Summary
Background
Pakistan has one of the highest levels of child and maternal undernutrition worldwide, but little information about geographical and socioeconomic inequalities is available. We aimed to analyse anthropometric indicators for childhood and maternal nutrition at a district level in Pakistan and assess the association of nutritional status with food security and maternal and household socioeconomic factors.
Methods
We used data from the 2011 Pakistan National Nutrition Survey, which included anthropometric measurements for 33 638 children younger than 5 years and 24 826 women of childbearing age. We estimated the prevalences of stunting, wasting, and underweight among children and of underweight, overweight, and obesity in women for all 143 districts of Pakistan using a Bayesian spatial technique. We used a mixed-effect linear model to analyse the association of nutritional status with individual and household sociodemographic factors and food security.
Findings
Stunting prevalence in Pakistan's districts ranged between 22% (95% credible interval 19–26) and 76% (69–83); the lowest figures for wasting and underweight were both less than 2·5% and the highest were 42% (34–50) for wasting and 54% (49–59) for underweight. In 106 districts, more women were overweight than were underweight; in 49 of these districts more women were obese than were underweight. Children were better nourished if their mothers were taller or had higher weight, if they lived in wealthier households, and if their mothers had 10 or more years of education. Severe food insecurity was associated with worse nutritional outcomes for both children and women.
Interpretation
We noted large social and geographical inequalities in child and maternal nutrition in Pakistan, masked by national and provincial averages. Pakistan is also beginning to face the concurrent challenge of high burden of childhood undernutrition and overweight and obesity among women of reproductive age. Planning, implementation, and evaluation of programmes for food and nutrition should be based on district-level needs and outcomes.
Funding
Bill & Melinda Gates Foundation, Grand Challenges Canada, UK Medical Research Council.
Introduction
The effect of maternal and early childhood nutrition on children's health and development, and on their long-term health and economic productivity, is well established.1, 2, 3, 4 Although child nutrition has improved globally, the prevalence of stunting and underweight remains high in sub-Saharan Africa and south Asia.5 At the same time, body-mass index (BMI) and obesity have increased among women in most regions.6, 7
Data for child and maternal nutrition have been reported at the national level for all low-income and middle-income countries5 but little information about subnational status and within-country inequalities is available. Some studies have analysed urban–rural differentials in child and maternal nutritional status or inequalities related to quintiles of socioeconomic status.2, 8, 9, 10, 11, 12, 13, 14 Geographically, results are often reported at the national and in rare occasions at the province level,15, 16, 17 with few or no studies providing robust assessment at finer spatial scale (as has been attempted for child mortality and morbidity and for environmental risks in some countries).18, 19, 20, 21, 22 National analyses, although useful for advocacy, have little programmatic value because they mask the fine geographical variations that are needed for targeted interventions in devolved food and health systems, and for measurement of geographical inequalities.
With a population of more than 180 million people, Pakistan is at present the sixth largest country in the world and is projected to be the fourth largest by 2050, according to estimates by the UN.23 Despite a reported annual growth of 4·4% in gross domestic product, 13% of the population lives under the poverty line of US$1·25 per day.24 Although high infant and child mortality (85·5 deaths per 1000 livebirths in 2013) and poor nutritional status in Pakistan have been reported,15 the information has so far been available only at the national or provincial level.25, 26 There are no reliable data about nutrition indicators at district level, despite large variations in the economic status of districts.15 With devolution of health and preventive services to provinces and local governments at the district level,27 such information is imperative for planning and action. We aimed to assess anthropometric indicators of child and maternal nutrition at the district level and in relation to socioeconomic variables, to understand the full extent of geographical and social inequalities. We also used survey data about maternal education, household wealth, and food security to better understand the social determinants of nutritional status.28
Methods
Study design and participants
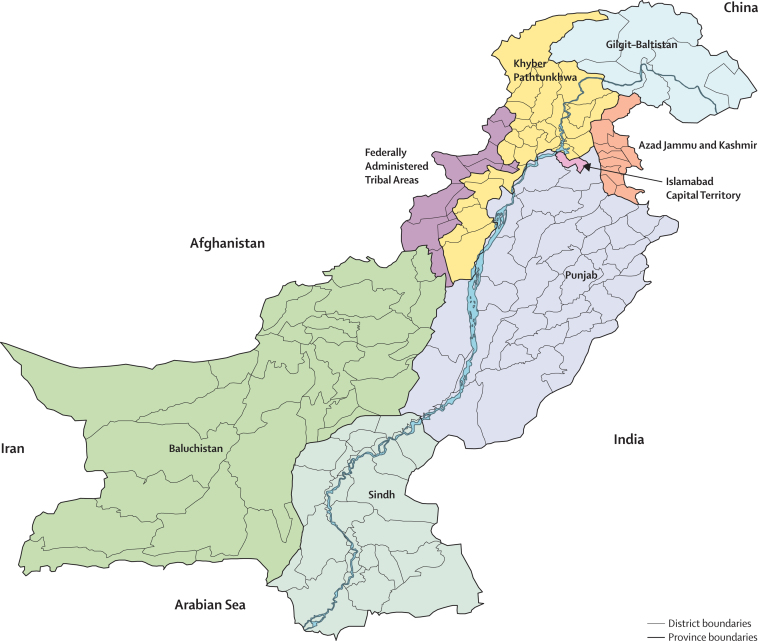
In this study we used data from the National Nutritional Survey (NNS) of Pakistan, 2011. The NNS applied multistage systematic clustered sampling to create a representative sample of the rural and urban populations of Pakistan as a whole, and its four main provinces (Balochistan, Khyber Pakhtunkhwa, Punjab, and Sindh), plus the administrative units of Gilgit Baltistan and the Federally Administered Tribal Areas (figure 1, appendix). Done between January and July, 2011, the NNS had a 93% consent rate, leading to a sample of children younger than 5 years and women of childbearing age in 27 963 households. The sample included 20 405 mother–child pairs using the youngest child in the household (referred to as the index child), 132 unpaired children (mother not selected because they were working or not available at home for other reasons), 4289 women without children younger than 5 years, and 3137 households without a woman of childbearing age or a child younger than 5 years. All other children aged 6–59 months (n=13 102) in the same households were also enrolled irrespective of whether they were siblings of the index child or not. Of the NNS households, 16 467 (59%) were rural and 11 496 (41%) urban. Data were missing in four districts (Kharan, Washuk, Ziarat, and the Frontier Region Bannu) because they could not be accessed during the survey period for reasons of insecurity.
Figure 1.
Map of Pakistan
The NNS included a questionnaire, answered by adult women, and physical measurements of weight, height, and selected biomarkers of disease and nutritional status. For this analysis we focused on anthropometric measurements of children and women of childbearing age. For children, we analysed height-for-age Z score (HAZ), weight-for-age Z score (WAZ), and weight-for-height Z score (WHZ); for women we analysed height and BMI. We calculated HAZ, WAZ, and WHZ using the 2006 WHO child growth standards.29 A plausibility criteria of −6 to 6 SD from the median of the reference population has been used for WAZ and WHZ, and −7 to 7 SD from the median of the reference population for HAZ. We defined stunting as HAZ more than 2 SD below the median of the reference population, underweight as WAZ more than 2 SD below the median, wasting as WHZ more than 2 SD below the median, and overweight as WHZ more than 2 SD above the median. We defined underweight for adult women as having a BMI of less than 18·5 kg/m2 and obesity has having a BMI of 30 kg/m2 or higher; we categorised normal weight and overweight individuals (BMI between 18·5 kg/m2 and 30 kg/m2) together to simplify presentation.
Statistical analysis
We report the association of children's and women's anthropometric indicators with deciles of household economic status and, for index children, with levels of mother's education. Following previous analyses of household data in low-income and middle-income countries,8, 30 we measured household economic status using principal component analysis of housing characteristics (eg, roof and wall materials, and number of rooms) and ownership of durable assets. We divided mothers' education into four categories: no schooling, 1–5 years of schooling, 6–9 years of schooling, and 10 or more years of schooling. We assessed food access insecurity following the United States Department of Agriculture guide based on a set of 11 questions covering household conditions, experiences, and behaviours related to food availability and affordability.31 On the basis of these questions, we divided households into four categories: food secure, food insecure without hunger, food insecure with hunger (moderate), and food insecure with hunger (severe).
To analyse geographical inequalities, we estimated prevalences of stunting, underweight, wasting, and overweight (for children) and of underweight, normal and overweight, and obesity (for women) for all 143 districts in Pakistan. To avoid unstable estimates due to the relatively small number of measurements in each district, we used a Bayesian spatial model with covariates. In the Bayesian spatial model, the estimated prevalence in each district is affected by its own data, as well as by those of its neighbours. The extent to which neighbours affect one another depends on how stable or uncertain the estimated effects in each district are, and on the empirical similarity among neighbouring districts. We used the Besag, York, and Mollie model in which cross-district variance is empirically partitioned into a spatial component, specified with a conditional autoregressive prior, and a component that does not have a spatial pattern, specified using a normal distribution.32, 33 The model also borrows strength through predictive covariates, including province, percentage of district population living in urban areas, average household economic status and food security scores in the district, and proportion of women who were illiterate. We accounted for complex survey design and post-stratification sample weights when calculating prevalences.
We also analysed crude and multivariable-adjusted associations of anthropometric status with its individual and household determinants. For children, these determinants included the child's age and sex; mother's education, height, and BMI; household wealth index, food security, water, sanitation, and type of fuel used for cooking; and rural versus urban place of residence. For women, we analysed associations with education; household economic status, food security, access to clean water, access to sanitation, and type of fuel used for cooking; and rural versus urban place of residence. To account for unmeasured factors that might affect the nutritional status of children and women we used a mixed-effects model, with random intercept at the primary-sampling-unit level, as done in previous analyses of associations using data from complex survey designs;34 we also adjusted all analyses for sample weights. These features of the regression model also account for the complex survey design.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, interpretation of the data, or in the writing of the report. The corresponding author had full access to data and the final responsibility to submit for publication.
Results
Table 1 shows descriptive statistics for the main variables. Child HAZ and WAZ and maternal height and BMI rose, and stunting and underweight declined, fairly steadily with household wealth and maternal education (figure 2). For example, whereas in the wealthiest 10% of the sample mean HAZ was −1·01 (95% CI −1·07 to 0·94) and prevalence of stunting was 24% (23 to 26), the children in the poorest households had mean HAZ of −2·13 (−2·20 to −2·06), with 56% (55 to 58) stunted. Similarly, women's average BMI ranged from 20·6 kg/m2 (95% CI 20·5 to 20·8) in the poorest decile to 26·5 kg/m2 (26·3 to 26·8) in the wealthiest. The socioeconomic associations of WHZ and wasting were less consistent, possibly because short-term weight loss and wasting have more complex or heterogeneous determinants.5
Table 1.
Descriptive statistics for main variables in the analysis
| Mean (SD) | Minimum | Maximum | |
|---|---|---|---|
| Child's age (months) | 30·1 (16·7) | 0 | 59 |
| Woman's age (years) | 31·0 (6·6) | 15 | 49 |
| Height-for-age Z score | −1·7 (1·9) | −7 | 6 |
| Weight-for-age Z score | −1·3 (1·4) | −6 | 6 |
| Weight-for-height Z score | −0·5 (1·7) | −6 | 6 |
| Body-mass index, kg/m2 | 23·5 (5·0) | 11 | 53 |
| Height, cm | 154·9 (6·3) | 82 | 199 |
Figure 2.
Child and maternal anthropometric indicators
(A) Indicators by deciles for household economic status. (B) Indicators by categories for maternal education. Prevalence refers to the proportion of individuals with HAZ more than 2 SD below median for stunting, WAZ more than 2 SD below median for underweight, WHZ more than 2 SD below median for wasting, and BMI less than 18·5 kg/m2 for underweight. HAZ=height-for-age Z score. WAZ=weight-for-age Z score. WHZ=weight-for-height Z score. BMI=body-mass index.
Geographically, households in Lahore and Mirpur were the wealthiest and those in Sherani and Tharparkar were the poorest (figure 3). The proportion of women who were illiterate ranged from less than 12% (95% credible interval [CrI] 7 to 16) to more than 95% (89 to 99), with half or more of women illiterate in 108 of 143 districts. Mirroring this finding, in only six districts did the proportion of women with 10 or more years of schooling surpass 40%, with no district exceeding 50%.
Figure 3.
Distribution of economic status and literacy
(A) Proportion of households in the two lowest quintiles of household economic status. (B) Proportion of women by district who are illiterate. The figures show posterior prevalences from a Bayesian spatial model.
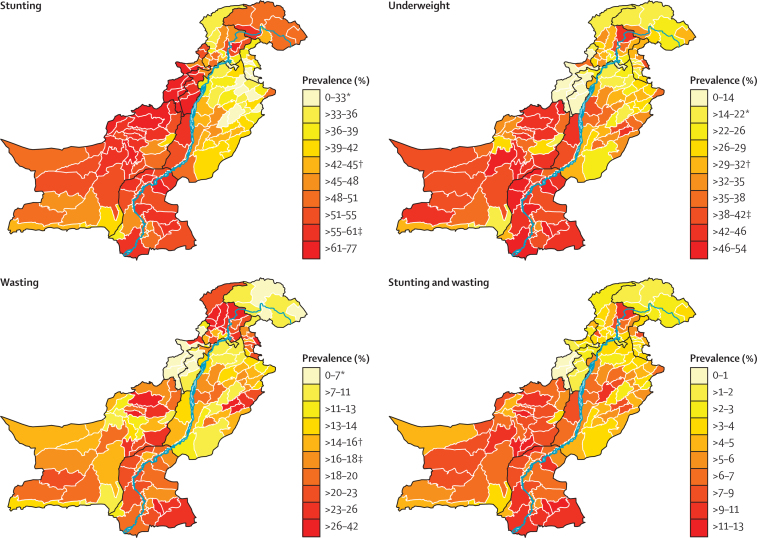
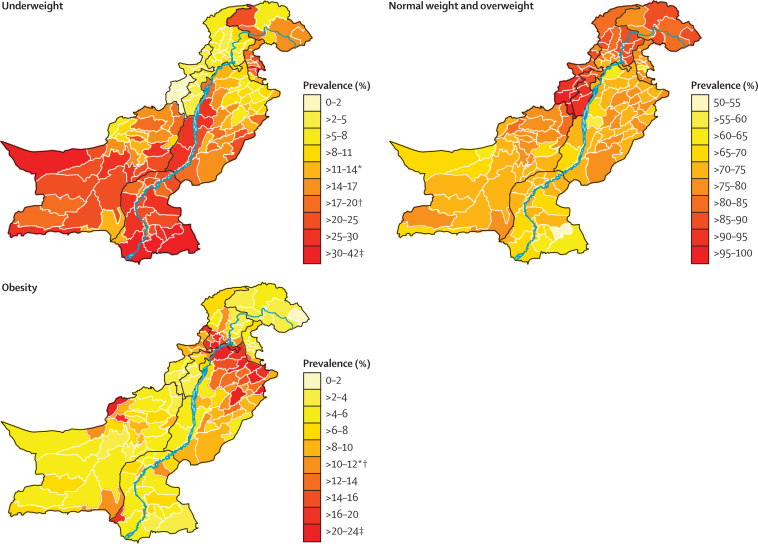
Stunting prevalence in Pakistan's districts ranged from about 22% (95% CrI 19 to 26) in affluent Islamabad to more than three-quarters in some districts near the Afghan border (figure 4); wasting and underweight prevalences were each less than 2·5% in a handful of districts but reached as high as 42% (34 to 50) and 54% (49 to 59), respectively, in a few districts. The prevalence of children who had both long-term and short-term nutritional deficits (ie, were both stunted and wasted), and hence affected by substantially higher risk of disease and death,35 ranged between less than 1% (95% CrI 0·1 to 2) and more than 12% (6 to 21). At a national level the joint occurrence of stunting and wasting was 5%, almost 2 percentage points less than would be expected if these exposures were independent. Prevalence of child overweight ranged from less than 2% to 80% (95% CrI 71 to 89%; figure 5). Similarly, the proportion of women who were underweight ranged from less than 2% to more than a third. Although many districts were affected by high prevalence of maternal underweight, obesity prevalence among women was 20% or more in eight districts. In 106 districts, more women were overweight than were underweight; in 49 of these districts, more women were obese than were underweight (figure 6).
Figure 4.
Prevalence of stunting, underweight, wasting, and stunting-plus-wasting among children younger than 5 years
Prevalences were estimated with a Bayesian spatial model with covariates. *Average prevalence of all developing countries in 2011. †Pakistan national prevalence in 2011. ‡Highest national prevalence all developing countries in 2011.
Figure 5.
Prevalence of overweight among children younger than 5 years
The district-level prevalences were estimated using a Bayesian spatial model with covariates.
Figure 6.
Prevalence of underweight, normal weight and overweight, and obesity among women of childbearing age
The prevalences were estimated with a Bayesian spatial model with covariates. *Average prevalence of all developing countries in 2011. †Pakistan national prevalence in 2011. ‡Highest national prevalence in all developing countries in 2011.
Consistent with analyses of surveys in different countries,36 child HAZ fell sharply with age up to 24 months, although we noted a less pronounced association for WAZ. Maternal BMI was positively associated with age, although the association flattened at about 40–45 years of age (appendix). In addition to the well known association with age,36 children's nutritional status was associated with mother's education and household economic, environmental, and food characteristics in crude (unadjusted) analyses (table 2, appendix).
Table 2.
Crude and adjusted associations between anthropometric status of children and their individual and household determinants
|
HAZ |
WAZ |
WHZ |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Crude |
Multivariable-adjusted* |
Crude |
Multivariable-adjusted* |
Crude |
Multivariable-adjusted* |
||||||||
| Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | ||
| Mother's education | |||||||||||||
| Illiterate | 0 | NA | 0 | NA | 0 | NA | 0 | NA | 0 | NA | 0 | NA | |
| 1–5 years of schooling | 0·19 (0·09 to 0·29) | 0·0002 | 0·06 (−0·04 to 0·15) | 0·24 | 0·11 (0·03 to 0·19) | 0·004 | 0 (−0·07 to 0·08) | 0·99 | −0·01 (−0·1 to 0·09) | 0·89 | −0·05 (−0·15 to 0·04) | 0·26 | |
| 6–9 years of schooling | 0·29 (0·18 to 0·41) | <0·0001 | 0·04 (−0·07 to 0·15) | 0·49 | 0·23 (0·14 to 0·32) | <0·0001 | 0·04 (−0·05 to 0·13) | 0·34 | 0·09 (−0·02 to 0·2) | 0·10 | 0·02 (−0·09 to 0·13) | 0·71 | |
| ≥10 years of schooling | 0·69 (0·60 to 0·78) | <0·0001 | 0·28 (0·18 to 0·38) | <0·0001 | 0·5 (0·43 to 0·57) | <0·0001 | 0·17 (0·10 to 0·25) | <0·0001 | 0·15 (0·06 to 0·24) | 0·0008 | 0·02 (−0·08 to 0·12) | 0·74 | |
| Mother's height | 0·05 (0·05 to 0·06) | <0·0001 | 0·05 (0·04 to 0·05) | <0·0001 | 0·03 (0·03 to 0·04) | <0·0001 | 0·03 (0·03 to 0·04) | <0·0001 | 0·01 (0 to 0·01) | 0·02 | 0·01 (0 to 0·01) | 0·03 | |
| Mother's BMI | 0·02 (0·01 to 0·03) | <0·0001 | 0·02 (0·01 to 0·03) | <0·0001 | 0·04 (0·04 to 0·05) | <0·0001 | 0·04 (0·03 to 0·04) | <0·0001 | 0·04 (0·04 to 0·05) | <0·0001 | 0·04 (0·03 to 0·04) | <0·0001 | |
| Wealth index | 0·34 (0·30 to 0·38) | <0·0001 | 0·16 (0·11 to 0·20) | <0·0001 | 0·29 (0·26 to 0·32) | <0·0001 | 0·13 (0·09 to 0·17) | <0·0001 | 0·13 (0·09 to 0·17) | <0·0001 | 0·06 (0·01 to 0·11) | 0·01 | |
| Food security | |||||||||||||
| Food secure | 0 | NA | 0 | NA | 0 | NA | 0 | NA | 0 | NA | 0 | NA | |
| Food insecure without hunger | −0·29 (−0·37 to −0·21) | <0·0001 | −0·09 (−0·17 to −0·01) | 0·03 | −0·26 (−0·32 to −0·20) | <0·0001 | −0·1 (−0·16 to −0·04) | 0·002 | −0·1 (−0·18 to −0·03) | 0·08 | −0·04 (−0·12 to 0·04) | 0·28 | |
| Food insecure with hunger—moderate | −0·49 (−0·58 to −0·40) | <0·0001 | −0·16 (−0·26 to −0·07) | 0·0005 | −0·43 (−0·49 to −0·36) | <0·0001 | −0·16 (−0·23 to −0·08) | <0·0001 | −0·18 (−0·27 to −0·10) | <0·0001 | −0·06 (−0·16 to 0·03) | 0·17 | |
| Food insecure with hunger—severe | −0·55 (−0·66 to −0·43) | <0·0001 | −0·15 (−0·27 to −0·03) | 0·01 | −0·59 (−0·68 to −0·50) | <0·0001 | −0·28 (−0·37 to −0·18) | <0·0001 | −0·31 (−0·42 to −0·20) | <0·0001 | −0·18 (−0·3 to −0·06) | 0·003 | |
Estimations adjusted for place of residence, type of fuel, water source, sanitation, child's age, and child's sex.
In the multivariable-adjusted analysis, some of these associations became statistically non-significant, especially for WHZ (which was only positively associated with maternal BMI and economic status, and was significantly decreased in children in households with severe food insecurity, but not other levels of food insecurity). After adjustment, household assets and mother's anthropometric status were associated with increased height and weight whereas being food insecure led to worse outcomes with a dose–response association. Only the highest category of maternal education was associated with children being tall or heavy for their age. Food insecurity was also significantly associated with being short and having low BMI in adult women; the adjusted effect on height was only about 1 cm in the households with severe food insecurity; that of BMI was about 0·6 kg/m2. Women in wealthy households were taller and heavier than women in poor households. Women in rural areas were, perhaps surprisingly, taller but weighed less than their urban counterparts (table 3, appendix).
Table 3.
Crude and adjusted associations between anthropometric status of women and their individual and household determinants
|
Height |
BMI |
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Crude |
Multivariable-adjusted* |
Crude |
Multivariable-adjusted* |
||||||
| Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | Coefficient (95% CI) | p value | ||
| Mother's education | |||||||||
| Illiterate | 0 | NA | 0 | NA | 0 | NA | 0 | NA | |
| 1–5 years of schooling | 0·15 (−0·17 to 0·47) | 0·36 | −0·08 (−0·40 to 0·25) | 0·63 | 0·58 (0·34 to 0·83) | <0·0001 | −0·03 (−0·28 to 0·21) | 0·78 | |
| 6–9 years of schooling | 0·4 (0·03 to 0·78) | 0·03 | −0·01 (−0·40 to 0·37) | 0·94 | 0·92 (0·63 to 1·21) | <0·0001 | −0·08 (−0·37 to 0·20) | 0·57 | |
| ≥10 years of schooling | 1·16 (0·87 to 1·45) | <0·0001 | 0·43 (0·10 to 0·76) | 0·01 | 1·57 (1·34 to 1·79) | <0·0001 | −0·01 (−0·26 to 0·23) | 0·92 | |
| Wealth index | 0·77 (0·65 to 0·89) | <0·0001 | 0·61 (0·45 to 0·77) | <0·0001 | 1·31 (1·22 to 1·4) | <0·0001 | 0·77 (0·65 to 0·90) | <0·0001 | |
| Food security | |||||||||
| Food secure | 0 | NA | 0 | NA | 0 | NA | 0 | NA | |
| Food insecure without hunger | −0·95 (−1·21 to −0·69) | <0·0001 | −0·55 (−0·82 to −0·28) | <0·0001 | −0·63 (−0·83 to −0·44) | <0·0001 | −0·06 (−0·26 to 0·14) | 0·58 | |
| Food insecure with hunger—moderate | −1·54 (−1·82 to −1·25) | <0·0001 | −0·9 (−1·21 to −0·59) | <0·0001 | −1·44 (−1·66 to −1·22) | <0·0001 | −0·5 (−0·74 to −0·27) | <0·0001 | |
| Food insecure with hunger—severe | −1·71 (−2·08 to −1·33) | <0·0001 | −0·98 (−1·38 to −0·58) | <0·0001 | −1·71 (−2·00 to −1·43) | <0·0001 | −0·61 (−0·91 to −0·31) | 0·0001 | |
Estimations adjusted for place of residence, type of fuel, water quality, and sanitation. Full results are provided in the appendix.
Discussion
Pakistan's progress in child nutrition and health has been substantially slower than in other south Asian countries,15, 28, 37 with a fall in moderate and severe stunting from about 60% in 1985 to more than 40% in 2011. Our analysis shows major geographical and socioeconomic differentials in maternal and childhood undernutrition, beyond what could be the consequence of localised acute events such as floods.38 We noted large spatial variations in children's and women's nutritional status, with about 30 districts having prevalences of children's stunting and underweight well above the highest reported at the national level among developing countries5 and ten districts having a prevalence of underweight children as low as the best low-middle-income country.7 The most affected districts are in the south of the country and within the provinces of Baluchistan, Khyber Pakhtunkhwa, and Sindh, largely matching the known poverty patterns and district-specific multidimensional poverty indices.15 By contrast, our findings show that Punjab has less undernutrition among children than other regions, although it seems to have come at the cost of increased prevalence of overweight and obesity among adult women. A north–south gradient is evident, with the southern districts of Punjab resembling Sindh in socioeconomic and malnutrition indicators. The 6 kg/m2 difference in women's BMI between the worst-off and best-off deciles almost equals the difference in mean BMI between women in the USA and those in the Central African Republic.6 We also noted high prevalence of maternal wasting (ie, low BMI) in some of the poorest districts of Pakistan.
Our individual-level results underscore the close links between child undernutrition and maternal height and BMI, household economic status, and severe food insecurity. The NNS 2011 did not include information about prematurity and intrauterine growth retardation. However, the close individual-level and district-level correlation between child and maternal undernutrition, and the fact that almost half of all reported childhood stunting in Pakistan is already established by 6 months of age, suggests the possible existence of a vicious cycle of undernutrition and stunting across generations.
We noted high rates of food insecurity in various districts of Pakistan, although there was weak correlation between food security and socioeconomic status based on household assets. We also did not note improved nutritional status in agrarian irrigated districts in southern Punjab and Sindh provinces, which are more water secure than other rural areas (appendix), possibly due to the overriding effect of other social determinants. For example, by contrast with the provinces of northern Punjab and Khyber Pakhtunkhwah, where large-scale landholding has diminished, the southern regions are mostly feudally controlled with land used for planting of cotton and sugarcane, which do not contribute to household-level food security. In most of these areas, maternal education is low, early marriage is common, and fertility rates are high, which might contribute substantially to the vicious cycle of maternal and child undernutrition.
To our knowledge, this study is the first district-level analysis of nutrition and its key determinants in a low-income country based on a large survey and Bayesian spatial methods to obtain stable district-level estimates (panel). This approach balances between (overly) unstable within-district estimates and (overly) simplified aggregate national estimates, with the degree of smoothing driven by the data (appendix). Some limitations must, however, be recognised. These limitations include missing data in some of the conflict-affected regions, including the Federally-Administered Tribal Areas and parts of Baluchistan, and relatively smaller sample size for food security estimation compared with other determinants because questions were asked from a subset of households only. The relatively small and non-representative sample in FATA and adjoining districts could have affected childhood obesity estimates therein. Further, we did not have data about gestational age and birthweight of children in the study, which would have allowed more systematic analysis of mother–child nutritional linkages. These factors have been studied in smaller regional studies in Pakistan. For example, findings from a population-based study in rural Sindh showed high rates of maternal wasting and rates of low birthweight in excess of 40%.42 This link is important for child survival2, 43 and because being born small for gestational age contributes to almost a fifth of all stunting by 6 months of age,2 a potentially important consideration in Pakistan. We could not assess trends over time at the district level because previous nutrition surveys did not have the same rich geographical information as did the NNS 2011. We do not, however, believe that these limitations detract from the key policy implications of these findings and the imperative for action.
Panel. Research in context.
Systematic review
We searched PubMed on Dec 6, 2014, with the terms “spatial analysis” (as MeSH term and in title and abstract) and “child” (as MeSH term) and “malnutrition” or “health” (both as MeSH terms). One study presented spatial variation in levels of anaemia among children.39 A few others had analysed child nutritional status in a specific community, without presenting the geographical distribution for the whole country,40 or across provinces41 or countries.5 Some studies have analysed small-area-level variation in child mortality, morbidity, and environmental risks.18, 19, 20, 21, 22 No study has reported child nutritional status at small-area level—eg, at the district level—for an entire country.
Interpretation
We noted large variations in children's and women's nutritional status across Pakistan's districts, with about 30 districts having levels of child stunting and underweight well in excess of the highest prevalence in the world and 10 districts having prevalence of underweight among children as low as the best low-middle-income country. Despite the fairly high prevalence of maternal underweight, in almost two-thirds of the districts more women were overweight than were underweight. Our results show the need for local-level planning, implementation, and monitoring of nutritional status.
Our results also raise the need for future local-level tracking of nutritional status for monitoring and programme evaluation. In view of the host of household-level information gathering by the Lady Health Workers (Pakistan's community health workers44) and multiple indicator cluster sampling surveys (MICS), collection of such data is feasible without substantial additional costs and will provide policy-relevant information at regular intervals at the district level. The major importance of our results is their relevance to district level planning for nutrition, which has not happened to date. Although there is some recognition that national data can mask wide disparities, subprovincial differentials in nutrition have only recently risen to the fore after recent emergencies especially the floods of 2010 and 2011 and resultant population displacement. There is a misperception that these malnourished populations are exceptional, resulting from extreme events such as floods, earthquakes, and drought,38, 44 which is especially underscored by the recent focus on child mortality in the drought-affected district of Tharparkar.45, 46 Our findings suggest that such differentials in nutrition status among districts and subpopulations in Pakistan are widespread, and probably longstanding as suggested by data for height and stunting (both long-term outcomes). Therefore, although community management of acute malnutrition might be an appropriate short-term response, much more needs to be done to address maternal and child undernutrition at district level in the long term. Local programmes need promotion of social and economic empowerment and education of women—elements that could have been key to the success of similar and even poorer countries in the region.47, 48 Recent work into the political economy of nutrition in Pakistan also underscores the fact that, although nutrition has been the business of many agencies, no single department or ministry has ever taken responsibility for it or developed a truly multisectoral initiative.49 The consequences of not having a national nutrition policy are particularly felt with devolution of economic and social responsibilities to local policy makers. Reversal of this attitude would require innovative approaches, including linking of the Benazir Income Support Program (an unconditional cash transfer programme for women) with maternal health and nutrition and with adolescent nutrition and education.39 Social safety nets for poor families, such as the Zakat and Baitul-Maal programmes, should also include cash or food support to address both overt and hidden hunger.
Finally, the close association between maternal and child undernutrition in Pakistan underscores the need for wide and sustained investments to address social determinants and reproductive health in Pakistan. These measures include investments in education and empowerment of girls, and provision of opportunities for women for gainful employment and participation in national economy. Our analysis provides further granular evidence from districts in Pakistan that concerted action on nutrition sensitive and specific interventions is needed urgently.
Contributors
ME and ZAB conceived the study. MDC, ZB, and SBS managed survey data. MDC and ZB analysed data and prepared results. LF, MDC, and ME developed statistical approach. MDC, ZB, ZAB, and ME wrote the Article with input from all other coauthors. ME and ZAB oversaw the research.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Black RE, Allen LH, Bhutta ZA, for the Maternal and Child Undernutrition Study Group Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–260. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Victora CG, Walker SP, for the Maternal and Child Nutrition Study Group Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–451. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 3.Victora CG, Adair L, Fall C, for the Maternal and Child Undernutrition Study Group Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–357. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adair LS, Fall CH, Osmond C, for the COHORTS group Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. 2013;382:525–534. doi: 10.1016/S0140-6736(13)60103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stevens GA, Finucane MM, Paciorek CJ, for the Nutrition Impact Model Study Group (Child Growth) Trends in mild, moderate, and severe stunting and underweight, and progress towards MDG 1 in 141 developing countries: a systematic analysis of population representative data. Lancet. 2012;380:824–834. doi: 10.1016/S0140-6736(12)60647-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Finucane MM, Stevens GA, Cowan MJ, for the Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index) National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–567. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stevens GA, Singh GM, Lu Y. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012;10:22. doi: 10.1186/1478-7954-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gakidou E, Oza S, Vidal Fuertes C. Improving child survival through environmental and nutritional interventions: the importance of targeting interventions toward the poor. JAMA. 2007;298:1876–1887. doi: 10.1001/jama.298.16.1876. [DOI] [PubMed] [Google Scholar]
- 9.Monteiro CA, Benicio MH, Conde WL. Narrowing socioeconomic inequality in child stunting: the Brazilian experience, 1974–2007. Bull World Health Organ. 2010;88:305–311. doi: 10.2471/BLT.09.069195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Victora CG, Wagstaff A, Schellenberg JA, Gwatkin D, Claeson M, Habicht JP. Applying an equity lens to child health and mortality: more of the same is not enough. Lancet. 2003;362:233–241. doi: 10.1016/S0140-6736(03)13917-7. [DOI] [PubMed] [Google Scholar]
- 11.Fotso JC. Child health inequities in developing countries: differences across urban and rural areas. Int J Equity Health. 2006;5:9. doi: 10.1186/1475-9276-5-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pampel FC, Denney JT, Krueger PM. Obesity, SES, and economic development: a test of the reversal hypothesis. Soc Sci Med. 2012;74:1073–1081. doi: 10.1016/j.socscimed.2011.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes Relat Metab Disord. 2004;28:1181–1186. doi: 10.1038/sj.ijo.0802716. [DOI] [PubMed] [Google Scholar]
- 14.McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- 15.Bhutta ZA, Hafeez A, Rizvi A. Reproductive, maternal, newborn, and child health in Pakistan: challenges and opportunities. Lancet. 2013;381:2207–2218. doi: 10.1016/S0140-6736(12)61999-0. [DOI] [PubMed] [Google Scholar]
- 16.Pathak P, Singh A. In: Population, poverty and health: analytical approaches. Singh K, Yadav R, Pandey A, editors. Hindustan Publishing Corporation; New Delhi: 2008. Geographical variation in poverty and child malnutrition in India; pp. 183–206. [Google Scholar]
- 17.Stevens G, Dias RH, Thomas KJ. Characterizing the epidemiological transition in Mexico: national and subnational burden of diseases, injuries, and risk factors. PLoS Med. 2008;5:e125. doi: 10.1371/journal.pmed.0050125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barufi AM, Haddad E, Paez A. Infant mortality in Brazil, 1980–2000: a spatial panel data analysis. BMC Public Health. 2012;12:181. doi: 10.1186/1471-2458-12-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kazembe LN, Namangale JJ. A Bayesian multinomial model to analyse spatial patterns of childhood co-morbidity in Malawi. Eur J Epidemiol. 2007;22:545–556. doi: 10.1007/s10654-007-9145-y. [DOI] [PubMed] [Google Scholar]
- 20.Stevens GA, Dias RH, Ezzati M. The effects of 3 environmental risks on mortality disparities across Mexican communities. Proc Natl Acad Sci USA. 2008;105:16860–16865. doi: 10.1073/pnas.0808927105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ram U, Jha P, Ram F. Neonatal, 1–59 month, and under-5 mortality in 597 Indian districts, 2001 to 2012: estimates from national demographic and mortality surveys. Lancet Glob Health. 2013;1:e219–e226. doi: 10.1016/S2214-109X(13)70073-1. [DOI] [PubMed] [Google Scholar]
- 22.Dwyer-Lindgren L, Kakungu F, Hangoma P. Estimation of district-level under-5 mortality in Zambia using birth history data, 1980–2010. Spat Spatiotemporal Epidemiol. 2014;11:89–107. doi: 10.1016/j.sste.2014.09.002. [DOI] [PubMed] [Google Scholar]
- 23.UN Department of Economic and Social Affairs. Population Division . World population prospects: the 2012 revision, volume I: comprehensive tables ST/ESA/SER.A/336. United Nations; New York: 2013. [Google Scholar]
- 24.The World Bank, 2015. http://data.worldbank.org/country/pakistan (accessed Feb 23, 2015).
- 25.Pakistan Institute of Development Economics M-nLAKUaMCK . National nutrition survey 2001–2002. Planning Commission, Government of Pakistan and UNICEF; Islamabad: 2004. [Google Scholar]
- 26.National Nutrition Survey (NNS) 2011; Aga Khan University; Pakistan Medical Research Council. Nutrition Wing Cabinet Division; Government of Pakistan; United Nations Children's Fund Pakistan . Pakistan National Nutrition Survey. Aga Khan University; Pakistan: 2011. [Google Scholar]
- 27.Nishtar S, Boerma T, Amjad S. Pakistan's health system: performance and prospects after the 18th Constitutional Amendment. Lancet. 2013;381:2193–2206. doi: 10.1016/S0140-6736(13)60019-7. [DOI] [PubMed] [Google Scholar]
- 28.Bhutta ZA, Gazdar H, Haddad L. Seeing the unseen: breaking the logjam of undernutrition in Pakistan. Ids Bull-I Dev Stud. 2013;44:1–9. [Google Scholar]
- 29.WHO child growth standards : length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age : methods and development. World Health Organization, Department of Nutrition for Health and Development; Geneva: 2006. [Google Scholar]
- 30.Wagstaff A. Socioeconomic inequalities in child mortality: comparisons across nine developing countries. Bull World Health Organ. 2000;78:19–29. [PMC free article] [PubMed] [Google Scholar]
- 31.Bickel G, Nord M, Price C, Hamilton W, Cook J. Guide to measuring household food security, revised 2000. US Department of Agriculture, Food and Nutrition Service; Alexandria, VA: 2000. [Google Scholar]
- 32.Besag J, York J, Mollie A. Bayesian image-restoration, with 2 applications in spatial statistics. Ann I Stat Math. 1991;43:1–20. [Google Scholar]
- 33.Wakefield JC, Best NG, Waller L. In: Spatial epidemiology: methods and applications. Elliott P, Wakefield JC, Best NG, Briggs DJ, editors. Oxford University Press; Oxford: 2000. Bayesian approaches to disease mapping; pp. 104–127. [Google Scholar]
- 34.Farzadfar F, Murray CJ, Gakidou E. Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet. 2012;379:47–54. doi: 10.1016/S0140-6736(11)61349-4. [DOI] [PubMed] [Google Scholar]
- 35.McDonald CM, Olofin I, Flaxman S. The effect of multiple anthropometric deficits on child mortality: meta-analysis of individual data in 10 prospective studies from developing countries. Am J Clin Nutr. 2013;97:896–901. doi: 10.3945/ajcn.112.047639. [DOI] [PubMed] [Google Scholar]
- 36.Victora CG, de Onis M, Hallal PC, Blossner M, Shrimpton R. Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics. 2010;125:e473–e480. doi: 10.1542/peds.2009-1519. [DOI] [PubMed] [Google Scholar]
- 37.Bhutta ZA, Gupta I, de'Silva H. Maternal and child health: is South Asia ready for change? BMJ. 2004;328:816–819. doi: 10.1136/bmj.328.7443.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hossain SM, Talat M, Boyd E. Evaluation of nutrition surveys in flood affected areas of Pakistan: seeing the unseen. IDS Bull. 2013;44:10–20. [Google Scholar]
- 39.Soares Magalhaes RJ, Langa A, Pedro JM, Sousa-Figueiredo JC, Clements AC, Vaz Nery S. Role of malnutrition and parasite infections in the spatial variation in children's anaemia risk in northern Angola. Geospat Health. 2013;7:341–354. doi: 10.4081/gh.2013.91. [DOI] [PubMed] [Google Scholar]
- 40.Spray AL, Eddy B, Hipp JA, Iannotti L. Spatial analysis of undernutrition of children in leogane Commune, Haiti. Food Nutr Bull. 2013;34:444–461. doi: 10.1177/156482651303400410. [DOI] [PubMed] [Google Scholar]
- 41.Adekanmbi VT, Uthman OA, Mudasiru OM. Exploring variations in childhood stunting in Nigeria using league table, control chart and spatial analysis. BMC Pub Health. 2013;13:361. doi: 10.1186/1471-2458-13-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bhutta ZA, Rizvi A, Raza F. A comparative evaluation of multiple micronutrient and iron-folic acid supplementation during pregnancy in Pakistan: impact on pregnancy outcomes. Food Nutr Bull. 2009;30(4 suppl):S496–S505. doi: 10.1177/15648265090304S404. [DOI] [PubMed] [Google Scholar]
- 43.Katz J, Lee AC, Kozuki N, for the CHERG Small-for-Gestational-Age-Preterm Birth Working Group Mortality risk in preterm and small-for-gestational-age infants in low-income and middle-income countries: a pooled country analysis. Lancet. 2013;382:417–425. doi: 10.1016/S0140-6736(13)60993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ministry of Health GoP . PC—I document of National Programme for Family Planning & Primary Health Care (FP & PHC) Ministry of Health, Government of Pakistan; Islamabad: 2003. [Google Scholar]
- 45.Rana RS, Naim H. Tharparkar: a forgotten disaster. Lancet Glob Health. 2014;2:e508. doi: 10.1016/S2214-109X(14)70254-2. [DOI] [PubMed] [Google Scholar]
- 46.Dawn. High child mortality in Thar no new phenomenon: say experts. Dawn (Karachi), Nov 24, 2014.
- 47.Chowdhury AM, Bhuiya A, Chowdhury ME, Rasheed S, Hussain Z, Chen LC. The Bangladesh paradox: exceptional health achievement despite economic poverty. Lancet. 2013;382:1734–1745. doi: 10.1016/S0140-6736(13)62148-0. [DOI] [PubMed] [Google Scholar]
- 48.El Arifeen S, Christou A, Reichenbach L. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. Lancet. 2013;382:2012–2026. doi: 10.1016/S0140-6736(13)62149-2. [DOI] [PubMed] [Google Scholar]
- 49.Zaidi S, Mohmand SK, Hayat N, Acosta AM. Nutrition policy in the post-devolution context in Pakistan: an analysis of provincial opportunities and barriers. IDS Bull. 2013;44:86–93. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.