Abstract
Little information exists on the impact of integrating family planning (FP) services into HIV care and treatment on patients’ familiarity with and attitudes toward FP. We conducted a cluster-randomized trial in 18 public HIV clinics with twelve randomized to integrated FP and HIV services and six to the standard referral-based system where patients are referred to an FP clinic. Serial cross-sectional surveys were done before (n=488 women, 486 men) and after (n=479 women, 481 men) the intervention to compare changes in familiarity with FP methods and attitudes toward FP between integrated and non-integrated sites. We created an FP familiarity score based on the number of more effective FP methods patients could identify (score range: 0-6). Generalized estimating equations were used to control for clustering within sites. An increase in mean familiarity score between baseline (mean=5.16) and post-intervention (mean=5.46) occurred with an overall mean change of 0.26 (95%CI= 0.09, 0.45; p=0.003) across all sites. At endline, there was no difference in increase of mean FP familiarity scores at intervention versus control sites (mean=5.41 vs. 5.49, p=0.94). We observed a relative decrease in the proportion of males agreeing that FP was “women’s business” at integrated sites (baseline 42% to endline 30%; reduction of 12%) compared to males at non-integrated sites (baseline 35% to endline 42%; increase of 7%); aOR=0.43; 95%CI=0.22, 0.85). Following FP-HIV integration, familiarity with FP methods increased but did not differ by study arm. Integration was associated with a decrease in negative attitudes toward FP among men.
Introduction
Integrating FP into HIV services offers an opportunity to provide FP information and services to women and men of reproductive age who are living with HIV as well as reduce negative attitudes towards contraception. Studies show that although individuals living with HIV vary in their desire for more children (Cooper et al., 2009; Kaida et al., 2011; Nattabi, Li, Thompson, Orach, & Earnest, 2009), in the absence of counseling and FP method provision, high rates of unplanned pregnancies occur (King et al., 1995; Schwartz et al., 2012) particularly in an environment where low contraceptive use and cultural constructs that support high fertility are prevalent (Grabbe et al., 2009). Several studies in sub-Saharan Africa (SSA) have highlighted that male partners’ negative attitudes towards contraception have an inhibiting effect on a woman’s ability to adopt a method of contraception (Agadjaian, 2002; Agha, 1998; Mbizvo & Adamchak, 1991; Singh, 1998). This barrier may be more pronounced in HIV patients since the negative attitudes towards contraception may be further compounded by the negative perceptions about their own health status (Grabbe et al., 2009). Integration of FP and HIV services may result in decreasing negative attitudes among males towards contraception by being able to facilitate male involvement in FP more easily since men present to HIV clinics for their own care (Newmann et al., 2013).
To date, few studies have described the effect of integration on familiarity with FP and the opportunity that integration of FP and HIV services provides to affect negative male attitudes towards FP. In this study we assess the impact of integrating FP and HIV services on HIV-infected men and women’s familiarity with FP methods and HIV-infected men’s attitudes towards women using FP in a high HIV prevalence population. We hypothesize that integrating FP and HIV services will be positively associated with increased familiarity with FP methods and a reduction in negative male attitudes towards FP.
Methods
Ethics statement
The Committee on Human Research at UCSF and the Ethical Review Committee at KEMRI approved this study. The study was registered with clinicaltrials.gov, NCT01001507. Written consent was obtained from individual patients to contribute data to the study; de-identified data were used in the analysis.
Study design
This study was nested within a cluster-randomized control trial (RCT), which evaluated the impact of integrating FP services into HIV services on contraceptive prevalence. The RCT utilized a 2:1 randomization strategy of integration sites to control sites. The 2:1 ratio was selected to respond to the Kenya Ministry of Health’s interest in moving forward with integration. We evaluated FP knowledge, attitudes and perceptions among HIV-infected men and women using a cross-sectional pre- and post-intervention design. More information on study methods is available elsewhere (Grossman et al., 2013)
Study sites and participants
The study was conducted at 18 HIV clinics in the Nyanza Region. Eligible sites were public sector HIV clinics in Kisumu, Migori and Homabay Counties of Nyanza Province, Kenya. The Family AIDS Care & Education Services (FACES) program supported all sites (Lewis Kulzer et al., 2012). Participants were included if they met the following criteria: 1) HIV-positive woman or man obtaining HIV care at the FACES-supported public HIV clinic, 2) not currently pregnant (if female), 3) age 18 to 45 years old, and 4) willing and able to give informed consent. At baseline, a total of 974 patients were surveyed and 960 patients were surveyed at endline.
Procedures
We conducted a baseline survey from June to August 2009, during a three-month period prior to intervention implementation, and an endline survey approximately 12 months later during the final three months of the study from July to September 2011. The sample size was based on the ability to detect at least a ten percent point difference in contraceptive knowledge between unique participants at intervention sites versus those at comparison sites. For a one-sided test of two proportions using two samples, power of 0.8, and an alpha level of 0.05, the required sample size was 325 patients from the intervention sites (12) and 163 patients from the comparison sites (6) for both men (N=488) and women (N=488), equaling approximately 28 men and 28 women from each study site. Convenience sampling was used to select participants. For both surveys, a questionnaire regarding knowledge, attitudes and practices (KAP) related to FP was administered. The surveys were administered face-to-face by an interviewer in the respondent’s preferred language (Dholuo, Kiswahili, or English) in a private area of the health facility. The survey was adapted from the Demographic and Health Survey modules on contraception, marriage and sexuality, and fertility preferences (Kenyan National Bureau of Statistics, 2010)
Intervention
In collaboration with the Kenyan Ministry of Health we initiated a FP-HIV integration intervention that had four pillars namely: patient education, provider training and counseling, method provision and systems strengthening, and monitoring and evaluation. HIV clinics assigned to the intervention [full integration (FI)] integrated FP counselling and method provision, including all reversible FP methods (barrier, hormonal and intrauterine), within the HIV clinic. Non-integrated (NI) facilities referred patients interested in FP to a separate maternal child and FP clinic that was the current standard of care. In both FI and NI sites Clinic and Community Health Assistants (CCHAs), provided health talks about FP in the waiting bay while patients waited to be seen (Onono et al., 2014) and trained nurses provided the FP methods. As such, patients at all FI and NI sites were exposed to information about FP. The intervention lasted twelve months.
Main outcome measures
Patients’ familiarity with more effective FP methods was obtained based on responses to the question “Which ways or methods [of FP] have you heard about?” More effective FP methods in this study refer to tubal ligation, vasectomy, subdermal implants, injectable progestins, intrauterine devices and oral contraceptive pills. For the purpose of analysis, a knowledge score was created based on the number of ‘yes’ responses. Scores could range from 0 (never heard of any of the 6 methods) to 6 (heard of all 6 methods). These scores were then scaled up to 0-100 in order to better indicate the change in score percentage from baseline to endline.
Male attitudes toward FP were ascertained based on male patient’s responses to two statements, “Contraception is women’s business and a man should not have to worry about it” and “Women who use contraception may become promiscuous.” Men could respond, “agree,” “disagree,” or “don’t know.”
Patient characteristics examined in the study included age, educational attainment, relationship status, disclosure of patient’s HIV status to his or her partner. Health markers assessed were self-reported health status (good, fair, poor), number of living children, and future fertility preferences.
Statistical Methods
Questionnaire data was stored in Microsoft Access Version 2007 (Microsoft Inc., Redmond, WA) and records were extracted to SAS Version 9.2 (SAS Institutes Inc., Cary, North Carolina, USA), which was used for all further data management and statistical analysis. All independent variables were reported using frequencies and proportions. Since this trial was randomized by site, analyses for all dependent variables were completed using generalized estimating equations (GEE). This method accounts for any covariance between independent variables due to clustering (LIANG & ZEGER, 1986). GEE were used to estimate proportions and detect differences in the change of familiarity scores between FI and NI from baseline compared to endline. The dependent variable for the knowledge score analysis was the knowledge score (0-100 scale). The knowledge scores were scaled up to 0-100 in order for the GEE equation to provide information on total percentage change in score. The GEE estimating change in knowledge score adjusted for all independent variables. GEE were also used to estimate proportions and detect differences in the change of attitudes toward FP between men at FI sites versus NI sites from baseline compared to end of the study period. For the purposes of analysis, we examined only men who responded either ‘agree’ or ‘disagree’ as the response ‘don’t know’ had low response levels and was also ambiguous.
For both these analyses the independent variables were: age, educational attainment, relationship status, disclosure of HIV status to partner, self-reported health status, number of living children, and desired fertility delay. The GEE equation for this analysis provided an odds ratio and 95% confidence intervals (CI), since the dependent variable was binomial in nature. The odds ratio was adjusted for all independent variables. Adjusted odds ratios were considered statistically significant at a p-value less than 0.05.
Results
Baseline characteristics of respondents
Figure 1 shows the number of participants’ surveys analyzed at baseline. Overall baseline patient characteristics between FI and NI sites were similar (see Table I). Among all participants, most were >26 years old, however, male participants were older than the female participants. A higher number of males reported being married than females. While the majority of both genders reported their main partner was HIV positive, males reported higher levels of their main partner being HIV negative compared to females, whereas females reported higher levels of not knowing their partners’ HIV status. Males reported higher levels of disclosure of their HIV status than females. Males and females also reported differences in desired fertility delay; more males than females reported wanting to have a child within the next 2 years.
Figure 1.
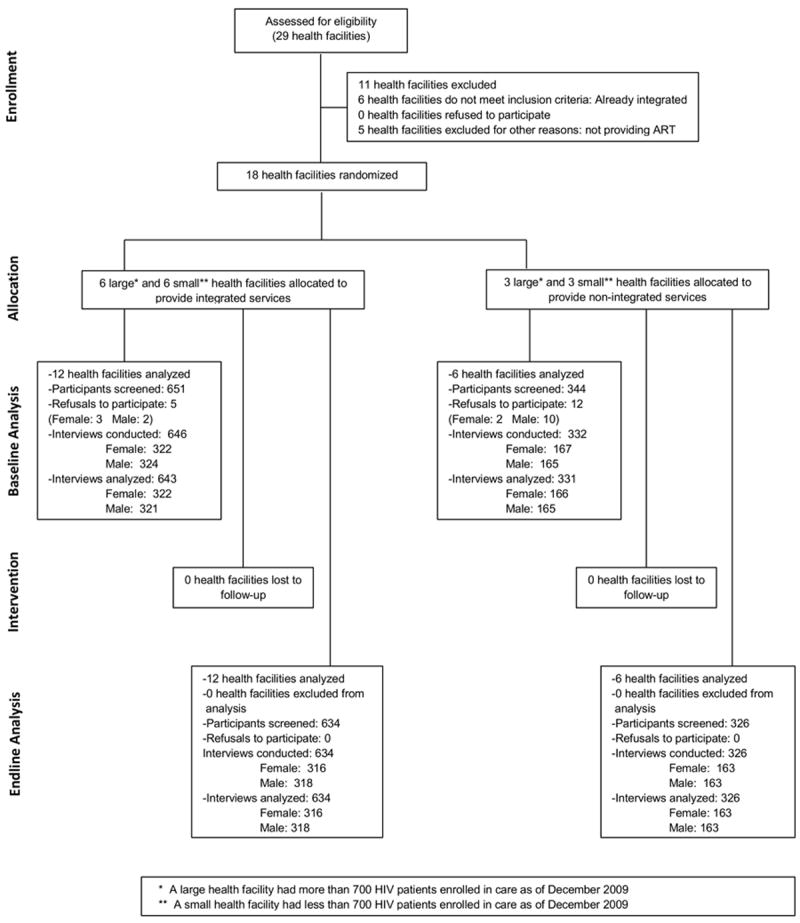
CONSORT flow diagram: Trial profile
Table I.
Baseline patient characteristics
| Measure | Males | Females | All | |||
|---|---|---|---|---|---|---|
| Integrated n=321 (%) |
Non-integrated n=165 (%) |
Integrated n=322 (%) |
Non-integrated n=166 (%) |
Integrated n=643 |
Non-integrated n=331 |
|
| Age (years) | ||||||
| 18 – 25 | 28 (8.7) | 23 (13.9) | 85 (26.5) | 47 (28.3) | 113 (14.6) | 70 (21.1) |
| 26 – 34 | 118 (36.9) | 66 (40.0) | 156 (48.6) | 80 (48.2) | 274 (42.7) | 146 (44.1) |
| 35+ | 174 (54.4) | 76 (46.1) | 80 (24.9) | 39 (23.5) | 254 (39.6) | 115 (34.7) |
| Highest educational level attained | ||||||
| None or primary | 239 (74.4) | 114 (69.1) | 269 (83.5) | 145 (87.4) | 508 (79.0) | 259 (78.2) |
| Secondary or greater | 89 (25.6) | 51 (30.9) | 53 (16.5) | 21 (12.6) | 135 (21.0) | 72 (21.7) |
| Covered floors in home | 50 (15.6) | 24 (14.5) | 71 (22.0) | 28 (16.9) | 121 (18.8) | 52 (15.7) |
| Household has a cell phone | 168 (52.5) | 86 (52.1) | 148 (46.0) | 77 (46.4) | 316 (49.2) | 163 (49.2) |
| Relationship status | ||||||
| Single | 22 (6.9) | 23 (13.9) | 51 (15.8) | 24 (14.6) | 73 (11.4) | 47 (14.3) |
| Living together | --- | --- | 14 (4.4) | 9 (5.5) | 14 (2.2) | 9 (2.7) |
| Girlfriend/Boyfriend | 16 (5.0) | 14 (8.5) | 31 (9.6) | 16 (9.8) | 47 (7.3) | 30 (9.1) |
| Married | 281 (88.1) | 128 (77.6) | 226 (70.2) | 115 (70.1) | 507 (79.1) | 243 (73.9) |
| HIV status main partner | ||||||
| HIV-positive | 200 (67.6) | 90 (63.8) | 167 (63.5) | 79 (58.5) | 169 (61.2) | 367 (65.7) |
| HIV-negative | 55 (18.6) | 28 (19.9) | 24 (9.1) | 17 (12.6) | 45 (16.3) | 79 (14.1) |
| Don’t know | 41 (13.8) | 23 (16.3) | 72 (27.4) | 39 (28.9) | 62 (22.5) | 113 (20.2) |
| Disclosed to partner | 266 (84.4) | 131 (80.4) | 213 (66.6) | 111 (66.9) | 479 (75.4) | 242 (73.6) |
| Reported health status | ||||||
| Good | 195 (61.1) | 89 (54.3) | 210 (65.4) | 107 (64.5) | 405 (63.3) | 196 (59.4) |
| Fair | 100 (31.4) | 61 (37.2) | 100 (31.2) | 55 (33.1) | 200 (32.2) | 116 (35.2) |
| Poor | 24 (7.5) | 14 (8.5) | 11 (3.4) | 4 (2.4) | 35 (5.5) | 18 (5.4) |
| Number of living children | ||||||
| 0 | 22 (6.9) | 27 (16.4) | 31 (9.7) | 17 (10.3) | 53 (8.3) | 44 (13.3) |
| 1 – 3 | 166 (51.7) | 80 (48.5) | 189 (58.9) | 89 (53.9) | 355 (55.3) | 169 (51.2) |
| ≥ 4 | 133 (41.4) | 58 (35.1) | 101 (31.5) | 59 (35.8) | 234 (36.4) | 117 (35.4) |
| Number of children infected with HIVa | ||||||
| 0 | 259 (87.2) | 120 (85.1) | 210 (71.2) | 115 (74.2) | 469 (79.2) | 235 (79.4) |
| ≥ 1 | 38 (12.8) | 21 (14.9) | 85 (28.8) | 40 (25.8) | 123 (20.8) | 60 (20.6) |
| Desired fertility delay | ||||||
| 0 – 2 years | 65 (20.8) | 48 (29.6) | 61 (19.0) | 29 (17.6) | 126 (19.9) | 77 (23.6) |
| > 2 years | 43 (13.7) | 29 (17.9) | 51 (15.9) | 25 (15.1) | 94 (14.8) | 54 (16.5) |
| Does not prefer to have any more children | 171 (54.6) | 64 (39.5) | 173 (53.9) | 97 (58.8) | 344 (54.3) | 161 (49.2) |
| Other | 34 (10.9) | 21 (13.0) | 36 (11.2) | 14 (8.5) | 70 (11.0) | 35 (10.7) |
of patients who have ever had children
Factors associated with FP method familiarity
Baseline knowledge scores among women and men were relatively high (see Figures 2a, 2b and 2c). Females and males at FI and NI sites had mean knowledge scores of >80 at baseline (0-100 scale), indicating they were familiar with approximately five out of six FP methods asked. We observed a statistically significant increase of 6.32 points (95% CI 2.67-9.97, p-value<0.001) between baseline and endline in mean knowledge score among women (see Figure 2b and Table II). However, the mean change in knowledge score among women did not differ between FI and NI sites. Among men, mean change in knowledge score was not statistically significant over time, or between FI and NI sites (see figure 2a).
Figure 2.

a: Familiarity with FP methods score (0-100 scale) between integrated and non-integrated sites from beginning to end of study among males (N=944).
b: Change in familiarity with FP score (0-100 scale) between integrated and non-integrated sites from beginning to end of study among females (N=954).
c: Change in familiarity with FP score (0-100 scale) between integrated and non-integrated sites from beginning to end of study among all participants (N=1898).
Table II.
Factors associated with familiarity with family planning methods among males and females over time, pre- and post family planning intervention
| Variable | Males (n=944) |
Females (n=954) |
All (n=1898) |
|||
|---|---|---|---|---|---|---|
| β, (95% CI) | p-value | β, (95% CI) | p-value | β, (95% CI) | p-value | |
| Interaction of time and integration Status | 1.05 (-6.01, 8.10) | 0.77 | -1.85 (-7.26, 3.55) | 0.50 | -0.42 (-6.52, 5.67) | 0.89 |
| Timea | 3.13 (-2.60, 8.86) | 0.28 | 6.32 (2.67, 9.97) | <0.001 | 4.83 (-0.00, 9.66) | 0.05 |
| Integration Status | 0.74 (-2.03, 3.51) | 0.60 | 0.85 (-2.52, 4.22) | 0.62 | 0.75 (-1.91, 3.40) | 0.58 |
| Gender | ||||||
| Male | … | … | … | … | -4.83 (-6.69, -2.96) | <0.001 |
| Female | … | … | … | … | 1.00 | ref |
| Age | ||||||
| 18-24 | -0.15 (-4.44, 4.13) | 0.94 | -3.56 (-5.77, -1.35) | 0.001 | -2.76 (-4.92, -0.60) | 0.01 |
| 25-34 | -2.47 (-5.86, 0.92) | 0.15 | -1.39 (-3.86, 1.07) | 0.27 | -2.14 (-4.62, 0.33) | 0.09 |
| 35+ | 1.00 | Ref | 1.00 | ref | 1.00 | ref |
| Higher education | 5.59 (3.17, 8.01) | <0.001 | 2.14 (0.36, 3.91) | 0.02 | 4.34 (2.85, 5.84) | <0.001 |
| Relationship Status | ||||||
| Single | 1.63 (-5.98, 0.91) | 0.67 | -4.99 (-7.90, -2.09) | <0.001 | -2.03 (-4.49, 0.43) | 0.11 |
| Living together | -1.20 (-10.85, 8.44) | 0.81 | -2.64 (-7.51, 2.24) | 0.29 | -2.37 (-6.22, 1.49) | 0.23 |
| Girlfriend/Boyfriend | 0.56 (-6.45, 7.56) | 0.88 | -1.03 (-4.21, 2.14) | 0.52 | -0.22 (-3.32, 2.88) | 0.89 |
| Married | 1.00 | ref | 1.00 | Ref | 1.00 | ref |
| Disclosed HIV Status to partner | 6.17 (0.46, 11.88) | 0.03 | -1.48 (-3.26, 0.29) | 0.10 | 1.48 (-1.48, 4.44) | 0.33 |
| Health Status | ||||||
| Poor | -11.99 (-17.63, -6.34) | <0.001 | -1.28 (-5.51, 2.94) | 0.55 | -8.22 (-12.24, -4.19) | <0.001 |
| Fair | -2.12 (-4.51, 0.27) | 0.08 | -3.40 (-4.94, -1.86) | <0.001 | -2.73 (-4.43, -1.03) | 0.002 |
| Good | 1.00 | ref | 1.00 | Ref | 1.00 | ref |
| Number of living children | ||||||
| 0 | 1.00 | ref | 1.00 | Ref | 1.00 | ref |
| 1-3 | 2.09 (-3.48, 7.67) | 0.46 | 1.49 (-2.01, 4.99) | 0.40 | 1.95 (-0.57, 4.47) | 0.13 |
| ≥4 | 2.45 (-4.63, 9.53) | 0.50 | 0.25 (-3.33, 3.84) | 0.89 | 1.61 (-1.54, 4.77) | 0.32 |
| Desired fertility delay | ||||||
| 0-2 years | 0.33 (-2.40, 3.07) | 0.81 | -1.09 (-3.77, 1.60) | 0.43 | -0.45 (-2.21, 1.30) | 0.61 |
| >2 years | -0.14 (-3.32, 3.05) | 0.93 | -0.99 (-4.29, 2.31) | 0.55 | -0.66 (-2.81, 1.49) | 0.55 |
| Other | -1.37 (-5.52, 2.67) | 0.52 | -4.76 (-9.49, -0.02) | 0.05 | -2.80 (-5.71, 0.11) | 0.06 |
| No more children | 1.00 | ref | 1.00 | ref | 1.00 | ref |
Analysis conducted with multiple linear regression, utilizing generalize estimating equations; knowledge scores on a 0-100 scale
Variable ‘Time’ is defined as end of study period compared to baseline
The significant factors associated with knowledge score were different between males and females (Table II). Among both men and women, higher education was a significant predictor of higher knowledge score. Among males, disclosure of HIV status to partner was also a significant predictor for male higher knowledge score. In women, younger age and being single were significantly associated with lower knowledge score. Health status was a significant predictor of lower score among both men and women. Poor health status compared to good health status was significantly associated with lower score among men, while fair health status compared to good health status was associated with lower score among women.
Factors associated with changes in negative male attitudes towards FP
We observed a relative decrease in the proportion of males agreeing that FP was “women’s business” at FI sites compared to males at NI sites (see Figure 3, Table III).
Figure 3.
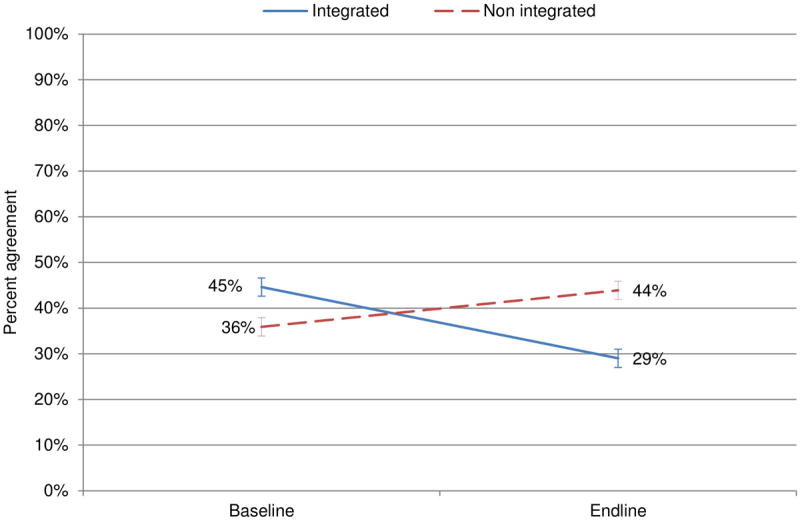
Change in male agreement with statement “FP is a woman’s business” between integrated and non-integrated sites during study period (N=929).
Table III.
Factors associated with change in male agreement that FP is a woman’s business from beginning to end of study period (N=929)
| Variable | aOR, (95% CI) | p-value |
|---|---|---|
| Interaction of time and integration Status | 0.43 (0.22, 0.85) | 0.02 |
| Time | 1.39 (0.92, 2.07) | 0.12 |
| Integration Status | 1.38 (0.65, 2.98) | 0.39 |
| Age | ||
| 18-24 | 1.23 (0.67, 2.24) | 0.50 |
| 25-34 | 0.84 (0.56, 1.25) | 0.38 |
| 35+ | 1.00 | ref |
| Higher education | 0.39 (0.29, 0.52) | <0.001 |
| Relationship Status | ||
| Single | 0.80 (0.44, 1.48) | 0.48 |
| Living together | 1.98 (0.54, 7.32) | 0.30 |
| Girlfriend | 0.68 (0.32, 1.45) | 0.32 |
| Married | 1.00 | ref |
| Disclosed HIV Status to partner | 0.38 (0.22, 0.64) | <0.001 |
| Health Status | ||
| Poor | 3.36 (1.65, 6.87) | <0.001 |
| Fair | 1.30 (1.04, 1.61) | 0.02 |
| Good | 1.00 | Ref |
| Number of living children | ||
| 0 | 1.00 | Ref |
| 1-3 | 1.15 (0.68, 1.96) | 0.59 |
| ≥4 | 1.40 (0.72, 2.69) | 0.32 |
| Desired fertility delay | ||
| 0-2 years | 1.39 (0.99, 1.94) | 0.05 |
| >2 years | 1.15 (0.79, 1.67) | 0.46 |
| Other | 1.03 (0.64, 1.64) | 0.91 |
| No more children | 1.00 | Ref |
Analysis conducted with multiple logistic regression, utilizing generalize estimating equations
Significant predictors for being more likely to disagree with the statement, ‘FP is women’s business’ included higher education and disclosure of HIV status to partner. Significant predictors for being more likely to agree with the statement included poor or fair health status compared to good health status (see Table III).
There was a relative, though non-significant, decrease in the proportion of males agreeing that FP was associated with promiscuity at FI sites compared to males at non-integrated sites (see Figure 4, Table IV). The significant predictors for disagreeing with the statement, ‘FP is associated with promiscuity’ included higher education and disclosure of HIV status to partner. Significant predictors for agreeing with the statement included younger age and poor health status compared to good health status (see Table IV).
Figure 4.
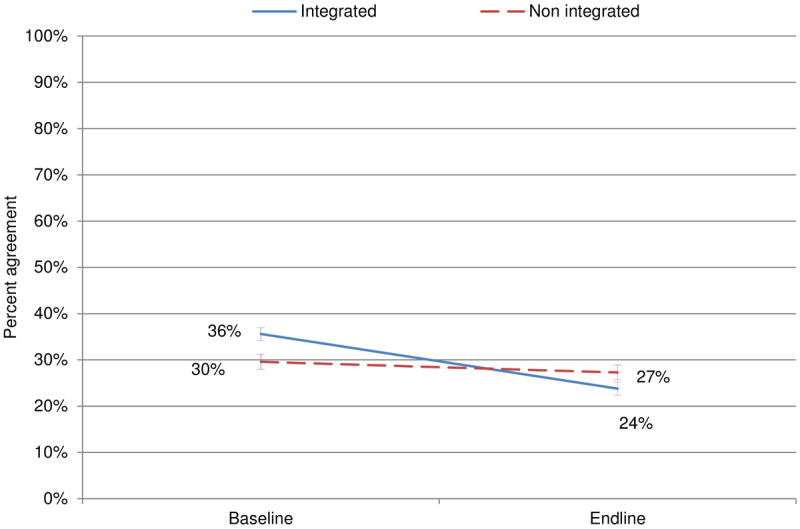
Change in male agreement with statement “FP is associated with promiscuity” between integrated and non-integrated sites during study period (N=819).
Table IV.
Factors associated with change in male agreement that ‘family planning is associated with promiscuity’ (N=819)
| Variable | aOR, (95% CI) | p-value |
|---|---|---|
| Interaction of time and integration status | 0.65 (0.34, 1.22) | 0.18 |
| Time | 0.92 (0.55, 1.52) | 0.74 |
| Integration Status | 1.54 (0.85, 2.78) | 0.15 |
| Age | ||
| 18-24 | 1.66 (1.06, 2.58) | 0.02 |
| 25-34 | 0.96 (0.63, 1.45) | 0.83 |
| 35+ | 1.00 | Ref |
| Higher education | 0.62 (0.48, 0.80) | <0.001 |
| Relationship Status | ||
| Single | 0.76 (0.44, 1.33) | 0.34 |
| Living together | 1.56 (0.32, 7.67) | 0.58 |
| Girlfriend | 0.81 (0.35, 1.91) | 0.63 |
| Married | 1.00 | Ref |
| Disclosed HIV Status to partner | 0.47 (0.30, 0.72) | <0.001 |
| Health Status | ||
| Poor | 2.72 (1.62, 4.58) | <0.001 |
| Fair | 1.39 (0.94, 2.04) | 0.09 |
| Good | 1.00 | Ref |
| Number of living children | ||
| 0 | 1.00 | Ref |
| 1-3 | 1.94 (0.93, 4.06) | 0.08 |
| ≥4 | 1.87 (0.80, 4.35) | 0.15 |
| Desired fertility delay | ||
| 0-2 years | 1.02 (0.66. 1.57) | 0.92 |
| >2 years | 1.02 (0.66, 1.58) | 0.93 |
| Other | 1.35 (0.80, 2.27) | 0.26 |
| No more children | 1.00 | Ref |
Analysis conducted with multiple logistic regression, utilizing generalize estimating equations
Discussion
Integration of FP into HIV services provides the unique opportunity to provide sexually active men and women who are HIV-infected with correct information, quality services and timely access to safe, effective modern contraception. We observed a small but significant increase in mean FP familiarity scores among women post intervention, yet no association between integration status and FP familiarity score. The lack of observed impact of integration status on FP familiarity may be attributed to the high baseline levels of knowledge familiarity in both arms (~80%) and the fact that during the intervention phase the participants in the NI sites were also exposed to FP education and counseling. Unfortunately a high level of contraceptive awareness does not always translate into high CPR (Omo-Aghoja et al., 2009; Solomon Avidime, 2010) particularly in HIV-infected patients where the common barriers to use of contraception such as, lack of female decision-making power (Chapagain, 2005), poor economic resources (Stephenson & Tsui, 2002), low-quality care of FP services (Hamid & Stephenson, 2006), and desire for large families (Singh, 1998) may be more pronounced.
Studies show improvements in uptake of contraception when men are involved in FP (Isaiah Ndong, 1999). As such there has been an intense interest to increase information about FP, encourage condom use and address men’s roles in FP. However, knowledge of FP methods in the absence of positive attitudes towards FP may not necessarily foster adoption and utilization. In a patriarchal society such as in many countries in SSA there must be a deliberate effort to move beyond increasing knowledge to changing male attitudes and practices while empowering women at the same time. The majority of HIV clinics in SSA do not segregate male and female patients. This setting thus provides a unique one-stop opportunity to integrate conversations about FP with men among their peers and with women. In such forums and in the presence of a trained health care worker, more in-depth information can be discussed and “peer-reviewed” to create a supportive and enabling environment for uptake of FP. Among persons living with HIV, integration of FP into HIV services as demonstrated in this study may have the potential to reduce negative attitudes towards contraception. Our study showed a relative decrease in the proportion of males agreeing that FP is a woman’s business at FI sites compared to males at NI sites. This is particularly important in an environment in which male desires for large numbers of children and high HIV prevalence may co-exist.
One of the predictors of positive attitudes toward FP included disclosure of HIV status. Conversely poor health status was a strong predictor of negative attitude towards FP. Individuals who disclose their status may be in a better position to make reproductive choices including use of contraception in an HIV clinic compared to a FP clinic (Steinfeld et al., 2013). In addition, disclosure facilitates other behaviors that may improve the management of HIV including adherence to drugs and better health outcomes (Deribe, Woldemichael, Wondafrash, Haile, & Amberbir, 2008; Pinkerton & Galletly, 2007; Waddell & Messeri, 2006). Similarly, people with HIV who are feeling well, as a result of treatment, are also likely to be in a better position to make reproductive health decisions which can be further facilitated by receiving HIV care and treatment and FP services in the same clinic. Lack of sexual health services and information places young people at high risk for pregnancy, abortion, HIV/AIDS and sexually transmitted diseases. In this study young age was a predictor of poor FP knowledge among women and negative male attitudes in this population. This highlights the need for current programs to go beyond traditional FP counseling and teaching techniques to discuss how to improve communication with partners and other lifestyle issues that may interfere with consistent use among young persons particularly those that are HIV infected.
This study had several limitations. The participants analyzed in this study may not be representative of the general HIV-infected adult population in Kenya. The data shown are taken from a convenience sample of men and women living with HIV attending HIV services in public health facilities. Additionally, the survey evaluated FP method familiarity by asking patients which FP methods they had heard of. Knowledge of the name of a method may not translate into actual knowledge of how that method works, what the side effects are, how it is administered. The lack of observed impact of integration status on FP familiarity may be attributed to contamination bias arising from the fact that during the intervention phase the participants in the NI sites were also exposed to FP education and counseling. The association observed between male attitudes and integrated FP/HIV services might have been stronger if the intervention included a specific module on gendered attitudes about FP,. Admittedly, the serial cross-section design does not allow us to look at intra-individual and inter-individual changes over time. However, since the intervention and randomization were applied at the clinic level, a serial rather than a longitudinal approach was important to capture information at the level of the clinic. Despite these limitations, the data presented here are a unique opportunity to understand the potential impact of integrating FP into HIV services on contraceptive knowledge and attitudes among HIV-infected reproductive-age men and women.
Ultimately the use of FP is inherently a product of correct knowledge about, cultural acceptance by both men and women of and access to available contraceptive methods. FP education can increase FP familiarity even in settings where persons appear to be already well informed. Additionally FP/HIV integration may help to decrease some negative male attitudes towards FP, which may in turn help increase FP uptake by women over time. In addition to increasing access to FP methods, our findings depict the importance of including education about FP methods and efforts to increase awareness of and modify preconceived negative gendered attitudes about FP as components of FP/HIV integrated services.
Acknowledgments
Funding
This work was supported by The Bill & Melinda Gates Foundation (http://www.gatesfoundation.org/) grant number OPPGH5361), and the Tides Africa Fund (http://www.tides.org/impact/fund-initiative-spotlight/tides-africa-fund/, grant numbers TFR10–01364 and TFR08–02986). Dr Newmann was supported by the National Center for Advancing Translational Sciences, National Institutes of Health through UCSF-CTSI grant number KL2TR000143.
We thank the Kenyan women and men who participated in the study. We acknowledge the important logistical support of the KEMRI-UCSF Collaborative Group and especially Family AIDS Care and Education Services (FACES). We gratefully acknowledge the Director of KEMRI, the Director of KEMRI’s Centre for Microbiology, and the Nyanza Provincial Ministries of Health and the provincial and district reproductive health coordinators for their support in conducting this research. We also thank Pauline Wekesa, Wanjiku King’ori, Gorrety Ongundi, Janet Opiyo, Phoebe Adhiambo, Christine Oray, Mercy Wanjiku, Violet Nasenya, and George Ochieng’ for their important contributions to this research.
References
- Agadjaian V. Men’s talk about “women’s matters”: gender, communication and contraception in urban Mozambique. Gender Society. 2002;16(2):194–215. doi: 10.1177/08912430222104903. [DOI] [Google Scholar]
- Agha S. Sexual activity and condom use in Lusaka, Zambia. Int Fam Plann Perspect. 1998;24:32–37. [Google Scholar]
- Chapagain M. Masculine interest behind high prevalence of female contraceptive methods in rural Nepal. Aust J Rural Health. 2005;13(1):35–42. doi: 10.1111/j.1440-1854.2004.00643.x. [DOI] [PubMed] [Google Scholar]
- Cooper D, Moodley J, Zweigenthal V, Bekker LG, Shah I, Myer L. Fertility intentions and reproductive health care needs of people living with HIV in Cape Town, South Africa: implications for integrating reproductive health and HIV care services. AIDS Behav. 2009;13(Suppl 1):38–46. doi: 10.1007/s10461-009-9550-1. [DOI] [PubMed] [Google Scholar]
- Deribe K, Woldemichael K, Wondafrash M, Haile A, Amberbir A. Disclosure experience and associated factors among HIV positive men and women clinical service users in southwest Ethiopia. BMC Public Health. 2008;8(1):81. doi: 10.1186/1471-2458-8-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabbe K, Stephenson R, Vwalika B, Ahmed Y, Vwalika C, Chomba E, Allen S, et al. Knowledge, use, and concerns about contraceptive methods among sero-discordant couples in Rwanda and Zambia. J Womens Health (Larchmt) 2009;18(9):1449–1456. doi: 10.1089/jwh.2008.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman D, Onono M, Newmann SJ, Blat C, Bukusi EA, Shade SB, Cohen CR, et al. Integration of family planning services into HIV care and treatment in Kenya: a cluster-randomized trial. AIDS. 2013;27:S77–S85. doi: 10.1097/QAD.0000000000000035. [DOI] [PubMed] [Google Scholar]
- Hamid S, Stephenson R. Provider and health facility influences on contraceptive adoption in urban Pakistan. Int Fam Plan Perspect. 2006;32(2):71–78. doi: 10.1363/ifpp.32.071.06. [DOI] [PubMed] [Google Scholar]
- Ndong Isaiah, B RM, Haws Jeanne M, Wegner Mary Nell. Men’s reproductive health: defining, designing, and delivering services. International Family Planning Perspectives. 1999;25(supplement):S53–S55. [Google Scholar]
- Kaida A, Laher F, Strathdee SA, Janssen PA, Money D, Hogg RS, Gray G. Childbearing intentions of HIV-positive women of reproductive age in Soweto, South Africa: the influence of expanding access to HAART in an HIV hyperendemic setting. Am J Public Health. 2011;101(2):350–358. doi: 10.2105/ajph.2009.177469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenyan National Bureau of Statistics, I. M. Kenya Demographic and Health Survey 2008-09 2010 [Google Scholar]
- King R, Estey J, Allen S, Kegeles S, Wolf W, Valentine C, Serufilira A. A family planning intervention to reduce vertical transmission of HIV in Rwanda. AIDS. 1995;9(Suppl 1):S45–51. [PubMed] [Google Scholar]
- Lewis Kulzer J, Penner JA, Marima R, Oyaro P, Oyanga AO, Shade SB, Cohen CR, et al. Family model of HIV care and treatment: a retrospective study in Kenya. J Int AIDS Soc. 2012;158(1) doi: 10.1186/1758-2652-15-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LIANG K-Y, ZEGER SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- Mbizvo MT, Adamchak DJ. Family planning knowledge, attitudes, and practices of men in Zimbabwe. Stud Fam Plann. 1991;22(1):31–38. [PubMed] [Google Scholar]
- Nattabi B, Li J, Thompson SC, Orach CG, Earnest J. A systematic review of factors influencing fertility desires and intentions among people living with HIV/AIDS: implications for policy and service delivery. AIDS Behav. 2009;13(5):949–968. doi: 10.1007/s10461-009-9537-y. [DOI] [PubMed] [Google Scholar]
- Newmann SJ, Grossman D, Blat C, Onono M, Steinfeld R, Bukusi EA, Cohen CR, et al. Does integrating family planning into HIV care and treatment impact intention to use contraception? Patient perspectives from HIV-infected individuals in Nyanza Province, Kenya. Int J Gynaecol Obstet. 2013 doi: 10.1016/j.ijgo.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omo-Aghoja LO, Omo-Aghoja VW, Aghoja CO, Okonofua FE, Aghedo O, Umueri C, Inikori KA, et al. Factors associated with the knowledge, practice and perceptions of contraception in rural southern Nigeria. Ghana Med J. 2009;43(3):115–121. doi: 10.4314/gmj.v43i3.55326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onono M, Blat C, Miles S, Steinfeld R, Wekesa P, Bukusi EA, Newmann SJ, et al. Impact of family planning health talks by lay health workers on contraceptive knowledge and attitudes among HIV-infected patients in rural Kenya. Patient education and counseling. 2014;94(3):438–441. doi: 10.1016/j.pec.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkerton SD, Galletly CL. Reducing HIV transmission risk by increasing serostatus disclosure: a mathematical modeling analysis. AIDS Behav. 2007;11(5):698–705. doi: 10.1007/s10461-006-9187-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz SR, Rees H, Mehta S, Venter WD, Taha TE, Black V. High incidence of unplanned pregnancy after antiretroviral therapy initiation: findings from a prospective cohort study in South Africa. PLoS One. 2012;7(4):e36039. doi: 10.1371/journal.pone.0036039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh ABS. Couple’s fertility and contraceptive decision making in developing countries; hearing the man’s voice. Int Fam Plann Perspect. 1998;24:15–24. [Google Scholar]
- Avidime Solomon, A-A L, Mohammed Ado Zakari, Adaji Sunday, Shittu Oladapo, Ejembi Clara. Fertility Intentions, Contraceptive Awareness and Contraceptive Use among Women in Three Communities in Northern Nigeria. African Journal of Reproductive Health. 2010;14(3):65–70. [Google Scholar]
- Steinfeld RL, Newmann SJ, Onono M, Cohen CR, Bukusi EA, Grossman D. Overcoming Barriers to Family Planning through Integration: Perspectives of HIV-Positive Men in Nyanza Province, Kenya. AIDS Research and Treatment. 2013;2013:8. doi: 10.1155/2013/861983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson R, Tsui AO. Contextual influences on reproductive health service use in Uttar Pradesh, India. Stud Fam Plann. 2002;33(4):309–320. doi: 10.1111/j.1728-4465.2002.00309.x. [DOI] [PubMed] [Google Scholar]
- Waddell EN, Messeri PA. Social support, disclosure, and use of antiretroviral therapy. AIDS Behav. 2006;10(3):263–272. doi: 10.1007/s10461-005-9042-x. [DOI] [PubMed] [Google Scholar]


