Summary
Trapping of muscle metabolites in forearm tissues worsens overall fatigue of CFS patients more than that of NC suggesting sensitized fatigue pathways in CFS.
Keywords: Ischemic Occlusion, Metabolites, Chronic Fatigue, Handgrip, Dynamometer
1. Introduction
Chronic fatigue syndrome (CFS) is a complex illness characterized by severe and prolonged disabling fatigue not alleviated by rest [14]. Additional symptoms include sleep disturbance, musculoskeletal pain, attention and short-term memory impairments [8]. For many years it has been suspected that “tiredness” and muscle pain could be elicited by metabolites produced during muscle contractions [1] but little was known about the mechanism of fatigue signaling. Since the 1990s, acid-sensing ion channels (ASICs) [53; 54] and transient receptor potential channel V1 (TRPV1) [23] were implicated as important metabo-receptors for peripheral metabolites like hydrogen ions and lactic acid [15]. However, only after it was discovered that ATP can enhance the sensitivity of ASICs to protons and lactate [35; 57] thus allowing them to gate sustained currents able to activate sensory nerve endings, the existence of metabo-receptors appeared to be firmly established. Subsequently, nerve endings containing ASICs have been detected on the outside of small arterioles and venules of fascia surrounding muscles bundles [6; 33], readily accessible to muscle produced metabolites [11].
Because one of the hallmarks of CFS is often long-lasting fatigue after minor physical exertion we hypothesized that muscle metabolites activate fatigue pathways and thus contribute to this phenomenon. This hypothesis appeared reasonable because pain and fatigue pathways seem to share similar receptors systems (i.e. ASIC, TRPV1, P2X) and sensitization of pain pathways of CFS patients during exercise has been reported previously [55]. Whereas healthy normal controls (NC) demonstrated increased pain thresholds, CFS patients showed incremental reduction in pain thresholds after modest exercise [55]. Normally, exercise increases pain threshold due to endogenous pain modulation including the release of endogenous opioids and growth factors [19]. We hypothesized that trapping of muscle metabolites in the forearms of CFS patients and NC after vigorous handgrip exercise would increase overall fatigue and thus provide indirect evidence for metabolite-induced activation of fatigue receptors and sensitization of fatigue pathways. We also tested CFS patients’ heat and mechanical hyperalgesia for possible interactions with exercise induced fatigue.
2. Methods
The University of Florida Institutional Review Board approved all procedures described in this report. Informed consent was obtained from all subjects, and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
2.1 Study Subjects
NC came from the local community. CFS subjects were recruited at the Health Science Center Outpatient Clinics and through TV advertising. The diagnosis of CFS was made by an experienced rheumatologist (R.S.) according to the 1994 International Research Case Definition (Fukuda Criteria) [8]. Chronically fatigued subjects were excluded from the study if they had any other significant diagnosis outside of CFS, specifically chronic muscle disease, major depression, or cancer. Use of analgesics, including non-steroidal anti-inflammatory drugs (NSAID), tramadol, and acetaminophen, was not allowed during the study. No subject was taking narcotic analgesics during the trial. Medication needed for treatment of chronic medical conditions, like hypertension or hypothyroidism were permitted during the study
2.2 Experimental Design
This study was designed to provide indirect evidence for the contributions of muscle metabolites to clinical fatigue. At least some of these metabolites, like H+, lactic acid, and ATP are known to not only activate metabo-receptors but also pain receptors (ASIC, TRPV1, P2X) [15; 23; 53; 54]. Therefore we also investigated the impact of experimental pain on fatigue using mechanical and heat stimuli suited for characterizing mechanical and heat pain sensitivity of study subjects.
2.2.1 Testing of Heat and Mechanical Hyperalgesia
Because individuals with CFS frequently report chronic pain [4; 28] all study subjects were evaluated for heat and mechanical hyperalgesia. Before the handgrip exercises several trains of 10 s heat or mechanical stimuli that predominantly activate C-fibers [42; 43; 58; 59] were applied to the center of the forearms for testing of heat and mechanical hyperalgesia of the study subjects. Stimulus intensities were chosen that have been well tolerated by hyperalgesic subjects in previous quantitative sensory testing protocols [47; 48]. The effect of tonic experimental heat and mechanical pain stimuli on clinical fatigue was tested at the forearms of study subjects.
2.2.2 Exercise Testing
In a cross-over design, all subjects underwent handgrip exercises to exhaustion followed by forearm occlusion or control condition, separated by approximately 30 min. Each handgrip exercise was immediately followed by forearm occlusion or control condition of identical duration. This way maximal metabolite production was likely as forearm occlusion during exercise causes significant pain thus limiting exercise duration. During the exercise the subjects rated the intensity of their perceived exertion on a Borg Scale every 30 s. Similarly, they were asked to rate the intensity of their pain using the VAS every 30 s.
Handgrip Exercise
To establish maximal handgrip force for either hand, the subjects were seated at a table. After they rested their exercising forearm comfortably on the table surface, they firmly gripped a Jamar Dynamometer (TEC, Clifton, NJ) with one hand compressing it at maximal force × 3 in intervals of 1 min. The dial of the dynamometer was visible in a mirror facing the subject, and both the subject as well as the investigator could visualize the force read-out with every squeeze. Subsequently, for the handgrip exercise, the subjects were asked to compress the dynamometer at 50% of their average maximal handgrip force and release it synchronized to recorded voice commands of “squeeze” or “release” every 1.5 s. During the exercise the subjects were asked to rate the level of their perceived exertion and their overall pain every 30 s. The participants were strongly encouraged by the experimenter to exercise to complete exhaustion. Overall fatigue ratings were obtained at baseline, end of the hand grip exercise, after the forearm occlusion or control condition, and at the end of the experiment (Figure 1)
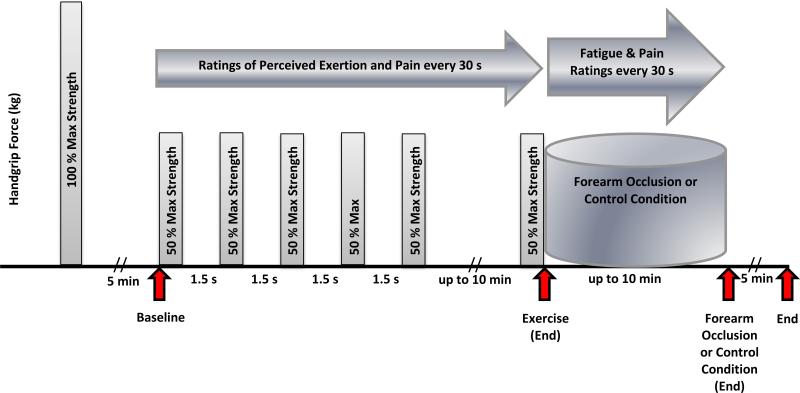
Figure 1.
Experimental Design of Handgrip Exercise Testing: Handgrip exercise to exhaustion was performed by all subjects using a cross-over design. After maximal grip strength had been established, each participant exercised at 50 % maximal grip strength for up to 10 min followed by forearm occlusion or the control condition in counterbalanced order. Complete forearm occlusions for up to 10 min were always done on the dominant arm after the handgrip exercise using a blood pressure cuff. During the control condition, a non-inflated blood pressure cuff was tightly wrapped around the upper part of the exercised extremity for up to 10 min serving as control condition. The red arrows represent time points at which overall fatigue ratings were obtained from all participants at baseline, after handgrip exercise, after forearm occlusion (or control condition), and at the end of the experiment.
Forearm Occlusion
For this experiment a Hokanson E20 Rapid Cuff Inflation System (Hokanson, WA) was used. This instrument can inflate a blood pressure cuff placed around the upper arm in 0.3 s with pressures of 200 mg Hg and maintain this level for the duration of the experiment, resulting in complete occlusion of blood flow to the forearm. Forearm occlusion was initiated immediately after the end of the handgrip exercise while the extremity remained resting on the table. Ratings of overall fatigue and pain were obtained every 30 s. At the end of the forearm occlusion the pressure of the blood pressure cuff was rapidly reduced and full circulation was re-established (Figure 1).
2.3 Testing of Mechanical and Heat Sensitivity
2.3.1 Thermal Probe
A Peltier thermode with a contact surface of 3 × 3 cm (9 cm2) (Pathways, Medoc Advanced Medical Systems, Ramat Yishai, Israel) was used for the heat stimuli. For heat pain testing the probe was brought into firm contact with the skin of the forearm for 10 s.
2.3.2 Heat Pain Stimuli
Experimental heat pain was elicited by 10 s pulses to the skin overlying the forearms. In order to preferentially activate C-fiber afferents the Peltier probe was programmed to gradually increase from warmth (38°C) to target temperature within 6 s. Subsequently, it remained at peak temperature for 4 s for a total stimulus duration of 10 s. Stimulus intensities included 46°C and 48°C. Three 10 s heat pulses each were applied to each forearm in counterbalanced order. The interval between heat pulses was at least 30 s or until pain aftersensations had ceased. All subjects rated the intensity of heat pain at the end of each stimulus using the VAS.
2.3.3 Mechanical Probe
A calibrated electronic algometer (Algomed, Medoc Advanced Medical System, Ramat Yishai, Israel) was utilized for the pressure stimuli. The rubber tip of the algometer was 1 cm in diameter. The algometer has an electronic display for pressure readings (kPa) as well as a serial connection to a laptop displaying the pressure applied to the forearm by the investigator in real time.
2.3.4 Mechanical Pain Stimuli
Two trains of three 10 s pressure stimuli were applied in counterbalanced order to each forearm. After the algometer was placed on the target area, pressure was gradually increased to 200 kPa or 400 kPa. The pressure increase ranged from 33 kPa/s for 200 kPa to 67 kPa/s for 400 kPa stimuli to reach peak pressure within 6 s. Subsequently, peak pressure was maintained for an additional 4 s. The subjects provided pressure pain ratings at the end of the stimulus. The interval between mechanical stimuli was at least 30 s or until pain aftersensations had ceased. The intensity of pressure pain was rated at the end of each stimulus using the VAS.
2.4 Ratings of Clinical and Experimental Pain and Fatigue
A 15 cm mechanical VAS (0 – 10) was utilized for ratings of clinical and experimental pain and fatigue during the experiments [41]. The scales are anchored on the left with “no fatigue (pain) at all” and on the right with “the most intense fatigue (pain) imaginable”. If necessary, the VAS scale was fastened with Velcro straps to a stable surface to be used with one hand. Although NC subjects were required to be pain free at enrollment, they were asked to rate any somatic pains before and after testing session to capture possible new onset symptoms like back pain, headaches, etc.
2.5 Borg Rating Scale of Perceived Exertion (RPE)
The Borg scale is an interval scale ranging from 6 to 20, where 6 means “no exertion at all” and 20 “maximal exertion” [2]. Participants were asked to select the number from the Borg scale that best described their level of exertion. All participants were asked to verbally rate their level of exertion during handgrip exercises. They were instructed that their rating of perceived exertion should reflect how heavy and strenuous the exercise felt, including all sensations and feelings of physical stress, effort, and fatigue. No single factor such as arm or shoulder pain or shortness of breath should dominate their exertion rating, instead they were asked to focus on their total feeling of exertion
2.6 Data Analysis
Statistical analyses were calculated using SPSS 21.0 software (IBM, Inc., Chicago, IL). Demographic data were analyzed with independent t-tests (two tailed). For comparisons of exercise related data two-way and three-way repeated measure ANOVAs were used. Significance levels were set at alpha < .05. Significant differences between groups were always decomposed with independent t-tests (two tailed) and effect sizes reported for each analysis. Our analytic plan focused on a-priori hypotheses. As the omnibus ANOVAs for these hypotheses were all statistically reliable, and thus well above that expected by chance we chose not to apply correction for multiple comparisons that tend to be excessively conservative and might have obscured findings that were targeted a priori. We provided effect sizes in addition to descriptive statistics, and significance values to allow the reader to evaluate the meaningfulness of statistically significant findings
3. Results
3.1 Study Participants
We enrolled 21 NC subjects (20 females) and 39 subjects with CFS (31 females) into the study. Whereas all NC subjects were recruited through advertising, 67 % of all CFS subjects came from University of Florida outpatient clinics. 37% of CFS subjects came from TV advertising. All CFS subjects fulfilled the 1994 International Research Case Definition (Fukuda Criteria) [8]. The mean age (SD) of study participants was 38.9 (16.8) and 45.7 (13.5) for NC and CFS subjects, respectively. An independent t-test demonstrated no significant age differences between the groups (p > .05).
3.2 Handgrip Exercise
All participants performed handgrip exercises to maximal exertion at 50% maximal force once with their dominant or non-dominant hand, in cross-over fashion and counterbalanced order (Figure 1). Subsequent complete forearm occlusions for trapping of exercise related metabolites were always done on the dominant arm (handgrip exercise + forearm occlusion = Occlusion Condition) as the dominant forearm generally has more muscle mass than the non-dominant forearm [36]. After exercising the non-dominant hand forearm occlusion was not performed but data were collected for the same amount of time as during the forearm occlusion. This served as a control for the forearm occlusion of the opposite forearm (Control Condition).
3.2.1 Estimates of Maximal Handgrip Force and Ratings of Perceived Exertion
During the occlusion condition the CFS and NC participants maximally compressed the dynamometer with their dominant hand using an average force of 26.1 (10.1) and 28.2 (9.6) kg, respectively (p > .05). Subsequent repeated handgrip squeezes at 50% maximal force were performed for 6.6 (2.4) and 7.0 (2.7) min by NC and CFS subjects, respectively (p > .05). During the handgrip exercises average ratings of perceived exertion increased from 0 to 16.5 (1.4) for NC and to 16.8 (1.8) Borg units for CFS participants (p >.05). Maximal forearm pain during the exercise was rated as 1.6 (1.6) VAS units by NCs and as 4.2 (2.2) VAS units by CFS subjects (t = 5.6; df 50; p < .001).
During the control condition the CFS and NC participants maximally compressed the dynamometer with their non-dominant hand using an average force of 26.0 (7.2) and 26.4 (9.2) kg, respectively (p > .05). Subsequent handgrip exercises at 50% maximal force were performed for 5.8 (2.2) and 6.8 (2.7) min by NC and CFS subjects, respectively (p > .05). During the handgrip exercises exertion ratings increased from 0 to 16.9 (.7) for NC and to 16.8 (1.8) Borg units for CFS participants (p >.05). Maximal forearm pain during the exercise was rated as 1.6 (1.6) VAS units by NCs and as 4.2 (2.2) VAS units by CFS subjects (t = 4.9; df 86; p < .001).
A repeated measures ANOVA with condition (2) and exercise (max grip force, max exertion, exercise duration) as within and diagnostic group (2) as between factors demonstrated a significant main effect for exercise ((F2,116) = 251.7; p < .001) but non-significant main effects for condition (p > .05; ηp2= .03) and diagnostic group (p > .05; ηp2= .02). All interaction effects were also non-significant (p > .05) demonstrating that exercise results were neither different between the occlusive and non-occlusive conditions nor between diagnostic groups
3.2.2 Comparison of Occlusion Condition and Control Condition on Fatigue
Fatigue ratings of NC and CFS participants were obtained at 4 time points during the occlusion condition (see 3.2.2.1) and the control condition (see 3.2.2.2), including a) at baseline; b) at the end of handgrip exercises; c) end of forearm occlusion or control condition; d) at the end of experiment (see Figure 1). A series of ANOVAs was performed modeling the effects of these experimental manipulations on fatigue as a cubic function. In the first analysis fatigue ratings obtained during the exercise + forearm occlusion were compared with ratings obtained during the control condition (exercise + rest). Subsequent ANOVAs were used to decompose interaction effects. The initial analysis comprised a 3-way mixed model ANOVA with condition (2) and exercise manipulations (4) as within and group (2) as between subjects’ factors which demonstrated a significant main effect of exercise manipulations ((F3,177) = 4.2; p = .007) and group ((F1,59) = 154.4; p < .001) but also a non-significant effect of condition ((F1,59) = 2.6; p > .05; ηp2= .04), However, the condition × exercise manipulation interaction effect was highly significant ((F3,177) = 8.3; p < .001: ηp2= .12) indicating that the fatigue changes observed during the forearm occlusion was statistically different from the fatigue changes associated with the control condition (Figure 6 A and B).
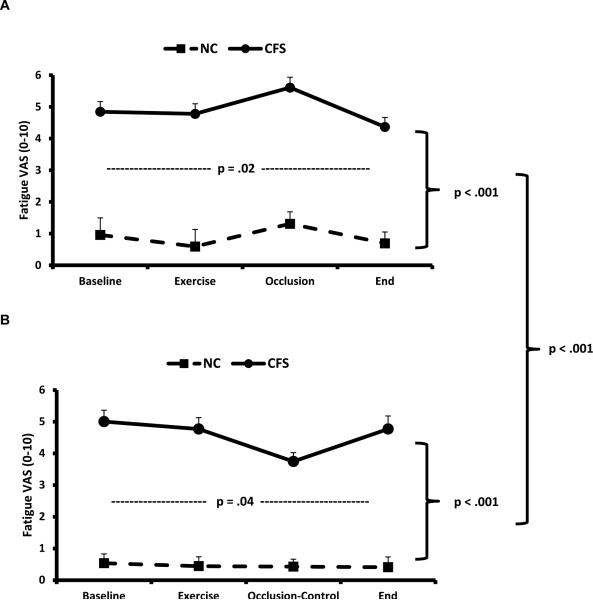
Figure 6.
All NC and CFS subjects performed handgrip exercises to maximal exertion followed A) by complete forearm occlusion to trap exercise related metabolites or B) by a non-occlusive control condition. All subjects rated their overall fatigue at baseline, after handgrip exercise, after forearm occlusion (or control condition), and at the end of the experiment.
A: During the exercise + forearm occlusion experiment average (SEM) fatigue ratings of CFS participants significantly increased from the end of exercise to the end of the occlusion period, followed by a reduction in fatigue ratings at the end of the experiment (p = .02). NC demonstrated a similar time course of fatigue ratings albeit of lesser magnitude. The fatigue ratings of CFS subject were significantly higher than NC (p < .001) indicating sensitization of fatigue pathways of CFS participants.
B: In contrast, during the exercise + control condition, average (SEM) fatigue ratings of CFS subjects significantly decreased from baseline to the end of the control condition (p = .04). Again NC showed a similar time course of fatigue ratings but of lesser magnitude (p < .001) demonstrating sensitization of fatigue pathways of CFS subjects. The time course of fatigue ratings during the exercise + forearm occlusion (A) was statistically different from the time course of fatigue ratings during the exercise + control condition (B) in CFS patients and NC (p < .001).
3.2.2.1 Occlusion Condition
Average (SD) fatigue ratings of NC and CFS subjects changed after handgrip exercise from baseline of 1.0 (1.9) to 0.6 (1.9) VAS units in NC and from 4.8 (2.0) to 4.9 (2.0) units in CFS participants (Figure 2 A). Subsequent forearm occlusion increased fatigue ratings to 1.3 (1.6) VAS units in NC and to 5.6 (2.1) VAS units in CFS subjects. At the end of the experiment the fatigue ratings of NC and CFS participants were .7 (1.3) and 4.4 (1.9) VAS units, respectively. A mixed model ANOVA with time (3) as within and diagnostic group (2) as between factors demonstrated a significant main effect of time ((F3,49) = 6.1; p = .02) and diagnostic group ((F1,49) = 65.8; p < .001). The time × diagnostic group interaction effect, however was non-significant ((F3, 49) = .4; p > .05; ηp2= .008), indicating that the fatigue changes were similar between NC and CFS subjects.
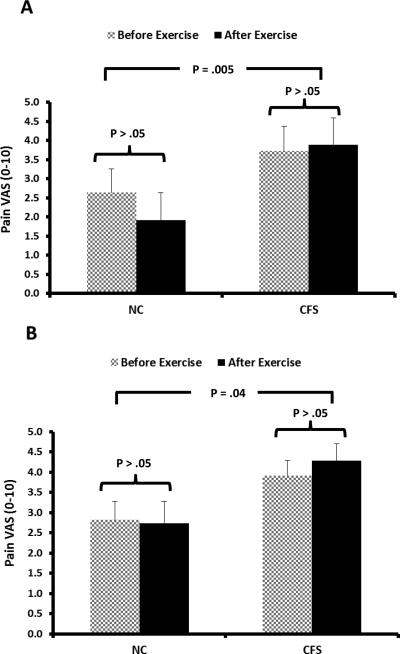
Figure 2.
NC and CFS subjects received 10 s heat stimuli to each forearm to characterize their heat pain sensitivity at baseline and after handgrip exercises. Heat intensity increased from baseline to target temperature in 6 s and was continued at this level for another 4 s. All subjects rated the heat pain intensity at the end of each stimulus using a VAS (0-10). The experimental pain ratings of 3 trials per arm were averaged
A: Average (SEM) heat pain ratings of 44°C heat stimuli to the forearm were significantly greater in CFS subjects than NC (p = .005). However, within each group there was no statistical difference between experimental pain ratings obtained before and after handgrip exercise (p > .05).
B: Average (SEM) heat pain ratings of 46°C heat stimuli to the forearm were significantly greater in CFS subjects than NC (p = .005). However, experimental pain ratings obtained before and after handgrip exercise were not statistical different within each group (p > .05).
3.2.2.2 Control Condition
During the control condition average (SD) fatigue ratings of NC and CFS subjects significantly decreased after the handgrip exercise from a baseline of .5 (1.0) to .4 (1.2) VAS units.4 (1.3) VAS units in NC and from 5.0 (1.8) to 4.8 (2.2) VAS units 4.8 (2.0) VAS units in CFS participants (Figure 2 B). Subsequent control condition decreased fatigue ratings to .4 (1.3) VAS units in NC and to 3.7 (2.1) VAS units in CFS subjects. At the end of the experiment the fatigue ratings of NC and CFS participants were .4 (1.1) and 4.8 (2.0) VAS units, respectively. A mixed model ANOVA with time (3) as within and diagnostic group (2) as between subjects’ factors demonstrated a significant main effect of time ((F3,49) = 2.7; p = .04) and diagnostic group ((F1,49) = 54.1; p < .001). The time × diagnostic group effect, however was non-significant ((F3, 49) = 2.3; p > .05; ηp2= .06), indicating that the fatigue changes were similar between NC and CFS subjects.
3.3 Heat Pain Testing
3.3.1 Effects of Handgrip Exercise on Heat Pain Ratings
3.3.1.1 Effects on 44 °C Heat Pain Ratings
All subjects underwent heat pain testing at 44°C and 46°C for 10 s at the forearm before and after the handgrip exercise. Average (SD) pain ratings of 44°C stimuli of NC changed from 2.6 (1.6) to 1.9 (1.0) VAS units and in CFS subjects from 3.7 (1.6) to 3.5 (1.6) VAS units (Figure 2 A). A repeated measures ANOVA with time (2) as within and diagnostic group (2) as between group factors demonstrated significant main effects for diagnostic group ((F1,45) = 8.9; p = .005) and non-significant effects for time ((F1,45) = 1.66; p > .05; ηp2= .04) and time × diagnostic group interaction ((F1,45) = 4.2; p > .05; ηp2= .09). These results demonstrate heat hyperalgesia in CFS subjects and indicate that the magnitude of heat sensitivity at 44°C was not significantly affected by handgrip exercise.
3.3.1.2 Effects on 46 °C Heat Pain Ratings
Average (SD) pain ratings of 46 °C stimuli of NC changed from 2.8 (2.0) to 2.7 (2.3) VAS units and in CFS subjects from 3.9 (2.2) to 4.3 (2.5) VAS units (Figure 2 B). A repeated measures ANOVA with time (2) as within and diagnostic group (2) as between group factors demonstrated significant main effects for diagnostic group ((F1,52) = 4.4; p = .04) and non-significant effects for time ((F1,51) = .65; p > .05; ηp2= .01) and time × diagnostic group interaction ((F1,52) = 1.5; p > .05; ηp2= .03). The results of both tests demonstrate heat hyperalgesia in CFS subjects and indicate that the magnitude of heat hyperalgesia was not significantly affected by handgrip exercise.
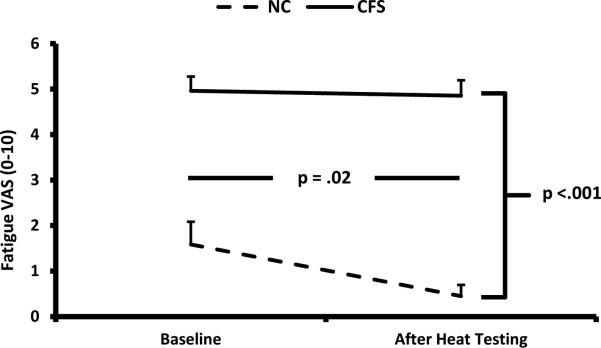
3.3.2 Effects of Heat Pain Testing on Fatigue
Average (SD) fatigue ratings obtained from NC at baseline and after heat pain testing ranged between 1.6 (2.1) and .45 (1.0) VAS units and in CFS subjects between 5.0 (1.9) and 4.9 (2.0) VAS units (Figure 3). A repeated measures ANOVA showed a significant main effect for time ((F1,52) = 5.8; p = .02) and diagnostic group ((F1,52) = 66.4; p < .001) but a non-significant time × diagnostic group interaction effect ((F1,52) = 4.0; p > .05; ηp2= .07). These findings indicate that fatigue ratings of CFS subjects were significantly higher than NC's ratings. In addition, the fatigue ratings significantly decreased after heat pain testing. This effect was similar in NC and CFS subjects.
Figure 3.
The effect of heat pain testing on fatigue was assessed in all study subjects. The subjects received trains of 44°C and 46°C heat stimuli to the forearms for 10 s each. Fatigue was assessed at baseline and after heat pain testing using the VAS (0-10). Fatigue ratings of CFS subjects were significantly higher than NC ratings. Fatigue ratings significantly decreased after heat pain testing but this effect was not significantly different between NC and CFS subjects.
3.4 Pressure Pain Testing
3.4.1 Effects of Handgrip Exercise on Pressure Pain
The subjects underwent pressure pain testing at 200 kPa and 400 kPa for 10 s at the forearm before and after the handgrip exercise.
3.4.1.1 Effects on 200 kPa Pressure Pain Ratings
Average (SD) pain ratings of 200 kPa stimuli of NC to the forearms changed from .4 (1.2) to .6 (1.2) VAS units and in CFS subjects from 2.9 (2.5) to 2.6 (2.2) VAS units (Figure 4A). A repeated measures ANOVA with time (2) as within and diagnostic group (2) as between group factor demonstrated significant main effects for diagnostic group ((F1,54) =16.5; p < .001) and non-significant effects for time ((F1,54) = .24; p > .05; ηp2= .004) and time × diagnostic group interaction effect ((F1,54) = 1.7; p > .05; ηp2= .03). These results provide evidence for mechanical hyperalgesia in CFS subjects and indicate their magnitude of mechanical hyperalgesia which was not significantly affected by handgrip exercise.
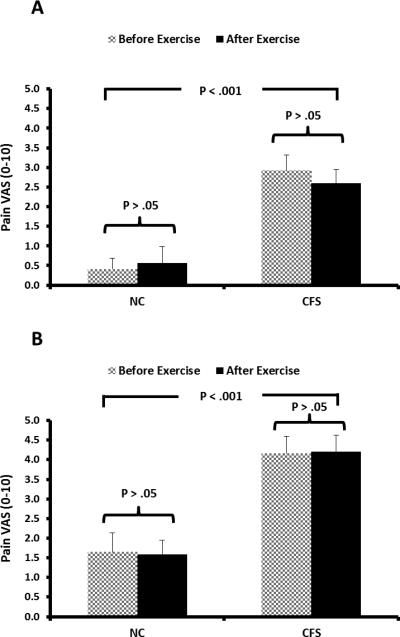
Figure 4.
NC and CFS subjects received 10 s pressure stimuli to each forearm to characterize their mechanical pain sensitivity at baseline and after handgrip exercises. Pressure was increased from baseline to target temperature in 6 s and then continued at this level for another 4 s. All subjects rated the pressure pain intensity at the end of each stimulus using the VAS (0-10). The experimental pain ratings of 3 trials per arm were averaged
A: Average (SEM) pressure pain ratings of 200 kPa pressure stimuli to the forearm were significantly greater in CFS subjects than NC (p < .001). However, within each group there was no statistical difference between experimental pressure pain ratings obtained at baseline and after handgrip exercise (p > .05).
B: Average (SEM) heat pain ratings of 400 kPa pressure stimuli to the forearm were significantly greater in CFS subjects than NC (p < .001). However, experimental pressure pain ratings obtained before and after handgrip exercise were not statistical different within each group (p > .05).
3.4.1.2 Effects on 400 kPa Pressure Pain Ratings
Average (SD) pain ratings of 400 kPa stimuli of NC to the forearms changed from 1.6 (2.1) to 1.6 (2,0) VAS units and in CFS subjects from 4.2 (2.6) to 4.2 (2.6) VAS units (Figure 4B). A repeated measures ANOVA with time (2) as within and diagnostic group (2) as between group factor demonstrated significant main effects for diagnostic group ((F1,54) =15.0; p < .001) and non-significant effects for time ((F1,54) = .1; p > .05; ηp2= .00) and time × diagnostic group interaction effect ((F1,54) = .4; p > .05; ηp2= .001). These results provide evidence for mechanical hyperalgesia in CFS subjects and indicate their magnitude of mechanical hyperalgesia which was not significantly affected by handgrip exercise.
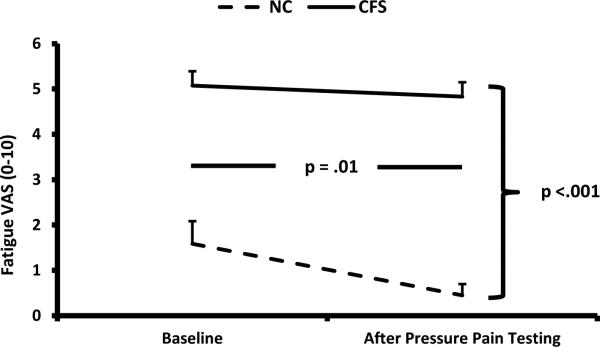
3.4.2 Effects of Pressure Pain Testing on Fatigue
Average (SD) fatigue ratings obtained from NC at baseline and after pressure pain testing at the forearms ranged between 1.5 (2.1) and .45 (1.0) VAS units and in CFS subjects between 5.1 (2.0) and 4.8 (2.0) VAS units (Figure 5). A repeated measures ANOVA showed a significant main effect for time ((F1,54) = 6.9; p = .01) and diagnostic group ((F1,54) = 70.0; p < .001) but a non-significant time × diagnostic group interaction effect ((F1,54) = 2.9; p > .05; ηp2= .05). These findings indicate that overall fatigue ratings of CFS subjects were significantly higher than NC ratings. In addition, the fatigue ratings significantly decreased after pressure pain testing. This effect was similar in NC and CFS subjects.
Figure 5.
The effect of pressure pain testing on fatigue was assessed in all study subjects. The subjects received trains of 200 kPa and 400 kPa pressure stimuli to the forearms for 10 s each. Fatigue was assessed at baseline and after pressure pain testing using the VAS (0-10). Fatigue ratings of CFS subjects were significantly higher than NC ratings. Fatigue ratings significantly decreased after pressure pain testing but this effect was not significantly different between NC and CFS subjects.
4. Discussion
CFS patients who underwent exhausting handgrip-exercises demonstrated significantly increased fatigue ratings after exercise related metabolites were trapped in their arms by complete forearm occlusion. In contrast, CFS patients’ fatigue ratings significantly decreased during the non-occlusive control condition. Similar, but significantly smaller effects were observed in NC suggesting that hypersensitive fatigue pathways play an important role for the often pronounced exercise related fatigue of CFS patients. The rapid return of fatigue ratings to baseline after termination of forearm occlusion also supports this conclusion. Because the forearm occlusion after exercise resulted in worsening of overall fatigue, central fatigue mechanisms may have become activated by this manipulation. Importantly, physical exertion itself did not seem to contribute directly to fatigue as fatigue ratings immediately obtained after exercise were not different compared to baseline. Because both fatigue and pain ratings increased during forearm occlusion of CFS patients, activation of pain pathways may have contributed to fatigue intensity. However, as demonstrated by our experiments, when similar experimental pain was induced in CFS patients without forearm occlusion, significant reductions in fatigue ratings were noted, suggesting that activation of sensitized deep tissue-receptors is critical for exercise + occlusion related fatigue.
4.1 Effects of exercise on CFS
The mechanisms of often pronounced exercise associated fatigue of CFS patients are only partially understood [18]. Muscle function at rest and during recovery is normal in CFS patients as assessed by maximum isometric voluntary contraction, tetanic force-ratio and maximum relaxation rate testing [10]. One study showed that exercise duration and the relationship between heart rate and work effort during exercise were similar in CFS patients and NC [10]. CFS patients, however, had higher perceived exertion scores than NC, despite normal muscle physiology before and after exercise [10]. Other studies demonstrated that both submaximal exercise and self-paced, limited exercise could trigger post-exertional malaise in CFS patients [50]. Specifically, decreased pressure pain thresholds during submaximal exercise were associated with post-exertional fatigue of CFS patients suggesting abnormal central pain processing during exercise. Some investigators could show that following moderate exercise, CFS patients exhibited significantly increased mRNA expression of metabolite-detecting receptor and adrenergic receptor genes which was observed shortly after onset of exercise [24]. More importantly, there were strong correlations between increased mRNA expression of metabo-receptor genes (ASIC3, TRPV1, P2X4, P2X5) of CFS patients and their reports of increased mental fatigue over several days following exercise. Similar correlations between metabo-receptor gene expression and CFS patients’ pain reports were observed after exercise challenges [24].
4.2 Muscle Metabolites and CFS
CFS is characterized by mental and physical fatigue, as well as muscle pain at rest, often exacerbated by exercise. Although a specific defect in muscle metabolism has not been clearly defined, several studies have reported abnormal oxidative metabolism, including increased activity of antioxidant enzymes catalase, glutathione peroxidase, transferase, and increases in total glutathione plasma levels [9]. Furthermore, a deficiency of serum acylcarnitine has been found [20], which could result in abnormalities of mitochondrial function. Reduced oxidative metabolism [25; 56] and higher plasma lactate concentration [44] have also been reported in CFS patients. However, many of these results were obtained in small trials and thus are considered controversial. For example, although a marked decrease of intracellular pH after moderate exercise and a lower rate of ATP synthesis during recovery have been reported in CSF patients [21] the results of VO2(max), HR(max), and the lactate threshold in CFS patients of both genders were not different from expected values in healthy sedentary age-matched NC [46]. Some of these differences may be related to differences in testing methodology but there is currently no clear evidence for specific muscle abnormalities in CFS available.
Other studies measured muscle metabolites of CFS patients in the medial gastrocnemius using (31)P-magnetic resonance spectroscopy while recording muscle oxygen saturation and blood volume with near-infrared spectroscopy [26; 27]. CFS and controls were not different in hyperemic blood-flow or phosphocreatine recovery rate after partially restricted blood-flow to the extremity. CFS patients showed evidence of reduced hyperemic flow and reduced oxygen delivery but no evidence of abnormal muscle metabolism
Overall there is only inconsistent evidence available for metabolic muscle abnormalities in CFS patients, either at rest or after exercise. Thus other possibilities need to be considered including fatigue signaling via sensitized metabo-receptors.
4.2 Activation of Fatigue Pathways
Over the last 15 years, investigators have repeatedly examined serum cytokine profiles of patients with CFS after earlier studies suggested an enhanced pro-inflammatory profile with high levels of TNF-α and IL-6 in this chronic illness [12; 34]. However, more recent investigations have not supported this link between CFS and pro-inflammatory cytokine-profiles [38; 49]. Another study which investigated exercise induced cytokine profiles in CFS patients demonstrated increased levels after a mild leg-exercise task (15 min of stair-step exercise) including IL-6 and IL-1ß as well as augmented lipo-polysaccharide-stimulated IL-6 levels [3]. However, this study failed to induce increased fatigue or other symptoms. Overall, despite the well-known ability of cytokines to induce fatigue and central sensitization [17], there is little evidence for the contribution of cytokines to exercise-related worsening of fatigue at this time.
The most robust evidence for activation of fatigue pathways by muscle metabolites comes from a recent study of NC where the investigators applied physiological concentrations of protons, lactate, and ATP to abductor pollicis muscles of the hands [39]. Importantly, infusion of single metabolites or metabolite combinations found in resting muscles (H+, lactate, ATP) evoked neither fatigue nor pain. However, injections of the same metabolites in concentrations found in muscle during moderate endurance exercise were strongly associated with fatigue-like sensations or “warmth” and “tired” in NC. This effect was dose dependent, i.e. higher doses produced stronger fatigue sensations but also pain. Thus, simultaneous intramuscular infusion of protons, lactate and ATP resulted in fatigue-like sensation and pain, possibly through activation of ASIC, TRPV1, and P2X receptors. These sensations, however, were described as local and not generalized.
Our study confirms and extends these findings in patients with CFS in two ways: 1) we elicited significant fatigue changes in NC and patients with CFS through entrapment of muscle metabolites after vigorous exercise; 2) the significantly greater increase of overall fatigue in CFS patients during forearm occlusion compared to NC provides evidence for sensitization of fatigue pathways in CFS. The observed increase in overall and not just local fatigue suggests a central effect.
4.4 Evidence for Central Sensitization in CFS
Central sensitization is a phenomenon of increased central neuronal responsiveness associated with hyperalgesia, allodynia, and referred pain across multiple spinal segments, often leading to chronic widespread pain [5; 22].There is increasing evidence supporting the important role of central sensitization for pain and possibly also fatigue in CFS patients [37]. Symptoms like fatigue, non-refreshing sleep, concentration difficulties, impaired short-term memory, sensitivity to bright light and chemicals, and widespread pain are suggestive of central nervous system involvement in CFS. A case–control study reported lower pressure pain thresholds in painful and painless body areas of CFS patients compared with healthy NC which was not explained by depression, hypervigilance or catastrophizing [29]. In the absence of detectable tissue damage, the presence of secondary hyperalgesia and widespread distribution of pain in CFS patients suggest abnormal central processing mechanisms for chronic pain and maybe also fatigue. The findings of our current study are consistent with these data as we also report mechanical and heat hyperalgesia of CFS patients in body areas without detectable tissue injury. Two studies compared the pain thresholds to electrical stimulation of muscle tissue, skin and subcutaneous tissues between patients with CFS and NC [51; 52]. No difference in electrical pain thresholds of cutaneous structures were observed, but much lower electrical pain threshold of muscle tissue were found in the CFS group (i.e. trapezius, deltoid and quadriceps muscle) [51; 52].
It is unclear at this time whether CFS patients who also report chronic pain differ from those who complain only of disabling fatigue or whether all CFS patients are similar. Given the high prevalence of chronic pain in CFS patients [4; 28; 30] the latter explanation appears more likely.
4.5 Limitations
Although animal experiments have provided convincing evidence for the important role of H+, ATP and lactate in activating metabo-receptors we can only speculate that the fatigue and pain sensations elicited by our exercise protocol were triggered by such metabolites. Recent data obtained in NC after metabolite injection into muscles seems to support this particular fatigue mechanism [40]. However, several other mediators have been found in muscles after exercise, including bradykinin, potassium, prostaglandin-E2, and various cytokines [7; 13; 16; 31; 32; 45]. It is therefore possible that they either directly activate or enhance the sensitivity of metabo-receptors in CFS.
5. Conclusions
Our study provided evidence for sensitized fatigue pathways in CFS patients. In addition, there was evidence for contributions of peripheral tissues to fatigue, most likely from muscles. Forearm occlusion seemed to be effective in trapping metabolites from exercised muscles resulting in increased overall and not just local fatigue. Thus trapped muscle metabolites may have activated peripheral and central fatigue pathways via metabo-receptors, including ASIC, TRPV1, and P2X.
Acknowledgment
This study was supported by NIH grant R01 NR014049-01 and NIH/NCATS Clinical and Translational Science grants UL1 TR000064.The expert assistance of Ricky Madhavan and Yesenia M. Lucas are gratefully acknowledged.
Footnotes
No disclosures
None of the authors have any financial or other relationships that might lead to a conflict of interest.
References
- 1.Alam M, Smirk FH. Observations in man upon a blood pressure raising reflex arising from the voluntary muscles. J Physiol. 1937;89:372–83. doi: 10.1113/jphysiol.1937.sp003485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Borg G. Borg's perceived exertion and pain scales. Human Kinetics. Champaign, Ill. 1998:1–120. [Google Scholar]
- 3.Cannon JG, Angel JB, Ball RW, Abad LW, Fagioli L, Komaroff AL. Acute phase responses and cytokine secretion in chronic fatigue syndrome. J Clin Immunol. 1999;19:414–21. doi: 10.1023/a:1020558917955. [DOI] [PubMed] [Google Scholar]
- 4.Clauw DJ, Chrousos GP. Chronic pain and fatigue syndromes: overlapping clinical and neuroendocrine features and potential pathogenic mechanisms. Neuroimmunomodulation. 1997;4:134–53. doi: 10.1159/000097332. [DOI] [PubMed] [Google Scholar]
- 5.Coderre TJ, Katz J. Peripheral and central hyperexcitability: differential signs and symptoms in persistent pain. Behav Brain Sci. 1997;20:404–19. doi: 10.1017/s0140525x97251484. [DOI] [PubMed] [Google Scholar]
- 6.Connor M, Naves LA, McCleskey EW. Contrasting phenotypes of putative proprioceptive and nociceptive trigeminal neurons innervating jaw muscle in rat. Mol Pain. 2005;1:31. doi: 10.1186/1744-8069-1-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cui J, McQuillan P, Momen A, Blaha C, Moradkhan R, Mascarenhas V, Hogeman C, Krishnan A, Sinoway LI. The role of the cyclooxygenase products in evoking sympathetic activation in exercise. Am J Physiol Heart Circ Physiol. 2007;293:H1861–H1868. doi: 10.1152/ajpheart.00258.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med. 1994;121:953–9. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 9.Fulle S, Mecocci P, Fano G, Vecchiet J, Vecchini A, Racciotti D, Cherubini A, Pizzigallo E, Vecchiet L, Senin U, Beal MF. Specific oxidative alterations in vastus lateralis muscle of patients with the diagnosis of chronic fatigue syndrome. Free Radic Biol Med. 2000;29:1252–9. doi: 10.1016/s0891-5849(00)00419-6. [DOI] [PubMed] [Google Scholar]
- 10.Gibson H, Carroll N, Clague JE, Edwards RH. Exercise performance and fatiguability in patients with chronic fatigue syndrome. J Neurol Neurosurg Psychiatry. 1993;56:993–8. doi: 10.1136/jnnp.56.9.993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gibson W, Arendt-Nielsen L, Taguchi T, Mizumura K, Graven-Nielsen T. Increased pain from muscle fascia following eccentric exercise: animal and human findings. Exp Brain Res. 2009;194:299–308. doi: 10.1007/s00221-008-1699-8. [DOI] [PubMed] [Google Scholar]
- 12.Gupta S, Aggarwal S, See D, Starr A. Cytokine production by adherent and non-adherent mononuclear cells in chronic fatigue syndrome. J Psychiatr Res. 1997;31:149–56. doi: 10.1016/s0022-3956(96)00063-5. [DOI] [PubMed] [Google Scholar]
- 13.Hoheisel U, Unger T, Mense S. Excitatory and modulatory effects of inflammatory cytokines and neurotrophins on mechanosensitive group IV muscle afferents in the rat. Pain. 2005;114:168–76. doi: 10.1016/j.pain.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 14.Holgate ST, Komaroff AL, Mangan D, Wessely S. Chronic fatigue syndrome: understanding a complex illness. Nature Reviews Neuroscience. 2011;12:539–44. doi: 10.1038/nrn3087. [DOI] [PubMed] [Google Scholar]
- 15.Immke DC, McCleskey EW. Lactate enhances the acid-sensing Na+ channel on ischemia-sensing neurons. Nat Neurosci. 2001;4:869–70. doi: 10.1038/nn0901-869. [DOI] [PubMed] [Google Scholar]
- 16.Kaufman MP, Longhurst JC, Rybicki KJ, Wallach JH, Mitchell JH. Effects of static muscular contraction on impulse activity of groups III and IV afferents in cats. J Appl Physiol Respir Environ Exerc Physiol. 1983;55:105–12. doi: 10.1152/jappl.1983.55.1.105. [DOI] [PubMed] [Google Scholar]
- 17.Kawasaki Y, Zhang L, Cheng JK, Ji RR. Cytokine mechanisms of central sensitization: distinct and overlapping role of interleukin-1beta, interleukin-6, and tumor necrosis factor-alpha in regulating synaptic and neuronal activity in the superficial spinal cord. J Neurosci. 2008;28:5189–94. doi: 10.1523/JNEUROSCI.3338-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kent-Braun JA, Sharma KR, Weiner MW, Massie B, Miller RG. Central basis of muscle fatigue in chronic fatigue syndrome. Neurology. 1993;43:125–31. doi: 10.1212/wnl.43.1_part_1.125. [DOI] [PubMed] [Google Scholar]
- 19.Koltyn KF, Arbogast RW. Perception of pain after resistance exercise. Br J Sports Med. 1998;32:20–4. doi: 10.1136/bjsm.32.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuratsune H, Yamaguti K, Takahashi M, Misaki H, Tagawa S, Kitani T. Acylcarnitine deficiency in chronic fatigue syndrome. Clin Infect Dis. 1994;18(Suppl 1):S62–S67. doi: 10.1093/clinids/18.supplement_1.s62. [DOI] [PubMed] [Google Scholar]
- 21.Lane RJ, Barrett MC, Taylor DJ, Kemp GJ, Lodi R. Heterogeneity in chronic fatigue syndrome: evidence from magnetic resonance spectroscopy of muscle. Neuromuscul Disord. 1998;8:204–9. doi: 10.1016/s0960-8966(98)00021-2. [DOI] [PubMed] [Google Scholar]
- 22.Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10:895–926. doi: 10.1016/j.jpain.2009.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Light AR, Hughen RW, Zhang J, Rainier J, Liu Z, Lee J. Dorsal root ganglion neurons innervating skeletal muscle respond to physiological combinations of protons, ATP, and lactate mediated by ASIC, P2X, and TRPV1. J Neurophysiol. 2008;100:1184–201. doi: 10.1152/jn.01344.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Light AR, White AT, Hughen RW, Light KC. Moderate exercise Increases expression for sensory, adrenergic, and Immune genes in Chronic Fatigue Syndrome patients but not in normal subjects. J Pain. 2009;10:1099–112. doi: 10.1016/j.jpain.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCully KK, Natelson BH, Iotti S, Sisto S, Leigh JS., Jr Reduced oxidative muscle metabolism in chronic fatigue syndrome. Muscle Nerve. 1996;19:621–5. doi: 10.1002/(SICI)1097-4598(199605)19:5<621::AID-MUS10>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 26.McCully KK, Smith S, Rajaei S, Leigh JS, Natelson BH. Blood flow and muscle metabolism in chronic fatigue syndrome. Clin Sci (Lond) 2003;104:641–7. doi: 10.1042/CS20020279. [DOI] [PubMed] [Google Scholar]
- 27.McCully KK, Smith S, Rajaei S, Leigh JS, Natelson BH. Muscle metabolism with blood flow restriction in chronic fatigue syndrome. J Appl Physiol. 2004;96:871–8. doi: 10.1152/japplphysiol.00141.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meeus M, Nijs J. Central sensitization: a biopsychosocial explanation for chronic widespread pain in patients with fibromyalgia and chronic fatigue syndrome. Clin Rheumatol. 2007;26:465–73. doi: 10.1007/s10067-006-0433-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meeus M, Nijs J, Huybrechts S, Truijen S. Evidence for generalized hyperalgesia in chronic fatigue syndrome: a case control study. Clin Rheumatol. 2010;29:393–8. doi: 10.1007/s10067-009-1339-0. [DOI] [PubMed] [Google Scholar]
- 30.Meeus M, Nijs J, Meirleir KD. Chronic musculoskeletal pain in patients with the chronic fatigue syndrome: A systematic review. Eur J Pain. 2007;11:377–86. doi: 10.1016/j.ejpain.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 31.Mense S. Nervous outflow from skeletal muscle following chemical noxious stimulation. J Physiol (Lond) 1977;267:75–88. doi: 10.1113/jphysiol.1977.sp011802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mense S, Schmidt RF. Activation of group IV afferent units from muscle by algesic agents. Brain Res. 1974;72:305–10. doi: 10.1016/0006-8993(74)90870-1. [DOI] [PubMed] [Google Scholar]
- 33.Molliver DC, Immke DC, Fierro L, Pare M, Rice FL, McCleskey EW. ASIC3, an acid-sensing ion channel, is expressed in metaboreceptive sensory neurons. Mol Pain. 2005;1:35. doi: 10.1186/1744-8069-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moss RB, Mercandetti A, Vojdani A. TNF-alpha and chronic fatigue syndrome. J Clin Immunol. 1999;19:314–6. doi: 10.1023/a:1020595709352. [DOI] [PubMed] [Google Scholar]
- 35.Naves LA, McCleskey EW. An acid-sensing ion channel that detects ischemic pain. Braz J Med Biol Res. 2005;38:1561–9. doi: 10.1590/s0100-879x2005001100001. [DOI] [PubMed] [Google Scholar]
- 36.Nicolay CW, Walker AL. Grip strength and endurance: Influences of anthropometric variation, hand dominance, and gender. Int J Ind Ergonom. 2006;36:605–10. [Google Scholar]
- 37.Nijs J, Meeus M, Van Oosterwijck J, Ickmans K, Moorkens G, Hans G, De Clerck LS. In the mind or in the brain? Scientific evidence for central sensitisation in chronic fatigue syndrome. European Journal of Clinical Investigation. 2012;42:203–12. doi: 10.1111/j.1365-2362.2011.02575.x. [DOI] [PubMed] [Google Scholar]
- 38.Patarca-Montero R, Antoni M, Fletcher MA, Klimas NG. Cytokine and other immunologic markers in chronic fatigue syndrome and their relation to neuropsychological factors. Appl Neuropsychol. 2001;8:51–64. doi: 10.1207/S15324826AN0801_7. [DOI] [PubMed] [Google Scholar]
- 39.Pollak KA, Swenson JD, Vanhaitsma TA, Hughen RW, Jo D, Light KC, Schweinhardt P, Amann M, Light AR. Exogenously applied muscle metabolites synergistically evoke sensations of muscle fatigue and pain in human subjects. Exp Physiol. 2014;99:368–80. doi: 10.1113/expphysiol.2013.075812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pollak KA, Swenson JD, Vanhaitsma TA, Hughen RW, Jo D, Light KC, Schweinhardt P, Amann M, Light AR. Exogenously applied muscle metabolites synergistically evoke sensations of muscle fatigue and pain in human subjects. Exp Physiol. 2014;99:368–80. doi: 10.1113/expphysiol.2013.075812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994;56:217–26. doi: 10.1016/0304-3959(94)90097-3. [DOI] [PubMed] [Google Scholar]
- 42.Price DD, Dubner R. Mechanisms of first and second pain in the peripheral and central nervous systems. J Invest Dermatol. 1977;69:167–71. doi: 10.1111/1523-1747.ep12497942. [DOI] [PubMed] [Google Scholar]
- 43.Price DD, Hu JW, Dubner R, Gracely RH. Peripheral suppression of first pain and central summation of second pain evoked by noxious heat pulses. Pain. 1977;3:57–68. doi: 10.1016/0304-3959(77)90035-5. [DOI] [PubMed] [Google Scholar]
- 44.Riley MS, O'Brien CJ, McCluskey DR, Bell NP, Nicholls DP. Aerobic work capacity in patients with chronic fatigue syndrome. BMJ. 1990;301:953–6. doi: 10.1136/bmj.301.6758.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rotto DM, Kaufman MP. Effect of metabolic products of muscular contraction on discharge of group III and IV afferents. J Appl Physiol (1985) 1988;64:2306–13. doi: 10.1152/jappl.1988.64.6.2306. [DOI] [PubMed] [Google Scholar]
- 46.Sargent C, Scroop GC, Nemeth PM, Burnet RB, Buckley JD. Maximal oxygen uptake and lactate metabolism are normal in chronic fatigue syndrome. Med Sci Sports Exerc. 2002;34:51–6. doi: 10.1097/00005768-200201000-00009. [DOI] [PubMed] [Google Scholar]
- 47.Staud R, Weyl EE, Bartley E, Price DD, Robinson ME. Analgesic and anti-hyperalgesic effects of muscle injections with lidocaine or saline in patients with fibromyalgia syndrome. Eur J Pain. 2014;18:803–12. doi: 10.1002/j.1532-2149.2013.00422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Staud R, Weyl EE, Price DD, Robinson ME. Mechanical and heat hyperalgesia highly predict clinical pain intensity in patients with chronic musculoskeletal pain syndromes. J Pain. 2012;13:725–35. doi: 10.1016/j.jpain.2012.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.ter Wolbeek M, van Doornen LJP, Kavelaars A, van de Putte EM, Schedlowski M, Heijnen CJ. Longitudinal analysis of pro- and anti-inflammatory cytokine production in severely fatigued adolescents. Brain Behavior and Immunity. 2007;21:1063–74. doi: 10.1016/j.bbi.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 50.Van Oosterwijck J, Nijs J, Meeus M, Lefever I, Huybrechts L, Lambrecht L, Paul L. Pain inhibition and postexertional malaise in myalgic encephalomyelitis/chronic fatigue syndrome: An experimental study. J Intern Med. 2010;268:265–78. doi: 10.1111/j.1365-2796.2010.02228.x. [DOI] [PubMed] [Google Scholar]
- 51.Vecchiet J, Cipollone F, Falasca K, Mezzetti A, Pizzigallo E, Bucciarelli T, De Laurentis S, Affaitati G, De Cesare D, Giamberardino MA. Relationship between musculoskeletal symptoms and blood markers of oxidative stress in patients with chronic fatigue syndrome. Neuroscience Letters. 2003;335:151–4. doi: 10.1016/s0304-3940(02)01058-3. [DOI] [PubMed] [Google Scholar]
- 52.Vecchiet L, Montanari G, Pizzigallo E, Iezzi S, de Bigontina P, Dragani L, Vecchiet J, Giamberardino MA. Sensory characterization of somatic parietal tissues in humans with chronic fatigue syndrome. Neurosci Lett. 1996;208:117–20. doi: 10.1016/0304-3940(96)12559-3. [DOI] [PubMed] [Google Scholar]
- 53.Waldmann R, Bassilana F, de WJ, Champigny G, Heurteaux C, Lazdunski M. Molecular cloning of a non-inactivating proton-gated Na+ channel specific for sensory neurons. J Biol Chem. 1997;272:20975–8. doi: 10.1074/jbc.272.34.20975. [DOI] [PubMed] [Google Scholar]
- 54.Waldmann R, Champigny G, Bassilana F, Heurteaux C, Lazdunski M. A proton-gated cation channel involved in acid-sensing. Nature. 1997;386:173–7. doi: 10.1038/386173a0. [DOI] [PubMed] [Google Scholar]
- 55.Whiteside A, Hansen S, Chaudhuri A. Exercise lowers pain threshold in chronic fatigue syndrome. Pain. 2004;109:497–9. doi: 10.1016/j.pain.2004.02.029. [DOI] [PubMed] [Google Scholar]
- 56.Wong R, Lopaschuk G, Zhu G, Walker D, Catellier D, Burton D, Teo K, Collins-Nakai R, Montague T. Skeletal muscle metabolism in the chronic fatigue syndrome. In vivo assessment by 31P nuclear magnetic resonance spectroscopy. Chest. 1992;102:1716–22. doi: 10.1378/chest.102.6.1716. [DOI] [PubMed] [Google Scholar]
- 57.Yagi J, Wenk HN, Naves LA, McCleskey EW. Sustained currents through ASIC3 ion channels at the modest pH changes that occur during myocardial ischemia. Circ Res. 2006;99:501–9. doi: 10.1161/01.RES.0000238388.79295.4c. [DOI] [PubMed] [Google Scholar]
- 58.Yarnitsky D, Simone DA, Dotson RM, Cline MA, Ochoa JL. Single C nociceptor responses and psychophysical parameters of evoked pain: effect of rate of rise of heat stimuli in humans. J Physiol. 1992;450:581–92. doi: 10.1113/jphysiol.1992.sp019144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yeomans DC, Proudfit HK. Nociceptive responses to high and low rates of noxious cutaneous heating are mediated by different nociceptors in the rat: electrophysiological evidence. Pain. 1996;68:141–50. doi: 10.1016/S0304-3959(96)03177-6. [DOI] [PubMed] [Google Scholar]