Abstract
Objectives
To explore associations between financial strain and self-rated health among 1341 Black adults.
Methods
Associations were investigated using a covariate-adjusted linear regression model. Mediation (via stress and/or depressive symptoms) was explored in additional models using a nonparametric bootstrapping procedure.
Results
Higher financial strain was associated with poorer self-rated health (p < .001). Stress and depressive symptoms were each significant mediators of this relation in both single and multiple mediator models (p values ≤ .05).
Conclusions
Financial strain may contribute to poorer health among Black adults, partially via greater stress and depressive symptoms. Potential theoretical, intervention, and policy implications are discussed. Future studies with longitudinal designs are needed to confirm these results.
Keywords: financial strain, self-rated health, depression, stress
Health disparities among Black adults have been an ongoing problem in the United States.1 For example, prevalence and mortality rates are higher among Black adults for heart disease, cancer, and stroke as compared to other ethnic groups.2–4 Blacks also have higher rates of HIV/AIDS than their White counterparts, and 2.3 times the infant mortality rate.4 These health disparities are reflected in perceived health status as well, with Black adults reporting substantially poorer self-reported health when compared to Whites.5 Self-reported health has been consistently linked to premature mortality and chronic conditions such as diabetes and heart disease, which particularly affect Black adults.6,7
Socioeconomic status (SES) has been linked to the health disparities experienced by Blacks. Relative to those at the higher end of the SES spectrum, individuals of lower SES experience comparatively worse health outcomes.8–10 Unfortunately, Blacks may be at particular risk for experiencing the negative ramifications of low SES on health, given that they tend to have lower SES than individuals of other race/ethnicities in this country.11 However, although a few studies have linked low SES with poorer health outcomes and higher mortality rates among Black adults,6,11 there remains debate on exactly how SES affects health. Previous studies have suggested that individuals of low SES may lack sufficient funds to satisfy basic needs and experience decreased access to healthcare and a lower quality of healthcare, potentially as a result of income inadequacy.12,13 Consequently, because income inadequacy may be a mechanism underlying the relations between low SES and negative health outcomes, it is of interest to better understand relations between income inadequacy and health status.
Income inadequacy, also known as financial strain, represents an individual’s unfavorable subjective perception of their income to needs ratio.14 As such, perceptions of financial strain can vary widely among individuals of low income (based on their needs), and can be relevant to individuals across the SES spectrum.15 Several studies have examined the relations between financial strain and health. Results indicate that financial strain is positively correlated with poor health outcomes such as early disability, increased psychological stress, chronic health conditions, and even mortality.16,17 For instance, using retrospective data about economic adversities experienced over a lifetime, one study found that long-term financial strain at the poverty level was associated with a variety of negative health outcomes in an older adult and elderly population of 1167 adults, including over 400 Black men and women.17 Another study also found a strong correlation between financial strain at the poverty level and poor health among a sample of 699 middle-aged Black twins.16 A third study found that as exposure to negative financial situations increased, the risk for poor self-rated health increased, as well as the risk for depressed mood, stress, smoking, and drug use in a sample of 1,506 urban emergency department patients, with over 50% of the sample under the age of 35 and overall 39% of whom were Black.18 However, no previous studies have examined the association of financial strain and self-rated health within a large sample of Blacks, with a diverse age range and wide-ranging spectrum of incomes. Since financial strain can be relevant to any period of life, not just older age, understanding more about the association between financial strain and self-rated health in diverse Black samples of adults is important.8
A neo-materialistic perspective suggests that inadequate access to resources accounts for the relation between financial strain and poor health.19–21 This approach posits that the social determinants of health affect one’s living conditions, which in turn influences health. However, conceptual models linking low SES (more generally) to poorer health and less desirable health behaviors have proposed that psychosocial mechanisms such as depression and stress might underlie these relations. For example, Gallo and Matthews reviewed the extant literature and found a correlation between lower SES and negative emotions and attitudes, particularly depressive symptoms.22 Research suggests that these negative emotions in turn have an adverse effect on health outcomes such as cardiovascular morbidity.22 In addition, studies have found that people with low SES face more chronically negative and stressful life events, which are also interpreted more negatively.22 Relevant to financial strain in particular, several studies have argued that those with lower SES have less material and psychological resources to manage these stressors, which may lead to increased susceptibility to future stresses.7,22 Although the aforementioned conceptual models make reference to objective SES indicators such as income, education, and/or occupation, similar pathways have been suggested to underlie relations between financial strain and poor self-rated health.23 This psychosocial perspective suggests that financial strain impacts health over time through chronic over-activation of physiologic systems related to stress (ie, increased allostatic load), which lead to assorted negative systemic effects.16,23,24 However, to the best of our knowledge, no previous studies have addressed the potential indirect effects of stress and depressive symptoms on the association between financial strain and self-rated health among a large sample of Black adults.
The purpose of the current study was to examine the relationship between financial strain and self-rated health in a large church-based sample of Black adults, while controlling for several important covariates including age, sex, partner status, income, education, and employment status. A secondary aim of the current study was to assess whether relations between financial strain and self-rated health were mediated by depressive symptoms and/or stress. Although at least one previous study has investigated the association between financial strain and self-rated health among Black adults (among middle-aged twins, in that case),16 more research is needed among Blacks of diverse ages and financial means. Based on the previous literature in this area, we hypothesized that greater financial strain would be associated with worse self-rated health, and that stress and depressive symptoms would underlie this association.
METHODS
Participants and Procedures
Data were from the second year (wave) of a longitudinal cohort study designed to investigate associations of biopsychosocial factors with health and health behaviors among Black adults. Data from this wave were analyzed because it represented the first year that financial strain was assessed. Participants (N = 1501) were originally recruited into the cohort study from a large, majority Black, Protestant church of 16,000 members located in Houston, Texas. A convenience sampling method was used. Recruitment strategies included printed and televised media within the church and in-person solicitation during church services and at a church health fair. Recruitment took place in the fall of 2008. Individuals were eligible to participate if they were ≥18 years old, residents of the Houston area, had a functional telephone number, and attended church (church membership was not a requirement).
Following enrollment, participants completed a baseline (first wave) survey focused on sociodemographics, health, and health behaviors. Approximately one year later, they were contacted via e-mail, phone, and/or mail to participate in the second wave of data collection. In total, 1375 participants (91.6% of the baseline sample) participated in the second wave. As with the baseline survey, questionnaires were completed in person at the church. Items were computer administered, and participants were compensated with a $30 gift card following survey completion. Only participants with complete data on the measures described below (N = 1341) were included in the current study. Data for the second wave were collected between January 2010 and August 2010.
Measures
Sociodemographics
Sociodemographics included age, sex, partner status (married/living with partner or single/widowed/divorced), total annual household income (<$40,000, $40,000–79,999, or ≥$80,000), educational level (<Bachelor’s degree, Bachelor’s degree, or ≥Master’s degree), and employment status (employed or unemployed).
Financial strain
The Financial Strain Questionnaire consisted of 7 items adapted from an economic strain measure to assess the degree to which it was financially difficult for participants to afford food, clothing, housing, major items (eg, car), furniture/household equipment, leisure activities, and bills at the moment.25 Response categories were: 1=no difficulty, 2=some difficulty, and 3=great difficulty. Total scores could range from 7 to 21, with higher scores indicative of greater financial strain. The Cronbach's alpha for the Financial Strain Questionnaire in this sample was .91.
Perceived stress
The Perceived Stress Scale-4 (PSS-4) is a 4-item self-report scale that was designed to assess the degree to which respondents perceive their lives to be stressful.26 The PSS-4 asks respondents to indicate how often they experienced certain situations, such as “In the last month, how often have you felt that you were unable to control the important things in your life?” and “In the last month, how often have you felt that things were going your way?” (reverse scored). Response categories were: 0=never, 1=almost never, 2=sometimes, 3=fairly often, and 4=very often. Responses were summed with a potential range of 0 to 16, where higher scores indicate greater perceived stress. The Cronbach's alpha for the PSS-4 in this sample was .74.
Depressive symptoms
The Center for Epidemiological Studies Depression 10-item scale (CESD-10) was developed to measure depressive symptoms in community non-clinical populations, and assesses the degree of depressive symptoms experienced over the past week.27,28 It includes items such as “I was bothered by things that usually don’t bother me,” and “I felt hopeful about the future” (reverse scored). Response categories were: 0=rarely or none of the time (< 1 day), 1=some or a little of the time (1–2 days), 2=occasionally or a moderate amount of time (3–4 days), and 3=all the time (5–7 days). Responses were summed with a potential range of 0 to 30, where higher scores indicate more severe depressive symptoms. The Cronbach's alpha for the CESD-10 in this sample was .54.
Self-rated health
Self-rated health was assessed with a single item asking participants to rate their health in general, with 5 response options: 1=poor, 2=fair, 3=good, 4=very good, and 5=excellent. Research suggests this item is a reasonable substitute for multi-item measures and has good psychometric utility for the assessment of general health status.29–35
Data Analysis
Preliminary analyses included summaries of participant characteristics using frequencies and descriptive statistics. Interrelations between study variables were assessed with correlations. In addition, a preliminary multiple regression analysis was conducted to explore the relations between each sociodemographic variable and financial strain (while controlling for the other sociodemographic variables).
The effect of financial strain on self-rated health was assessed with a covariate-adjusted linear regression model. The indirect effects of financial strain on self-rated health through stress and depressive symptoms, respectively, were assessed using 2 single mediation models and a multiple mediator analysis that included both stress and depressive symptoms in the same model. Indirect effects were tested using a non-parametric, bias-corrected bootstrapping procedure.36 The bootstrapping procedure generated an empirical approximation of the sampling distribution of the product of the estimated coefficients in the indirect paths using 5000 resamples from the data set. All models were adjusted for sociodemographics, including age, sex, partner status, income, education, and employment status. All analyses were performed using Statistical Analysis Software version 9.3 (SAS Institute, Cary, NC).
RESULTS
Preliminary Analyses
Participants were 46.5 (±12.7) years old on average. The majority of the sample were women (76.4%). Three quarters of participants were employed, 51.4% reported at least a Bachelor’s Degree, and 37.7% reported an annual household income of at least $80,000. Participant characteristics are displayed in Table 1. In this sample, 7.4% reported excellent health, 33.6% reported very good health, 44.4% reported good health, 13.0% reported fair health, and 1.5% reported poor health. Interrelations between study variables are shown in Table 2.
Table 1.
Participant Characteristics
| Total Sample | |
|---|---|
| N = 1341 | |
| Participant Characteristics | Mean (Std) / N [%] |
| Age | 46.5 (12.7) |
| Sex | |
| Female | 1024 [76.4] |
| Male | 317 [23.6] |
| Education | |
| < Bachelor’s Degree | 653 [48.7] |
| Bachelor’s Degree | 407 [30.4] |
| ≥ Master’s Degree | 281 [21.0] |
| Income | |
| < $40,000 | 345 [25.7] |
| $40,000–79,999 | 491 [36.6] |
| ≥ $80,000 | 505 [37.7] |
| Partner status | |
| Married/Living with partner | 605 [45.1] |
| Single/Widowed/Divorced | 736 [54.9] |
| Employment status | |
| Employed | 1007 [75.1] |
| Unemployed | 334 [24.9] |
| Self-rated Health | 3.3 (0.8) |
| Financial Strain | 11.2 (3.9) |
| Stress | 4.6 (3.0) |
| Depression | 9.2 (3.6) |
Note: Std = standard deviation. Financial Strain = The Financial Strain Questionnaire; Stress = Perceived Stress Scale; Depressive Symptoms = Center for Epidemiological Studies Depression 10-item scale.
Table 2.
Interrelations between Participant Characteristics
| Participant Characteristics | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Age | 1.000 | |||||||||
| 2. | Sex | .010 | 1.000 | ||||||||
| Female | |||||||||||
| Male (REF) | |||||||||||
| 3. | Education level | .032 | .074** | 1.000 | |||||||
| < Bachelor’s Degree (REF) | |||||||||||
| Bachelor’s Degree | |||||||||||
| ≥ Master’s Degree | |||||||||||
| 4. | Annual Household Income | .032 | −.127** | .326** | 1.000 | ||||||
| < $40,000 (REF) | |||||||||||
| $40,000–79,999 | |||||||||||
| ≥ $80,000 | |||||||||||
| 5. | Partner status | .125** | −.247** | .000 | .375** | 1.000 | |||||
| Married/Living with partner | |||||||||||
| Single/Widowed/Divorced (REF) | |||||||||||
| 6. | Employment status | −.127** | −.028 | .128** | .293** | .047 | 1.000 | ||||
| Employed | |||||||||||
| Unemployed (REF) | |||||||||||
| 7. | Self-rated Health | −.055* | −.057* | .149** | .153** | .027 | .120** | 1.000 | |||
| 8. | Financial Strain | −.140** | .070* | −.198** | −.380** | −.119** | −.173** | −.237** | 1.000 | ||
| 9. | Stress | −.154** | .037 | −.140** | −.155** | −.044 | −.084** | −.276** | .387** | 1.000 | |
| 10. | Depression | −.122** | .064* | −.130** | −.173** | −.098** | −.094** | −.277** | .316** | .657** | 1.000 |
Note:
p < .01;
p < .05.
Interrelations between participant characteristics were evaluated using Pearson correlations for continuous-continuous variable associations, Point-biserial correlations for continuous-binary associations, Spearman correlations for continuous-ordinal and ordinal-ordinal associations, Phi coefficients for binary-binary associations, and Rank biserial coefficient for ordinal-binary associations. Financial Strain = The Financial Strain Questionnaire; Stress = Perceived Stress Scale; Depressive Symptoms = Center for Epidemiological Studies Depression 10-item scale. REF= Reference group.
Results of a preliminary analysis assessing differences in financial strain as a function of sociodemographic variables are shown in Table 3. Controlling for the other sociodemographic variables, unemployed participants reported significantly greater financial strain than employed participants (means = 12.3 versus 10.8), those making less money reported significantly greater financial strain than those with higher incomes (means = 13.39 versus 11.2 versus 9.6), and those with less than a Bachelor’s degree reported significantly greater financial strain than those with at least a Master’s degree (means = 11.8 versus 10.0). In addition, younger participants experienced significantly greater financial strain than older participants.
Table 3.
Adjusted Relations of Sociodemographics and Financial Strain
| Unstandardized Coefficients |
||||
|---|---|---|---|---|
| Variables | β | Std. Error |
t | p |
| Age | −0.04 | 0.01 | −5.63 | <.001 |
| Sex | ||||
| Female | 0.37 | 0.24 | 1.56 | 0.120 |
| Male (REF) | ||||
| Education | ||||
| < Bachelor’s Degree (REF) | ||||
| Bachelor’s Degree | 0.04 | 0.23 | 0.17 | 0.865 |
| ≥ Master’s Degree | −0.68 | 0.27 | −2.51 | 0.012 |
| Income | ||||
| < $40,000 (REF) | ||||
| $40,000–79,999 | −1.76 | 0.27 | −6.61 | <.001 |
| ≥$80,000 | −3.27 | 0.30 | −10.99 | <.001 |
| Partner status | ||||
| Married/Living with partner | 0.27 | 0.22 | 1.24 | 0.215 |
| Single/Widowed/Divorced (REF) | ||||
| Employment status | ||||
| Employed | −0.79 | 0.24 | −3.31 | 0.001 |
| Unemployed (REF) | ||||
Note: Results represent relations between sociodemographic variables and financial strain, as assessed using multiple linear regression.
Main Analyses
The first hypothesis was that there would be a significant relationship between financial strain and self-rated health. Results supported this hypothesis, as greater financial strain was associated with poorer self-rated health in covariate-adjusted analyses (β = −.047, SE = .006, t = −7.41, p < .0001). The average financial strain among participants reporting excellent health was 10.1 (±3.3), versus 10.3 (±3.6) among those reporting very good health, 11.3 (±3.8) among those reporting good health, 13.0 (±4.1) among those reporting fair health, and 14.2 (±4.3) among those reporting poor health.
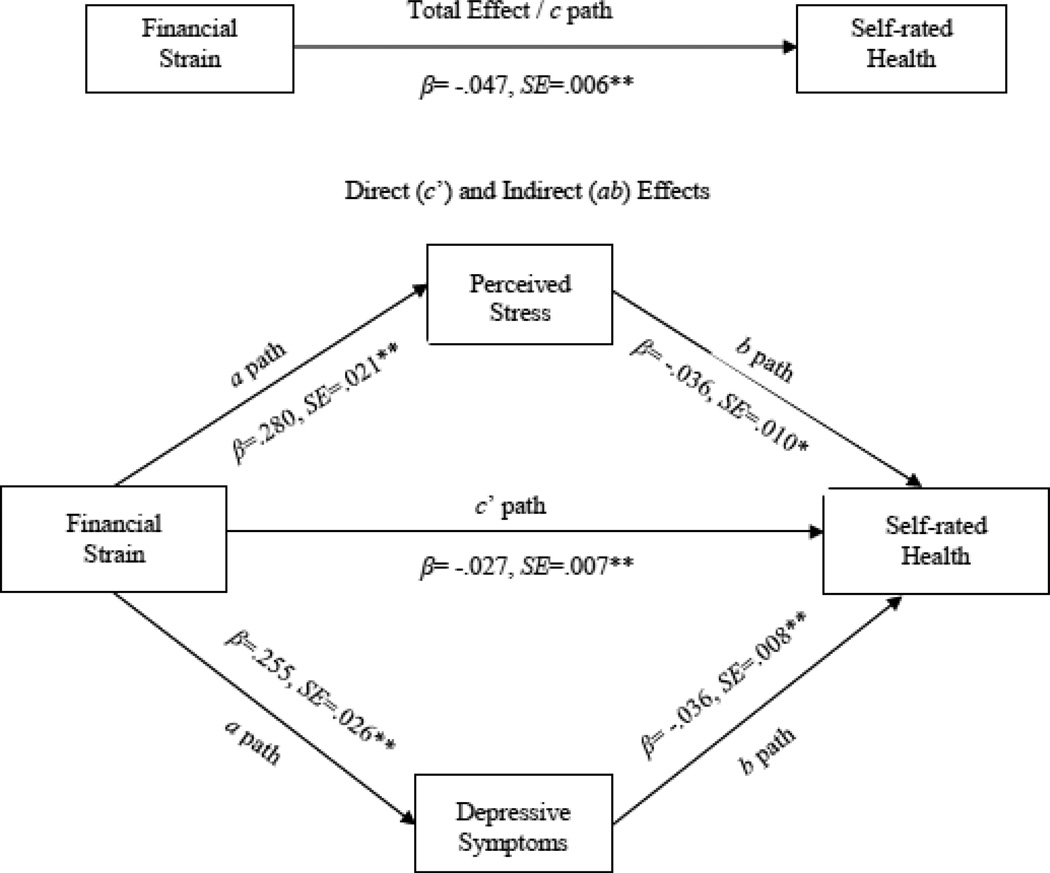
The second hypothesis was that the relationship between financial strain and self-rated health would be mediated by stress and depressive symptoms. Results supported this hypothesis, as significant indirect effects were found for both stress and depressive symptoms in the association between financial strain and self-rated health (p values ≤. 05; see Table 4). The direction of each path in the models (not shown in Table) were as follows: greater financial strain was associated with greater perceived stress (β = .28, SE = .02, t = 13.14, p < .0001) and more severe depressive symptoms (β = .26, SE = .03, t = 9.85 p < .0001), whereas greater stress and more severe depressive symptoms were each associated with poorer self-rated health (stress: β = −.06, SE = .01, t = −7.92, p < .0001; depressive symptoms β = −.05, SE = .01, t = −8.31, p < .0001).
Table 4.
Indirect Effects of Financial Strain on Self-rated Health through Stress and Depressive Symptoms
| Single Mediator Models | ||||
| Estimate of indirect effect | BCa 95% CI | |||
| Proposed Mediator | Effect Estimate | SE | Lower | Upper |
| Stress | −0.018 | 0.003 | −0.024 | −0.012 |
| Depressive Symptoms | −0.014 | 0.002 | −0.019 | −0.01 |
| Multiple Mediator Model | ||||
| Estimate of indirect effect | BCa 95% CI | |||
| Proposed Mediators | Effect Estimate | SE | Lower | Upper |
| Stress | −0.010 | 0.003 | −0.017 | −0.005 |
| Depressive Symptoms | −0.009 | 0.002 | −0.014 | −0.005 |
| Combined | −0.019 | 0.003 | −0.026 | −0.014 |
Note: Effect Estimate = The mean of the indirect effect estimates calculated across 5000 bootstrap samples. SE = The standard deviation of the 5000 bootstrap estimates of the indirect effect. BCa 95% CI= Bias corrected and accelerated 95% confidence interval. Financial Strain = The Financial Strain Questionnaire; Stress = Perceived Stress Scale; Depressive Symptoms = Center for Epidemiological Studies Depression 10-item scale.
Although stress and depressive symptoms are conceptually distinct, they were highly correlated in this sample (r = .66, p < .01). A multiple mediator analysis was conducted to take into account any shared variance. As hypothesized, results indicated significant indirect effects for stress and depressive symptoms, both uniquely as well as jointly, in the association between financial strain and self-rated health (p values ≤ .05; see Table 4 and Figure 1). Again, greater financial strain was associated with greater stress and more severe depressive symptoms, and greater stress and more severe depressive symptoms were associated with poorer self-rated health.
Figure 1.
Total (c path) and indirect effect (ab paths) of financial strain on self-rated health through proposed mediators. Mediational results presented in Figure 1 represent those from the multiple mediator analysis. Note: **p<.0001, *p<.001.
DISCUSSION
This study was the first to investigate associations between financial strain and self-rated health in a large, church-based Black sample of diverse age and financial means (eg, 25.7% reported $40,000 or less in annual income, 37.7% reported ≥$80,000/year). Results indicated that greater financial strain was significantly associated with poorer self-rated health over and above the influence of age, sex, partner status, income, education, and employment status. These findings add to a growing literature supporting relations between financial strain and health among Black adults,16,23 and extend them to a church-based, diverse sample of adults. The current study was cross-sectional in nature, and a causal link between greater financial strain and poorer perceived health cannot be inferred. However, a great deal of research has been done on the links between SES and health, and the results have consistently shown that those with lower SES exhibit poorer health outcomes, greater incidences of psychological distress, and higher mortality rates than those at the higher end of the SES spectrum.8,37 Less is known about the relationship between financial strain and health specifically, but it appears to be a promising avenue of research as initial findings have linked it to poor health outcomes,17,38 health disparities,39,40 and, in the current study, poorer self-rated health among Black adults of varying ages and socioeconomic means.
The current study also extended the extant literature by examining 2 potential mediators of the association between financial strain and self-rated health. Results indicated that stress and depressive symptoms, both individually and jointly, yielded significant indirect effects even after accounting for several major sociodemographic variables including traditional indicators of SES. The present results, although cross-sectional, appear to support the potential relevance of a psychosocial pathway in accounting for the influence of financial strain on the self-rated health of Black adults. This is particularly important because, relative to Whites and Hispanics, Black adults report experiencing more stressful events, regardless of their SES.41 It is possible that financial strain represents a significant additional (and potentially chronic) stressor that also contributes to their allostatic load, and ultimately to the relatively poorer health of Blacks. Results also support previous literature wherein depressive symptoms have been implicated as a possible mediator of the relationship between financial strain and self-rated health, but not directly examined as such.18,42 The current findings suggest that even though this sample may benefit from a supportive religious network and church attendance, financial strain nonetheless may affect their self-rated health through greater stress and depressive symptoms.
Although stress and depressive symptoms were supported as potential mechanisms underlying the association between financial strain and self-rated health, it is important to note that the direct relation between these variables remained highly significant, even after accounting for the effects of stress and depressive symptoms. This pattern of findings may provide support for the neo-material perspective, which suggests that insufficient access to healthcare and other health promoting resources directly accounts for the relation between financial strain and poor health.19–21 More specifically, this approach would argue that by virtue of inadequate financial resources, those with high financial strain do not have the opportunity to seek appropriate medical attention, pay for necessary prescriptions, tests, or follow-up care, and may not be able to sustain a healthier lifestyle (eg, eat healthier foods). Therefore, it may be that the neo-material perspective16 has additive applicability in explaining associations (ie, there is a direct effect of inadequate resources on health) in conjunction with the psychosocial perspective. Alternatively, it may also be that other potential psychosocial mechanisms not examined in this study (eg, mastery, social support),23 play salient roles in the association between financial strain and health. Additional research is needed to further elucidate the contributions of the neo-materialistic and the psychosocial perspectives in the relation of financial strain and health among Black adults.
The current results suggest that interventions aimed at Blacks experiencing financial strain need to address stress and depressive symptoms. Such efforts may help to reduce the potential impact of financial strain on health. Interventions might utilize church-based ministries or outreach efforts (eg, financial planning courses, provision of material aid), stress management/coping skills classes, and by referral to community professionals willing to work pro bono or on a sliding scale to address more severe stress and depressive symptoms (as applicable). However, church-based approaches may not reach or appeal to non-church goers. Consequently, to the extent to which these findings may be generalizable to the broader population of Black adults, results also suggest that healthcare or community agencies who routinely work with individuals at risk of income inadequacy (eg, federally qualified health centers, neighborhood centers) might consider screening for financial strain problems and proactively addressing them to the extent possible by enabling connections with local resources, and providing education about how to deal with stress in adaptive ways such as via mindfulness training or relaxation techniques. In addition, the Black community itself could be an important resource for intervention development. Investigators aiming to address the impact of financial strain on health might partner with churches or other agencies for community-based participatory collaborations that involve community members in all aspects of the intervention process. In addition, qualitative methods such as focus groups conducted with affected community members can aid in the identification of important factors that generate and perpetuate financial strain, as well as components that might be important to address within intervention designs. Finally, facilitating the availability of resources at a state or federal level for individuals experiencing financial strain is also important, potentially via policy changes including increased tax credits or the extension and expansion of government-supplemented mental health and medication coverage (eg, prescription drug support).16 Recent federal health care reform efforts (eg, Patient Protection and Affordable Care Act, 2010) may be a viable mechanism through which to implement changes to better integrate social work practices (as well as other relevant resources) into routine healthcare visits to assist with the alleviation of financial strain and its sequelae, as discussed in previous work (see18 for more information). In addition, ongoing discussions with local and state elected officials may raise awareness about these issues.
The limitations of this study should be noted and include design, measurement, and sampling drawbacks. Due to the study’s cross-sectional design, causation cannot be inferred and the potential for reverse causality in mediational analyses cannot be ruled out. Future studies should investigate the mediational pathways between financial strain and self-rated health using a longitudinal design in order to avoid these complications and clarify the temporal relationships between these variables. The current study used only self-report measures, which may be biased (eg, social desirability, recall errors). In addition, the measure of depressive symptoms used in this study had less than desirable internal consistency, which could be due to the study’s use of the shorter, 10-item version of CESD rather than the standard 20-item form. Furthermore, past research has found that Blacks may present atypically with regards to depressive symptoms43 which could have affected the response patterns of our sample. Future studies might also use objective measures of health status, when possible, such as medical records, blood pressure readings, etc. Furthermore, this study only was focused on 2 potential mediators of the relationship between financial strain and self-rated health. Future research might include other psychosocial mechanisms of interest as suggested by previous work in the area (ie, mastery, social support).23
This study focused on a large, convenience sample of predominately female Black church-goers from a large metropolitan city in the southern United States. Consequently, results may not be generalizable to church attendees from other congregations. In addition, Black women attend church services at a higher rate than Black men. Consequently, results may be more applicable to Black women than men. Moreover, the majority of our sample was comprised of Black women, which adds to the possibility that these results could be more relevant to Black women than to Black men. Moreover, results may not generalize to individuals of other racial/ethnic groups. However, there were several benefits to the examination of these relations among a Black sample (eg, removes confounding of race/ethnicity). Finally, the study sample was comprised of church-goers, and results may not generalize to Blacks who do not attend church. However, statistics suggest that up to 55% of Black adults regularly attend church services.44
This study benefitted from a large sample of diversely aged Black adults of varying financial means and the inclusion of a wide range of covariates. Future research might improve upon the present study by examining other variables that might impact or play an important role in the association between financial strain and self-rated health among Black adults. For example, racism, both perceived and overt, might affect the direct and indirect associations between financial strain and self-rated health. Previous studies have found a relationship between self-reported racism and negative mood states,45 poor coping responses,46 and negative mental and physical health outcomes.47 Of those focusing on the Black community, initial support has been found for the relationship between racism-related stress and poor health, suggesting that further study is warranted.48,49 Consequently, future studies might, for example, examine racism as a moderator of associations between financial strain and self-rated health, or otherwise determine its potential contributory effects within more comprehensive conceptual model. In addition, because we collected income information in broad ranges, we were unable to calculate poverty status in the present sample. However, it is likely that many participants in the current sample were living above the poverty level (eg, 37.7% reported ≥$80,000 in annual household income). Future studies with similar samples might consider the role of not only poverty status but also relative poverty status on health and the mechanisms that influence health status among Black adults. Finally, participant’s religiosity could have moderated association of financial strain and self-rated health, and future studies might also investigate this possibility.
In summary, greater financial strain was significantly associated with worse self-rated health, and both stress and depressive symptoms significantly mediated this relationship in a church-based sample. These findings extend the literature through the inclusion of a large sample of Black adults of diverse ages and economic means, and by implicating both stress and depressive symptoms as possible mediators of the relation of financial strain and self-rated health. Future research should attempt to further test these pathways using longitudinal designs in order to better infer causation and elucidate the relationship between depressive symptoms, stress, financial strain, and self-rated health. The current study provides direction to inform future work in this area.
Acknowledgements
Data collection and management were supported by funding from the University Cancer Foundation; the Duncan Family Institute through the Center for Community-Engaged Translational Research; the Ms. Regina J. Rogers Gift: Health Disparities Research Program; the Cullen Trust for Health Care Endowed Chair Funds for Health Disparities Research; the Morgan Foundation Funds for Health Disparities Research and Educational Programs; and the National Cancer Institute at the National Institutes of Health through The University of Texas MD Anderson's Cancer Center Support Grant (CA016672). Manuscript authorship and publication were supported by institutional funds from The University of Texas MD Anderson Cancer Center and the University of Houston. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the project supporters.
We would like to acknowledge the research staff at The University of Texas MD Anderson Cancer Center who assisted with implementation of the original project. We are also appreciative of the Patient-Reported Outcomes, Survey, and Population Research Shared Resource at The University of Texas MD Anderson Cancer Center, which was responsible for scoring the survey measures used in this research. Finally, we especially want to thank the church leadership and participants, whose efforts made this study possible.
Footnotes
This work was completed while the first author was a Graduate Trainee in the Department of Health Disparities Research at The University of Texas MD Anderson Cancer Center, Houston, TX.
Human Subjects Statement
All procedures were approved by the University of Texas MD Anderson Cancer Center Institutional Review Board. Informed consent was obtained from participants prior to data collection.
Conflict of Interest Statement
The authors have no competing interests pertaining to this research.
Contributor Information
Elaine J. Savoy, Department of Clinical Psychology, University of Houston, Houston, TX.
Lorraine R. Reitzel, Department of Educational Psychology, College of Education, University of Houston, Houston, TX.
Nga Nguyen, Department of Biostatistics, The University of Texas MD Anderson Cancer Center, Houston, TX.
Pragati S. Advani, Department of Health Promotion and Behavioral Sciences, The University of Texas School of Public Health.
Felicia D. Fisher, Department of Educational Psychology, College of Education, University of Houston, Houston, TX.
David W. Wetter, Department of Health Disparities Research, The University of Texas MD Anderson Cancer Center, Houston, TX.
Adolfo G. Cuevas, Department of Psychology, Portland State University, Portland, OR.
Lorna H. McNeill, Department of Health Disparities Research, The University of Texas MD Anderson Cancer Center, Houston, TX.
REFERENCES
- 1.Centers for Disease Control and Prevention. Black or African American populations. [Accessed June 11, 2013]; (on-line). Available at: http://www.cdc.gov/minorityhealth/populations/REMP/black.html.
- 2.Fagan P, Moolchan ET, Lawrence D, et al. Identifying health disparities across the tobacco continuum. Addiction. 2007;102(2):5–29. doi: 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- 3.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102(25):3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 4.Office of Minority Health. African American profile. [Accessed June 17 2013]; (on-line). Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3&lvlid=23.
- 5.Boardman JD. Health pessimism among black and white adults: the role of interpersonal and institutional maltreatment. Soc Sci Med. 2004;59(12):2523–2533. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Idler EL, Russel LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I epidemiological follow-up study, 1992. First national health and nutrition examination survey. Am J Epidemiol. 2000;152(9):874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- 7.Latham K, Peek CW. Self-rated health and morbidity onset among late midlife U.S. adults. J Gerontol B Psychol Sci Soc Sci. 2013;68B(1):107–116. doi: 10.1093/geronb/gbs104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- 9.House JS, Lepkowski JM, Kinney AM, et al. The social stratification of aging and health. J Health Soc Behav. 1994;35(3):213–234. [PubMed] [Google Scholar]
- 10.Keppel KG, Pearcy JN, Wagener DK. Trends in racial and ethnic-specific rates for the health status indicators:United States, 1990–98. Healthy People 2000 Stat Notes. 2002;(23):1–16. [PubMed] [Google Scholar]
- 11.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94(8):666–668. [PMC free article] [PubMed] [Google Scholar]
- 12.Fleegler EW, Lieu TA, Wise PH, Muret-Wagstaff S. Families' health-related social problems and missed referral opportunities. Pediatrics. 2007;119(6):e1332–e1341. doi: 10.1542/peds.2006-1505. [DOI] [PubMed] [Google Scholar]
- 13.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, D.C.: National Academies Press; 2003. pp. 25–190. [PubMed] [Google Scholar]
- 14.Oakes JM, Rossi PH. The measurement of SES in health research: current practice and steps towards a new approach. Soc Sci Med. 1982;56(4):769–784. doi: 10.1016/s0277-9536(02)00073-4. [DOI] [PubMed] [Google Scholar]
- 15.Szanton SL, Allen JK, Thorpe RJ, Jr, et al. Effect of financial strain on mortality in community-dwelling older women. J Gerontol B Psychol Sci Soc Sci. 2008;63(6):S369–S374. doi: 10.1093/geronb/63.6.s369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szanton SL, Thorpe RJ, Whitfield K. Life-course financial strain and health in African-Americans. Soc Sci Med. 2010;71(2):259–265. doi: 10.1016/j.socscimed.2010.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47(1):17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 18.Bisgaier J, Rhodes KV. Cumulative adverse financial circumstances: associations with patient health status and behaviors. Health Soc Work. 2011;36(2):129–137. doi: 10.1093/hsw/36.2.129. [DOI] [PubMed] [Google Scholar]
- 19.Krieger N, Chen JT, Coull BA, Selby JV. Lifetime socioeconomic position and twins' health: an analysis of 308 pairs of United States women twins. PLoS Med. 2005;2(7):0645–0653. doi: 10.1371/journal.pmed.0020162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Link BG, Phelan JC. Understanding sociodemographic differences in health--the role of fundamental social causes. Am J Public Health. 1996;86(4):471–473. doi: 10.2105/ajph.86.4.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phelan JC, Link BG, Diez-Roux A, et al. "Fundamental causes" of social inequalities in mortality: a test of the theory. J Health Soc Behav. 2004;45(3):265–285. doi: 10.1177/002214650404500303. [DOI] [PubMed] [Google Scholar]
- 22.Gallo LC, Matthews KA. Understanding the association between socioeconomic status and physical health: do negative emotions play a role? Psychol Bull. 2003;129(1):10–51. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- 23.Lincoln KD. Financial strain, negative interactions, and mastery: pathways to mental health among older African Americans. J Black Psychol. 2007;33(4):439–462. doi: 10.1177/0095798407307045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 25.Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. J Health Soc Behav. 1981;22(4):337–356. [PubMed] [Google Scholar]
- 26.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D scale. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 28.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (center for epidemiologic studies depression scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 29.DeSalvo KB, Fisher WP, Tran K, et al. Assessing measurement properties of two single-item general health measures. Qual Life Res. 2006;15(2):191–201. doi: 10.1007/s11136-005-0887-2. [DOI] [PubMed] [Google Scholar]
- 30.McHorney CA. Health status assessment methods for adults: past accomplishments and future challenges. Annu Rev Public Health. 1999;20:309–335. doi: 10.1146/annurev.publhealth.20.1.309. [DOI] [PubMed] [Google Scholar]
- 31.Kempen GI. The MOS short-form general health survey: single item vs multiple measures of health-related quality of life: some nuances. Psychol Rep. 1992;70(2):608–610. doi: 10.2466/pr0.1992.70.2.608. [DOI] [PubMed] [Google Scholar]
- 32.Cunny KA, Perri M. Single-item vs multiple-item measures of health-related quality of life. Psychol Rep. 1991;69(1):127–130. doi: 10.2466/pr0.1991.69.1.127. [DOI] [PubMed] [Google Scholar]
- 33.Bierman AS, Bubolz TA, Fisher ES, Wasson JH. How well does a single question about health predict the financial health of medicare managed care plans? Eff Clin Pract. 1999;2(2):56–62. [PubMed] [Google Scholar]
- 34.Jylha M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 35.Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol. 2009;170(3):343–351. doi: 10.1093/aje/kwp144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 37.Hayward MD, Miles TP, Crimmins EM, Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Am Sociol Rev. 2000;65(6):910–930. [Google Scholar]
- 38.Matthews RJ, Smith LK, Hancock RM, et al. Socioeconomic factors associated with the onset of disability in older age: a longitudinal study of people aged 75 years and over. Soc Sci Med. 2005;61(7):1567–1575. doi: 10.1016/j.socscimed.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 39.Kahn JR, Fazio EM. Economic status over the life course and racial disparities in health. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):76–84. doi: 10.1093/geronb/60.special_issue_2.s76. [DOI] [PubMed] [Google Scholar]
- 40.Kendzor DE, Businelle MS, Costello TJ, et al. Financial strain and smoking cessation among racially/ethnically diverse smokers. Am J Public Health. 2010;100(4):702–706. doi: 10.2105/AJPH.2009.172676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Businelle MS, Mills BA, Chartier KG, et al. Do stressful events account for the link between socioeconomic status and mental health? J Public Health (Oxf) doi: 10.1093/pubmed/fdt060. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DeRijk RH, Wust S, Meijer OC, et al. A common polymorphism in the mineralocorticoid receptor modulates stress responsiveness. J Clin Endocrinol Metab. 2006;91(12):5083–5089. doi: 10.1210/jc.2006-0915. [DOI] [PubMed] [Google Scholar]
- 43.Wohi M, Lesser I, Smith M. Clinical presentations of depression in African American and white outpatients. Cult Divers Ment Health. 1997;3(4):279–284. doi: 10.1037/1099-9809.3.4.279. [DOI] [PubMed] [Google Scholar]
- 44.Gallup. Americans' church attendance inches up in 2010: Increase accompanies rise in economic confidence. [Accessed June 18, 2013]; (on-line). Available at: http://www.gallup.com/poll/141044/american-church-attendance-inches-2010.aspx#22010. [Google Scholar]
- 45.Cuevas AG, Reitzel LR, Adams CE, et al. Discrimination, affect, and cancer risk factors among African Americans. Am J Health Behav. 2014;38(1):31–41. doi: 10.5993/AJHB.38.1.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brondolo E, Thompson S, Brady N, et al. The relationship of racism to appraisals and coping in a community sample. Ethn Dis. 2005;15(4):S5-14–S5-19. [PubMed] [Google Scholar]
- 47.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 48.Utsey SO, Giesbrecht N, Hook J, Stanard PM. Cultural, sociofamilial, and psychological resources that inhibit psychological distress in African Americans exposed to stressful life events and race-related stress. J Couns Psychol. 2008;55(1):49–62. [Google Scholar]
- 49.Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans: a biopsychosocial model. Am Psychol. 1999;54(10):805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]