Abstract
Contact with the criminal justice system, including incarceration, is a common experience for many people living with HIV/AIDS. Optimism has recently been expressed that correctional facilities could be important locations for Treatment-as-Prevention (TasP)-based initiatives. We review recent findings regarding the effect of incarceration on patterns of HIV transmission, testing, treatment initiation and retention. We found that the prevalence of HIV infection among incarcerated individuals remains higher than analogous non-incarcerated populations. Recent studies have shown that voluntary HIV/AIDS testing is feasible in many correctional facilities, although the number of previously undiagnosed individuals identified has been modest. Studies have implied enhanced linkage to HIV/AIDS treatment and care in jails in the United States was associated with improvements in the HIV cascade of care. However, for many individuals living with HIV/AIDS, exposure to the correctional system remains an important barrier to retention in HIV/AIDS treatment and care. Future research should evaluate structural interventions to address these barriers and facilitate the scale-up of TasP-based efforts among individuals living in correctional settings.
Keywords: HIV, AIDS, antiretroviral therapy, incarceration
INTRODUCTION
Since its first detection three decades ago, the HIV/AIDS pandemic has been profoundly shaped by criminal justice systems. Surveillance studies have commonly observed significantly higher prevalences of HIV infection among incarcerated populations as compared to analogous non-incarcerated groups [1–3]. The elevated seroprevalences among individuals held in correctional facilities are, for the most part, a result of the political and criminal justice structures that penalize groups who already face multiple HIV/AIDS-related vulnerabilities, including individuals addicted to illicit drugs, sex workers, and sexual/gender minorities [4]. However, evidence from a variety of studies, including molecular contact-tracing investigations and entry/exit antibody testing, have also identified within-prison transmission, facilitated by the dearth of evidence-based HIV prevention tools [5–7]. In addition, exposure to correctional facilities has been strongly associated with elevated levels of co-morbidities (i.e., hepatitis C, tuberculosis, untreated mental illness including unmanaged substance use disorders) and social/structural factors (stigma, discrimination, political disempowerment, socio-economic marginalization and exclusion from non-correctional healthcare systems) linked to increased risk of HIV transmission and pathogenesis [8–10].
Coincident with the emergence and spread of the HIV/AIDS pandemic has been the growth in the global population of individuals held in penal facilities [9,11,12]. According to the most recent estimates, approximately 10.1 million people were held in penal institutions, including police cells, pre-trial detention, so-called mandatory treatment facilities, jails, prisons and penitentiaries in 2011, equal to a rate of incarceration of 146 per 100,000 individuals [11]. Driven in many settings by increased numbers of criminalized drug users, global correctional populations have nearly doubled since 2005 [9,11]. While unequalled in size or scope, the United States’ correctional systems exemplify these trends [12]. In the 1980s, the United States enacted harshly punitive laws against illicit drug users, including mandatory minimum sentencing requirements, as a reaction to the emergence of crack cocaine, especially among the country’s urban African-American population. As a result, the number of individuals incarcerated in state and federal prisons increased by almost 500% in a generation [12,13]. More likely than the general population to be non-white [14], poor [12], not engaged in regular medical care [15], and suffering from untreated substance abuse [16], prisoners in the United States exhibit an HIV prevalence of 1.5% [17], and approximately 15% of all people living with HIV/AIDS are in contact with the criminal justice system each year [18].
Recent advances in our understanding of HIV/AIDS transmission dynamics, in particular the central role played by HIV-1 RNA viral loads (VL), have revealed the substantial impact of effective HIV treatment on the incidence of new infections [19,20]. In the wake of the HPTN-052 multicenter randomized controlled trial that demonstrated a >95% decrease in the likelihood of HIV transmission as a result of earlier highly-active antiretroviral treatment (HAART) [19], as well as other evidence from observational studies and mathematical models [21], renewed HIV/AIDS prevention campaigns with HIV treatment as a cornerstone have been launched. These seek to reduce the incidence of new infections by lowering the community-level HIV RNA viral load. Some key aspects of Treatment-as-Prevention (TasP) efforts are identifying undiagnosed individuals and engaging and retaining them in medical care including HAART, with the goal of achieving non-detectable plasma HIV-1 RNA viral loads (VL) [20,22].
Given the high proportion of individuals living with HIV/AIDS held in correctional facilities, optimism has been expressed that criminal justice systems could be an ideal focus of HIV testing and treatment efforts [23]. However, studies of people living with HIV/AIDS in community settings have consistently observed that incarceration is a substantial barrier to consistent engagement in HIV treatment and care, including antiretroviral therapy [24–26]. Thus, the criminal justice-based approach to individuals at high risk for HIV infection, especially people who use illicit drugs (PWID) and sex workers, and the high rates of incarceration borne by these groups, might compromise the impact of TasP-based campaigns [27]. In order to contribute to efforts to optimize TasP-efforts as well as reduce HIV/AIDS morbidity and mortality among incarcerated individuals, we performed this review of incarceration among people living with HIV/AIDS, focusing on HIV prevalence and transmission, HIV testing, and HIV treatment among incarcerated populations.
HIV PREVALENCE/RISK
As a result of the ethical and logistical challenges often faced by researchers working with incarcerated populations, the majority of scientific investigations into HIV/AIDS-related transmission and pathogenesis risks among prisoners have been cross-sectional serosurveys of infection with HIV or related conditions, including tuberculosis (TB), often anonymized and rarely longitudinal (i.e., before, during and after incarceration) or linked to external data sources. These surveys (for example, in the United States [28], Brazil [29] and Scotland [7]) have consistently identified elevated prevalence of infection compared to non-incarcerated populations. Meanwhile, observational studies conducted in non-correctional settings among groups at higher risk of infection with HIV, including injection drug users, sex workers, and members of sexual/gender minorities, have commonly associated incarceration with elevated risk of HIV infection in both crude and adjusted analyses [30,31].
Recent analyses of the prevalence of HIV and related infections in correctional populations have confirmed this pattern [32–36]. Of particular note are the results from an HIV/TB screening program established in six prisons in Zambia [34]. Among 2323 individuals entering, residing in or exiting the facility during the study period, 27.4% were living with HIV/AIDS, approximately twice the national level, and the prevalence of bacteriologically-confirmed TB, at 3900 per 100,000, was 4.5 times the national average [34]. The first published survey of HIV and TB in an African prison, the results suggest important linkages between HIV and TB infection in the prison and, through prison workers, prisoners and ex-prisoners, the local community [34]. Similarly, a representative nationwide survey of 402 soon-to-be-released prisoners in Ukraine found high seroprevalences of both infectious disease, including HIV (19%) and untreated substance use disorders, with over half screened positive for alcohol use disorders and over one-third reporting use of opioids in the 30 days prior to arrest [33]. Notably, more than half of the HIV-positive prisoners were unaware of their serostatus [33] and only five individuals (6.4%) were receiving ART. If TasP efforts are to have a beneficial impact on HIV incidence, the authors suggest, the under-diagnosis and under-treatment of people living with HIV/AIDS in prison systems must be addressed [33]. The studies from Ukraine and Zambia underline the important burden of co-infections described in many recent studies from prison settings, including high seroprevalences of hepatitis B and C [32,33,35–38] and TB [33,34,38–42].
Many studies among injection drug users in varied settings, including Canada [43], Thailand [44] and the United States [45] have identified a heightened risk of HIV infection associated with incarceration, possibly a result of higher rates of used syringe sharing within correctional facilities. A number of recent studies explored the effect of incarceration on sexual risk among African-Americans [46–48], who have not only borne among the heaviest burden of the HIV/AIDS epidemic in the United States, but make up approximately 40% of those currently incarcerated in the United States [49]. Among 1553 black men who have sex with men in six US cities, 60% reported a lifetime history of incarceration [48]. Although some have hypothesized the incarceration contributes to the high levels of HIV infection among African-Americans [50], and incarceration was common over the course of the study [47], there was no association between incarceration during follow-up and incident HIV infection [47]. In two separate studies, incarceration, in combination with marginal housing conditions, was associated with sexual risk behaviours among African-Americans [46] and in a multi-racial sample of young gay men in New York City [51].
HIV TESTING
Voluntary counseling and testing (VCT) for HIV infection has long been recognized as an important component of HIV prevention and treatment programmes [52]. In TasP efforts, which seek in part to lower community-level HIV viral loads through engagement in antiretroviral therapy, high levels of testing are prioritized in order to seek out undiagnosed individuals and link them to care [53]. Mathematical models have suggested that universal voluntary HIV testing followed by immediate ART initiation regardless of CD4+ cell count could lead to sharp declines in HIV incidence [54]. Since large proportions of HIV-positive individuals are unaware of their status, even in developed settings with advanced HIV/AIDS treatment and care systems where HIV tests are mandated to be a regular part of medical care [55,56], there is a clear need to increase testing rates, especially among populations with a high prevalence of HIV infection, such as incarcerated individuals. [17].
Due to the special conditions imposed by incarceration, in particular that they are coercive environments that constrain the freedom and privacy of individuals, there have long been concerns around the legal and ethical implications of HIV testing within penal settings [9,57,58]. As respect for patient autonomy, confidentiality and voluntary consent are fundamental aspects of healthcare and human rights, many national and international organizations oppose mandatory or compulsory testing of individuals in correctional settings, including the World Health Organization and UNAIDS [57,59]. In many correctional systems, early policies of compulsory HIV testing among all prisoners have been abandoned following legal challenges, the cost of providing HIV/AIDS care, and the finding that they were ineffective [59]. However, mandatory or compulsory testing continues in many state prison systems in the United States, Russia and some countries in Asia and the Pacific [59,60].
In their 2006 guidance document on HIV testing in prisons and other closed settings, the World Health Organization, UNAIDS and the United Nations Office on Drugs and Crime recommend that all prisoners have access to voluntary and confidential HIV testing, including pre- and post-test counseling [61]. In the United States, despite the wide variety of correctional settings and laws governing their operation [60], the United States Centers for Disease Control and Prevention recommends universal voluntary opt-out HIV testing for all adults in health-care settings, including correctional systems, unless prevalence of undiagnosed infection has been documented to be less than 0.1% [52]. Unfortunately, data on HIV testing within correctional systems globally is unavailable, and the distribution of different testing regimes — including mandatory, opt-in, opt-out, testing on demand, and none at all — is not known [59]. Further, only limited data exists on the actual practice of HIV testing within correctional settings, almost all from federal, state and local prison systems in the United States [61].
New findings from a multi-centre observational study conducted in jails in the United States offered some evidence of the possible results of jail-based voluntary testing and linkage to care initiatives [62]. Based on the recognition that 9 million individuals are admitted to a jail each year in the United States, the EnhanceLink initiative collected client and program-level data on patterns of HIV testing and linkage to care at 20 jails in 10 communities [62]. For HIV testing, the initiative’s objective was to demonstrate its feasibility within jail settings and identify new and previously-detected infections [62]. From 2007 to 2011, more than 877,000 admissions to the twenty institutions resulted in 212,464 (24.2%) individuals accepting an HIV test. In total, 822 (0.09% of all admissions, or 0.4% of all completed tests) newly-diagnosed individuals were detected [62]. In a study of a subset of these HIV-positive individuals, newly-diagnosed individuals were younger (34 years versus 41 years), exhibited far higher levels of HIV risk behaviours and were much less likely to report possessing healthcare benefits than previously-diagnosed individuals [63]. Newly-diagnosed individuals had a median CD4+ cell count of 432 cell/mL and less than one-quarter initiated ART prior to release from custody [63].
These findings add to evidence that jail-based opt-in or opt-out screening can identify previously-undiagnosed individuals, often earlier in their disease course [64,65]. For example, an evaluation of a programme of rapid HIV testing in three urban jails in settings with high HIV prevalence (Baltimore, Maryland; Philadelphia, PA; and the District of Columbia), reported that of more than 129,000 admissions over the study period, 41,612 (32%) completed voluntary rapid testing, resulting in 142 newly-identified infections (0.11% of all admissions, or 0.34% of all tests) [64]. These results come as a survey of prison and jails in the United States found that only a small proportion follow HIV testing and linkage guidelines [66]. Most notably, a study using blood sera collected during a compulsory screening programme for syphilis infection at intake into the state prison system in North Carolina found that the HIV prevalence among incarcerated individuals was approximately 1.45%. However, only 20 of 22,134 tests, or 0.09%, were HIV positive and previously undiagnosed, although the authors reported they did not have access to each individual’s entire testing history [67]. Thus, although voluntary HIV testing may be feasible even in busy correctional environments with high rates of inmate turnover, and detection of HIV among previously undiagnosed individuals is of obvious medical benefit to them, this evidence suggests expansion of jail- and prison-based HIV testing might not substantially reduce the number of individuals unaware of being HIV-positive [67].
IN-PRISON HIV TREATMENT AND LINKAGE TO POST-RELEASE CASE
In theory, correctional environments offer many advantages for the delivery of ART to HIV-positive individuals, including very low loss to follow-up, assured dosing schedules, and lower levels of availability of substances of misuse. Thus, controlled trials of directly-observed therapy among prisoners have demonstrated very high levels of optimal treatment outcomes [68,69]. Most notably, a recent retrospective cohort study of 882 HIV-infected and ART-initiated individuals incarcerated in the Connecticut correctional system found that while approximately 30% entered custody with plasma VL levels < 400 copies/mL, at exit, 70% of individuals were virally suppressed [70]. Although studies on HIV treatment patterns among incarcerated individuals in low-income settings are rare, a recent analysis of 148 individuals incarcerated in South Africa reported that almost three-quarters had plasma VL < 400 copies/mL after 96 weeks on ART [71].
Unfortunately, the clinical benefits of in-prison treatment for many are lost as individuals discontinue treatment upon release from custody. Most notably, only 5% of released prisoners filled a prescription for ART in the first 10 days following release from custody, thus avoiding treatment interruption, in one study from the prison system in Texas [72]. Observational studies of individuals transitioning from secure custody to community settings have identified a variety of barriers to retaining engagement in HIV/AIDS care, including poor or non-existent pre-release planning [66]; systematic removal of healthcare benefits from incarcerated individuals [73]; high-intensity drug and alcohol use in the immediate post-release period [74]; and poor housing status [75]. These barriers, along with sub-optimal HIV/AIDS treatment capacity in some correctional settings and a desire by some prisoners to conceal their serostatus, likely account for much of the observed association between incarceration and discontinuation or non-adherence to prescribed ART [76–78] and plasma VL rebound [24,79].
Recent studies among community-recruited groups of individuals engaged in HIV/AIDS treatment and care with substantial rates of incarceration confirm these dynamics. Studies among women living with HIV as well as illicit drug users identified associations between exposure to correctional settings and sub-optimal HIV/AIDS outcomes, including shorter time to AIDS [80], loss of virologic control [81] and dropping out of HIV care [82]. Although these studies were from settings in the United States, a similar dynamic was observed in a notable study from Ukraine [83]. Among 97 newly-released HIV-positive individuals, short-term detention by police was common and contributed directly to inability to access ART and prescribed opioid substitution therapy [83].
This study is one of a number to highlight the important role played by evidence-based treatment for substance use disorders for HIV-positive individuals engaged in the criminal justice system [84,85]. In one of the first studies on HIV-infected opioid-dependent individuals in Asia transitioning from correctional settings, optimal dosing with methadone (>80mg/day) was strongly associated with greater retention in treatment at 12 months [85]. Similarly, retention on treatment with buprenorphine/naloxone treatment was associated with maximal viral suppression among 94 opioid-dependent individuals released from custody in New England, United States [84]. An controlled trial of extended-release naltrexone for alcohol-dependent HIV-positive individuals released from custody currently underway may also provide evidence tom improve HIV treatment outcomes post-release [86].
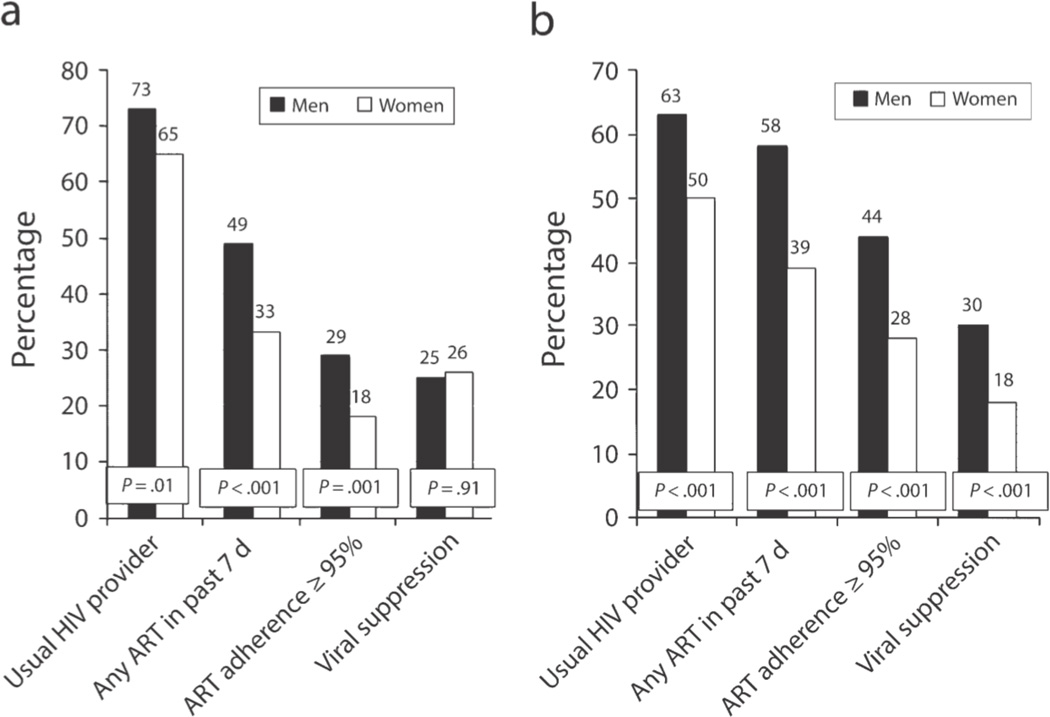
As with HIV testing, the EnhanceLink study delivered some important insights into the factors associated with linking incarcerated individuals to care [75,87–96]. Conducted in 20 penal institutions in 10 cities in the United States between 2008 and 2011, the study enrolled 867 incarcerated individuals and followed them longitudinally in the first six months after release from custody. Activities associated with enhanced HIV linkage included case management programs, counseling, education and social support [87]. Of the 867 individuals, 34% were lost to care. Successful linkage to HIV/AIDS care within the first 30 days was associated with HIV/medication education and stable housing [75]. Services associated with staying in sustained care over six months were in-prison discharge planning and disease management sessions (both p < 0.05); and, after release, HIV education, a needs assessment, and transportation [88]. Although engagement in the HIV cascade of care improved for individuals at six months post-release (Figure 1), women were less likely to experience these benefits [87]. For example, while women and men did not differ in levels of viral suppression at baseline (26 vs. 25%; p = 0.91), women were significantly less likely to exhibit viral suppression after six months (18 vs. 30%, p < 0.001). Among all individuals, 26% had plasma VL < 400 copies/mL at six months, associated with attending a meeting with an HIV care provider within 30 days of release, after adjustment for achieving viral suppression in jail [97].
Figure 1.
Prevalences of various measures of engagement in HIV/AIDS treatment and care among individuals enrolled in the EnhanceLink study, stratified by gender, during incarceration (a) and six-months after release from incarceration (b), as reported by Meyer et al., [87]
The ultimate step on the HIV cascade of care is achieving non-detectable plasma VL through effective engagement in HIV treatment and care [98]. Unfortunately, few studies have investigated important virologic outcomes among criminal justice-involved populations, including community-level plasma VL, molecular cluster analysis or viral resistance to antiretrovirals. One study from Vancouver, Canada, using data from a long-running cohort of HIV-positive illicit drug users recruited from community settings found that incarceration was associated with detectable VL and, during periods of detectable VL, incarceration was also associated with sharing contaminated syringes [99], pointing to the need for effective ART among incarcerated individuals. In a notable study from Brazil, a survey of 1167 incarcerated individuals found that 110 (6.6%) were HIV-positive. A molecular phylogeny inferred from the analysis of viral RNA sequences from 40 individuals did not find any evidence of between-prisoner transmission; however, analysis of sequences from the pol gene evidenced high rates of HIV primary and secondary resistance [100]. In contrast, a survey of 367 viral sequences from individuals incarcerated in the state prison system of North Carolina found moderate levels of drug resistance, comparable to non-incarcerated populations [101].
CONCLUSION
In this review, we summarized the recent evidence regarding the effect of incarceration and correctional systems on patterns of HIV testing and treatment. Studies from a variety of settings confirmed that HIV prevalence remains higher among incarcerated populations as compared to analogous non-incarcerated groups [33–36,39] and often co-occurs with other infectious diseases, especially viral hepatitis and tuberculosis [32,34–36,39]. Recent evidence from the United States indicates that voluntary HIV rapid testing within jail and prison settings is feasible and effective [62,63]. However, the number of undiagnosed individuals identified in some surveys was low, indicating that voluntary testing in correctional populations might not yield enough new cases to have a substantial impact on the HIV cascade of care in the United States [64,67]. A large observational study of testing and linkage to care in 10 cities in the United States demonstrated improved HIV treatment outcomes at six-months post release [87]. Evidence on viral resistance to antiretrovirals among incarcerated populations was mixed [100,101], however incarceration was associated with elevated VL and associated risk factors among illicit drug users in Vancouver, Canada [99].
As many countries look to scale-up TasP campaigns to engage HIV-positive individuals in care, lower community-level plasma VL and curb the incidence of new infections, correctional populations are attractive targets. Unfortunately, there remain unanswered questions about whether the entrenched barriers to HIV/AIDS treatment and care in penal settings will compromise TasP campaigns, especially among people who use illicit drugs, sex workers, members of sexual/gender minorities and those criminalized for HIV non-disclosure [27]. Fortunately, there is emerging evidence that individuals from these traditionally hard-to-reach groups can be successfully engaged in HIV/AIDS treatment and care through TasP-based campaigns in community settings [102,103]. Although observational studies of recent programmatic interventions among prisoners have identified modest gains in HIV/AIDS testing and linkage to care, future research should evaluate the effect of structural changes to correctional systems. These reforms might include transferring responsibility for in-prison HIV/AIDS treatment to public health authorities and diverting people living with HIV/AIDS from custodial settings [9].
Four decades into the HIV/AIDS pandemic, all available evidence continues to describe persistent deficits and iniquities in HIV/AIDS prevention and treatment among incarcerated individuals. Through incarceration, many individuals with elevated risks of HIV disease progression continue to be exposed to environments with sub-optimal HIV/AIDS treatment and care. In light of the fundamental right of incarcerated individuals living with HIV/AIDS to receive healthcare equivalent to that delivered in analogous non-penal settings [104], the increased global adoption of universal access to ART underscores the urgent need to guarantee the benefits of HIV/AIDS treatment for all people, including those living in custody.
ACKNOWLEDGEMENTS
We thank Deborah Graham, Carmen Rock and Kristie Starr for their administrative assistance. This work was supported by the National Institutes of Health (R01 DA021525.) Dr. Milloy is supported by fellowships from the Canadian Institutes of Health Research and the Michael Smith Foundation for Health Research. This work was supported in part by a Tier 1 Canada Research Chair in Inner-City Medicine awarded to Dr. Wood.
Dr. Montaner has received grants from Abbott, Biolytical, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead Sciences, Janssen, Merck and ViiV Healthcare. He is also is supported: by the Ministry of Health Services and the Ministry of Healthy Living and Sport, from the Province of British Columbia; through a Knowledge Translation Award from the Canadian Institutes of Health Research (CIHR); and through an Avant-Garde Award (No. 1DP1DA026182) from the National Institute of Drug Abuse, at the US National Institutes of Health. He has also received support from the International AIDS Society, United Nations AIDS Program, World Health Organization, National Institute on Drug Abuse, National Institutes of Health Research-Office of AIDS Research, National Institute of Allergy & Infectious Diseases, the United States President’s Emergency Plan for AIDS Relief (PEPfAR), Bill & Melinda Gates Foundation, French National Agency for Research on AIDS & Viral Hepatitis (ANRS), Public Health Agency of Canada.
Footnotes
COMPLIANCE WITH ETHICS GUIDELINES
HUMAN AND ANIMAL RIGHTS AND INFORMED CONSENT
This article does not contain primary reporting of any studies by the authors involving human or animal subjects.
Drs. Wood and Milloy declare that they have no conflicts of interest.
REFERENCES
- 1.Macalino GE, Vlahov D, Sanford-Colby S, Patel S, Sabin K, Salas C, et al. Prevalence and incidence of HIV, hepatitis B virus, and hepatitis C virus infections among males in Rhode Island prisons. Am J Public Health. 2004;94:1218–1223. doi: 10.2105/ajph.94.7.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rotily M, Weilandt C, Bird SM, Käll K, Van Haastrecht HJ, Iandolo E, et al. Surveillance of HIV infection and related risk behaviour in European prisons. A multicentre pilot study. Eur J Public Health. 2001;11:243–250. doi: 10.1093/eurpub/11.3.243. [DOI] [PubMed] [Google Scholar]
- 3.Allwright S. Prevalence of antibodies to hepatitis B, hepatitis C, and HIV and risk factors in Irish prisoners: results of a national cross sectional survey. BMJ. 2000;321:78–82. doi: 10.1136/bmj.321.7253.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Amiya RM, Cope JE, Poudel KC, Jimba M. At the intersection of public health and criminal justice systems. Lancet. England; 2013;381:534. doi: 10.1016/S0140-6736(13)60276-7. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention (CDC) HIV transmission among male inmates in a state prison system--Georgia, 1992–2005. MMWR Morb. Mortal. Wkly. Rep. 2006;55:421–426. [PubMed] [Google Scholar]
- 6.Dolan KA, Wodak A. HIV transmission in a prison system in an Australian State. Med. J. Aust. 1999;171:14–17. doi: 10.5694/j.1326-5377.1999.tb123490.x. [DOI] [PubMed] [Google Scholar]
- 7.Taylor A, Goldberg D, Emslie J, Wrench J, Gruer L, Cameron S, et al. Outbreak of HIV infection in a Scottish prison. BMJ. 1995;310:289–292. doi: 10.1136/bmj.310.6975.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zack B. Correctional health and the HIV stages of care. Journal of Correctional Health Care. United States; 2013;19:229–230. doi: 10.1177/1078345813486444. [DOI] [PubMed] [Google Scholar]
- 9. Jürgens R, Nowak M, Day M. HIV and incarceration: prisons and detention. Journal of the International AIDS Society. BioMed Central Ltd; 2011;14:26. doi: 10.1186/1758-2652-14-26. • The most comprehensive review of the epidemiological, clinical and policy implications of incarceration among individuals living with/at risk of HIV.
- 10.Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. The Lancet. Elsevier Ltd; 2010;376:367–387. doi: 10.1016/S0140-6736(10)60829-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walmsley R. World Prison Population List. ninth edition. Essex, England: International Centre for Prison Studies; 2013. pp. 1–6. [Google Scholar]
- 12.Incarceration and Crime: A Complex Relationship. Washington, DC, USA: The Sentencing Project; 2005. pp. 1–11. [Google Scholar]
- 13.Blumstein A, Beck AJ. Population growth in US prisons, 1980–1996. Crime. & Just. HeinOnline. 1999;26:17. [Google Scholar]
- 14.West H, Sabol WJ, Greenman S. Prisoners in 2009. Washington, DC, USA: United States Department of Justice; 2011. pp. 1–38. [Google Scholar]
- 15. Rich JD, Diclemente R, Levy J, Lyda K, Ruiz MS, Rosen DL, et al. Correctional facilities as partners in reducing HIV disparities. J. Acquir. Immune Defic. Syndr. 2013;63(Suppl 1):S49–S53. doi: 10.1097/QAI.0b013e318292fe4c. • An important call from leading US-based researchers into correctional health to engage correctional facilities in addressing HIV/AIDS-associated disparities
- 16.Chandler RK, Fletcher BW, Volkow ND. Treating drug abuse and addiction in the criminal justice system: improving public health and safety. JAMA: The Journal of the American Medical Association. 2009;301:183–190. doi: 10.1001/jama.2008.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Westergaard RP, Spaulding AC, Flanigan TP. HIV among persons incarcerated in the USA: a review of evolving concepts in testing, treatment, and linkage to community care. Current Opinion in Infectious Diseases. 2013;26:10–16. doi: 10.1097/QCO.0b013e32835c1dd0. • A review of seek, test, treat and retain campaigns among incarcerated individuals in the United States
- 18.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among Inmates of and Releasees from US Correctional Facilities, 2006: Declining Share of Epidemic but Persistent Public Health Opportunity. PLoS ONE. 2009;4:A16–A21. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 Infection with Early Antiretroviral Therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montaner JSG, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet. 2010;376:532–539. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Granich R, Kahn JG, Bennett R, Holmes CB, Garg N, Serenata C, et al. Expanding ART for treatment and prevention of HIV in South Africa: estimated cost and cost-effectiveness 2011–2050. PLoS ONE. 2012;7:e30216. doi: 10.1371/journal.pone.0030216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montaner JSG, Hogg R, Wood E, Kerr T, Tyndall M, Levy AR, et al. The case for expanding access to highly active antiretroviral therapy to curb the growth of the HIV epidemic. Lancet. 2006;368:531–536. doi: 10.1016/S0140-6736(06)69162-9. [DOI] [PubMed] [Google Scholar]
- 23.Draine J, Ahuja D, Altice FL, Arriola KJ, Avery AK, Beckwith CG, et al. Strategies to enhance linkages between care for HIV/AIDS in jail and community settings. Aids Care-Psychol. Socio-Med. Asp. Aids-Hiv. 2011;23:366–377. doi: 10.1080/09540121.2010.507738. [DOI] [PubMed] [Google Scholar]
- 24.Westergaard RP, Kirk GD, Richesson DR, Galai N, Mehta SH. Incarceration Predicts Virologic Failure for HIV-Infected Injection Drug Users Receiving Antiretroviral Therapy. Clinical Infectious Diseases. 2011;53:725–731. doi: 10.1093/cid/cir491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Milloy M-J, Kerr T, Bangsberg DR, Buxton J, Parashar S, Guillemi S, et al. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS Patient Care STDS. 2012;26:60–67. doi: 10.1089/apc.2011.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clatts MC, Rodriguez-Diaz CE, Garcia H, Vargas-Molina RL, Jovet-Toledo GG, Goldsamt LA. Preliminary Evidence of Significant Gaps in Continuity of HIV Care among Excarcerated Populations in Puerto Rico. Journal of the International Association of Physicians in AIDS Care (JIAPAC) 2011;10:339–341. doi: 10.1177/1545109711418833. [DOI] [PubMed] [Google Scholar]
- 27.Milloy MJ, Montaner J, Wood E. Barriers to HIV treatment among people who use injection drugs: implications for 'treatment as prevention'. Current Opinion in HIV and AIDS. 2012;7:332–338. doi: 10.1097/COH.0b013e328354bcc8. [DOI] [PubMed] [Google Scholar]
- 28.Rich JD, Dickinson BP, Macalino G, Flanigan TP, Towe CW, Spaulding A, et al. Prevalence and incidence of HIV among incarcerated and reincarcerated women in Rhode Island. JAIDS Journal of Acquired Immune Deficiency Syndromes. 1999;22:161–166. doi: 10.1097/00126334-199910010-00008. [DOI] [PubMed] [Google Scholar]
- 29.Burattini M, Massad E, Rozman M, Azevedo R, Carvalho H. Correlation between HIV and HCV in Brazilian prisoners: evidence for parenteral transmission inside prison. Rev Saude Publica. 2000;34:431–436. doi: 10.1590/s0034-89102000000500001. [DOI] [PubMed] [Google Scholar]
- 30.Tyndall MW, Currie S, Spittal P, Li K, Wood E, O'shaughnessy MV, et al. Intensive injection cocaine use as the primary risk factor in the Vancouver HIV-1 epidemic. AIDS. 2003;17:887–893. doi: 10.1097/00002030-200304110-00014. [DOI] [PubMed] [Google Scholar]
- 31.Choopanya K, Jarlais Des DC, Vanichseni S, Kitayaporn D, Mock PA, Raktham S, et al. Incarceration and risk for HIV infection among injection drug users in Bangkok. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2002;29:86–94. doi: 10.1097/00126334-200201010-00012. [DOI] [PubMed] [Google Scholar]
- 32.Reekie JM, Levy MH, Richards AH, Wake CJ, Siddall DA, Beasley HM, et al. Trends in HIV, hepatitis B and hepatitis C prevalence among Australian prisoners - 2004, 2007, 2010. Med. J. Aust. 2014;200:277–280. doi: 10.5694/mja13.11062. [DOI] [PubMed] [Google Scholar]
- 33. Azbel L, Wickersham JA, Grishaev Y, Dvoryak S, Altice FL. Burden of infectious diseases, substance use disorders, and mental illness among Ukrainian prisoners transitioning to the community. PLoS ONE. 2013;8:e59643. doi: 10.1371/journal.pone.0059643. • The authors present the results from a representative survey of HIV and related matters among recently-released Ukranian prisoners
- 34. Henostroza G, Topp SM, Hatwiinda S, Maggard KR, Phiri W, Harris JB, et al. The high burden of tuberculosis (TB) and human immunodeficiency virus (HIV) in a large Zambian prison: a public health alert. PLoS ONE. 2013;8:e67338. doi: 10.1371/journal.pone.0067338. •• In the first published survey of its kind, the authors present the results of a screening programme for HIV and TB in a large Zambian prison, establishing that correctional-associated HIV transmission and pathogenesis should be an urgent priority in efforts to address the pandemic in Sub-Saharan Africa
- 35.Mohamed HI, Saad ZM, Abd-Elreheem EM, Abd-ElGhany WM, Mohamed MS, Abd Elnaeem EA, et al. Hepatitis C, hepatitis B and HIV infection among Egyptian prisoners: seroprevalence, risk factors and related chronic liver diseases. J Infect Public Health. 2013;6:186–195. doi: 10.1016/j.jiph.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 36.Semaille C, Le Strat Y, Chiron E, Chemlal K, Valantin MA, Serre P, et al. Prevalence of human immunodeficiency virus and hepatitis C virus among French prison inmates in 2010: a challenge for public health policy. Euro Surveill. 2013;18 doi: 10.2807/1560-7917.es2013.18.28.20524. [DOI] [PubMed] [Google Scholar]
- 37.Honarvar B, Odoomi N, Moghadami M, Afsar Kazerooni P, Hassanabadi A, Zare Dolatabadi P, et al. Blood-borne hepatitis in opiate users in Iran: a poor outlook and urgent need to change nationwide screening policy. PLoS ONE. 2013;8:e82230. doi: 10.1371/journal.pone.0082230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vagenas P, Azbel L, Polonsky M, Kerimi N, Mamyrov M, Dvoryak S, et al. A review of medical and substance use co-morbidities in Central Asian prisons: implications for HIV prevention and treatment. Drug and Alcohol Dependence. 2013;132(Suppl 1):S25–S31. doi: 10.1016/j.drugalcdep.2013.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Telisinghe L, Fielding KL, Malden JL, Hanifa Y, Churchyard GJ, Grant AD, et al. High tuberculosis prevalence in a South African prison: the need for routine tuberculosis screening. PLoS ONE. 2014;9:e87262. doi: 10.1371/journal.pone.0087262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Winetsky DE, Almukhamedov O, Pulatov D, Vezhnina N, Dooronbekova A, Zhussupov B. Prevalence, risk factors and social context of active pulmonary tuberculosis among prison inmates in Tajikistan. PLoS ONE. 2014;9:e86046. doi: 10.1371/journal.pone.0086046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Margolis B, Al-Darraji HAA, Wickersham JA, Kamarulzaman A, Altice FL. Prevalence of tuberculosis symptoms and latent tuberculous infection among prisoners in northeastern Malaysia. Int. J. Tuberc. Lung Dis. 2013;17:1538–1544. doi: 10.5588/ijtld.13.0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Skrahina A, Hurevich H, Zalutskaya A, Sahalchyk E, Astrauko A, Hoffner S, et al. Multidrug-resistant tuberculosis in Belarus: the size of the problem and associated risk factors. Bull World Health Organ. 2013;91:36–45. doi: 10.2471/BLT.12.104588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Milloy M-J, Wood E, Tyndall M, Lai C, Montaner J, Kerr T. Recent incarceration and use of a supervised injection facility in Vancouver, Canada. Addict Res Theory. 2009;17:538–545. [Google Scholar]
- 44.Buavirat A. Risk of prevalent HIV infection associated with incarceration among injecting drug users in Bangkok, Thailand: case-control study. BMJ. 2003;326:308–308. doi: 10.1136/bmj.326.7384.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Epperson M, El-Bassel N, Gilbert L, Orellana ER, Chang M. Increased HIV Risk Associated with Criminal Justice Involvement among Men on Methadone. AIDS and Behavior. 2007;12:51–57. doi: 10.1007/s10461-007-9298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Widman L, Noar SM, Golin CE, Willoughby JF, Crosby R. Incarceration and unstable housing interact to predict sexual risk behaviours among African American STD clinic patients. International Journal of STD & AIDS. 2014;25:348–354. doi: 10.1177/0956462413505999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brewer RA, Magnus M, Kuo I, Wang L, Liu T-Y, Mayer KH. Exploring the relationship between incarceration and HIV among black men who have sex with men in the United States. J. Acquir. Immune Defic. Syndr. 2014;65:218–225. doi: 10.1097/01.qai.0000434953.65620.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Brewer RA, Magnus M, Kuo I, Wang L, Liu T-Y, Mayer KH. The high prevalence of incarceration history among Black men who have sex with men in the United States: associations and implications. Am J Public Health. 2014;104:448–454. doi: 10.2105/AJPH.2013.301786. • An important analysis of the effects of mass incarceration on Black men who have sex with men in the United States
- 49.Alexander M. The New Jim Crow. The New Press; 2013. [Google Scholar]
- 50.Millett GA, Peterson JL, Wolitski RJ, Stall R. Greater risk for HIV infection of black men who have sex with men: a critical literature review. Am J Public Health. 2006;96:1007–1019. doi: 10.2105/AJPH.2005.066720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Halkitis PN, Kapadia F, Siconolfi DE, Moeller RW, Figueroa RP, Barton SC, et al. Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am J Public Health. 2013;103:889–895. doi: 10.2105/AJPH.2012.300963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006:1–17. [PubMed] [Google Scholar]
- 53.Branson BM, Viall A, Marum E. Expanding HIV Testing: Back to the Future. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2013;63:S117. doi: 10.1097/QAI.0b013e3182986f25. [DOI] [PubMed] [Google Scholar]
- 54.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373:48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 55.Yang Q, Boulos D, Yan P, Zhang F, Remis RS, Schanzer D, et al. Estimates of the number of prevalent and incident human immunodeficiency virus (HIV) infections in Canada, 2008. Can J Public Health. 2010;101:486–490. doi: 10.1007/BF03403969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dieffenbach CW, Fauci AS. Universal voluntary testing and treatment for prevention of HIV transmission. JAMA: The Journal of the American Medical Association. 2009;301:2380–2382. doi: 10.1001/jama.2009.828. [DOI] [PubMed] [Google Scholar]
- 57. Gagnon M, Jacob JD, Cormier L. Total control: a critical analysis of mandatory HIV testing in U.S. prisons. J. forensic nurs. 2013;9:154–161. doi: 10.1097/JFN.0b013e31827a1f66. • The authors summarize the substantial ethical, legal and human rights concerns around HIV testing in US correctional settings
- 58.Seal DW, Eldridge GD, Zack B, Sosman J. HIV testing and treatment with correctional populations: people, not prisoners. Journal of Health Care for the Poor and Underserved. 2010;21:977–985. doi: 10.1353/hpu.0.0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.HIV testing and counselling in prisons and other closed settings. Geneva, Switzerland: United Nations Office on Drug Control and Crime; 2009. pp. 1–72. [Google Scholar]
- 60.Pope JL. HIV testing in state correctional systems. JL & Health. 2009;22:17. [Google Scholar]
- 61.HIV/AIDS Prevention, Care, Treatment and Support in Prison Settings. New York City, NY, USA: United Nations Office on Drugs and Crime; 2006. pp. 1–50. [Google Scholar]
- 62.Spaulding AC, Booker CA, Freeman SH, Ball SW, Stein MS, Jordan AO, et al. Jails, HIV testing, and linkage to care services: an overview of the EnhanceLink initiative. AIDS and Behavior. 2013;17(Suppl 2):S100–S107. doi: 10.1007/s10461-012-0339-2. [DOI] [PubMed] [Google Scholar]
- 63.de Voux A, Spaulding AC, Beckwith C, Avery A, Williams C, Messina LC, et al. Early Identification of HIV: Empirical Support for Jail-Based Screening. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0037603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Beckwith CG, Nunn A, Baucom S, Getachew A, Akinwumi A, Herdman B, et al. Rapid HIV testing in large urban jails. Am J Public Health. 2012;102(Suppl 2):S184–S186. doi: 10.2105/AJPH.2011.300514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Centers for Disease Control and Prevention (CDC) Routine HIV screening during intake medical evaluation at a County Jail - Fulton County, Georgia, 2011–2012. MMWR Morb. Mortal. Wkly. Rep. 2013;62:495–497. [PMC free article] [PubMed] [Google Scholar]
- 66. Solomon L, Montague BT, Beckwith CG, Baillargeon J, Costa M, Dumont D, et al. Survey Finds That Many Prisons And Jails Have Room To Improve HIV Testing And Coordination Of Postrelease Treatment. Health Aff (Millwood) 2014;33:434–442. doi: 10.1377/hlthaff.2013.1115. • This survey of prison and jail systems in the United States reveals that a low proportion of settings offer HIV testing and linkage consistent with official guidelines
- 67.Wohl DA, Golin C, Rosen DL, May JM, White BL. Detection of undiagnosed HIV among state prison entrants. JAMA: The Journal of the American Medical Association. 2013;310:2198–2199. doi: 10.1001/jama.2013.280740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Springer S, Friedland G, Doros G, Pesanti E, Altice F. Antiretroviral Treatment Regimen Outcomes Among HIV-Infected Prisoners. HIV Clinical Trials. 2007;8:205–212. doi: 10.1310/hct0804-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Babudieri S, Aceti A, D'Offizi GP, Carbonara S, Starnini G. Directly observed therapy to treat HIV infection in prisoners. JAMA-J. Am. Med. Assoc. 2000;284:179–180. doi: 10.1001/jama.284.2.179. [DOI] [PubMed] [Google Scholar]
- 70. Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of Human Immunodeficiency Virus Treatment During Incarceration: Viral Suppression at the Prison Gate. JAMA Intern Med. 2014 doi: 10.1001/jamainternmed.2014.601. • This retrospective review of all known individuals living with HIV/AIDS in a US state correctional system found substantial improvements in virologic control during incarceration.
- 71. Davies N, Karstaedt AS. Antiretroviral Outcomes in South African Prisoners: A Retrospective Cohort Analysis. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0033309. • This small study of individuals in the South African prison system reported virologic outcomes comparable to that observed in high-resource settings
- 72.Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. JAMA: The Journal of the American Medical Association. 2009;301:848–857. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wakeman SE, McKinney ME, Rich JD. Filling the Gap: The Importance of Medicaid Continuity for Former Inmates. J GEN INTERN MED. 2009;24:860–862. doi: 10.1007/s11606-009-0977-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, et al. Release from prison--a high risk of death for former inmates. N Engl J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Booker CA, Flygare CT, Solomon L, Ball SW, Pustell MR, Bazerman LB, et al. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release. AIDS and Behavior. 2013;17(Suppl 2):S128–S136. doi: 10.1007/s10461-012-0354-3. • This study identified important correlates of successful linkage following incarceration, including stable housing, in individuals participating in the EnhanceLink initiative
- 76.Small W, Wood E, Betteridge G, Montaner J, Kerr T. The impact of incarceration upon adherence to HIV treatment among HIV-positive injection drug users: a qualitative study. AIDS Care. 2009;21:708–714. doi: 10.1080/09540120802511869. [DOI] [PubMed] [Google Scholar]
- 77.Milloy M-J, Kerr T, Buxton J, Rhodes T, Guillemi S, Hogg R, et al. Dose-response Effect of Incarceration Events on Nonadherence to HIV Antiretroviral Therapy Among Injection Drug Users. J. Infect. Dis. 2011;203:1215–1221. doi: 10.1093/infdis/jir032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kerr T, Marshall A, Walsh J, Palepu A, Tyndall M, Montaner J, et al. Determinants of HAART discontinuation among injection drug users. AIDS Care. 2005;17:539–549. doi: 10.1080/09540120412331319778. [DOI] [PubMed] [Google Scholar]
- 79.Milloy M-J, Kerr T, Buxton J, Rhodes T, Krusi A, Guillemi S, et al. Social and environmental predictors of plasma HIV RNA rebound among injection drug users treated with antiretroviral therapy. J. Acquir. Immune Defic. Syndr. 2012;59:393–399. doi: 10.1097/QAI.0b013e3182433288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Youmans E, Burch J, Moran R, Smith L, Duffus WA. Disease progression and characteristics of HIV-infected women with and without a history of criminal justice involvement. AIDS and Behavior. 2013;17:2644–2653. doi: 10.1007/s10461-011-0057-1. • This study describes how women with a history of involvement in the criminal justice system exhibit faster disease progression
- 81.Westergaard RP, Hess T, Astemborski J, Mehta SH, Kirk GD. Longitudinal changes in engagement in care and viral suppression for HIV-infected injection drug users. AIDS. 2013;27:2559–2566. doi: 10.1097/QAD.0b013e328363bff2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Pecoraro A, Royer-Malvestuto C, Rosenwasser B, Moore K, Howell A, Ma M, et al. Factors contributing to dropping out from and returning to HIV treatment in an inner city primary care HIV clinic in the United States. AIDS Care. 2013;25:1399–1406. doi: 10.1080/09540121.2013.772273. [DOI] [PubMed] [Google Scholar]
- 83.Izenberg JM, Bachireddy C, Soule M, Kiriazova T, Dvoryak S, Altice FL. High rates of police detention among recently released HIV-infected prisoners in Ukraine: implications for health outcomes. Drug and Alcohol Dependence. 2013;133:154–160. doi: 10.1016/j.drugalcdep.2013.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Springer SA, Qiu JJ, Saber-Tehrani AS, Altice FL. Retention on Buprenorphine Is Associated with High Levels of Maximal Viral Suppression among HIV-Infected Opioid Dependent Released Prisoners. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0038335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wickersham JA, Zahari MM, Azar MM, Kamarulzaman A, Altice FL. Methadone dose at the time of release from prison significantly influences retention in treatment: implications from a pilot study of HIV-infected prisoners transitioning to the community in Malaysia. Drug and Alcohol Dependence. 2013;132:378–382. doi: 10.1016/j.drugalcdep.2013.01.005. • This study reveals how methadone dose at time of release from prison improved retention in treatment among formerly-incarcerated prisoners in Malaysia
- 86.Springer SA, Altice FL, Herme M, Di Paola A. Design and methods of a double blind randomized placebo-controlled trial of extended-release naltrexone for alcohol dependent and hazardous drinking prisoners with HIV who are transitioning to the community. Contemporary Clinical Trials. 2014;37:209–218. doi: 10.1016/j.cct.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, Altice FL. Gender disparities in HIV treatment outcomes following release from jail: results from a multicenter study. Am J Public Health. 2014;104:434–441. doi: 10.2105/AJPH.2013.301553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Althoff AL, Zelenev A, Meyer JP, Fu J, Brown S-E, Vagenas P, et al. Correlates of retention in HIV care after release from jail: results from a multi-site study. AIDS and Behavior. 2013;17(Suppl 2):S156–S170. doi: 10.1007/s10461-012-0372-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Avery AK, Ciomcia RW, Lincoln T, Desbrais M, Jordan AO, Rana AI, et al. Jails as an opportunity to increase engagement in HIV care: findings from an observational cross-sectional study. AIDS and Behavior. 2013;17(Suppl 2):S137–S144. doi: 10.1007/s10461-012-0320-0. [DOI] [PubMed] [Google Scholar]
- 90.Chen NE, Meyer JP, Avery AK, Draine J, Flanigan TP, Lincoln T, et al. Adherence to HIV treatment and care among previously homeless jail detainees. AIDS and Behavior. 2013;17:2654–2666. doi: 10.1007/s10461-011-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chitsaz E, Meyer JP, Krishnan A, Springer SA, Marcus R, Zaller N, et al. Contribution of substance use disorders on HIV treatment outcomes and antiretroviral medication adherence among HIV-infected persons entering jail. AIDS and Behavior. 2013;17(Suppl 2):S118–S127. doi: 10.1007/s10461-013-0506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jordan AO, Cohen LR, Harriman G, Teixeira PA, Cruzado-Quiñones J, Venters H. Transitional care coordination in New York City jails: facilitating linkages to care for people with HIV returning home from Rikers Island. AIDS and Behavior. 2013;17(Suppl 2):S212–S219. doi: 10.1007/s10461-012-0352-5. [DOI] [PubMed] [Google Scholar]
- 93.Krishnan A, Wickersham JA, Chitsaz E, Springer SA, Jordan AO, Zaller N, et al. Post-release substance abuse outcomes among HIV-infected jail detainees: results from a multisite study. AIDS and Behavior. 2013;17(Suppl 2):S171–S180. doi: 10.1007/s10461-012-0362-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Spaulding AC, Pinkerton SD, Superak H, Cunningham MJ, Resch S, Jordan AO, et al. Cost analysis of enhancing linkages to HIV care following jail: a cost-effective intervention. AIDS and Behavior. 2013;17(Suppl 2):S220–S226. doi: 10.1007/s10461-012-0353-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Williams CT, Kim S, Meyer J, Spaulding A, Teixeira P, Avery A, et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS and Behavior. 2013;17(Suppl 2):S195–S202. doi: 10.1007/s10461-012-0391-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zelenev A, Marcus R, Kopelev A, Cruzado-Quiñones J, Spaulding A, Desabrais M, et al. Patterns of homelessness and implications for HIV health after release from jail. AIDS and Behavior. 2013;17(Suppl 2):S181–S194. doi: 10.1007/s10461-013-0472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Spaulding AC, Messina LC, Kim BI, Chung K-W, Lincoln T, Teixeira P, et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS and Behavior. 2013;17(Suppl 2):S203–S211. doi: 10.1007/s10461-012-0341-8. [DOI] [PubMed] [Google Scholar]
- 98.Gardner EM, McLees MP, Steiner JF, del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases. 2011;52:793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Milloy M-J, Kerr T, Salters K, Samji H, Guillemi S, Montaner J, et al. Incarceration is associated with used syringe lending among active injection drug users with detectable plasma HIV-1 RNA: a longitudinal analysis. BMC Infectious Diseases. 2013;13:565. doi: 10.1186/1471-2334-13-565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Prellwitz IM, Alves BM, Ikeda MLR, Kuhleis D, Picon PD, Jarczewski CA, et al. PLoS ONE. Vol. 8. United States: Programa de Genetica, Instituto Nacional de Cancer, Rio de Janeiro, Brazil; 2013. HIV behind bars: human immunodeficiency virus cluster analysis and drug resistance in a reference correctional unit from southern Brazil; p. e69033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Menezes P, Rosen D, Wohl DA, Kiziah N, Sebastian J, Eron JJJ, et al. Low prevalence of antiretroviral resistance among HIV type 1-positive prisoners in the Southeast United States. AIDS Research and Human Retroviruses. 2013;29:136–141. doi: 10.1089/aid.2012.0102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Montaner JSG, Lima VD, Harrigan PR, Lourenço L, Yip B, Nosyk B, et al. Expansion of HAART Coverage Is Associated with Sustained Decreases in HIV/AIDS Morbidity, Mortality and HIV Transmission: The “HIV Treatment as Prevention” Experience in a Canadian Setting. PLoS ONE. 2014;9:e87872. doi: 10.1371/journal.pone.0087872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cescon A, Kanters S, Brumme CJ, Lepik KJ, Forrest JI, Hull M, et al. Trends in plasma HIV-RNA suppression and antiretroviral resistance in British Columbia, 1997–2010. J. Acquir. Immune Defic. Syndr. 2013 doi: 10.1097/QAI.0b013e3182a8efc3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Jürgens R, Betteridge G. Prisoners who inject drugs: public health and human rights imperatives. Health Hum Rights. 2005;8:46–74. [PubMed] [Google Scholar]