Abstract
Purpose
To evaluate the therapeutic effect of human adipose-derived stem cells (hASCs) overlaid on a scleral contact lens (SCL) carrier in a rabbit model of ocular alkaline burn.
Materials and Methods
After inducing alkaline burn in 11 New Zealand white rabbits, hASCs cultured on SCLs were placed on the right eye of 5 rabbits, SCLs without cells were used in 5, and no treatment was applied in 1 eye. Each eye was examined and photographed for corneal vascularization, opacities, and epithelial defect in week 1, 2, and 4 after surgery. After 1 month, rabbits were killed and the corneas were removed and cut in half for electron and light microscopy examination.
Results
Human adipose-derived stem cells were attached to SCL surface and confluent easily. Human adipose-derived stem cells on SCL eyes showed smaller epithelial defect, less corneal opacity, corneal neovascularization relative to SCL eyes. Both groups showed no symblepharon. However, the cornea in the untreated eye was melted in 2 weeks and developed severe symblepharon.
Conclusion
Human adipose-derived stem cells on SCL can reduce inflammation and corneal haziness in severe ocular alkaline burn injury in rabbits.
Keywords: Limbal stem cell deficiency, Adipose-derived stem cell, scleral contact lens, alkaline burn
Limbal stem cell deficiency (LSCD) is a vision-threatening condition with a significant socioeconomic impact for reasons that include the necessity for long-term follow-up care and high cost/poor prognosis of treatments such as penetrating keratoplasty.1–3 Recently, particular attention has focused on the development of regenerative cell therapy such as tissue-engineered cultivated epithelial stem cell transplantation as a new approach for ocular surface reconstruction in cases of severe LSCD.4–10 Pellegrini et al.8 reported the first successful ocular surface reconstruction for patients with unilateral LSCD using autologous cultivated corneal epithelial stem cells. Since then, scientists around the world have attempted to develop new and better methods for ocular surface reconstruction, especially for bilateral severe LSCD. Buccal mucosa,11 hair follicles,12 as well as umbilical cord lining stem cells13 and dental pulp,14 have been studied as alternative stem cell sources but have been variably effective and yet to be approved for clinical use. There is still a clear need for a cell source that has the ability to remodel tissues in vivo to treat LSCD. Therefore, mesenchymal stem cells (MSCs) have been considered as an ocular regenerative source by several research groups.15–19 Abundant evidence demonstrates that the repair and regeneration of damaged tissue by MSCs is because of differentiation and paracrine signaling induced by injury. Mesenchymal stem cell differentiation contributes by regenerating damaged tissue, whereas MSC paracrine signaling regulates the local cellular responses to injury. Current data suggest that the contribution of MSC differentiation is limited because of poor engraftment and survival of MSCs at the site of injury.20,21 Given these limitations, it has been proposed that MSC paracrine signaling is the primary mechanism of action in response to injury such as inflammation. Inflammation results in activation of MSCs to express an anti-inflammatory protein such as TNF-α–stimulated gene/protein 6 (TSG-6).20,21
In addition to obtaining a source of stem cells, a carrier is needed to deliver the cultured stem cells to the ocular surface. Human amniotic membrane, for example, is a commonly used carrier22 because it has angiostatic and anti-inflammatory properties.23 Its biodegradation time, however, is variable and depends on the processing and the particular storage regimes used in the tissue banks.24 In addition, despite extensive screening, there is some risk of viral disease transmission.25 Thus, there is a clear need to develop a synthetic biocompatible material that could be used as a substitute for the amniotic membrane and would function to allow both the attachment of the stem cells and their subsequent delivery onto the cornea. Soft contact lenses,26,27 recombinant collagen,28 electrospun scaffolds,29 temperature sensitive polymers,30 and polymer gels31 have all been investigated. We described a preliminary report on the therapeutic effect of human adipose-derived stem cells (hASCs) overlaid on a scleral contact lens (SCL) carrier in a rabbit model of ocular alkaline burn.
MATERIALS AND METHODS
Human Adipose-Derived Stem Cell Culture
Human adipose-derived stem cells were isolated from lip-oaspirates as previously described.32 Briefly, human subcutaneous adipose tissue samples that obtained from liposuction aspirates were treated with type 1 collagenase at 37°C for approximately 60 min. After digestion, the samples were centrifuged to separate the stromal vascular fraction from primary adipocytes. Stromal vascular fraction was washed, plated, and then cryopreserved. For the experiment, cryopreserved hASCs were thawed and cultured in complete culture medium (CCM) containing DMEM/F12, 10% FBS (Atlanta Biologicals, Lawrenceville, GA) and 1X antibiotic-antimycotic (Invitrogen-Gibco, Grand Island, NY). The cells were incubated in a humidified atmosphere at 37°C with 5% CO2, and the media was changed every 3 to 4 days. Cells from 2 different donors between passages 3 and 4 were used for the experiment.
Customized Scleral Contact Lens Suitable for Rabbit Eyes
Scleral contact lenses (Essilor Company, Dallas, TX) were designed with optical, transition, and landing zones and base curve of 7.2 mm, sagittal depth of 2.7 mm, and diameter of 15.4 mm based on average rabbit cornea diameter, cornea curvature, anterior chamber depth, and equator diameter.33 They were made from tisilfocon A (Menicon Z) with Dk of 163 and wetting angle of 24.
Culture of Human Adipose-Derived Stem Cells on Scleral Contact Lens
Passage 3 of hASCs was cultured on customized SCL in a 6-well plate (Costar; Sigma–Aldrich, St. Louis, MO) at a concentration of 125,000 cells per milliliter per well in CCM. The 6-well plate kept in a 37°C incubator with 5% carbon dioxide for 72 hr. The cell attachment and morphological features were examined by an inverted microscope (Axio Observer; Carl Zeiss Microscopy, Thornwood, NY).
Animal Study
Animal protocol was approved by the Institutional Animal Care and Use Committee at Tulane University. Eleven adult New Zealand White rabbits (weight, 2–3 kg) were used for the experiment. All animal procedures were performed in compliance with the Association for Research in Vision and Ophthalmology Statement for Use of Animals in Ophthalmic and Vision Research. Rabbits were anesthetized with a combination of intramuscular ketamine hydrochloride (50 mg/kg) and xylazine hydrochloride (5 mg/kg) and topical proparacaine drops. Thereafter, the right eye of each rabbit underwent severe acute alkaline burn, a 15-mm filter paper soaked in solution of 1 M sodium hydroxide was applied for 1 min and then the eye was copiously washed with balanced salt solution until PH became approximately 7 to 7.5 (measured by PH paper). Then, SCL with hASCs overlay were applied over five eyes, five eyes were covered by SCL only and one eye was left without treatment as a control. Postoperatively, eye drops (prednisolone acetate 1%, and moxifloxacin hydro-chloride 0.5%) were used twice daily for 2 weeks in all eyes.
Clinical Observation
Each eye was examined by portable slitlamp (Keeler PSL, Broomall, PA), photographed and scored for corneal neovascularization (CNV), haziness, and epithelial defect surface area in weeks 1, 2, and 4 after surgery. Haze was evaluated on a scale of 0 to 4 (0 for total transparency and 4 for severe haze that makes it impossible to observe the details of iris and pupil). Corneal neovascularization was quantified based on the number of corneal quadrant involvement. Epithelial defect surface area was measured after applying fluorescein to the cornea.
Tissue Procurement
Rabbits were killed using intravenous pentobarbital sodium, 100 mg/kg, at week 4. The corneas were removed and cut in half; one half were placed in glutaraldehyde, 2.5%, then tissue samples were dissected into 1- to 1.5-mm2 cubes and sent for transmission electron microscopy (TEM) study (Hitachi H-7500 TEM; Tokyo, Japan). The other half was placed in neutral formaldehyde, 10%, and fixed in paraffin for light microscopy (Axio Imager; Carl Zeiss Microscopy, Thornwood, NY) and underwent hematoxylin-eosin staining. Tissue blocks were cut at 5-mm thickness.
Statistical Analysis
Mean and standard deviation of epithelial defect surface area in each group was calculated. The Kruskal-Wallis test (nonparametric equivalent to analysis of variance) was used to compare groups at each time point (Table 1). A P<0.05 was established as statistically significant value.
TABLE 1.
Clinical Findings During Follow-up
| Week 1 |
Week 2 |
Week 4 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Eyes | ED (Mean±SD), mm2 | CNV | CO | Sym | ED (Mean±SD), mm2 | CNV | CO | Sym | ED (Mean±SD), mm2 | CNV | CO | Sym |
| Treated SCL-ASC (average of 5 eyes) | 50.24±12.56 | 1/4 | 4 | – | 12.56±3.14 | 1/4 | 3 | – | 3.14±0.785 | 1/4 | 2 | – |
| Treated SCL only (average of 5 eyes) | 113.04±15.68 | 2/4 | 4 | – | 50.24±12.56 | 2/4 | 4 | – | 28.26±9.75 | 2/4 | 3 | – |
| Untreated (1 eye) | 452.16±50.24 | 3/4 | 4 | + | 452.16±50.24 | 3/4 | Melt | ++ | Killed at week 2 | |||
| Kruskal-Wallis test (P-value) | <0.0001 | <0.0001 | 0.01 | |||||||||
CNV, corneal neovascularization; CO, corneal opacity; ED, epithelial defect surface area; SCL-ASC, scleral contact lens with adipose-derived stem cell overlay; SD, standard deviation; Sym, symblepharon; –, negative; +, mild; ++, moderate.
RESULTS
Human Adipose-Derived Stem Cells Culture on Scleral Contact Lens
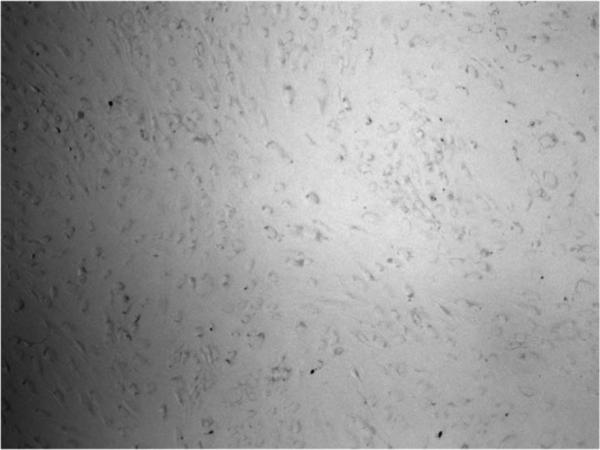
Figure 1 shows attachment and morphology of hASCs on SCL. The cells were attached within 24 hr and expanded to form spindle-shaped cells and formed confluence after 72 hr.
FIG. 1.
Attachment and morphology of human adipose-derived stem cells on scleral contact lens 24 hr after culture. The cells were attached and formed spindle-shaped cells. Magnification, ×5.
Clinical Observation
Epithelial defect surface area, corneal opacity, CNV, and symblepharon documented as shown in Table 1. Treated eyes with hASC-SCL showed statistically significant smaller epithelial defect (P<0.0001), less corneal opacity, and less CNV relative to SCL-treated eyes at each time point. Symblepharon was not observed in hASC-SCL and SCL groups. However, the cornea in the untreated eye was melted and the rabbit was euthanized in 2 weeks (Fig. 2A–C).
FIG. 2.
Photographic pictures of corneas at last follow-up. (A) One of the treated eyes (SCL-ASC) that shows central corneal opacity and clear periphery without significant neovascularization and epithelial defect. (B) One of the treated eyes with SCL only that shows more aggravated eye with more corneal opacity, neovascularization, and epithelial defect. (C) An untreated eye with corneal melting, severe central thinning, and symblepharon (it was hard to keep eyelids open). ASC, adipose-derived stem cell; SCL, scleral contact lens.
Light and Electron Microscopic Examination
In light microscopic examination, the treated eyes showed fair collagen alignments and epithelialization and minimal inflamma-tory reactions (Fig. 3A). Cellular infiltration and vascularization of the cornea with central epithelial defect were observed in eyes that covered only by SCL (Fig. 3B), and control eye without treatment showed severe disorganization of cornea stroma with scar tissue, thinning, infiltration, melting, and vascularization (Fig. 3C). In TEM, treated eyes showed better collagen alignment and less fibroblastic reaction compared with disorganization and separation of collagen fibers and stromal edema in untreated eye (Fig. 4A–C).
FIG. 3.
Micrographic pictures of hematoxylin-eosin staining at last follow-up. (A) One of the treated eyes (SCL-ASC) that shows better collagen organization and epithelialization and no inflammation in central cornea. (B) One of the treated eyes with SCL only that shows infiltration and vascularization in periphery with central epithelial defect. (C) An untreated eye with severe disorganization of cornea stroma with scar tissue, thinning, infiltration, and melting. ASC, adipose-derived stem cell; SCL, scleral contact lens.
FIG. 4.
Electron microscopy pictures at last follow-up. (A) One of the treated eyes (SCL-ASC) that shows normal collagen alignment, no infiltration, and less fibroblast reaction. (B) One of the treated eyes with SCL only that shows inflammatory cells and more fibroblastic reaction. (C) An untreated eye with separation of collagen fibers and stromal edema and severe disorganization. ASC, adipose-derived stem cell; SCL, scleral contact lens.
DISCUSSION
Ocular alkaline burns are considered one of the most serious work-related accidents with a significant socioeconomic impact because of the high cost of treatment and the severe visual impairment due to severe LSCD, which often ends in disability.34 Because MSCs are easy to isolate and have the potential to differentiate into epithelial cells and have anti-inflammatory characteristics, several groups tested whether MSCs can be used to treat corneal disorders.15 We have chosen to explore the effect of hASCs and the use of a scleral rigid contact lens as a carrier for the management of LSCD for several reasons:
Human adipose-derived stem cells are multipotent and can differentiate into other cell lines, such as limbal epithelial stem cells, corneal epithelial cells, and keratocytes.35–37
Adipose tissue is a good source of stem cells because it is easy to harvest, and the yield of MSC from adipose tissue is 100- to 500-fold higher than that from the bone marrow.38
Human adipose-derived stem cells have anti-inflammatory potential,39,40 therefore, have the potential to serve as universal donor cells.
Scleral contact lens is a well-known and effective method for visual rehabilitation in ocular surface disorders and severe dry eye syndrome because of the tear reservoir behind the contact lens and optical properties.41
In this study, we showed even in acute severe alkaline burn, application of hASCs overlaid on SCL prevents corneal melting and symblepharon. Hematoxylin-eosin staining showed epithelialization and less inflammation in treated eyes, and TEM study showed less inflammatory and fibroblastic reaction in treated eyes. Previous studies by Zeppieri et al.42 and Lin et al.43 showed that the adipose-derived stem cell (ASC)-treated eyes had significantly smaller epithelial defects at each time point compared with control eyes, and stem cell-treated corneas had complete re-epithelization, with less inflammatory cells and limited fibroblast activation structure compared with control eyes. We used SCL as a carrier for stem cells in contrast to Zeppieri et al. who investigate topical use of ASC for treating chemically injured rat cornea and Lin et al. who used subconjunctival injection of human ASCs for regeneration of rabbit cornea after alkaline chemical burn. We believe that the use of carrier will extend the duration of interaction between stem cells and ocular surface, which will be beneficial in long term. In our study, ASCs were detectable on the surface of contact lens after removal at 4 weeks (data were not shown).
We showed that SCL is a viable carrier for cells because hASCs were attached and proliferated easily on SCLs within 24 hr after culture. The material is nontoxic, has high oxygen permeability, can be easily fabricated, and plasma treated. To the best of our knowledge, this is the first study that uses SCL as a cell carrier. Our study has some limitations such as small sample size, inducing severe alkaline burn, short-term follow-up, and lack of immunostaining studies. Future studies in our laboratory will address these issues. In conclusion, more studies are needed to optimized application of hASCs in LSCD; however, we believe that this study similar to Zeppieri et al. and Lin et al. shows promising therapeutic role of hASCs in severe ocular alkaline injury.
ACKNOWLEDGMENTS
The authors would like to thank Corey Dickson for his contribution in contact lens design and ordering and Majid Roohafza for his assistance in preparing figures.
Supported by Department of Ophthalmology Research Fund and in part by CTRECP grant from Tulane University.
Footnotes
The authors have no other funding or conflicts of interest to disclose.
REFERENCES
- 1.Lee P, Wang CC, Adamis AP. Ocular neovascularization: An epidemiologic review. Surv Ophthalmol. 1998;43:245–269. doi: 10.1016/s0039-6257(98)00035-6. [DOI] [PubMed] [Google Scholar]
- 2.Brodovsky SC, McCarty CA, Snibson G, et al. Management of alkali burns: An 11-year retrospective review. Ophthalmology. 2000;107:1829–1835. doi: 10.1016/s0161-6420(00)00289-x. [DOI] [PubMed] [Google Scholar]
- 3.Dua HS, King AJ, Joseph A. A new classification of ocular surface burns. Br J Ophthalmol. 2001;85:1379–1383. doi: 10.1136/bjo.85.11.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liang L, Sheha H, Li J, et al. Limbal stem cell transplantation: New progresses and challenges. Eye (Lond) 2009;23:1946–1953. doi: 10.1038/eye.2008.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kenyon KR, Tseng SCG. Limbal autograft transplantation for ocular surface disorders. Ophthalmology. 1989;96:709–722. doi: 10.1016/s0161-6420(89)32833-8. [DOI] [PubMed] [Google Scholar]
- 6.Tsai RJF, Tseng SCG. Human allograft limbal transplantation for corneal surface reconstruction. Cornea. 1994;13:389–400. doi: 10.1097/00003226-199409000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Tsubota K, Satake Y, Kaido M, et al. Treatment of severe ocular surface disorders with corneal epithelial stem-cell transplantation. N Engl J Med. 1999;340:1697–1703. doi: 10.1056/NEJM199906033402201. [DOI] [PubMed] [Google Scholar]
- 8.Pellegrini G, Traverso CE, Franzi AT, et al. Long-term restoration of damaged corneal surfaces with autologous cultivated corneal epithelium. Lancet. 1997;349:990–993. doi: 10.1016/S0140-6736(96)11188-0. [DOI] [PubMed] [Google Scholar]
- 9.Tsai RJF, Li LM, Chen JK. Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med. 2000;343:86–93. doi: 10.1056/NEJM200007133430202. [DOI] [PubMed] [Google Scholar]
- 10.Shortt AJ, Secker GA, Notara MD, et al. Transplantation of ex vivo cultured limbal epithelial stem cells: A review of techniques and clinical results. Surv Ophthalmol. 2007;52:483–502. doi: 10.1016/j.survophthal.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Inatomi T, Nakamura T, Koizumi N, et al. Midterm results on ocular surface reconstruction using cultivated autologous oral mucosal epithelial transplantation. Am J Ophthalmol. 2006;141:267–275. doi: 10.1016/j.ajo.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 12.Meyer-Blazejewska CM, Yamanaka O, Liu H, et al. From hair to cornea: Toward the therapeutic use of hair follicle-derived stem cells in the treatment of limbal stem cell deficiency. Stem Cells. 2011;29:57–66. doi: 10.1002/stem.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reza HM, Ng BY, Gimeno FL, et al. Umbilical cord lining stem cells as a novel and promising source for ocular surface regeneration. Stem Cell Rev. 2011;7:935–947. doi: 10.1007/s12015-011-9245-7. [DOI] [PubMed] [Google Scholar]
- 14.Gomes JA, Geraldes Monteiro B, Melo GB, et al. Corneal reconstruction with tissue-engineered cell sheets composed of human immature dental pulp stem cells. Invest Ophthalmol Vis Sci. 2010;51:1408–1414. doi: 10.1167/iovs.09-4029. [DOI] [PubMed] [Google Scholar]
- 15.Ma Y, Xu Y, Xiao Z, et al. Reconstruction of chemically burned rat corneal surface by bone marrow-derived human mesenchymal stem cells. Stem Cells. 2006;24:315–321. doi: 10.1634/stemcells.2005-0046. [DOI] [PubMed] [Google Scholar]
- 16.Oh JY, Kim MK, Shin MS, et al. The anti-inflammatory and anti-angiogenic role of mesenchymal stem cells in corneal wound healing following chemical injury. Stem Cells. 2008;26:1047–1055. doi: 10.1634/stemcells.2007-0737. [DOI] [PubMed] [Google Scholar]
- 17.Yao L, Li ZR, Su WR, et al. Role of mesenchymal stem cells on cornea wound healing induced by acute alkali burn. PLoS One. 2012;7:e30842. doi: 10.1371/journal.pone.0030842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang TS, Cai L, Ji WY, et al. Reconstruction of the corneal epithelium with induced marrow mesenchymal stem cells in rats. Mol Vis. 2010;16:1304–1316. [PMC free article] [PubMed] [Google Scholar]
- 19.Lan Y, Kodati S, Lee HS, et al. Kinetics and function of mesenchymal stem cells in corneal injury. Invest Ophthalmol Vis Sci. 2012;53:3638–3644. doi: 10.1167/iovs.11-9311. [DOI] [PubMed] [Google Scholar]
- 20.Roddy GW, Lee RH, Bartosh TJ, et al. Action at a distance: Systemically administered adult stem/progenitor cells (MSCs) reduce inflammatory damage to the cornea without engraftment and primarily by secretion of TNF-a stimulated gene/protein 6. Stem Cells. 2011;29:1572–1579. doi: 10.1002/stem.708. [DOI] [PubMed] [Google Scholar]
- 21.Oh JY, Roddy GW, Choi H, et al. Anti-inflammatory protein TSG-6 reduces inflammatory damage to the cornea following chemical and mechanical injury. Proc Natl Acad Sci U S A. 2010;107:16875–16880. doi: 10.1073/pnas.1012451107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Arora R, Mehta D, Jain V. Amniotic membrane transplantation in acute chemical burns. Eye (Lond) 2004;19:273–278. doi: 10.1038/sj.eye.6701490. [DOI] [PubMed] [Google Scholar]
- 23.Hao Y, Ma D, Hwang D, et al. Identification of antiangiogenic and anti-inflammatory proteins in human amniotic membrane. Cornea. 2000;19:348–352. doi: 10.1097/00003226-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Koizumi N, Cooper LJ, Fullwood NJ, et al. An evaluation of cultivated corneal limbal epithelial cells, using cell-suspension culture. Invest Ophthalmol Vis Sci. 2002;43:2114–2121. [PubMed] [Google Scholar]
- 25.Pratoomsoot C, Taniok H, Hori K, et al. A thermoreversible hydrogel as a biosynthetic bandage for corneal wound repair. Biomaterials. 2008;29:272–281. doi: 10.1016/j.biomaterials.2007.09.031. [DOI] [PubMed] [Google Scholar]
- 26.Deshpande P, Notara M, Bullett N, et al. Development of a surface-modified contact lens for the transfer of cultured limbal epithelial cells to the cornea for ocular surface diseases. Tissue Engl Part A. 2009;15:2889–2902. doi: 10.1089/ten.tea.2008.0528. [DOI] [PubMed] [Google Scholar]
- 27.Di Girolamo N, Chui J, Wakefield D, et al. Cultured human ocular surface epithelium on therapeutic contact lenses. Br J Ophthalmol. 2007;91:459–464. doi: 10.1136/bjo.2006.103895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dravida S, Gaddipati S, Griffith M, et al. A biomimetic scaffold for culturing limbal stem cells: A promising alternative for clinical transplantation. J Tissue Eng Regen Med. 2008;2:263–271. doi: 10.1002/term.91. [DOI] [PubMed] [Google Scholar]
- 29.Deshpande P, McKean R, Blackwood K, et al. Using poly (lactide-co-glycolide) electrospun scaffolds to deliver cultured epithelial cells to the cornea. Regen Med. 2010;5:395–401. doi: 10.2217/rme.10.16. [DOI] [PubMed] [Google Scholar]
- 30.Nishida K, Yamato M, Hayashida Y, et al. Corneal reconstruction with tissue-engineered cell sheets composed of autologous oral mucosal epithelium. N Engl J Med. 2004;351:1187–1196. doi: 10.1056/NEJMoa040455. [DOI] [PubMed] [Google Scholar]
- 31.Sudha B, Madhavan H, Sitalakshmi G, et al. Cultivation of human corneal limbal stem cells in Mebiol gel®—A thermo-reversible gelation polymer. Indian J Med Res. 2006;124:655–664. [PubMed] [Google Scholar]
- 32.Yu G, Floyd ZE, Wu X, et al. Isolation of human adipose-derived stem cells from lipoaspirates. Methods Mol Biol. 2011;702:17–27. doi: 10.1007/978-1-61737-960-4_2. [DOI] [PubMed] [Google Scholar]
- 33.Roth N. Relationship between corneal radius of curvature and age in rabbits. Br Vet J. 1969;125:560. doi: 10.1016/s0007-1935(17)48658-1. [DOI] [PubMed] [Google Scholar]
- 34.Luengo Gimeno F, Lavigne V, Gatto S, et al. Advances in corneal stem-cell transplantation in rabbits with severe ocular alkali burns. J Cataract Refract Surg. 2007;33:1958–1965. doi: 10.1016/j.jcrs.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 35.Martínez-Conesa EM, Espel E, Reina M, et al. Characterization of ocular surface epithelial and progenitor cell markers in human adipose stromal cells derived from lipoaspirates. Invest Ophthalmol Vis Sci. 2012;53:513–520. doi: 10.1167/iovs.11-7550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arnalich-Montiel F, Pastor S, Blazquez-Martinez A, et al. Adipose-derived stem cells are a source for cell therapy of the corneal stroma. Stem Cells. 2008;26:570–579. doi: 10.1634/stemcells.2007-0653. [DOI] [PubMed] [Google Scholar]
- 37.Nieto-Miguel T, Galindo S, Reinoso R, et al. In vitro simulation of corneal epithelium microenvironment induces a corneal epithelial-like cell phenotype from human adipose tissue mesenchymal stem cells. Curr Eye Res. 2013;38:933–944. doi: 10.3109/02713683.2013.802809. [DOI] [PubMed] [Google Scholar]
- 38.De Ugarte DA, Morizono K, Elbarbary A, et al. Comparison of multi-lineage cells from human adipose tissue and bone marrow. Cells Tissues Organs. 2003;174:101–109. doi: 10.1159/000071150. [DOI] [PubMed] [Google Scholar]
- 39.Puissant B, Barreau C, Bourin P, et al. Immunomodulatory effect of human adipose tissue-derived adult stem cells: Comparison with bone marrow mesenchymal stem cells. Br J Haematol. 2005;129:118–129. doi: 10.1111/j.1365-2141.2005.05409.x. [DOI] [PubMed] [Google Scholar]
- 40.Tse WT, Pendleton JD, Beyer WM, et al. Suppression of allogeneic T-cell proliferation by human marrow stromal cells: Implications in transplantation. Transplantation. 2003;75:389–397. doi: 10.1097/01.TP.0000045055.63901.A9. [DOI] [PubMed] [Google Scholar]
- 41.Van der Worp E. A Guide to scleral lens Fitting [monograph online] Scleral Lens Education Society; 2010. [February 12, 2014]. Available at: http://commons.pacificu.edu/mono/4/. [Google Scholar]
- 42.Zeppieri M, Salvetat ML, Beltrami AP, et al. Human adipose-derived stem cells for the treatment of chemically burned rat cornea: Preliminary results. Curr Eye Res. 2013;38:451–463. doi: 10.3109/02713683.2012.763100. [DOI] [PubMed] [Google Scholar]
- 43.Lin HF, Lai YC, Tai CF, et al. Effects of cultured human adipose-derived stem cells transplantation on rabbit cornea regeneration after alkaline chemical burn. Kaohsiung J Med Sci. 2013;29:14–18. doi: 10.1016/j.kjms.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]