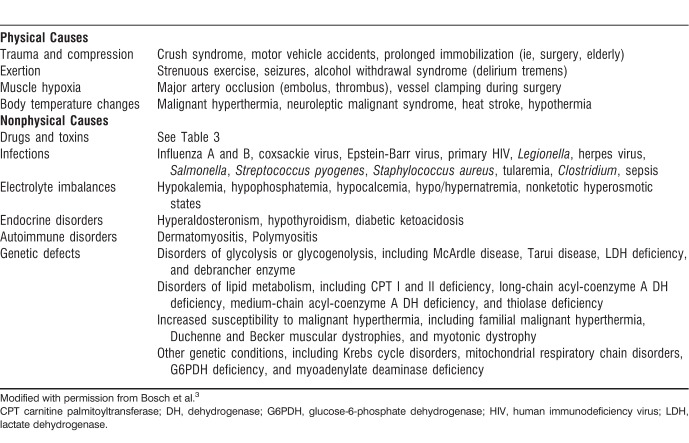
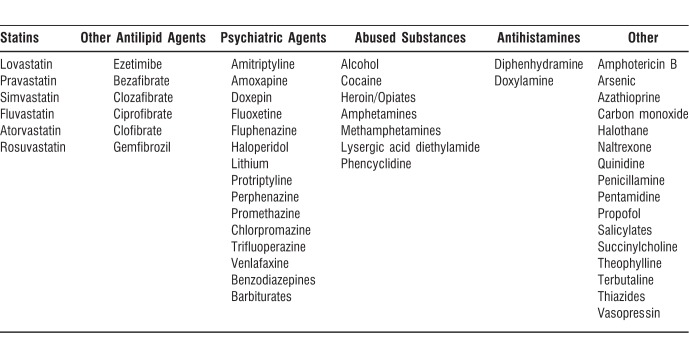
Theoretically, any form of muscle damage and, by extension, any entity that leads to or causes muscle damage, can initiate rhabdomyolysis. In adults, the available data show that the most common causes of rhabdomyolysis are drug or alcohol abuse, medicinal drug use, trauma, NMS, and immobility.18 The data in the pediatric population skew toward different leading causes, suggesting that viral myositis, trauma, connective tissue disorders, exercise, and drug overdose are responsible for much of the rhabdomyolysis seen in these patients; viral myositis alone may account for up to one-third of pediatric cases of rhabdomyolysis.14,15,19 While not a comprehensive list, many of the causes of rhabdomyolysis, both physical and nonphysical, are listed in Table 2. Table 3 lists drugs and other agents that can cause rhabdomyolysis. A few of the frequent causes are explored in more depth below.
Table 2.
Physical and Nonphysical Causes of Rhabdomyolysis
Table 3.
Drugs and Other Agents That Can Cause Rhabdomyolysis
Statins
The link between statins, 3-hydroxymethyl-3-methylglutaryl coenzyme A reductase inhibitors, and drug-induced myalgia and rhabdomyolysis has been the topic of much investigation since the introduction of this drug class in the 1980s. Statins have rapidly become the most widely prescribed class of drugs in the world because of their therapeutic benefit on the mortality of patients with preexisting cardiovascular disease, the leading cause of death in industrialized nations.20 However, the risk for statin-induced myopathy is real and should always be considered when adding this drug to a patient's regimen.
In 2012, the US Food and Drug Administration (FDA) issued a notification concerning the use of statins and their potential side effects, including liver injury, cognitive decline, type 2 diabetes mellitus, and myopathy/rhabdomyolysis. The warning labels on all statin medications were expanded to include these potential side effects; in particular, the label for Mevacor (lovastatin) was required to incorporate contraindications to taking the drug with a variety of other agents, including human immunodeficiency virus (HIV) protease inhibitors and certain antibacterial and antifungal medications.21 At the same time, the FDA removed its requirement to periodically monitor the liver enzymes of patients taking statins, because monitoring had shown no benefit in detecting or preventing serious liver injury.21 The FDA now recommends acquiring baseline levels of liver enzymes prior to starting statin therapy and checking enzyme levels if clinically necessary thereafter.
Randomized controlled trials estimate the incidence of myopathic events in patients taking statins at 1.5%-5.0%; however, in clinical practice, these rates have varied from 0.3%-33%.22-24 This disconnect likely has two causes. First, the lack of a consensus definition of the terminology used to describe myopathic events likely leads to myopathic events being underreported and underdiagnosed. Second, many of the randomized controlled trials exclude patients with renal insufficiency, hepatic insufficiency, a history of muscle complaints, hypertriglyceridemia, and poorly controlled diabetes to minimize muscle toxicity.25,26
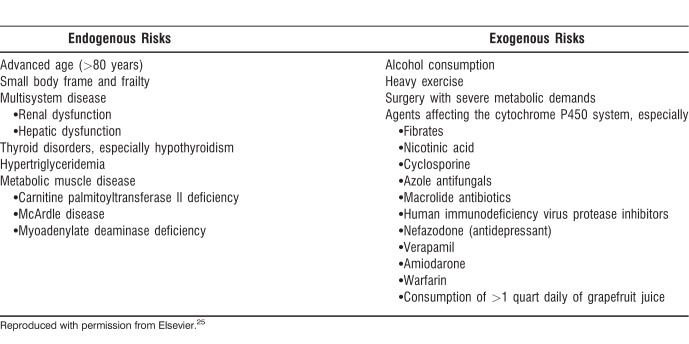
Risk factors for the development of statin-induced rhabdomyolysis include high dosages, advanced age, female sex, renal or hepatic insufficiency, and diabetes mellitus.1 Table 4 provides a more comprehensive list of proposed risk factors.
Table 4.
Proposed Risk Factors for Statin-Induced Rhabdomyolysis
Despite the high incidence of general muscle toxicity because of statin use, rhabdomyolysis secondary to statin use has proven to be extremely rare.23 Guyton suggests that the mortality risk associated with rhabdomyolysis is far outweighed by the reduction in all-cause mortality seen with statin use.27 An analysis of 30 randomized controlled trials (n=83,858) identified 7 vs 5 cases of rhabdomyolysis when comparing patients who received statin therapy vs placebo, respectively.28 The FDA Adverse Event Reporting System (FAERS) reported rates of 1.07 cases of rhabdomyolysis per 1 million statin prescriptions from 1998-2000, with an increase to 3.56 cases per 1 million statin prescriptions from 2002-2004.29 The FAERS also documented that rhabdomyolysis rates were lowest for pravastatin (1.63 cases) and highest for rosuvastatin (13.54 cases).29 These numbers from the FAERS were limited because of a reliance on self-reporting and the requirement for much higher elevations in CK for classification of rhabdomyolysis compared to the ACC/AHA/NHLBI definitions.29
Davidson et al looked at the rates of fatal rhabdomyolysis based on the 2001 FAERS data and found that they varied by statin.29 The 2001 data showed one reported case of fatal rhabdomyolysis per 5.2 million lovastatin prescriptions, 8.3 million simvastatin prescriptions, 23.4 million atorvastatin prescriptions, and 27.1 million pravastatin prescriptions.29 Staffa et al reported no fatal rhabdomyolysis events in a separate study with patients taking fluvastatin.30 According to Cervellin et al, the FAERS data from 2001 showed a rate of one case of fatal rhabdomyolysis per 316,000 prescriptions for cerivastatin, a statin that was pulled from the market in 2001 because of high rates of fatal rhabdomyolysis, especially when taken in conjunction with fibrates, most notably gemfibrozil.2 Cerivastatin has been shown to increase the risk of rhabdomyolysis up to 12-fold.31 In an FDA study during 29 months, the occurrence of rhabdomyolysis was most common with simvastatin (36%) and cerivastatin (32%); less common occurrences were seen with atorvastatin (12%), pravastatin (12%), lovastatin (6%), and fluvastatin (2%).32
Cytochrome P450 Inhibitors
The potential for increased risk of myopathy and rhabdomyolysis when statins are taken in conjunction with other commonly used pharmaceuticals further complicates statin therapy. Statin-induced rhabdomyolysis is related to drug interactions in approximately 60% of cases.33 Often, these interactions happen because both statins and commonly coadministered drugs are metabolized by the cytochrome P450 system.
Not all statins, however, share the same physiochemical properties. Some statins (atorvastatin, simvastatin, and lovastatin) undergo phase I metabolism by cytochrome P450 3A4 and are called 3A4 substrates, while other statins (pravastatin, fluvastatin, and rosuvastatin) are not metabolized by the 3A4 isoenzyme.34 This same 3A4 isoenzyme is also responsible for the metabolism of >50% of marketed pharmaceuticals.34 Administration of 3A4 inhibitors with a statin leads to significantly increased plasma statin levels, in turn leading to considerable statin toxicity.34 Drugs that are 3A4 inhibitors and are often prescribed with statins include fibrates (especially gemfibrozil), calcium channel blockers, histamine H2 antagonists, antibiotics (eg, clarithromycin), antifungals (eg, itraconazole), antidepressants, antiretroviral drugs (eg, protease inhibitors), and immunosuppresives (eg, cyclosporine).
A 2004 study by Jacobson evaluating multiple-dose pharmacokinetic interaction profiles showed that both simvastatin and atorvastatin (3A4 substrates) had significant changes in their pharmacokinetics when coadministered with various 3A4 inhibitors, with as much as a 5-fold increase in the incidence of myopathy.35 Fluvastatin (metabolized mainly by cytochrome P450 2C9) and pravastatin (not a major substrate of the cytochrome P450 system) showed significant changes in their pharmacokinetics when administered with 3A4 inhibitors.35 Similarly, Law and Rudnicka showed that the incidence of rhabdomyolysis was higher for patients receiving lovastatin, simvastatin, and atorvastatin and lower for those receiving fluvastatin and pravastatin, echoing the data from the FAERS.36 They postulated that the reason is that lovastatin, simvastatin, and atorvastatin are metabolized by cytochrome P450 3A4 while fluvastatin and pravastatin are not.
One specific interaction that has been widely studied and is clinically significant given the comorbidities often found in patients is the interaction between statins and fibrates. A review of 36 published clinical trials involving the use of a statin-fibrate combination therapy found a 0.12% prevalence of myopathic events.37 The Davidson et al FAERS study also looked at the rates of rhabdomyolysis when either fenofibrate or gemfibrozil was used in conjunction with various statins.29 The data showed that while both fenofibrate and gemfibrozil use with any statin led to an increased rate of rhabdomyolysis compared to the use of a statin alone, the use of fenofibrate with a statin resulted in fewer reports of rhabdomyolysis (4.5 cases per million prescriptions) than the use of gemfibrozil with a statin (87 cases per million prescriptions).29 Notably, only 2.3% (14 of 606) reports of rhabdomyolysis with fibrate/statin therapy resulted from the use of cerivastatin and fenofibrate, whereas 88% (533 of 606) reports of rhabdomyolysis were caused by the use of cerivastatin and gemfibrozil.38 Recent studies have suggested that the increased observation of myotoxicity seen with gemfibrozil/statin therapy may be partly because of gemfibrozil's ability to inhibit the glucuronidation of statins, thereby leading to a decreased rate of statin elimination from the body and increased plasma concentrations of statins.38 Fenofibrate has shown no capacity for affecting either the glucuronidation or oxidation of statins.39,40
Trauma
Blunt injuries and crush injuries are common causes of trauma-induced rhabdomyolysis. Interestingly, for crush injuries associated with severe natural disasters or man-made traumatic events such as bombings, earthquakes, or building collapses, the onset of rhabdomyolysis is noted to occur only once the acute compression of muscle is relieved, thereby allowing the products of muscle breakdown to enter the circulatory system.17 High-voltage electrical injuries (ie, electrocution or lightning strikes) are other causes of trauma-induced rhabdomyolysis. Up to 10% of patients who survive the initial electrical accident are estimated to develop rhabdomyolysis.10
Exercise/Exertion
One of the major challenges in diagnosing exertional rhabdomyolysis is the fact that serum CK levels will naturally rise after strenuous exercise in almost all normal humans, potentially up to 10 times the higher limit of normal.41 The increase in CK levels also varies widely among patients, and it is possible for one individual to develop exertional rhabdomyolysis while exerting the same energy under the same conditions as another individual who does not develop exertional rhabdomyolysis.41 Increased temperature and humidity during exercise/exertion may also play a role in higher rates of rhabdomyolysis.42 A retrospective cohort study of military personnel enrolled in basic military training showed 22.2 cases of exertional rhabdomyolysis per 100,000 recruits per year.43 The same study showed that the incidence and risk of recurrence for exertional rhabdomyolysis were low among young, physically active individuals.
Temperature, NMS, and MH
Heat stroke, NMS, and MH have the potential to cause rhabdomyolysis.
Heat stroke occurs when a patient's core body temperature exceeds 40.5°C. Prolonged exposure to extremely high temperatures can lead to the development of not only rhabdomyolysis but also associated hypotension, lactic acidosis, hypoglycemia, disseminated intravascular coagulation, and multiorgan failure.43 Interestingly, exertional heat stroke is rarely seen in females, perhaps because of the protective effect that increased estrogen levels in women have on muscle.44 For this reason, women who present with rhabdomyolysis seemingly because of heat stroke should be investigated for underlying muscle disease or other exogenous factors.44
NMS, often seen in conjunction with the use of antipsychotic medications (usually first generation/atypical antipsychotics such as haloperidol), can lead to the development of rhabdomyolysis, likely because of the massive generation of heat caused by the rigidity and tremor in patients who develop NMS.43 The exact mechanism of insult is thought to result from either a central nervous system dopamine receptor blockade or from withdrawal of an exogenous dopaminergic agonist.1
MH has been shown to be an autosomal dominant genetic disorder in 50% of affected individuals and an autosomal recessive genetic disorder in another 20% of affected individuals.1 Similar to NMS, symptoms include skeletal muscle rigidity, hyperventilation, tachycardia, fever, hemodynamic instability, and lactic acidosis.43 MH usually occurs in the setting of general anesthesia in predisposed patients, and the incidence of MH has been approximated at 1 in 15,000 anesthetic uses in children and 1 in 50,000-100,000 anesthetic uses in adults.45
Muscle Ischemia
Muscle cell necrosis can result from prolonged periods of oxygen deprivation to muscle, ultimately precipitating rhabdomyolysis and ARF. Causes of localized muscle ischemia include compression of blood vessels during surgery or otherwise, thromboses, emboli, compartment syndrome, carboxyhemoglobinemia, or sickle cell disease.17 Although rare, hypothermia can lead to the development of rhabdomyolysis by reducing muscle perfusion.1,17
Infection
Rhabdomyolysis has been described in all types of infections, ranging from localized muscle infections with erythema (bacterial pyomyositis) to patients with sepsis and no direct muscle infection.1,46 Proposed mechanisms for the development of rhabdomyolysis include tissue hypoxia secondary to sepsis or dehydration, toxin release, associated fever, direct bacterial invasion of muscle, or rigors/tremors.1 Classically, Legionella bacteria have been associated with bacterial rhabdomyolysis.47 Viral infections have also been implicated in rhabdomyolysis development, most commonly influenza A and B viruses.48,49 Rhabdomyolysis because of other viruses such as HIV,50 coxsackie virus,51 Epstein-Barr virus,52 Cytomegalovirus,53 herpes simplex virus,54 varicella zoster virus,55 and West Nile virus56 has also been described.
SYMPTOMS/PRESENTATION
Presenting symptoms tend to reflect the primary disease process, as well as superimposed symptoms of renal failure or muscle injury. The classic triad of symptoms of rhabdomyolysis consists of myalgia, weakness, and tea-colored urine. The muscle mass of the patient, the concentration of urine, and glomerular function can affect the color of the urine. Gabow et al, in a study of 87 cases (CK >500 IU/L), found that 26% of patients tested negative with the urine orthotolidine-toluidine dipstick test for myoglobin.57 Mannix et al showed that common presenting symptoms of pediatric rhabdomyolysis, regardless of kidney injury, were muscle pain, fever, and viral prodromes.19 Dark or tea-colored urine was reported in only 3.6% of cases.19 Patients may also have tense and swollen muscles on examination. The classic triad is observed in <10% of patients only, and >50% of patients do not complain of muscle pain or weakness. Systemic manifestations may include tachycardia, general malaise, fever, and nausea and vomiting and as such are nonspecific. The clinical manifestations of ARF, disseminated intravascular coagulation, and multiorgan failure may subsequently appear.2
DIAGNOSIS
The physician must have a high index of suspicion and a thorough history and physical examination to accurately diagnose rhabdomyolysis. With the classic triad being observed in only <10% of patients, any patient with known risk factors––including trauma, sepsis, muscular disease, and immobilization––should be suspected for rhabdomyolysis. Other indirect clues include the presence of muscle injury with an unexpected rise in serum phosphate or aspartate transaminase. A neuromuscular examination focusing on the extremities can also give important physical clues. Color, pulse, sensation, muscle power, and size are all informative, even in nonverbalizing patients.16 The gold standard for laboratory diagnosis is the determination of plasma CK. Although a cutoff threshold has not been established, a concentration 5 times the upper limit of the normal reference range (ie, 1,000 IU/L) is commonly used.2 CK level is generally considered predictive of the likelihood of developing ARF, and a concentration >5,000 IU/L is closely related to the development of kidney damage. CK has a half-life of 1.5 days. As a consequence, CK blood levels remain increased longer than the concentration of myoglobin that has a half-life of 2-4 hours. Myoglobin concentrations tend to normalize within 6-8 hours following the muscle injury.2 Plasma myoglobin is not as sensitive as CK for diagnosis because of its short half-life, resulting in false-negative tests.16 Urine myoglobin will show erythrocyte positivity on urine dipstick because the orthotoluidine portion of the dipstick turns blue in the presence of myoglobin.
SELECTED COMPLICATIONS
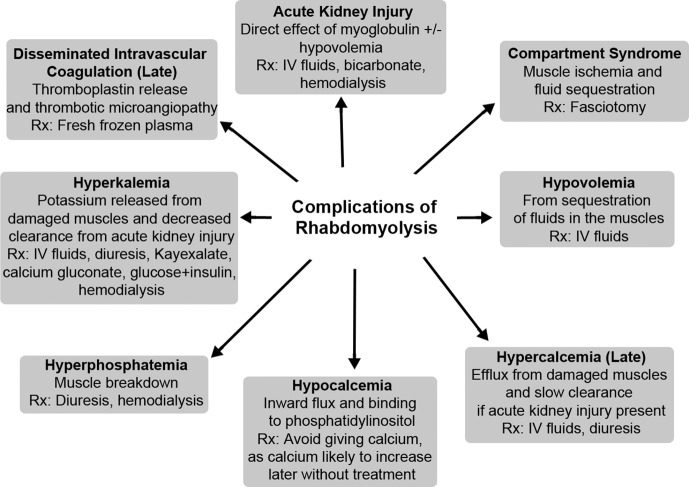
Potential complications of rhabdomyolysis include compartment syndrome and acute kidney injury. Figure 2 lists these and other complications often seen with rhabdomyolysis, as well as initial treatments associated with each complication.
Figure 2.
Complications of rhabdomyolysis.
Reproduced with permission from Springer.59 IV, intravenous; Rx, treatment.
Compartment Syndrome
Posttraumatic and/or ischemic muscle damage to muscle groups sheathed in noncompliant fascia leads to an elevation in intracompartmental hypertension.58 The muscle compartments are subjected to further muscle damage and pressure once the crushed muscle becomes engorged with blood and becomes edematous, a condition referred to as rebound hyperperfusion. This excessive blood flow and compromised lymphatic drainage can compromise arteriolar perfusion. Once the pressure is sufficient to collapse arterioles, effective perfusion of muscles and nerves stops with the onset of compartment syndrome,2 generally seen when intracompartmental pressure is >30 mmHg. Further muscle damage is manifested as the second wave phenomenon, the persistent elevation or rebound elevation in CK levels 48-72 hours after the initial insult.17
Acute Kidney Injury
Acute kidney injury is the most serious complication of rhabdomyolysis in the days following initial presentation and develops in 33% of patients.17 It is well accepted that acute kidney injury is the result of accumulation of myoglobin, which is nephrotoxic, in the kidney. Hypovolemia is another associated factor that leads to renal hypoperfusion.
Various clinical factors are used to predict the risk of acute kidney injury, including serum CK, creatinine, potassium, and Ca2+ levels, as well as the urine myoglobin level, but no single parameter has been established.17
MANAGEMENT
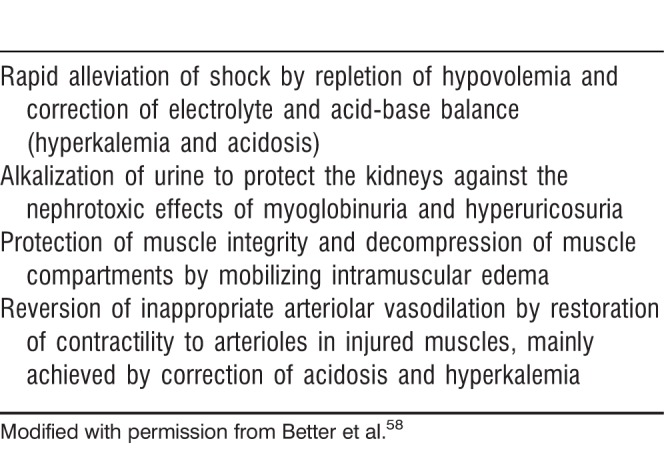
When rhabdomyolysis is suspected, regardless of the underlying etiology, one of the most important treatment goals is to avoid acute kidney injury. Because of the possible accumulation of fluids in muscular compartments and the associated hypovolemia, fluid management is imperative to prevent prerenal azotemia. Azotemia is prevented primarily by aggressive hydration at a rate of 1.5 L/h.59 Another option is 500 mL/h saline solution alternated every hour with 500 mL/h of 5% glucose solution with 50 mmol of sodium bicarbonate for each subsequent 2-3 L of solution. A urinary output goal of 200 mL/h, urine pH >6.5, and plasma pH <7.5 should be achieved.2 Table 5 outlines the aims of aggressive fluid resuscitation for rhabdomyolysis in an acute setting. Notably, urinary alkalization with sodium bicarbonate or sodium acetate is unproven, as is the use of mannitol to promote diuresis.60 Drugs such as statins that are known to be a risk factor for rhabdomyolysis should also be immediately stopped. Fasciotomy may be required in compartment syndrome to limit damage to muscles and kidneys.
Table 5.
Aims of Early Vigorous Fluid Resuscitation in Rhabdomyolysis
ANESTHETIC CONSIDERATIONS
Data related to anesthetic choices in patients with rhabdomyolysis are lacking, perhaps because of the rarity of the disease. However, many retrospective studies discuss the treatment of patients with muscular dystrophies. These patients are at an increased risk of general anesthetic-related hazards, including rhabdomyolysis.61 In a review by Muenster et al of 232 patients with Duchenne muscular dystrophy, the patients were treated with total intravenous anesthesia, using no volatile anesthetic agents, and with opioids and nondepolarizing muscle relaxants depending on the type and duration of the surgical procedure at the discretion of the anesthetist.61 If a muscle relaxant is used, succinylcholine must be avoided, and monitoring of muscle relaxation is performed by acceleromyography.61 Nitrous oxide and propofol were used for induction. Muenster et al found no serious anesthetic complications and no cases of rhabdomyolysis.61 Segura et al found in their review of 117 patients with dystrophinopathies that succinylcholine may trigger rhabdomyolysis, hyperkalemia, and cardiac arrest; however, evidence regarding the use of inhalational anesthetics was lacking.62 Segura et al also found no cases of rhabdomyolysis with total intravenous anesthesia in their retrospective study and no evidence for or against volatile anesthetic usage in this patient population.62 No anesthetic agent is risk free; rhabdomyolysis has been reported with nontriggering anesthetics, barbiturates, benzodiazepines, propofol, ketamine, and fasting.62
Ketamine
Ketamine hydrochloride is often used in the operating room as a dissociative anesthetic for procedural sedation.63 Ketamine, an analog of phencyclidine, is hypothesized to produce agitation and prolonged muscular activity that may ultimately lead to the development of rhabdomyolysis.63 Weiner et al showed this result in their case study of 20 patients aged 15-40 who presented to the emergency room after ketamine abuse; 2 of the 20 patients developed clinical rhabdomyolysis.64
Succinylcholine
Succinylcholine is a common neuromuscular depolarizing agent used in operating rooms to induce muscle relaxation and short-term paralysis, usually as a precursor to tracheal intubation. In addition, succinylcholine has long been known to cause succinylcholine-induced MH, a phenomenon that often occurs concurrently with clinically significant rhabdomyolysis.65 However, the popularity of succinylcholine in the operating room––especially in trauma situations––remains high despite its potentially life-threatening complications because succinylcholine is believed to have the fastest onset of action and the shortest duration of action of all the muscle relaxants.
Although the mechanism of succinylcholine-induced rhabdomyolysis remains elusive, there have been numerous reports of this phenomenon.66 When rhabdomyolysis occurs in the setting of succinylcholine administration, severe hyperkalemia and, potentially, cardiac arrest occur.65 Most patients with rhabdomyolysis after administration of succinylcholine are subsequently found to also have concomitant MH or an undiscovered muscular dystrophy.65 In fact, succinylcholine-induced rhabdomyolysis in a patient after the onset of puberty is rare if no underlying cause is present.67 The mortality rate for patients with undiscovered muscular dystrophies who develop cardiac arrest as a result of succinylcholine-induced rhabdomyolysis appears to be approximately 30%.65 However, the link between succinylcholine and rhabdomyolysis in patients with muscular dystrophies needs to be investigated further, as rhabdomyolysis can still be seen in this patient population under general anesthesia when succinylcholine is not used.65
Propofol
Coined by Bray in 1998, propofol-infusion syndrome (PRIS) was initially used to describe a clinical state observed in children, usually critically ill, who had been sedated on propofol for a prolonged period of time.68 Since its initial discovery, the syndrome has been noted in adults as well, with the first PRIS-related adult death reported in 2000.69 The syndrome does not appear to be unique to critically ill patients, as PRIS has been reported in healthy patients and patients on short-term, high-dose propofol infusions.70,71 Among the widely varying signs and symptoms associated with PRIS, rhabdomyolysis is an often-observed symptom that usually occurs later in the course of the syndrome.68 Risk factors for PRIS are severe head injury, airway infection, young age, large total cumulative dose, high catecholamine and serum glucose levels, low carbohydrate/high fat intake, critical illness, and inborn errors of metabolism.68 Rhabdomyolysis has been shown to be an independent risk factor for death as a result of PRIS.68
The first large, prospective study of PRIS looked at the development of PRIS in patients in the intensive care unit in 11 medical centers who were given a propofol infusion for >24 hours.72 PRIS was strictly defined as metabolic acidosis and cardiac dysfunction, along with one of the following: rhabdomyolysis, hypertriglyceridemia, or renal failure.72 The study showed a 1.1% incidence of PRIS in the patient population while also revealing that 91% of patients who developed PRIS were on a vasopressor. However, only 18% of patients had received propofol at a rate of >5 mg/kg/h, lending credence to the hypothesis that the total cumulative dose, rather than the rate of infusion, may be a better predictor of the development of PRIS.72
CONCLUSION
Rhabdomyolysis is a complex process associated with morbidity and mortality. Although the condition is often caused by direct traumatic injury, other potential etiologies are drugs, toxins, infections, muscle ischemia, electrolyte and metabolic disorders, genetic disorders, exertion or prolonged bed rest, and temperature-induced states such as NMS and MH. Rhabdomyolysis is exhibited by a triad of symptoms including myalgia, weakness, and myoglobinuria, with an elevation in CK level being the most sensitive test for muscle injury–induced rhabdomyolysis. All clinicians should be aware of common causes, diagnosis, and treatment options.
Footnotes
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care and Medical Knowledge.
REFERENCES
- 1.Huerta-Alardín AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis––an overview for clinicians. Crit Care. 2005 Apr;9(2):158–169. doi: 10.1186/cc2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cervellin G, Comelli I, Lippi G. Rhabdomyolysis: historical background, clinical, diagnostic and therapeutic features. Clin Chem Lab Med. 2010 Jun;48(6):749–756. doi: 10.1515/CCLM.2010.151. [DOI] [PubMed] [Google Scholar]
- 3.Bosch X, Poch E, Grau JM. Rhabdomyolysis and acute kidney injury. N Engl J Med. 2009 Jul 2;361(1):62–72. doi: 10.1056/NEJMra0801327. [DOI] [PubMed] [Google Scholar]
- 4.Book of Numbers. 11:18–34. [Google Scholar]
- 5.Korkmaz I. Kukul Güven FM, Eren SH, Dogan Z. Quail consumption can be harmful. J Emerg Med. 2011 Nov;41(5):499–502. doi: 10.1016/j.jemermed.2008.03.045. [DOI] [PubMed] [Google Scholar]
- 6.Billis AG, Kastanakis S, Giamarellou H, Daikos GK. Acute renal failure after a meal of quail. Lancet. 1971 Sep 25;2(7726):702. doi: 10.1016/s0140-6736(71)92264-1. [DOI] [PubMed] [Google Scholar]
- 7.Lewis DC, Metallinos-Katzaras E, Grivetti LE. Coturnism: human poisoning by European migratory quail. J Cultur Geogr. 1987;7(2):51–65. [Google Scholar]
- 8.Rizzi D, Basile C, Di Maggio A, et al. Clinical spectrum of accidental hemlock poisoning: neurologic manifestations, rhabdomyolysis and acute tubular necrosis. Nephrol Dial Transplant. 1991;6(12):939–943. doi: 10.1093/ndt/6.12.939. [DOI] [PubMed] [Google Scholar]
- 9.Bagley WH, Yang H, Shah KH. Rhabdomyolysis. Intern Emerg Med. 2007 Oct;2(3):210–218. doi: 10.1007/s11739-007-0060-8. [DOI] [PubMed] [Google Scholar]
- 10.Vanholder R, Sever MS, Erek E, Lameire N. Rhabdomyolysis. J Am Soc Nephrol. 2000 Aug;11(8):1553–1561. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- 11.Bywaters EG, Beall D. Crush injuries with impairment of renal function. Br Med J. 1941 Mar 22;1(4185):427–432. doi: 10.1136/bmj.1.4185.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pasternak RC, Smith SC, Jr, Bairey-Merz CN, et al. ACC/AHA/NHLBI Clinical Advisory on the Use and Safety of Statins. Stroke. 2002 Sep;33(9):2337–2341. doi: 10.1161/01.str.0000034125.94759.41. [DOI] [PubMed] [Google Scholar]
- 13.Kasaoka S, Todani M, Kaneko T, et al. Peak value of blood myoglobin predicts acute renal failure induced by rhabdomyolysis. J Crit Care. 2010 Dec;25(4):601–604. doi: 10.1016/j.jcrc.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Watanabe T. Rhabdomyolysis and acute renal failure in children. Pediatr Nephrol. 2001 Dec;16(12):1072–1075. doi: 10.1007/s004670100030. [DOI] [PubMed] [Google Scholar]
- 15.Watemberg N, Leshner RL, Armstrong BA, Lerman-Sagie T. Acute pediatric rhabdomyolysis. J Child Neurol. 2000 Apr;15(4):222–227. doi: 10.1177/088307380001500404. [DOI] [PubMed] [Google Scholar]
- 16.Al-Ismaili Z, Piccioni M, Zappitelli M. Rhabdomyolysis: pathogenesis of renal injury and management. Pediatr Nephrol. 2011 Oct;26(10):1781–1788. doi: 10.1007/s00467-010-1727-3. [DOI] [PubMed] [Google Scholar]
- 17.Khan FY. Rhabdomyolysis: a review of the literature. Neth J Med. 2009 Oct;67(9):272–283. [PubMed] [Google Scholar]
- 18.Melli G, Chaudhry V, Cornblath DR. Rhabdomyolysis: an evaluation of 475 hospitalized patients. Medicine (Baltimore) 2005 Nov;84(6):377–385. doi: 10.1097/01.md.0000188565.48918.41. [DOI] [PubMed] [Google Scholar]
- 19.Mannix R, Tan ML, Wright R, Baskin M. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006 Nov;118(5):2119–2125. doi: 10.1542/peds.2006-1352. [DOI] [PubMed] [Google Scholar]
- 20.Jukema JW, Cannon CP, de Craen AJ, Westendorp RG, Trompet S. The controversies of statin therapy: weighing the evidence. J Am Coll Cardiol. 2012 Sep 4;60(10):875–881. doi: 10.1016/j.jacc.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Food and Drug Administration. FDA announces safety changes in labeling for some cholesterol-lowering drugs. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm293623.htm. February 28, 2012. Updated March 2, 2012. Accessed November 21, 2014. [Google Scholar]
- 22.Chatzizisis YS, Koskinas KC, Misirli G, Vaklavas C, Hatzitolios A, Giannoglou GD. Risk factors and drug interactions predisposing to statin-induced myopathy: implications for risk assessment, prevention and treatment. Drug Saf. 2010 Mar 1;33(3):171–187. doi: 10.2165/11319380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Joy TR, Hegele RA. Narrative review: statin-related myopathy. Ann Intern Med. 2009 Jun 16;150(12):858–868. doi: 10.7326/0003-4819-150-12-200906160-00009. [DOI] [PubMed] [Google Scholar]
- 24.Bays H. Statin safety: an overview and assessment of the data––2005. Am J Cardiol. 2006 Apr 17;97((8A)):6C–26C. doi: 10.1016/j.amjcard.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 25.Antons KA, Williams CD, Baker SK, Phillips PS. Clinical perspectives of statin-induced rhabdomyolysis. Am J Med. 2006 May;119(5):400–409. doi: 10.1016/j.amjmed.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Fernandez G, Spatz ES, Jablecki C, Phillips PS. Stain myopathy: a common dilemma not reflected in the clinical trials. Cleve Clin J Med. 2011 Jun;78(6):393–403. doi: 10.3949/ccjm.78a.10073. [DOI] [PubMed] [Google Scholar]
- 27.Guyton JR. Benefit versus risk in statin treatment. Am J Cardiol. 2006 Apr 17;97((8A)):95C–97C. doi: 10.1016/j.amjcard.2005.12.016. [DOI] [PubMed] [Google Scholar]
- 28.Thompson PD, Clarkson P, Karas RH. Statin-associated myopathy. JAMA. 2003 Apr 2;289(13):1681–1690. doi: 10.1001/jama.289.13.1681. [DOI] [PubMed] [Google Scholar]
- 29.Davidson MH, Clark JA, Glass LM, Kanumalla A. Statin safety: an appraisal from the adverse event reporting system. Am J Cardiol. 2006 Apr 17;97((8A)):32C–43C. doi: 10.1016/j.amjcard.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 30.Staffa JA, Chang J, Green L. Cerivastatin and reports of fatal rhabdomyolysis. N Engl J Med. 2002 Feb 14;346(7):539–540. doi: 10.1056/NEJM200202143460721. [DOI] [PubMed] [Google Scholar]
- 31.Kashani A, Phillips CO, Foody JM, et al. Risks associated with statin therapy: a systematic overview of randomized clinical trials. Circulation. 2006 Dec 19;114(25):2788–2797. doi: 10.1161/CIRCULATIONAHA.106.624890. [DOI] [PubMed] [Google Scholar]
- 32.Allison RC, Bedsole DL. The other medical causes of rhabdomyolysis. Am J Med Sci. 2003 Aug;326(2):79–88. doi: 10.1097/00000441-200308000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Tomaszewski M, Stępień KM, Tomaszewska J, Czuczwar SJ. Statin-induced myopathies. Pharmacol Rep. 2011;63(4):859–866. doi: 10.1016/s1734-1140(11)70601-6. [DOI] [PubMed] [Google Scholar]
- 34.Rowan CG, Brunelli SM, Munson J, et al. Clinical importance of the drug interaction between statins and CYP3A4 inhibitors: a retrospective cohort study in the Health Improvement Network. Pharmacoepidemiol Drug Saf. 2012 May;21(5):494–506. doi: 10.1002/pds.3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jacobson TA. Comparative pharmacokinetic interaction profiles of pravastatin, simvastatin, and atorvastatin when coadministered with cytochrome P450 inhibitors. Am J Cardiol. 2004 Nov 1;94(9):1140–1146. doi: 10.1016/j.amjcard.2004.07.080. [DOI] [PubMed] [Google Scholar]
- 36.Law M, Rudnicka AR. Statin safety: a systematic review. Am J Cardiol. 2006 Apr 17;97((8A)):52C–60C. doi: 10.1016/j.amjcard.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 37.Goh IX, How CH, Tavintharan S. Cytochrome P450 drug interactions with statin therapy. Singapore Med J. 2013 Mar;54(3):131–135. doi: 10.11622/smedj.2013044. [DOI] [PubMed] [Google Scholar]
- 38.Jones PH, Davidson MH. Reporting rate of rhabdomyolysis with fenofibrate + statin versus gemfibrozil + any statin. Am J Cardiol. 2005 Jan 1;95(1):120–122. doi: 10.1016/j.amjcard.2004.08.076. [DOI] [PubMed] [Google Scholar]
- 39.Pan WJ, Gustavson LE, Achari R, et al. Lack of clinically significant pharmacokinetic interaction between fenofibrate and pravastatin in healthy volunteers. J Clin Pharmacol. 2000 Mar;40(3):316–323. doi: 10.1177/00912700022008874. [DOI] [PubMed] [Google Scholar]
- 40.Davidson MH. Combination therapy for dyslipidemia: safety and regulatory considerations. Am J Cardiol. 2002 Nov 20;90((10B)):50K–60K. doi: 10.1016/s0002-9149(02)02970-3. [DOI] [PubMed] [Google Scholar]
- 41.Landau ME, Kenney K, Deuster P, Campbell W. Exertional rhabdomyolysis: a clinical review with a focus on genetic influences. J Clin Neuromuscul Dis. 2012 Mar;13(3):122–136. doi: 10.1097/CND.0b013e31822721ca. [DOI] [PubMed] [Google Scholar]
- 42.Schwaber MJ, Liss HP, Steiner I, Brezis M. Hazard of sauna use after strenuous exercise. Ann Intern Med. 1994 Mar 1;120(5):441–442. doi: 10.7326/0003-4819-120-5-199403010-00029. [DOI] [PubMed] [Google Scholar]
- 43.Alpers JP, Jones LK., Jr Natural history of exertional rhabdomyolysis: a population-based analysis. Muscle Nerve. 2010 Oct;42(4):487–491. doi: 10.1002/mus.21740. [DOI] [PubMed] [Google Scholar]
- 44.Warren JD, Blumbergs PC, Thompson PD. Rhabdomyolysis: a review. Muscle Nerve. 2002 Mar;25(3):332–347. doi: 10.1002/mus.10053. [DOI] [PubMed] [Google Scholar]
- 45.Loke J, MacLennan DH. Malignant hyperthermia and central core disease: disorders of Ca2+ release channels. Am J Med. 1998 May;104(5):470–486. doi: 10.1016/s0002-9343(98)00108-9. [DOI] [PubMed] [Google Scholar]
- 46.Bagnulo H, Rodríguez F. Rhabdomyolysis during a case of streptococcal toxic shock syndrome [in Spanish] Enferm Infecc Microbiol Clin. 2001 Feb;19(2):82–83. doi: 10.1016/s0213-005x(01)72569-4. [DOI] [PubMed] [Google Scholar]
- 47.Erdogan H, Yilmaz A, Kal O, Erdogan A, Arslan H. Rhabdomyolysis-induced acute renal failure associated with legionnaires' disease. Scand J Urol Nephrol. 2006;40(4):345–346. doi: 10.1080/00365590600795248. [DOI] [PubMed] [Google Scholar]
- 48.Swaringen JC, Seiler JG, 3rd, Bruce RW., Jr Influenza A induced rhabdomyolysis resulting in extensive compartment syndrome. Clin Orthop Relat Res. 2000 Jun;(375):243–249. doi: 10.1097/00003086-200006000-00029. [DOI] [PubMed] [Google Scholar]
- 49.Paletta CE, Lynch R, Knutsen AP. Rhabdomyolysis and lower extremity compartment syndrome due to influenza B virus. Ann Plast Surg. 1993 Mar;30(3):272–273. doi: 10.1097/00000637-199303000-00013. [DOI] [PubMed] [Google Scholar]
- 50.Peraldi MN, Maslo C, Akposso K, Mougenot B, Rondeau E, Sraer JD. Acute renal failure in the course of HIV infection: a single-institution retrospective study of ninety-two patients and sixty renal biopsies. Nephrol Dial Transplant. 1999 Jun;14(6):1578–1585. doi: 10.1093/ndt/14.6.1578. [DOI] [PubMed] [Google Scholar]
- 51.Wang YM, Zhang Y, Ye ZB. Rhabdomyolysis following recent severe coxsackie virus infection in patient with chronic renal failure: one case report and a review of the literature. Renal Fail. 2006;28(1):89–93. doi: 10.1080/08860220500461310. [DOI] [PubMed] [Google Scholar]
- 52.Osamah H, Finkelstein R, Brook JG. Rhabdomyolysis complicating acute Epstein-Barr virus infection. Infection. 1995 Mar-Apr;23(2):119–120. doi: 10.1007/BF01833879. [DOI] [PubMed] [Google Scholar]
- 53.Wong WM. Wai-Hung Shek T, Chan KH, Chau E, Lai KC. Rhabdomyolysis triggered by cytomegalovirus infection in a heart transplant patient on concomitant cyclosporine and atorvastatin therapy. J Gastroenterol Hepatol. 2004 Aug;19(8):952–953. doi: 10.1111/j.1440-1746.2004.03543.x. [DOI] [PubMed] [Google Scholar]
- 54.Shanmugam S, Seetharaman M. Viral rhabdomyolysis. South Med J. 2008 Dec;101(12):1271–1272. doi: 10.1097/SMJ.0b013e318183649a. [DOI] [PubMed] [Google Scholar]
- 55.Will MJ, Hecker RB, Wathen PI. Primary varicella-zoster-induced rhabdomyolysis. South Med J. 1996 Sep;89(9):915–920. doi: 10.1097/00007611-199609000-00015. [DOI] [PubMed] [Google Scholar]
- 56.Gupta M, Ghaffari M, Freire AX. Rhabdomyolysis in a patient with West Nile encephalitis and flaccid paralysis. Tenn Med. 2008 Apr;101(4):45–47. Erratum in: Tenn Med. 2008 Jun;101(6):61. [PubMed] [Google Scholar]
- 57.Gabow PA, Kaehny WD, Kelleher SP. The spectrum of rhabdomyolysis. Medicine (Baltimore) 1982 May;61(3):141–152. doi: 10.1097/00005792-198205000-00002. [DOI] [PubMed] [Google Scholar]
- 58.Better OS, Abassi ZA. Early fluid resuscitation in patients with rhabdomyolysis. Nat Rev Nephrol. 2011 May 17;7(7):416–422. doi: 10.1038/nrneph.2011.56. [DOI] [PubMed] [Google Scholar]
- 59.Elsayed EF, Reilly RF. Rhabdomyolysis: a review, with emphasis on the pediatric population. Pediatr Nephrol. 2010 Jan;25(1):7–18. doi: 10.1007/s00467-009-1223-9. [DOI] [PubMed] [Google Scholar]
- 60.Cereda M, Horak J, Neligan PJ. Renal diseases. In: Fleisher LA, editor. Anesthesia and Uncommon Diseases. 5th ed. Philadelphia, PA: Saunders Elsevier;; 2006. pp. 229–260. [Google Scholar]
- 61.Muenster T, Mueller C, Forst J, Huber H, Schmitt HJ. Anaesthetic management in patients with Duchenne muscular dystrophy undergoing orthopaedic surgery: a review of 232 cases. Eur J Anaesthesiol. 2012 Oct;29(10):489–494. doi: 10.1097/EJA.0b013e3283566789. [DOI] [PubMed] [Google Scholar]
- 62.Segura LG, Lorenz JD, Weingarten TN, et al. Anesthesia and Duchenne or Becker muscular dystrophy: review of 117 anesthetic exposures. Paediatr Anaesth. 2013 Sep;23(9):855–864. doi: 10.1111/pan.12248. [DOI] [PubMed] [Google Scholar]
- 63.Coco TJ, Klasner AE. Drug-induced rhabdomyolysis. Curr Opin Pediatr. 2004 Apr;16(2):206–210. doi: 10.1097/00008480-200404000-00017. [DOI] [PubMed] [Google Scholar]
- 64.Weiner AL, Vieira L, McKay CA, Bayer MJ. Ketamine abusers presenting to the emergency department: a case series. J Emerg Med. 2000 May;18(4):447–451. doi: 10.1016/s0736-4679(00)00162-1. [DOI] [PubMed] [Google Scholar]
- 65.Gurnaney H, Brown A, Litman RS. Malignant hyperthermia and muscular dystrophies. Anesth Analg. 2009 Oct;109(4):1043–1048. doi: 10.1213/ane.0b013e3181aa5cf6. [DOI] [PubMed] [Google Scholar]
- 66.Friedman S, Baker T, Gatti M, Simon G, Paskin S. Probable succinylcholine-induced rhabdomyolysis in a male athlete. Anesth Analg. 1995 Aug;81(2):422–423. doi: 10.1097/00000539-199508000-00040. [DOI] [PubMed] [Google Scholar]
- 67.Ryan JF, Kagen LJ, Hyman AI. Myoglobinemia after a single dose of succinylcholine. N Engl J Med. 1971 Oct 7;285(15):824–827. doi: 10.1056/NEJM197110072851503. [DOI] [PubMed] [Google Scholar]
- 68.Wong JM. Propofol infusion syndrome. Am J Ther. 2010 Sep-Oct;17(5):487–491. doi: 10.1097/MJT.0b013e3181ed837a. [DOI] [PubMed] [Google Scholar]
- 69.Stelow EB, Johari VP, Smith SA, Crosson JT, Apple FS. Propofol-associated rhabdomyolysis with cardiac involvement in adults: chemical and anatomic findings. Clin Chem. 2000 Apr;46(4):577–581. [PubMed] [Google Scholar]
- 70.Mehta N, DeMunter C, Habibi P, Nadel S, Britto J. Short-term propofol infusions in children. Lancet. 1999 Sep 4;354(9181):866–867. doi: 10.1016/S0140-6736(05)75936-5. [DOI] [PubMed] [Google Scholar]
- 71.Burrow BK, Johnson ME, Packer DL. Metabolic acidosis associated with propofol in the absence of other causative factors. Anesthesiology. 2004 Jul;101(1):239–241. doi: 10.1097/00000542-200407000-00035. [DOI] [PubMed] [Google Scholar]
- 72.Roberts RJ, Barletta JF, Fong JJ, et al. Incidence of propofol-related infusion syndrome in critically ill adults: a prospective, multicenter study. Crit Care. 2009;13(5):R169. doi: 10.1186/cc8145. [DOI] [PMC free article] [PubMed] [Google Scholar]