Abstract
BACKGROUND
School programs can be effective in modifying knowledge, attitudes, and habits relevant to long-term risk of chronic diseases associated with sedentary lifestyles. As part of a long-term research strategy, we conducted an educational intervention in preschool facilities to assess changes in preschoolers’ knowledge, attitudes, and habits toward healthy eating and living an active lifestyle.
METHODS
Using a cluster design, we randomly assigned 14 preschool facilities in Bogotá, Colombia to a 5-month educational and playful intervention (7 preschool facilities) or to usual curriculum (7 preschool facilities). A total of 1216 children aged 3–5 years, 928 parents, and 120 teachers participated. A structured survey was used at baseline, at the end of the study, and 12 months later to evaluate changes in knowledge, attitudes, and habits.
RESULTS
Children in the intervention group showed a 10.9% increase in weighted score, compared with 5.3% in controls. The absolute adjusted difference was 3.90 units (95% confidence interval [CI], 1.64–6.16; P <.001). Among parents, the equivalent statistics were 8.9% and 3.1%, respectively (absolute difference 4.08 units; 95% CI, 2.03 to 6.12; P <.001), and among teachers, 9.4% and 2.5%, respectively (absolute difference 5.36 units; 95% CI, −0.29–11.01; P = .06). In the intervened cohort 1 year after the intervention, children still showed a significant increase in weighted score (absolute difference of 6.38 units; P <.001).
CONCLUSIONS
A preschool-based intervention aimed at improving knowledge, attitudes, and habits related to healthy diet and active lifestyle is feasible, efficacious, and sustainable in very young children.
Keywords: Cardiovascular disease (CVD), Global health, Health education, Noncommunicable disease (NCD), Preschool children
Noncommunicable diseases are responsible for the majority of deaths throughout the world.1 According to the World Bank, 56% of all deaths in low- and middle-income countries may be attributed to noncommunicable diseases, mainly cardiovascular diseases,2 and by 2020, 80% of all deaths may be attributed to these diseases.3 The growing burden of these diseases stresses the need for population-based studies on effective strategies for their primary prevention in both developed and developing nations.
There is growing evidence that negative health behaviors initiated in childhood may persist through adulthood, leading to risk factors of cardiovascular disease and other chronic diseases.4,5 This represents an opportunity for primary prevention, particularly in low- and middle-income countries, where rapid changes are occurring in chronic disease-relevant behaviors.6 School and community programs that promote regular physical activity are recommended toward reducing the burden of chronic diseases associated with sedentary lifestyle and obesity.7–10
We therefore decided to design and implement a long-term pedagogic and communication research program aimed at developing and evaluating effective strategies for modifying knowledge, attitudes, and habits of preschool children and other stakeholders in Colombia.
Over a 5-month period, we assessed the impact on children’s knowledge, attitudes, and habits towards healthy eating and living an active lifestyle following a pre-school-based intervention. As secondary objectives, we evaluated parents’ and teachers’ knowledge, attitudes, and habits, changes in children’s nutritional status, and body mass index (BMI), the association between children’s BMI and knowledge, attitudes, and habits, and changes in knowledge, attitudes, and habits 12 months after the intervention ended.
METHODS
Study Design
We conducted a cluster, randomized controlled trial in 14 preschool facilities in Usaquén (Bogotá, Colombia) between May and November, 2009. Usaquén represents the different socioeconomic status levels seen in Colombia, and includes an underprivileged community with a high migration rate. Randomization occurred at the preschool facility level. We used a blinded randomization assignment schedule, concealed until treatments had been allocated. All children 3–5 years of age at baseline, and their parents and teachers, were eligible. We excluded children, parents, or teachers who had received formal training in healthy habits, nutrition, or physical activity in the 6 months before the study and children whose parents did not consent.
It was assumed that the improvement rate in knowledge, attitudes, and habits in the control group would be 5%. A total sample size of 1043 children was calculated based on being able to detect a doubling of the improvement rate under the intervention, with 80% power, a 2-sided 5% significance test, and 1:1 allocation. We estimated 10% losses to follow-up. Institutional review board approval was obtained from both the Mount Sinai School of Medicine and Fundación Cardioinfantil in Bogotá.
Study Intervention
Based on the knowledge that negative health behaviors initiated in childhood that persist through adulthood can be risk factors that predict chronic diseases,4,5 we designed an intervention based on social cognitive theory and the transtheoretical model in health promotion,11 which was incorporated in a ludic and pedagogical strategy teaching pre-school children key messages on the importance of healthy eating and living an active lifestyle in 3 integrated areas: body and heart, nutrition, and physical activity.
The intervened children were provided classroom educational and playful activities during 5 months, which included Sesame Workshop Healthy Habits story-books, posters, videos, games, and songs (1 hour daily); a “Healthy family day” workshop (1 hour); and weekly health notes. Parents participated in 3 workshops and weekly notes containing positive health messages about nutrition and active lifestyles to share with their children. Teachers also participated in 3 centralized training sessions, plus personalized working sessions with a research supervisor (2 hours every 15 days), and received a teacher’s guide (Appendix 1, online only). Meanwhile, the control preschool facilities continued with their usual pre-school curriculum. As part of a requirement of a local institutional review board, these preschool facilities were provided with a similar intervention of 8 months, after the initial 5-month study ended.
Study Measurements
We developed questionnaires to measure knowledge, attitudes, and habits on healthy eating and living an active lifestyle in children, parents, and teachers. A panel composed of experts in psychology, qualitative research, pediatrics, nutrition, child development, and education was convened to ensure face and content validity of the instruments, based on item identification and extraction from published and unpublished questionnaires.12,13
The surveys were pilot tested in groups of children 3–5 years old (n = 20), parents, and teachers (n = 20). The final children questionnaire contained 21 simple items (10 for knowledge, 6 for attitudes, and 5 for habits) and used age-and sex-appropriate photographs to frame each question. The parent and teacher questionnaire had 28 and 30 items, respectively (Appendix 2, online only).
Children’s, parents’, and teachers’ knowledge, attitudes, and habits were measured by a group of trained psychologists using a standardized protocol, blinded to intervention status. Study population was initially measured in May 2009, immediately before randomization and intervention allocation. The intervention was administered between June and October, 2009, and the second measurement was performed in November 2009 in all 14 preschool facilities. To assess long-term changes, the study population was again evaluated 12 months after the intervention ended.
Children’s height and weight were measured by nutritionists, using standard techniques.14 Nutritional status of children was assessed using the Centers for Disease Control and Prevention growth charts for age (in months) and sex for BMI,15 with children classified as malnourished if BMI is < −2 SD, risk of malnourished (−2 SD and < −1 SD), eutrophic (−1 SD and +1 SD), overweight (> +1 and +2 SD), and obese (> +2 SD). Socioeconomic status was measured with a tool used routinely by the Colombian government.16
Outcomes
The primary outcome was the mean change in children’s knowledge, attitudes, and habits related to healthy eating and living an active lifestyle. Secondary outcomes were the mean change in parents’ and teachers’ knowledge, attitudes, and habits about healthy eating and living an active lifestyle. Baseline and end-of-study scores were initially standardized to a scale of 0–100. Because we hypothesized that the mean change in knowledge scores associated with this short intervention period would be larger than the mean changes in scores due to attitudes and habits, we a priori gave differential weights (70, 20, and 10, respectively) to the scores to compose a standardized weighted total score. We also evaluated changes in children’s nutritional status and BMI, as well as the association between children’s BMI and knowledge, attitudes, and habits.
To explore the long-term impact of the intervention at 12 months after study completion, we evaluated the change in knowledge, attitudes, and habits scores and BMI in the intervened cohort. This analysis was performed on those subjects with complete data for all 3 measurements: baseline, 6, and 18 months. Similarly, we report results on the effects of the 8-month intervention in the initial control group.
Statistical Analysis
All analyses were performed according to a predefined statistical analysis plan and were based on the intention-to-treat principle. The primary analysis was conducted in those subjects with baseline and end-of-study scores. The analyses of results at 18 months were restricted to subjects with nonmissing data at all 3 measurements. The effect of the intervention was evaluated using generalized estimating equations models. Changes between baseline and end-of-study scores were modeled as the outcome, randomization assignment as the independent predictor variable of interest, and subject’s preschool facilities as the clustering variable. We also used generalized estimating equations models to assess interactions between variables, specifically children’s age and intervention, and to assess the association between a child’s BMI at baseline and their knowledge, attitudes, and habits regarding healthy eating and living an active lifestyle. We ran additional models simultaneously, adjusting by the effect of parents’ and teachers’ age, and children’s weight.
Chi-squared test was used for the analysis of categorical variables (nutritional status) and unpaired t-test for between-group comparisons of BMI.
RESULTS
The total study population comprised 1216 children 3–5 years of age at baseline, 135 teachers, and 928 parents (Figure 1). There were no significant differences between the 2 groups with respect to baseline characteristics (Tables 1, 2), except for modest differences in teachers’ educational level, age in parents and teachers, and children’s weight. One hundred (8.2%) children, 58 (6.3%) parents, and 15 (11.1%) teachers were lost to follow-up between baseline and 6-month measurements.
Figure 1.
Enrollment, randomization, and follow-up of study population.
*(PF) = preschool facilities.
Table 1.
Baseline Summary Statistics by Intervention Group
| Variable | Preschool Facility* Intervention Arm n (%) |
Preschool Facility Control Arm n (%) |
P-Value |
|---|---|---|---|
| Children | |||
| Number of children included | 622 (51.2) | 594 (48.9) | |
| Age (years) | .15 | ||
| 3 | 342 (55.0) | 309 (52.0) | |
| 4 | 270 (43.4) | 266 (44.8) | |
| 5 | 10 (1.6) | 19 (3.2) | |
| Socioeconomic status of the neighborhood where the preschool facility is located | .50 | ||
| 1–2 | 4 (57.1) | 5 (71.4) | |
| 3–4 | 3 (42.9) | 2 (28.6) | |
| Children’s sex | .65 | ||
| Girls | 296 (47.6) | 275 (46.3) | |
| Children’s nutritional status by BMI | <.01 | ||
| Risk of undernourished | 46 (8.2) | 60 (11.2) | |
| Undernourished | 25 (4.5) | 39 (7.3) | |
| Eutrophic | 358 (63.9) | 324 (60.2) | |
| Overweight | 115 (20.54) | 103 (19.14) | |
| Obese | 16 (2.9) | 12 (2.2) | |
| Parents or caregivers | |||
| Number of parents included | 493 (53.1) | 435 (46.9) | |
| Age mean (SD) | 31.25 (8.1) | 29.94 (6.8) | .01 |
| Female | 412 (83.6) | 373 (85.8) | .36 |
| Teachers | |||
| Number of teachers included | 64 (47.4) | 71 (52.6) | |
| Age Mean (SD) | 39.04 (10.6) | 35.05 (8.9) | .03 |
| Female | 55 (100) | 64 (98.5) | 1.0 |
| Schooling level of the teachers | <.001 | ||
| High school | 7 (12.7) | 1 (1.54) | |
| Technical training | 17 (30.9) | 46 (70.8) | |
| College/university | 30 (54.6) | 18 (27.7) | |
| Postgraduate | 1 (1.8) | 0 (0.0) | |
BMI = body mass index.
Table 2.
Further Baseline Summary Statistics by Intervention Group
| Variable | Preschool Facility Intervention Arm
|
Preschool Facility Control Arm
|
P-Value | ||
|---|---|---|---|---|---|
| n | Median (IQR) | n | Median (IQR) | ||
| Children | |||||
| Baseline total score | 488 | 64.1 (56.8–71.3) | 476 | 63.97 (57.0–69.8) | .39 |
| Baseline score on knowledge | 561 | 77.1 (65.7–88.6) | 538 | 77.1 (65.7–88.5) | .79 |
| Baseline score on attitudes | 591 | 50.0 (50.0–66.7) | 569 | 50.0 (50.0–66.7) | .65 |
| Baseline score on habits | 550 | 60.0 (40.0–70.0) | 533 | 60.0 (40.0–70.0) | .13 |
| Baseline weighted (70/20/10) score | 488 | 71.0 (63.6–79.3) | 476 | 71.3 (62.5–79.0) | .84 |
| Parents | |||||
| Total baseline score | 477 | 67.0 (61.4–73.1) | 422 | 67.4 (58.1–73.1) | .07 |
| Baseline score on knowledge | 485 | 70.0 (60.0–80.0) | 433 | 70.0 (60.0–80.0) | .07 |
| Baseline score on attitudes | 485 | 75.0 (66.0–82.1) | 429 | 73.2 (64.3–80.4) | .06 |
| Baseline score on habits | 492 | 62.5 (50.0–68.8) | 429 | 56.3 (43.8–68.8) | .28 |
| Baseline weighted (70/20/10) score | 477 | 69.1 (62.5–77.2) | 422 | 69.6 (60.2–76.7) | .11 |
| Teachers | |||||
| Total baseline score | 43 | 77.8 (69.2–84.2) | 43 | 73.9 (70.7–79.3) | .34 |
| Baseline score on knowledge | 49 | 80.0 (70.0–90.0) | 57 | 70.0 (70.0–80.0) | .39 |
| Baseline score on attitudes | 51 | 78.8 (73.2–89.2) | 58 | 80.4 (71.4–89.3) | .91 |
| Baseline score on habits | 50 | 75.0 (62.5–79.2) | 54 | 75.0 (62.5–79.1) | .88 |
| Baseline weighted (70/20/10) score | 43 | 76.6 (68.9–85.0) | 43 | 72.0 (68.4–79.9) | .19 |
IQR = interquartile range.
Primary Outcome
After adjustment for cluster, children’s sex, age, weight, and teacher’s educational level, children in the intervention group showed a larger mean increase in weighted score when compared with that of the control group (P <.001). The percent improvement rate in the intervention arm was 10.8% in weighted score, compared with 5.3% in controls (Table 3). We found a significant increase in the standardized change score for attitudes (P <.001) as compared with the control group, with no evidence of significant change in knowledge (P = .30) or habits (P = .16). There was no heterogeneity in adjusted weighted score change by children sex or age group; P = .78, and P = .77, respectively.
Table 3.
Change Score in Knowledge, Attitudes, and Habits by Study Group, Controlling for Cluster Effect, Sex, Age, Children’s Weight, and Teacher’s Educational Level after 5-Month Intervention
| Group | Within-group Differences
|
Difference (95% CI) | P-Value | |
|---|---|---|---|---|
| Intervention Arm n (Mean) |
Control Arm n (Mean) |
|||
| Children | ||||
| Knowledge | 503 (14.36) | 484 (12.35) | 2.01 (−1.72–5.74) | .29 |
| Attitudes | 539 (0.99) | 522 (−7.48) | 8.47 (4.79–12.14) | <.001 |
| Habits | 498 (−20.05) | 485 (−29) | 8.95 (−3.39–21.29) | .16 |
| Change in WTS | 433 (7.66) | 425 (3.76) | 3.90 (1.64–6.16) | <.001 |
| Change (%) | 10.9 | 5.4 | ||
| Parents | ||||
| Knowledge | 440 (6.44) | 396 (2.39) | 4.05 (1.64–6.46) | <.01 |
| Attitudes | 422 (5.52) | 382 (2.69) | 2.83 (1.20–4.47) | <.001 |
| Habits | 445 (6.98) | 393 (3.36) | 3.62 (−0.25–7.50) | .06 |
| Change in WTS | 402 (6.12) | 360 (2.04) | 4.08 (2.03–6.12) | <.001 |
| Change (%) | 8.9 | 3.1 | ||
| Teachers | ||||
| Knowledge | 46 (11.6) | 51 (5.71) | 5.89 (−0.51–12.30) | .07 |
| Attitudes | 48 (1.27) | 53 (−4.85) | 6.12 (1.38–10.86) | .01 |
| Habits | 45 (10.59) | 53 (5.31) | 5.28 (0.01–10.55) | .05 |
| Change in WTS | 37 (7.24) | 35 (1.88) | 5.36 (−0.29–11.01) | .06 |
| Change (%) | 9.5 | 2.5 | ||
CI = confidence interval; WTS = weighted total score.
Secondary Outcomes
After adjustment for cluster, sex, and teacher’s educational level, parents and teachers who received the intervention showed a larger mean increase in weighted score as compared with the control group. The difference was statistically significant in parents (difference 5.8%, P <.001) but not in teachers (difference 7.0%, P = .06) (Table 3). Intervened parents had significant increases in scores for knowledge (P = .001) and attitudes (P <.001) when compared with the control group, while the increase in habits did not reach the formal level of significance (P = .06) (Table 3). Intervened teachers increased the scores significantly for attitudes (P = .01) and habits (P = .05) when compared with the control group, with no evidence of significant changes in knowledge (P = .07).
Most of the children were eutrophic at baseline (692/ 1098; 62.11%) and in the second measurement (742/1097; 67.64%). BMI means and SDs in the intervention and control groups at baseline were 15.99 (0.09) and 15.77 (0.08), respectively, P = .09; and at 6 months, 16.57 (0.45) and 16.40 (0.49), respectively, P = .810. There were no significant differences between groups (P = .193). We did not find any association between children’s baseline BMI and their knowledge, attitudes, and habits change.
Follow-up of the Study Cohorts at 18 Months
There were 216 (38%) children, 214 (47%) parents, and 10 (18%) teachers lost to follow-up between the 6- and the 18-month measurements in the intervention cohort. In the control cohort there were 304 (56%) children, 263 (64%) parents, and 16 (25%) teachers lost to follow-up between the 6- and the 18-month additional measurements.
In both groups, attrition was mainly due to school change or migration associated with factors such as local violence or changing jobs. There were no significant differences associated with sex or weighted score change observed after the initial 5-month period between those lost to follow-up and those remaining in the study. In both cohorts, children lost to follow-up were older (3.7 and 3.3 years, P <.0001; and 3.8 and 3.1 years, P <.0001, respectively).
In the intervened cohort 1 year after its completion, children showed a significant increase in weighted score (absolute difference of 6.38 units, P <.001, Figure 2A). Parents and teachers maintained the scores seen after 5 months (Figure 2B, C). In the control cohort, there was a clear increase in the weighted score in children after they received the modified intervention (absolute difference of 10.3 units, P <.001), as well as in teachers (absolute difference 6.1, P = .001), but no increase was demonstrated in parents (0.61 units, P = .4). Most of the children were eutrophic at baseline, 6-month, and 18-month follow-ups (Figure 3). There were no significant differences in the BMI in the intervened group or the control group between the 6-and 18-month measurements (P = .2 and P = .5, respectively).
Figure 2.
Changes in knowledge, attitudes, and habits in children (A), parents (B), and teachers (C), over the 18-month study period.
Mean values correspond to the weighted total score (WTS). The WTS assumes differential weights to knowledge, attitudes, and habits (70, 20, 10, respectively).
*During this period of time, the initial control group received an 8-month intervention.
†Statistical significance of changes obtained between baseline and 6-month measurements.
‡Statistical significance of changes obtained between 6- and 18-month measurements.
§Population with data available for all 3 measurements.
Figure 3.
Distribution of children by nutritional status at baseline and 6-month and 18-month follow-ups.
BMI = body mass index.
DISCUSSION
In this randomized study, children of preschool age, parents, and teachers who received an intervention based on a unique program funded and implemented by a public-private partnership aimed at changing knowledge, attitudes, and habits related to healthy diet and active lifestyle, showed larger increases after 5 months in knowledge, attitudes, and habits scores when compared with a control cohort. Results in the intervened cohort were maintained or improved after 1 year. Additionally, comparable results were obtained after the initial control cohort received an 8-month intervention.
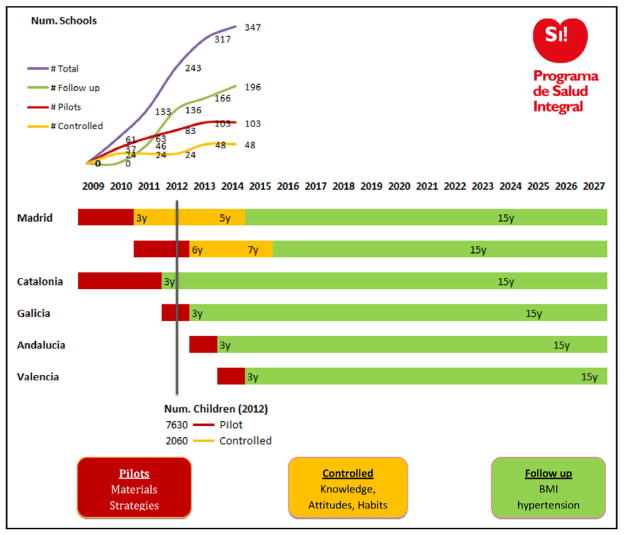
These results contribute to the evidence that well-designed interventions targeted to young children might be an effective first step toward reducing the risk of chronic disease later in life. To the best of our knowledge, our project in preschool children in Colombia is the first such study conducted in a low- and middle-income country, and represents the proof of principle for a research program aimed at developing effective preventive strategies targeted toward preschool and elementary school children in both Colombia and Spain. A similar program in Spain (Figure 4, online only) involves children aged 3 to 7 years at baseline in a large number of preschool facilities and primary schools in 5 regions of the country. Our study has strengths like the cluster randomized design, a large sample size, the concomitant evaluation of parents and teachers, the structured intervention, and the evaluation process where evaluators were not aware of the status of the preschool facilities. Similar to other studies,17,18,19 the education intervention incorporated the “fun while learning” concept into its various activities, increasing the children’s attention and motivation to learn.
Figure 4.
Program to prospectively evaluate the long-term knowledge, attitudes, and habits longitudinally in Spain.
BMI = body mass index.
As with other studies,20 our study was implemented in schools,17,21,22 involving different influencers around the child, using a strategy with multiple components, like the provision of information about the benefits and importance of health and active living;23,24 types of physical activity suitable for a particular age range; use of age-specific and enjoyable activities;25–27 availability of new materials for classes;25 and adaptable, flexible, and culturally sensitive activities based on socioeconomic status.26,27 The effectiveness of the intervention was related to the active participation of the entire educational community, who, motivated by a desire to improve health of preschool children, were a positive influence on their eating and physical activity habits.
Some studies have shown that 2-month interventions in children and adolescents are sufficient to improve nutrition knowledge.17,28,29 In contrast, our study observed a greater impact on children’s attitudes than on their knowledge and habits,17,30–32 with a concomitant improvement in the waste difference, which could be explained by the fact that the prior studies evaluated children over the age of 7 years (different neurodevelopmental stage).
Similar to the proportions of the 2010 National Nutritional Survey ENSIN 2010,33 at baseline, 2.55% of the study children were obese and 19.85% were overweight. After the intervention period, the proportion of eutrophic children increased in both groups, from 62.2% to 67.0% and from 60.8% to 64.6% in the intervened and control group, respectively. Although the differences were not statistically significant, these results are encouraging and raise the hypothesis that maintaining over a longer period some elements of the pedagogical strategy in the educational community, larger changes could be observed.
This study had some limitations that could affect our results. First, although the input of the teachers in the preschool facilities was obtained for the planning and overall inclusion of the intervention into the curriculum, their participation in the initial planning stage was minimal. It is conceivable that newer interventions that include their input from the start may show even larger changes in knowledge, attitudes, and habits over time.34,35 Second, the small number of teachers evaluated has limited the statistical power in this group. Third, while the measurement tool was developed in structured steps, formal psychometric properties are part of a study that is being currently implemented.
In conclusion, despite the relatively short duration of this intervention, results suggest that a preschool-based intervention aimed at changing knowledge, attitudes, and habits related to healthy diet and active lifestyle, is feasible, effective up to 1 year in very young children, parents, and teachers. Preschool programs are feasible, as they reach virtually all children at a relatively low cost with existing infrastructure. Further steps of our research program include an assessment of the intervention over a longer period of time, including anthropometric measurements and validated biomarkers of cardiovascular disease and metabolic syndromes, in addition to knowledge, attitudes, and habits, as well as a replication on a larger scale in preschool children in low- and middle-income countries as well as high-income countries (Spain).
CLINICAL SIGNIFICANCE.
Preschool-aged children undergoing this Healthy Habits intervention had a significant improvement in their cardiac well-being.
The study also saw a positive outcome of knowledge, attitudes, and habits on parents and teachers.
The intervention appears to have durability when evaluated 1 year later.
Acknowledgments
Funding: Santo Domingo Foundation.
Appendix 1 Study Intervention
| People | Activities (duration, frequency) |
|---|---|
| Teachers |
|
| Children |
|
| Parents |
|
Appendix 2 Surveys
| CHILDREN’S SURVEY
| |
|---|---|
| Question | Domain |
| KNOWLEDGE | |
| Body and heart | |
| 1 | Location of the heart |
| 2 | Heart changes with exercise |
| 3 | Understands what it means to be healthy |
| 4 | Recognizes what helps him/her be healthy |
| Nutrition | |
| 5 | Recognizes that eating fruits and vegetables every day helps him/her be healthy |
| 6 | Recognizes the foods that should be eaten once in a while |
| 7 | Recognizes that a varied diet helps him/her be healthy |
| Physical activity | |
| 8 | Recognizes a variety of possibilities for carrying out physical activity |
| 9 | Identifies the activities he/she should carry out every day to be healthy |
| 10 | Identifies the activities he/she should do once in a while |
| ATTITUDES | |
| Body and heart | |
| 11 | Body and heart care models |
| Nutrition | |
| 12 | Inappropriate nutrition models (once in a while foods) |
| 13 | Appropriate nutrition models (every day foods) |
| 14 | Appropriate nutrition models (variety of foods) |
| Physical activity | |
| 15 | Physical activity models (sedentarism) |
| 16 | Physical activity models (to be active) |
| HABITS | |
| Nutrition | |
| 17 | Vegetable consumption (last day) |
| 18 | Fruit consumption (last day) |
| 19 | Junk food consumption (last day) |
| Physical activity | |
| 20 | Physical exercise (on a typical day) |
| 21 | Sedentarism (on a typical day) |
| PARENTS’ SURVEY
| |
|---|---|
| Question | Domain |
| KNOWLEDGE | |
| Body and heart | |
| 1 | Cardiovascular disease is a problem that kills people. |
| 2 | Adopting healthy lifestyle habits is one of the most important ways to protect the family’s health. |
| Nutrition | |
| 3 | Recognizes which foods to eat every day in order to be healthy |
| 4 | Recognizes that there should be variety in the diet (food groups) |
| 5 | Recognizes which foods to eat once in a while in order to be healthy |
| 6 | Recognizes how to manage the food budget |
| Physical activity | |
| 7 | The balance between eating and physical activity is a fundamental part of good health. |
| 8 | Recognizes the benefits of avoiding sedentarism |
| 9 | Importance of providing opportunities for the children to engage in exercise |
| 10 | Knows the ideal amount of time for children to exercise |
| ATTITUDES | |
| Body and heart | |
| 11 | Adoption of healthy habits |
| 12 | Adoption of healthy habits |
| Nutrition | |
| 13 | Healthy diet within the budget (negative) |
| 14 | Healthy diet within the budget (positive) |
| 15 | Fruits and vegetables included in the child’s daily diet |
| 16 | Fruits and vegetables included in the child’s daily diet |
| 17 | Junk food avoided in the child’s daily diet |
| 18 | Junk food avoided in the child’s daily diet |
| Physical activity | |
| 19 | Provide the child with physical activity opportunities |
| 20 | Provide the child with physical activity opportunities |
| 21 | Children involved in daily physical activity |
| 22 | Children involved in daily physical activity |
| 23 | Restriction of children’s sedentary activities |
| 24 | Restriction of children’s sedentary activities |
| HABITS | |
| Nutrition | |
| 25 | Fruit and vegetable consumption |
| 26 | Soft drink, candy and/or fried foods consumption |
| Physical activity | |
| 27 | Carries out physical activity |
| 28 | Avoid sedentary activities |
| TEACHER’S SURVEY
| |
|---|---|
| Question | Domain |
| KNOWLEDGE | |
| Body and heart | |
| 1 | Cardiovascular disease is a problem that kills people. |
| 2 | Adopting healthy lifestyle habits is one of the most important ways to protect the family’s health. |
| Nutrition | |
| 3 | Recognizes which foods to eat every day in order to be healthy |
| 4 | Recognizes that there should be variety in the diet (food groups) |
| 5 | Recognizes which foods to eat once in a while in order to be healthy |
| 6 | Recognizes how to manage the food budget |
| Physical activity | |
| 7 | The balance between eating and physical activity is a fundamental part of good health. |
| 8 | Recognizes the benefits of avoiding sedentarism |
| 9 | Importance of providing opportunities for the children to engage in exercise |
| 10 | Knows the ideal amount of time for children to exercise |
| ATTITUDES | |
| Body and heart | |
| 11 | Adoption of healthy habits |
| 12 | Adoption of healthy habits |
| Nutrition | |
| 13 | Healthy diet within the budget (negative) |
| 14 | Healthy diet within the budget (positive) |
| 15 | Fruits and vegetables included in the child’s daily diet |
| 16 | Fruits and vegetables included in the child’s daily diet |
| 17 | Junk food avoided in the child’s daily diet |
| 18 | Junk food avoided in the child’s daily diet |
| Physical activity | |
| 19 | Provide the child with physical activity opportunities |
| 20 | Provide the child with physical activity opportunities |
| 21 | Children involved in daily physical activity |
| 22 | Children involved in daily physical activity |
| 23 | Restriction of children’s sedentary activities |
| 24 | Restriction of children’s sedentary activity |
| HABITS | |
| Nutrition | |
| 25 | Fruit and vegetable consumption |
| 26 | Soft drink, candy and/or fried foods consumption |
| 27 | Health-related activities carried out by teachers in class |
| Physical activity | |
| 28 | Carries out physical activity |
| 29 | Avoids sedentary activities |
| 30 | Health-related activities carried out by teachers in class |
Footnotes
Conflict of Interest: None.
Authorship: All authors had access to the data and a role in writing this manuscript.
References
- 1.Olsen J, Chongsuvivatwong V, Beaglehole R. Prevention and control of chronic, non-communicable diseases. In: Detels R, Beaglehole R, Lansang M, Gulliford M, editors. Oxford Textbook of Public Health. 5. Oxford, UK/New York: Oxford University Press; 2009. [Google Scholar]
- 2.Adeyi O, Smith O, Robles S. Public Policy and the Challenge of Chronic Noncommunicable Diseases. Washington, DC: World Bank; 2007. [Accessed August 10, 2010]. Available at: http://siteresources.worldbank.org/INTPH/Resources/PublicPolicyandNCDsWorldBank2007FullReport.pdf. [Google Scholar]
- 3.World Health Organization (WHO) Global Strategy on Diet, Physical Activity and Health: A Framework to Monitor and Evaluate Implementation. Geneva, Switzerland: WHO Press; 2006. [Accessed April 12, 2010]. Available at: http://www.who.int/dietphysicalactivity/Indicators%20English.pdf. [Google Scholar]
- 4.Deshmukh-Taskar P, Nicklas TA, Morales M, Yang SJ, Zakeri I, Berenson GS. Tracking of overweight status from childhood to young adulthood: the Bogalusa Heart Study. Eur J Clin Nutr. 2006;60:48–57. doi: 10.1038/sj.ejcn.1602266. [DOI] [PubMed] [Google Scholar]
- 5.Freedman DS, Khan LK, Dietz WH, Srinivasan SR, Berenson GS. Relationship of childhood obesity to coronary heart disease risk factors in adulthood: the Bogalusa Heart Study. Pediatrics. 2001;108:712–718. doi: 10.1542/peds.108.3.712. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) [Accessed April 10, 2010];Global Strategy on Diet, Physical Activity and Health. 2004 Available at: http://www.who.int/dietphysicalactivity/strategy/eb11344/strategy_spanish_web.pdf.
- 7.Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, U.S. Department Of Health and Human Services. [Accessed February 12, 2009];Physical Activity and Good Nutrition: Essential Elements to Prevent Chronic Diseases and Obesity. 2008 Available at: http://www.cdc.gov/nccdphp/publications/aag/pdf/dnpa.pdf.
- 8.Summerbell CD, Waters E, Edmunds L, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;(3):CD001871. doi: 10.1002/14651858.CD001871.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Increasing physical activity: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep. 2001;50(RR-18):1–14. [PubMed] [Google Scholar]
- 10.Ekelund U, Luan J, Sherar L, Esliger D, Griew F, Cooper A. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307(7):704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, Department of Health and Human Services. Physical Activity Evaluation Handbook. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2002. Theories and models used in physical activity promotion. [Google Scholar]
- 12.SitiSabariah B, Zalilah MS, Norlijah O, et al. Reliability and validity of the primary school children’s nutrition knowledge, attitude and practice instrument used in the HELIC Study. Mal J Nutr. 2006;12:33–44. [Google Scholar]
- 13.Zalilah MS, SitiSabariah B, Norlijah O, et al. Nutrition education intervention improves nutrition knowledge, attitude and practices of primary school children: a pilot study. Int Electron J Health Educ. 2008;11:119–132. [Google Scholar]
- 14.Shamah-Levy T, Villalpando-Hernández S, Rivera-Dommarco J. Manual de Procedimientos para Proyectos de Nutrición [Spanish] Cuernavaca, México: Instituto Nacional de Salud Pública; 2006. [Google Scholar]
- 15.Kuczmarski RJ, Ogden CL, Guo SS, et al. CDC growth charts for the United States: methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 16.El Departamento Adminstrativo Nacional de Estadística (DANE) [Accessed November 10, 2010];Estratificación socioeconómica [Spanish] Available at: http://www.dane.gov.co/index.php?Itemid=281&id=93&option=com_content§ionid=23&task=category.
- 17.Vasquez F, Andrade M, Rodríguez M. Efecto de un programa de educación nutricional en el consumo de energía y macronutrientes de preescolares asistentes a jardines infantiles Junji de la zona oriente de Santiago, Chile [Spanish] Arch Latinoam Nutr. 2008;58:241–248. [PubMed] [Google Scholar]
- 18.Davis M, Baranowski T, Resnicow K, et al. Gimme 5 fruit and vegetables for fun and health: process evaluation. Health Educ Behav. 2000;27:167–176. doi: 10.1177/109019810002700203. [DOI] [PubMed] [Google Scholar]
- 19.Caballero B, Clay T, Davis S, Ethelbah B, Rock B. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–1038. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoehner CM, Soares J, Parra Perez D, et al. Physical activity interventions in Latin America: a systematic review. Am J Prev Med. 2008;34:224–233. doi: 10.1016/j.amepre.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 21.Smith R, Huaraz A. Effectiveness of an educational program focusing in healthy lifestyles for overweight and obesity reduction in School, Peru. Acta Med Per. 2008;25:204–209. [Google Scholar]
- 22.Chiang M, Torres M, Maldonado M. Propuesta de un Programa de Promoción Sobre un Estilo de Vida Saludable en Preescolares Mediante Una Intervención Multidisciplinaria [Spanish] Rev Cubana Invest Biomed. 2003;22:245–252. [Google Scholar]
- 23.Da Cunha CT. São Paulo, Master Thesis. Universidade Federal de São Paulo; 2002. Impacto de Programa Educativo no Gasto Energético de Escolares nas aulas de Educação Física: ensaiorandomizado controlado [Spanish] [Google Scholar]
- 24.Kain J, Uauy R, Albala, Vio F, Cerda R, Leyton B. School-based obesity prevention in Chilean primary school children: methodology and evaluation of a controlled study. Int J Obes Relat Metab Disord. 2004;28:483–493. doi: 10.1038/sj.ijo.0802611. [DOI] [PubMed] [Google Scholar]
- 25.Bonhauser M, Fernandez G, Püschel K, et al. Improving physical fitness and emotional well-being in adolescents of low socioeconomic status in Chile: results of a school-based controlled trial. Health Promot Int. 2005;20:113–122. doi: 10.1093/heapro/dah603. [DOI] [PubMed] [Google Scholar]
- 26.Coleman KJ, Tiller CL, Sanchez J, et al. Prevention of the epidemic increase in child risk of overweight in low-income schools: the El Paso coordinated approach to child health. Arch Pediatr Adolesc Med. 2005;159:217–224. doi: 10.1001/archpedi.159.3.217. [DOI] [PubMed] [Google Scholar]
- 27.Heath EM, Coleman KJ. Evaluation of the institutionalization of the coordinated approach to child health (CATCH) in a US/Mexico border community. Health Educ Behav. 2002;29:444–460. doi: 10.1177/109019810202900405. [DOI] [PubMed] [Google Scholar]
- 28.McAleese JD, Rankin LL. Garden-based nutrition education affects fruit and vegetable consumption in sixth-grade adolescents. J Am Diet Assoc. 2007;107:662–665. doi: 10.1016/j.jada.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 29.Choi ES, Shin NR, Jung EI, Park HR, Lee HM, Song KH. A study on nutrition knowledge and dietary behavior of elementary school children in Seoul. Nutr Res Pract. 2008;2(4):308–316. doi: 10.4162/nrp.2008.2.4.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson AS, Porteous LE, Foster E, et al. The impact of a school-based nutrition education intervention on dietary intake and cognitive and attitudinal variables relating to fruits and vegetables. Public Health Nutr. 2005;8:650–656. doi: 10.1079/phn2004721. [DOI] [PubMed] [Google Scholar]
- 31.Perry CL, Bishop D, Taylor G, et al. A randomized school trial of environmental strategies to encourage fruit and vegetable consumption among children. Health Educ Behav. 2004;31:65–76. doi: 10.1177/1090198103255530. [DOI] [PubMed] [Google Scholar]
- 32.Yoon HS, Yang HL, Her ES. Effect of nutrition education program on nutrition knowledge, dietary diversity of elementary school children. Korean J Comm Nutr. 2000;5:513–521. [Google Scholar]
- 33. [Accessed April 12, 2012];Encuesta Nacional de la situación nutricional en Colombia (ENSIN 2010) Available at: https://www.icbf.gov.co/icbf/directorio/portel/libreria/php/frame_detalle.php?h_id=7685.
- 34.World Health Organization (WHO) Interventions on diet and physical activity: what works. WHO; 2009. [Accessed July 15, 2010]. Available at: http://www.who.int/dietphysicalactivity/whatworks/en/ [PubMed] [Google Scholar]
- 35.National Institute for Health and Clinical Excellence. [Accessed March 22, 2010];Promoting physical activity, active play and sport for pre-school and school-age children and young people in family, pre-school, school and community settings. 2009 Available at: http://www.nice.org.uk/PH17.