Abstract
The year 2014 marks the centennial of events that led to World War 1 (“the war to end all wars”) following the assassination of Archduke Ferdinand of the crumbling Austro-Hungarian Empire. It also marks the 120th anniversary of the birth of Stephen Rothman and the 60th anniversary of the publication of his epic textbook The Physiology and Biochemistry of the Skin. In this review we document our belief that Rothman had a seismic impact on moving investigative dermatology from a medical backwater to a scientific discipline that can hold its own with that of any other specialty.
Stephen Rothman (Figure 1) was described as the “widely acknowledged grand master of modern investigative dermatology” by Allan Lorincz (1924–2010) in his forward to a 1958 Festschrift in the Journal of Investigative Dermatology (JID) honoring Rothman (Lorincz, 1958). Few would dispute this accolade. The year 2014 marks the 60th anniversary of the publication of Rothman’s classic textbook Physiology and Biochemistry of the Skin (Rothman, 1954), as well as the 120th anniversary of his birth. It seems an appropriate time to revisit Rothman’s scientific career and its decisive impact on modern investigative dermatology.
Figure 1.
Stephen Rothman (courtesy of Gerd Plewig, MD, Munich, Germany)
Rothman took a circuitous route to his lofty position (Everett, 2013; Rothman and Lorincz, 1995). He was born into a wealthy Jewish family in Budapest, Hungary, on September 10, 1894. After graduating from medical school at the University of Budapest in 1917, he served in the Austro-Hungarian army during World War I and helped to manage a debilitating scabies epidemic in calvary horses. Rothman trained in dermatology with Albert Jesionek (1870–1935), a pioneer in cutaneous photobiology at the University of Giessen, Germany, from 1920 to 1928. He also spent six months with Bruno Bloch (1878–1933) at the University of Zurich doing pigment cell research and crossing paths with Marion Sulzberger (1895–1983). He returned to Budapest, opened a private practice, ran a large public outpatient clinic and continued his research at Semmelweis University where Lajos Nékám (1868–1967) was chairman. As Secretary-General, he helped Nékám organize the 9th International Congress of Dermatology and Syphilology in Budapest in 1935, making numerous international contacts that later helped him.
In the 1930s, anti-Semitism flared in Hungary and a variety of repressive measures were instituted. Rothman travelled to the United States in 1938 ostensibly to attend a meeting in San Francisco but in fact to immigrate. Sulzberger introduced him to Samuel W. Becker (1894–1964) who offered him a faculty position at the University of Chicago where he spent the rest of his academic life.
Rothman advanced rapidly at the university, immediately starting to publish on a wide variety of investigative topics. After Becker and Maximillian Obermayer (1896–1982) left the Section of Dermatology in the Department of Medicine in 1942, he was named Chief, and three years later promoted to Professor. He retired in 1959 but remained active in research until his death on August 31, 1963 (Lorincz, 1964).
Rothman’s impact on investigative dermatology can be tracked in several ways. He trained a cadre of superb research scientists, as well as many outstanding clinicians. Table 1 contains an abridged list of his students and their contributions. With his strong encouragement, Harvey Blank (1918–2001), then a medical student at the University of Chicago, trained in dermatology; Blank later developed a premier department at the University of Miami. In addition, Gerd Klaus Steigleder (1925-) spent time with Rothman; he later became chairman of dermatology at the University of Cologne (Burgdorf and Bickers, 2013).
Table 1.
Students of Stephen Rothman
| Name | Later affiliations | Major contributions |
|---|---|---|
| Calvin B. Dillaha | Arkansas | Systemic corticosteroids for alopecia areata, 5-fluoruracil for actinic keratoses |
| Kenneth Halprin | Miami | Psoriasis |
| Allan L. Lorincz | Chicago | Cutaneous physiology and pharmacology |
| Frederick D. Malkinson | Rush-St. Luke’s | Percutaneous absorption, effects of ionizing radiation and chemotherapy on hair matrix, oral biology |
| Roger W. Pearson | Rush-St. Luke’s | Electron microscopy of blistering disorders |
| Richard B. Stoughton | Case Western, Scripps, UC San Diego | Percutaneous absorption, topical corticosteroids |
| Eugene J. Van Scott | NIH, Temple | Epidermal kinetics, psoriasis, |
| Dorothy Windhorst | Minnesota, Hoffman-LaRoche | Immunodermatology, pharmacology (isotretinoin) |
Rothman also wrote and edited a remarkable textbook Physiology and Biochemistry of the Skin in 1954 that was unprecedented in its erudition and comprehensiveness (Rothman, 1954). To assemble this magnum opus he enlisted an extraordinary cohort of co-authors (Table 2)but still wrote 23 of the 28 chapters himself. The book was enthusiastically reviewed by the Archives of Dermatology and the reviewer thanked Rothman for “having compiled such a great fund of information…” (1954), while the British Journal of Dermatology recommended it to “any dermatologist interested in his subject beyond morphological diagnosis and empirical treatment.” (1955) In the preface to his epic two-volume textbook “Biochemistry and Physiology of the Skin” published in 1983, Lowell Goldsmith commented, “Yet no single text has attempted to review all of skin biochemistry and physiology since Rothman’s Physiology and Biochemistry of the Skin (1954), an extraordinary benchmark for dermatology.” (Goldsmith, 1983)
Table 2.
Contributors to Physiology and Biochemistry of the Skin
| Name | Later affiliations | Major contributions |
|---|---|---|
| Zachary Felsher | Illinois, Northwestern | Collagen biochemistry |
| Peter Flesch | Pennsylvania | Disorders of keratinization |
| Aaron B. Lerner | Yale | Melanocyte physiology, identified both melanocyte-stimulating hormone and melatonin, described cryoglobulins |
| Allan L. Lorincz | Chicago | Cutaneous physiology and pharmacology |
| Hermann Pinkus | Wayne State | Dermatopathology |
| George C. Wells | St. Thomas-London | Histochemistry, immunodermatology, described eosinophilic cellulitis (Wells’ syndrome) |
Rothman’s bibliography shows that he was creative, insightful, and extraordinarily productive and that he concentrated most of his efforts in a few major areas. The epidermis was perhaps his first love and his students throughout their careers carried this forward, several becoming acknowledged leaders—keratinization (Flesch), epidermal fragility (Pearson), epidermal kinetics (van Scott) and percutaneous absorption (Stoughton). His other main interests were epidermal lipids, melanogenesis, neurophysiology, endocrinology and photobiology. While he was a multi-faceted clinician, pruritus was a special focus. In Rothman’s era, research in skin biology was largely descriptive and generally considered to be vastly inferior to that occurring in most other specialities. This makes his prescient accomplishments all the more impressive. In his introduction to the Rothman Festschrift, Lorincz listed 11 seminal contributions (Lorincz, 1958). With the help of several present-day leaders, we show how these advances have helped lead the way to the current elevated status of dermatologic research in 2014.
Cutaneous neurobiology: Rothman worked with Julius M. Coon (1910–2000), a pharmacologist, to analyze the role of acetylcholine (Ach) in the skin (Rothman and Coon, 1940). They identified the axon flare, which we now know is driven by a branching network of axons that also interact with sensory nerves which may be involved in “flushing” and “blushing” (Roosterman et al., 2006), as well as the pilomotor response that that has been described as “gooseflesh”. They also identified cholinergic signaling as the primary mediator for parasympathetic cutaneous vasodilation as well as for sympathetic eccrine sweating. Because Ach is also released by non-neuronal cells and receptors for Ach are widely expressed, e.g. on keratinocytes, the effects of this neurotransmitter extend far beyond its classical neurobiological role. The remarkable efficacy of injected botulinum toxin in hyperhidrosis exploits its anticholinergic effect (Shibasaki et al., 2009). Botulinum toxin also blocks cutaneous vasodilation during menopausal hot flashes (Low et al., 2011). Ach mediates sweat-induced itch in patients with atopy (Heyer et al., 1997). Finally, cholinergic signaling can facilitate communication between immune and epidermal cells to mount a physiological response to injury or infection and to maintain epidermal barrier function (Curtis and Radek, 2012).
-
Ultraviolet radiation (UVR) and melanogenesis: Rothman was very interested in the effects of UVR on melanogenesis (Rothman, 1942). His studies of tanning suggested that tyrosine was photochemically converted to dihydroxyphenylalanine (dopa) by UVR, followed by the enzymatic conversion of dopa to dopaquinone with subsequent polymerization into melanin. He confirmed this by dissolving tyrosine in water and irradiating it with UVR and showing its conversion to dopa and then to melanin.
Today we know that the melanocyte-keratinocyte complex reacts to a wide range of stimuli to produce melanin. While UVR is the main trigger, many other signaling proteins, hormones and cytokines can be involved. After exposure to UVR, melanocytes increase their expression of proopiomelanocortin (precursor of melanocyte-stimulating hormone; POMC) and its receptor, but also tyrosinase and tyrosinase-related protein 1, as well as many other factors. Keratinocytes also release endothelin-1 and POMC, stimulating melanogenesis in a paracrine manner. Although the induction of melanogenesis is incredibly complex, Rothman was tantalizingly close with his emphasis on tyrosine (Costin and Hearing, 2007; Hearing, 2006).
-
Para-amino benzoic acid (PABA) as a sunscreen: Rothman originally thought that sunburn erythema in human skin was neurogenic in origin. To test this he injected the local anesthetic agent procaine into the skin of a human subject prior to UV irradiation and observed that the erythema response was decreased. Initially he concluded that sunburn requires intact sensory nerves but then showed that pre-treatment with cocaine had no effect on the erythema response. (Rothman, 1926). Ultimately he proved that procaine consists structurally of an ester of beta-diethyl amino ethanol acid and PABA and that it is the PABA component that strongly absorbs at 300nm. (Rothman and Rubin, 1942).
Rothman then conducted a clinical trial to verify the photoprotective efficacy of topical formulations containing PABA (Rothman and Henningsen, 1947), showing that areas treated with 15% PABA in a cream base were 50–100 times more resistant to sunburn than vehicle-treated area. He pointed out that PABA was non-irritating, non-soiling and stable during exposure to UVR. Twenty years later PABA’s photoprotective efficacy was confirmed on prisoners in the Arizona desert and volunteers on a Swiss glacier (Pathak et al., 1969). Numerous PABA-containing products enjoyed early commercial success. But it soon became clear that Rothman had been mistaken about PABA’s non-irritating nature, as it proved to be a potent contact allergen. It was then replaced by PABA esters and later by a wide variety of other chemicals. Modern sunscreens are now of two broad types--chemical and physical, providing good protection against both ultraviolet A and B (UVA and UVB) and represent extensions of the principles Rothman so ingeniously articulated decades ago.
High levels of iron in human red hair: Working with several pounds of natural red hair obtained from a barber college in Chicago, Flesch and Rothman extracted an iron-containing substance, which they named trichosiderin (Flesch and Rothman, 1945). They thus described melanin’s ability to bind metal ions, a property critical for many of the biological functions of these pigments including iron accumulation into dopaminergic neurons of the substantia nigra. Today we know that cysteine, which interacts with iron in many systems, is the compound that diverts eumelanin synthesis to pheomelanin (Napolitano et al., 2013). In the presence of cysteine, dopaquinone is converted stoichiometrically into 3- or 5-cysteinyldopa that oxidizes and polymerizes to pheomelanin, the red melanin that so interested Rothman.
Insensible water loss: Rothman was fascinated by insensible perspiration. He showed that transepidermal water loss (TEWL) was preferentially elevated in psoriasis—hyperproliferative hyperkeratosis—and decreased in ichthyosis vulgaris—retention hyperkeratosis (Felsher and Rothman, 1945). In addition to sweat and post-inflammatory epidermal alterations, Rothman was convinced that insensible water loss was intimately coupled to cornification, as the water content of maturing corneocytes drops from 70% to 10%. While his work antedated our current knowledge regarding cutaneous inflammation impairing skin barrier function due to reduced synthesis of barrier-related proteins (Feingold et al., 2007), he noted that insensible perspiration returned to normal levels with barrier restoration. While Rothman was a pioneer in recognizing the importance of TEWL, he over-emphasized the contribution of altered cornification to this process.
Allergic contact dermatitis to procaine: Procaine sensitivity became a major problem among dentists in Rothman’s era because they wore no gloves and the anesthetic was essential to their practice. Studying a 26-year-old dentist with contact allergy to procaine (Rothman et al., 1945), he devised skin tests to identify the allergenic components of procaine that as discussed above is an ester of PABA and beta-diethyl amino ethanol. Neither compound alone elicited a positive skin test reaction. He rigorously tested numerous chemical derivatives and showed that only PABA esters with secondary or tertiary amine side chains produced positive patch test reactions. Thus he elaborated the principle that contact allergens can cross-react stereochemically. These observations pointed the way to the development of quantitative structure-activity relationship (QSAR) analysis of chemical substances (Hasdenteufel et al., 2012).
Hardening to treat solar urticaria: Two patients with solar urticaria were given the antihistamine pyribenzamine 50 mg t.i.d. and then UV-irradiated. The drug dose was reduced after 37 UV treatments and then stopped after 54, while phototherapy continued. Phototesting confirmed that the urticarial threshold was increased 200-fold in irradiated skin as compared to a control site (Rubin et al., 1947). The mechanism proposed was thickening of the stratum corneum, rather than some immunological effect. The combination of oral antihistamines and phototherapy remains the treatment of choice for solar urticaria (Beissert et al., 2000); rush hardening may provide an alternative approach (Masuoka et al., 2012).
Skin testing to enhance diagnosis of late syphilis: He postulated that individuals with latent syphilis and negative serologies would respond to intradermal injection of purified Treponema pallidum by converting to positive treponemal tests, while normal controls and biological false-positive individuals would not (Pearson et al., 1958; Rothman and Marshak, 1951). Skin testing for the diagnosis of late syphilis was one of Rothman’s few unsuccessful ideas.
-
Skin surface lipids: Rothman was fascinated by skin surface lipids and collaborated with Konrad Bloch (1912–2000) who won the Nobel Prize for Medicine in 1964 for his work on cholesterol and fatty acid synthesis. His group showed that cholesterol synthesis was blocked at squalene in sebaceous glands, but proceeded to cholesterol in the epidermis (Nicolaides and Rothman, 1955). Rothman had noticed that mid-length free fatty acid chains especially those with 11 carbon atoms had antifungal properties. He contacted László Reiner, a childhood friend from Budapest, who was a biochemist and head of research at Wallace and Tiernan in Belleville, New Jersey. Reiner suggested castor oil as a commercial source of undecylenic acid which his firm compounded and successfully marketed as the topical antifungal agent Desenex (Rothman and Shapiro, 1945). In addition, Rothman deduced that at puberty scalp sebum free fatty acid levels increased and inhibited Microsporum audouinii, explaining why anthrophilic tinea capitis disappears during adolescence (Rothman et al., 1946).
Today we appreciate that keratinocyte-derived cholesterol comprises 25% of the lipids of lamellar membranes and is essential for epidermal barrier function (Feingold and Elias, 2014). Lauric acid and sapienic acid derived from human sebaceous triglycerides, as well as skin long-chain bases (sphingosine, dihydrosphingosine and 6-hydroxysphingosine) are potent antimicrobial agents (Fischer et al., 2014). Rothman’s work foreshadowed these insights into barrier function, antimicrobial cutaneous defense and regulation of innate immunity.
Immunotherapy of alopecia areata: Dillaha and Rothman reported that patients with alopecia areata (AA) responded to systemic cortisone (Dillaha and Rothman, 1952a, b).. The usual dose was 150 mg daily of cortisone acetate; lower doses were ineffective and continuous therapy was required. Today AA is considered a T-cell–mediated autoimmune disease in which the gradual loss of protection provided by immune privilege of the normal hair follicle drives the pathologic process (Gilhar and Kalish, 2006).. Using the approach of Genome Wide Association Studies (GWAS) Angela Christiano’s group has identified a set of disease susceptibility genes, as well as a series of novel markers that are targetable by available drugs (Petukhova and Christiano, 2013). Their efficacy has been verified in mouse models of AA and now clinical trials assessing the efficacy of abatacept, a fusion protein that down-regulates T-cell activity, as well as the Janus kinase (JAK) inhibitors ruxolitinib and tofacitinib are underway..
Role of progesterone and other hormones in regulating sebaceous gland size and activity: He published a series of prescient articles on sebaceous glands in white rats showing that testosterone increased sebaceous gland volume via hyperplasia, not just hypertrophy; that the effect of adrenocorticotropic hormone (ACTH) depended on an intact pituitary-adrenal axis (Haskin et al., 1953; Lasher et al., 1954). and that there was an unidentified pituitary gland sebaceous trophic factor Five decades later testosterone and its metabolite 5α-dihydrotestosterone were found to markedly stimulate human sebaceous gland cell proliferation (Akamatsu et al., 1992), binding to steroidogenic receptors (Fritsch et al., 2001) and inducing sebocyte differentiation and lipogenesis (Makrantonaki and Zouboulis, 2007). Rothman’s unidentified pituitary gland sebaceous trophic factor (Lasher et al., 1955) may have been corticotropin-releasing hormone (CRH) (Zouboulis et al., 2002).
In addition to these scientific achievements, Rothman summarized the potential negative consequences of these discoveries that continue to challenge us (Rothman, 1961). He predicted that indiscriminate use of topical antibiotics would increase the risk of skin sensitization as well as promote bacterial resistance. He foresaw that some drugs, hormones and vitamins would become promoted for dubious indications and anticipated the advent of “skin rejuvenation” modalities all too often associated with exaggerated claims. He also emphasized the need for good medical judgment in treating dermatologic conditions such as acne, warning against leaving patient care in the hands of pharmacists, patients and parents making uninformed choices of non-prescription medications. Rothman never received a penny in royalties for his landmark discoveries of PABA sunscreens and undecylenic acid antifungal agents that continue to have annual sales in the billions of dollars.
The Society for Investigative Dermatology has honored Rothman in two ways:
Rothman started the Dermatology Research Club, a group of young researchers who met during the annual meeting of the American Academy of Dermatology. The club was renamed The Stephen Rothman Club and Rothman was the first person over the age limit of 44 allowed to attend. For many years, the club met to celebrate Rothman and to introduce young investigators to in a relaxed social setting to enhance collegiality, networking and potential collaborations.
The Stephen Rothman Medal (Figure 2) is awarded by the SID to recognize singular achievement in investigative dermatology. The first recipient was Marion B. Sulzberger in 1967.
Figure 2.
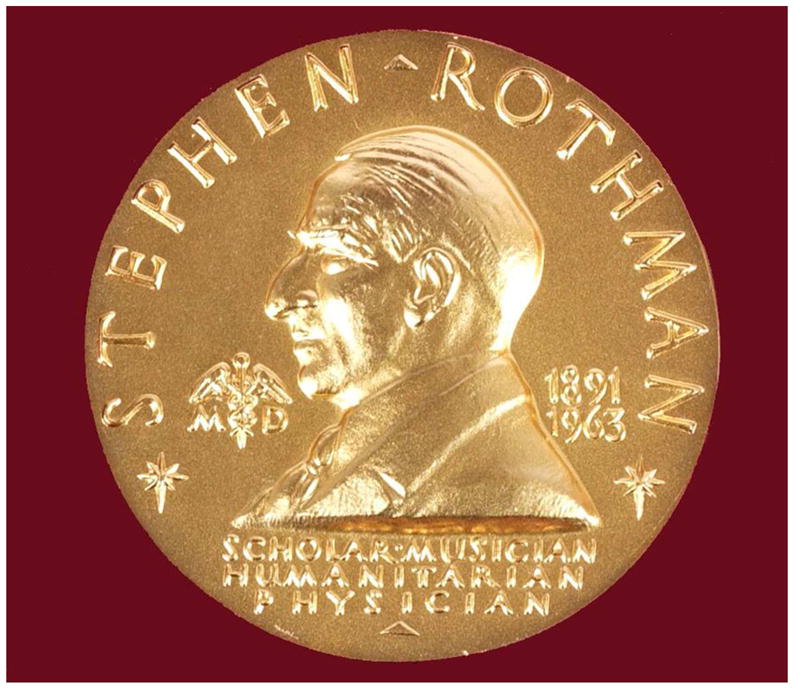
Stephen Rothman Medal (courtesy of Georg Stingl, MD, Vienna, Austria; recipient of the award in 2003)
In summary, Rothman was a true pioneer in establishing the scientific basis of cutaneous biology/investigative dermatology. His credo regarding basic research was described in his SID presidential address (Rothman, 1949):
“Basic research in medicine can be defined as research with the purpose of unravelling simple elementary biological facts. It need not have the purpose of applying the resulting knowledge to a clinical problem. As a matter of fact, in basic research we never know in advance whether there will be any application, or if there is any, when it will come or to what it will apply. Basic research is inconceivable without experimentation because simplification of complicated natural phenomena requires establishment of arbitrarily chosen conditions.”
This was his mantra and his bequest to us and his words are as relevant today as they were when uttered in 1949.
Acknowledgments
The following colleagues helped us re-interpret Rothman’s experimental findings: Donald V. Belsito, New York City; Angela Christiano, New York City; Edgar Frenk, Lausanne, Switzerland; Alexandra Geusau, Vienna, Austria; Percy Lehmann, Wuppertal, Germany; Bodo Melnik, Osnabrück, Germany; Alessandra Napolitano, Naples, Italy; James J. Nordlund, Cincinnati, Ohio; Matthias Schmuth, Innsbruck, Austria; Martin Steinhoff, Dublin, Ireland; Christos C. Zouboulis, Dessau, Germany.
Abbreviations
- AA
alopecia areata
- Ach
acetylcholine
- ACTH
adrenocorticotropic hormone
- CRH
corticotropin-releasing hormone
- dopa
dihydroxyphenylalanine
- JAK
Janus kinase
- JID
Journal of Investigative Dermatology
- PABA
para-aminobenzoic acid
- POMC
precursor of melanocyte-stimulating hormone
- QSAR
quantitative structure- activity relationship
- TEWL
transepidermal water loss
- UVA
ultraviolet A
- UVB
ultraviolet light B
- UVR
ultraviolet radiation
Footnotes
Conflict of Interest
The authors state no conflict of interest.
Contributor Information
Walter H. C. Burgdorf, Email: wburgdorf@gmx.de.
David R. Bickers, Email: drb25@columbia.edu.
References
- Physiology and Biochemistry of the Skin. Arch Dermatol Syphilol. 1954;70:549–50. [Google Scholar]
- Physiology and Biochemistry of the Skin. Brit J Dermatol. 1955;67:31. [Google Scholar]
- Akamatsu H, Zouboulis CC, Orfanos CE. Control of human sebocyte proliferation in vitro by testosterone and 5-alpha-dihydrotestosterone is dependent on the localization of the sebaceous glands. J Invest Dermatol. 1992;99:509–11. doi: 10.1111/1523-1747.ep12616181. [DOI] [PubMed] [Google Scholar]
- Beissert S, Stander H, Schwarz T. UVA rush hardening for the treatment of solar urticaria. J Am Acad Dermatol. 2000;42:1030–2. doi: 10.1016/s0190-9622(00)90299-8. [DOI] [PubMed] [Google Scholar]
- Burgdorf WH, Bickers DR. Dermatologic relationships between the United States and German-speaking countries: part 3--the Europeans come to the United States. JAMA Dermatol. 2013;149:1217–20. doi: 10.1001/jamadermatol.2013.5783. [DOI] [PubMed] [Google Scholar]
- Costin GE, Hearing VJ. Human skin pigmentation: melanocytes modulate skin color in response to stress. FASEB J. 2007;21:976–94. doi: 10.1096/fj.06-6649rev. [DOI] [PubMed] [Google Scholar]
- Curtis BJ, Radek KA. Cholinergic regulation of keratinocyte innate immunity and permeability barrier integrity: new perspectives in epidermal immunity and disease. J Invest Dermatol. 2012;132:28–42. doi: 10.1038/jid.2011.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dillaha CJ, Rothman S. Therapeutic experiments in alopecia areata with orally administered cortisone. JAMA. 1952a;150:546–50. doi: 10.1001/jama.1952.03680060018006. [DOI] [PubMed] [Google Scholar]
- Dillaha CJ, Rothman S. Treatment of alopecia areata totalis and universalis with cortisone acetate. J Invest Dermatol. 1952b;18:5–6. doi: 10.1038/jid.1952.3. [DOI] [PubMed] [Google Scholar]
- Everett MA. Stephan Rothman (1894–1963) In: Löser C, Plewig G, Burgdorf WHC, editors. Pantheon of Dermatology: Outstanding Historical Figures. Heidelberg: Springer; 2013. pp. 967–71. [Google Scholar]
- Feingold K, Elias P. The important role of lipids in the epidermis and their role in the formation and maintenance of the cutaneous barrier. Biochim Biophys Acta. 2014;1841:280–94. doi: 10.1016/j.bbalip.2013.12.004. [DOI] [PubMed] [Google Scholar]
- Feingold KR, Schmuth M, Elias PM. The regulation of permeability barrier homeostasis. J Invest Dermatol. 2007;127:1574–6. doi: 10.1038/sj.jid.5700774. [DOI] [PubMed] [Google Scholar]
- Felsher Z, Rothman S. The insensible perspiration of the skin in hyperkeratotic conditions. J Invest Dermatol. 1945;6:271–8. [Google Scholar]
- Fischer CL, Blanchette DR, Brogden KA, et al. The roles of cutaneous lipids in host defense. Biochim Biophys Acta. 2014;1841:319–22. doi: 10.1016/j.bbalip.2013.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flesch P, Rothman S. Isolation of an iron pigment from human red hair. J Invest Dermatol. 1945;6:257–70. [Google Scholar]
- Fritsch M, Orfanos CE, Zouboulis CC. Sebocytes are the key regulators of androgen homeostasis in human skin. J Invest Dermatol. 2001;116:793–800. doi: 10.1046/j.1523-1747.2001.01312.x. [DOI] [PubMed] [Google Scholar]
- Gilhar A, Kalish RS. Alopecia areata: a tissue specific autoimmune disease of the hair follicle. Autoimmun Rev. 2006;5:64–9. doi: 10.1016/j.autrev.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Goldsmith LA, editor. Biochemistry and Physiology of the Skin. Oford University Press; New York: 1983. [Google Scholar]
- Hasdenteufel F, Luyasu S, Hougardy N, et al. Structure-activity relationships and drug allergy. Curr Clin Pharmacol. 2012;7:15–27. doi: 10.2174/157488412799218815. [DOI] [PubMed] [Google Scholar]
- Haskin D, Lasher N, Rothman S. Some effects of ACTH, cortisone, progesterone and testosterone on sebaceous glands in the white rat. J Invest Dermatol. 1953;20:207–12. doi: 10.1038/jid.1953.24. [DOI] [PubMed] [Google Scholar]
- Hearing VJ. The regulation of melanin formation. In: Nordlund JJ, Boissy RE, Hearing VJ, King RA, Oetting WS, Ortonne JP, editors. Pigmentary System: Physiology and Pathophysiology. Oxford: Blackwell; 2006. pp. 191–212. [Google Scholar]
- Heyer G, Vogelgsang M, Hornstein OP. Acetylcholine is an inducer of itching in patients with atopic eczema. J Dermatol. 1997;24:621–5. doi: 10.1111/j.1346-8138.1997.tb02305.x. [DOI] [PubMed] [Google Scholar]
- Lasher N, Lorincz AL, Rothman S. Hormonal effects on sebaceous glands in the white rat. II. The effect of the pituitary-adrenal axis. J Invest Dermatol. 1954;22:25–9. doi: 10.1038/jid.1954.6. [DOI] [PubMed] [Google Scholar]
- Lasher N, Lorincz AL, Rothman S. Hormonal effects on sebaceous glands in the white rat. III. Evidence for the presence of a pituitary sebaceous gland tropic factor. J Invest Dermatol. 1955;24:499–505. doi: 10.1038/jid.1955.69. [DOI] [PubMed] [Google Scholar]
- Lorincz AL. Dr. Stephen Rothman. J Invest Dermatol. 1958;31:1–9. doi: 10.1038/jid.1958.66. [DOI] [PubMed] [Google Scholar]
- Lorincz AL. Stephen Rothman, MD, 1894–1963. Arch Dermatol. 1964;89:167–9. doi: 10.1001/archderm.1964.01590260005001. [DOI] [PubMed] [Google Scholar]
- Low DA, Hubing KA, Del Coso J, et al. Mechanisms of cutaneous vasodilation during the postmenopausal hot flash. Menopause. 2011;18:359–65. doi: 10.1097/gme.0b013e3181f7a17a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makrantonaki E, Zouboulis CC. Testosterone metabolism to 5alpha-dihydrotestosterone and synthesis of sebaceous lipids is regulated by the peroxisome proliferator-activated receptor ligand linoleic acid in human sebocytes. Br J Dermatol. 2007;156:428–32. doi: 10.1111/j.1365-2133.2006.07671.x. [DOI] [PubMed] [Google Scholar]
- Masuoka E, Fukunaga A, Kishigami K, et al. Successful and long-lasting treatment of solar urticaria with ultraviolet A rush hardening therapy. Br J Dermatol. 2012;167:198–201. doi: 10.1111/j.1365-2133.2012.10944.x. [DOI] [PubMed] [Google Scholar]
- Napolitano A, Panzella L, Leone L, et al. Red hair benzothiazines and benzothiazoles: mutation-inspired chemistry in the quest for functionality. Acc Chem Res. 2013;46:519–28. doi: 10.1021/ar300219u. [DOI] [PubMed] [Google Scholar]
- Nicolaides N, Rothman S. The site of sterol and squalene synthesis in the human skin. J Invest Dermatol. 1955;24:125–9. doi: 10.1038/jid.1955.20. [DOI] [PubMed] [Google Scholar]
- Pathak MA, Fitzpatrick TB, Frenk E. Evaluation of topical agents that prevent sunburn--superiority of para-aminobenzoic acid and its ester in ethyl alcohol. N Engl J Med. 1969;280:1459–63. doi: 10.1056/NEJM196906262802607. [DOI] [PubMed] [Google Scholar]
- Pearson RW, Portnoy J, Magnuson HJ, et al. The combined use of treponemin skin testing and specific serological tests in the diagnosis of syphilis. J Invest Dermatol. 1958;31:75–81. [PubMed] [Google Scholar]
- Petukhova L, Christiano AM. The genetic architecture of alopecia areata. J Investig Dermatol Symp Proc. 2013;16:S16–22. doi: 10.1038/jidsymp.2013.5. [DOI] [PubMed] [Google Scholar]
- Roosterman D, Goerge T, Schneider SW, et al. Neuronal control of skin function: the skin as a neuroimmunoendocrine organ. Physiol Rev. 2006;86:1309–79. doi: 10.1152/physrev.00026.2005. [DOI] [PubMed] [Google Scholar]
- Rothman FG, Lorincz AL. Stephen Rothman, pioneer of investigative dermatology. Perspect Biol Med. 1995;39:93–109. doi: 10.1353/pbm.1995.0040. [DOI] [PubMed] [Google Scholar]
- Rothman S. Die Beeinflussung der Lichtentzündung und der Pigmentierung durch Novokaineinspritzungen (The effect of novacaine injections on light-induced erythema and pigmentation) Strahlentherapie. 1926;22:729–35. [Google Scholar]
- Rothman S. In vitro studies on pigmentation. I. The oxidation of tyrosine by ultraviolet light. J Invest Dermatol. 1942;5:61–7. [Google Scholar]
- Rothman S. Basic research in dermatology. J Invest Dermatol. 1949;13:165–70. doi: 10.1038/jid.1949.84. [DOI] [PubMed] [Google Scholar]
- Rothman S. Physiology and Biochemistry of the Skin. University of Chicago; Chicago: 1954. p. 741. [Google Scholar]
- Rothman S. Drugs in cosmetics. JAMA. 1961;178:38–42. doi: 10.1001/jama.1961.03040400040008. [DOI] [PubMed] [Google Scholar]
- Rothman S, Coon JM. Axon reflex responses to acetylcholine in the skin. J Invest Dermatol. 1940;3:79–97. [Google Scholar]
- Rothman S, Henningsen AB. The sunburn-protecting effect of para-aminobenzoic acid. J Invest Dermatol. 1947;9:307–13. doi: 10.1038/jid.1947.103. [DOI] [PubMed] [Google Scholar]
- Rothman S, Marshak LC. Skin testing with a purified suspension of Treponema pallidum. Am J Syph Gonorrhea Vener Dis. 1951;35:35–41. [Google Scholar]
- Rothman S, Orland FJ, Flesch P. Group specificity of epidermal allergy to procaine in man. J Invest Dermatol. 1945;6:191–9. [Google Scholar]
- Rothman S, Rubin J. Sunburn and para-aminobenzoic acid. J Invest Dermatol. 1942:5. doi: 10.1038/jid.1947.103. [DOI] [PubMed] [Google Scholar]
- Rothman S, Shapiro AL. Undecylenic acid in the treatment of dermatomycosis. Arch Dermatol Syphilol. 1945;52:166–71. doi: 10.1001/archderm.119.4.345. [DOI] [PubMed] [Google Scholar]
- Rothman S, Smiljanic AM, Weitkamp AW. Mechanism of spontaneous cure in puberty of ringworm of the scalp. Science. 1946;104:201–3. [PubMed] [Google Scholar]
- Rubin L, Beal PL, Rothman S. A method for protection of patients with solar urticaria. J Invest Dermatol. 1947;8:189. doi: 10.1038/jid.1947.25. [DOI] [PubMed] [Google Scholar]
- Shibasaki M, Davis SL, Cui J, et al. Botulinum toxin abolishes sweating via impaired sweat gland responsiveness to exogenous acetylcholine. Br J Dermatol. 2009;161:757–61. doi: 10.1111/j.1365-2133.2009.09248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zouboulis CC, Seltmann H, Hiroi N, et al. Corticotropin-releasing hormone: an autocrine hormone that promotes lipogenesis in human sebocytes. Proc Natl Acad Sci U S A. 2002;99:7148–53. doi: 10.1073/pnas.102180999. [DOI] [PMC free article] [PubMed] [Google Scholar]


