Abstract
Acute myeloid leukemia (AML) is an aggressive cancer of the blood that is linked with poor survival. The disease requires immediate intensive chemotherapy treatment that leaves patients hospitalized for at least one month and often longer, depending on their supportive care needs. Mothers undergoing treatment for AML may benefit from having attention paid to their supportive care needs during that time.
Keywords: acute myeloid leukemia, supportive care, parental cancer
Acute myeloid leukemia (AML) is a disease of the blood and bone marrow that is fatal if not treated emergently (Pulte, Gondos, & Brenner, 2010). Patients with AML typically receive inpatient induction chemotherapy during the course of one week, then remain hospitalized for at least one month because of treatment-associated complications, such as neutropenic fever, anemia, and thrombocytopenia. Patients commonly experience fluctuating levels of health, and they may have the potential to become ill quickly (Button & Chan, 2014). Patients’ labile health may exacerbate what is already a stressful experience (Danhauer et al., 2013). Therefore, the hospitalization period for the patient diagnosed with AML must include vigilant nursing and supportive care.
Case Study
J.C., a 43-year-old mother of four children, was diagnosed with AML seven months ago. Her initial induction chemo-therapy treatment was complicated by infectious colitis and fungal pneumonia, which left her hospitalized for more than 45 days. She was discharged and returned to the hospital two weeks later to begin consolidation chemotherapy; she learned that her disease had relapsed. In addition, she was exhibiting new and concerning symptoms, including visual changes and a constant dull headache. A lumbar puncture confirmed the presence of blast cells in her cerebrospinal fluid. She then began another induction treatment that was administered in conjunction with intrathecal chemotherapy for the AML that now also involved her central nervous system.
J.C. confided to her nurse that she felt nervous about everything. The goal of her treatment was to get her into remission long enough to receive a transplantation, but J.C. was wary. She shared that she had a cousin with AML who received a transplantation and then died soon afterward. She did not know what was best for her; the induction treatments were awful, she said, and she was not sure that the transplantation would be any better. J.C. told the nurse that she was tired of being so sick and that she missed being at home with her children. Her twins just started kindergarten, but she did not have the opportunity to put them on the bus. Her middle daughter also just started high school, which J.C. referred to as a tough time; she said she does not feel able to be there for her daughter like she wants to be.
J.C.'s second induction was complicated by pneumonia. She was again hospitalized for 44 days for supportive care as her counts recovered and the infection was managed with IV antibiotics. This hospitalization took an immense toll on her hope.
Patient Assessment
Nurses caring for J.C. noted that she was continually down and even distraught at times. They remarked that J.C. was upset because she did not have an updated family photograph, and was afraid she was not going to live to marry her fiancé or to see her children off to college. Throughout her hospitalization, J.C. complained of severe pain (rated 3 out of 4), numbness and tingling (rated 3 out of 4), sweats (rated 3 out of 4), depression (rated 5 out of 10), and overall distress (rated 7 out of 10). J.C. also told the nurses that she frequently worried, was anxious, and had trouble sleeping. She was neutropenic with an absolute neutrophil count of less than 500, and on a few occasions had developed a temperature of 38.3°C (101°F). In addition, she required transfusions to keep her platelets above 10,000 mcl and her hemoglobin above 8 g/dl.
Nursing Management
J.C.'s nursing care included systemic and psychologic support. Febrile neutropenia is a common complication for patients with hematologic cancers, and is defined as a single oral temperature of 38.3°C or greater or a temperature of 38°C (100.4°F) or greater that is sustained during a one-hour period in combination with neutropenia (Freifeld et al., 2011). In several instances, J.C.'s fever exceeded 38.3°C, and she underwent testing that included peripheral and central line blood cultures, a urine culture, and a two-view chest x-ray (Bryant, Walton, & Albrecht, 2014).
J.C.'s treatment was complicated by the neutropenic fevers and fungal pneumonia. To treat known and potential infections, J.C. received broad-spectrum antibiotics and antifungals during her hospitalization. Nursing care included timely administration of these drugs, monitoring for allergic reactions, strict neutropenic precautions, and supportive care, which involved supplying cool washcloths and encouraging hydration, for example.
The constant headache that J.C. experienced was a critical nursing concern, given her severe thrombocytopenia. However, her neurologic status and vital signs were stable, and a computed tomography scan ruled out an intracranial hemorrhage. Therefore, her pain was managed with analgesics. At this time, supportive care also included the clustering of care by nurses, which allowed J.C. to have periods of rest in a quiet, dimly lit room.
Emotional distress is common in patients with cancer and has been of interest to healthcare providers for decades (Holland, 1977; Weisman & Worden, 1976). Emotional distress is an established factor in patients’ decisions to reduce or stop treatment (Nerenz, Leventhal, & Love, 1982). The psychosocial support that J.C. requires is extensive and not uncommon, particularly because she is a parent (Compas et al., 1994). Further assessment is necessary to determine the source of J.C.'s distress. If her symptoms and distress are related to a lack of information or challenges pertaining to decision making, she may benefit from a psychoeducational intervention. Psycho-educational interventions can include education and supportive attention, which are recommended for the reduction of anxiety (Galway et al., 2012). For J.C., a psychosocial intervention could consist of equipping her with specific information about her treatment options or side effects, or making her aware of resources that would help her to cope with cancer after discharge.
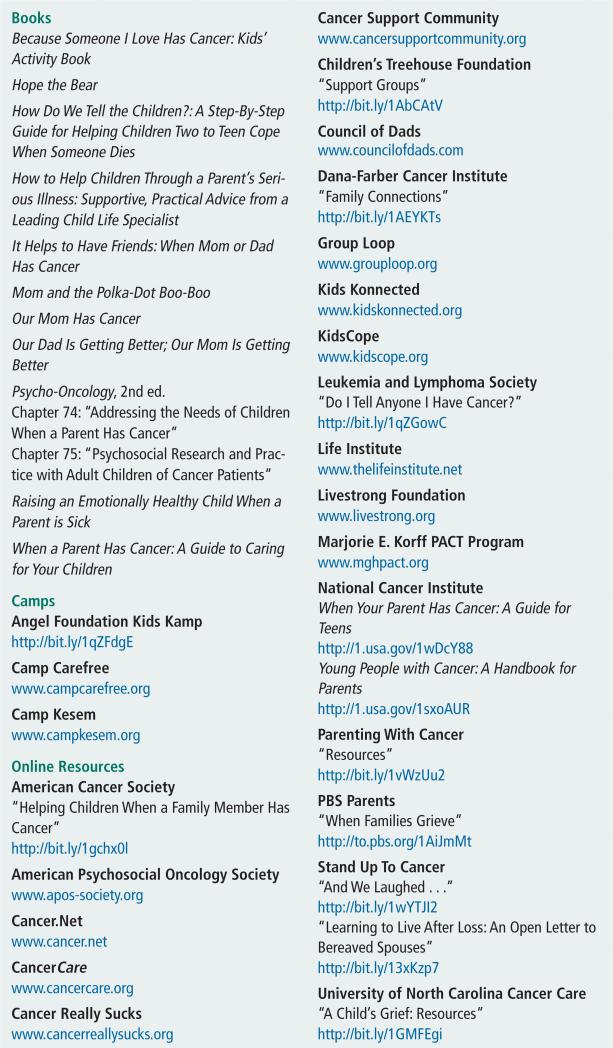
However, if J.C's distress is found to be related to her family life, her concerns for her children, and her desire to be there for them during treatment, that distress is a challenge that also must be approached by nurses (Helseth & Ulfsaet, 2005). The resources that are available for families dealing with a parent's diagnosis of cancer have grown considerably and now include an array of materials geared at parents and children of all ages: literature, live and online support groups, camps and retreats, and information clearinghouses (see Figure 1). Various technologic advances, including video conferencing tools like FaceTime and Skype, allow families to stay connected even when they cannot physically be together. In addition, continued work is being done regarding “legacy making” (Allen, 2009). Legacy making involves the creation of a scrap-book, cookbook, audiotape, or other item that celebrates the relationships of the person with the life-threatening illness. J.C's distress may be eased if she and her family are provided with an opportunity to have a family portrait taken, which would help to construct and celebrate their legacy.
FIGURE 1.
Resources for Families Dealing With a Parent's Diagnosis of Cancer
Meeting J.C.'s needs for deciding a course of treatment and being able to better communicate with and find strategies to support her children may alleviate some of her feelings of generalized distress, depression, anxiety, and worry, as well as help to address her trouble sleeping. Compassionate validation by her treatment team of all that she is experiencing, along with team members’ presence and sensitivity to her situation, may also aid in improving J.C.'s emotional state. J.C. and her family members each met with a psychologist to receive psychoeducational support and discuss the complex feelings they were experiencing.
Other interventions to ameliorate depression, anxiety, and sleeping problems include exercise (Brown et al., 2012; Galvão & Newton, 2005; Mishra et al., 2012). If J.C. is able, she should be encouraged to conserve her energy and walk around the inpatient unit a couple of times a day, potentially after school with her high school-aged daughter; doing so would create time for them to be together. In addition, mindfulness-based stress reduction is another strategy that has been recommended to mitigate depression, anxiety, and sleep disturbance (Piet, Würtzen, & Zachariae, 2012; Win-bush, Gross, & Kreitzer, 2007).
Conclusion
This case illuminates some of the physical and psychologic complexities that are involved in the care of adults with cancer who are caring for young children. Oncology nurses must provide medical management, as well as psychosocial care, to these patients. This care should often include other members of the interdisciplinary healthcare team in the supportive care plan. Oncology nurses must work in collaboration with other healthcare professionals to promote the best outcomes for patients and their families.
At a Glance.
The fluctuating health of many patients with cancer, particularly those who care for young children, may further intensify their stress levels during hospitalizations.
These periods of hospitalization should include vigilant nursing and supportive care.
Many resources are available for families dealing with a parent's diagnosis of cancer.
Acknowledgments
This study was supported, in part, by grants from the Sigma Theta Tau International Small Grants program and from the Interdisciplinary Training for Nurse Scientists in Cancer Survivorship Research program (No. T32 NR011972) offered by the National Institute of Nursing Research at the University of Pittsburgh School of Nursing to Albrecht; by a fellowship in cancer, aging, and end-of-life care (No. T32 NR013456) offered by the National Institute of Nursing Research at the University of Utah College of Nursing to Walton; by a Doctoral Scholarship in Cancer Nursing (renewal DSCNR-13-276-03) offered by the American Cancer Society to Walton; and by the UNC Oncology Clinical Translational Research Training Program (NCI 5K12CA120780-07) to Bryant.
Contributor Information
Tara Albrecht, School of Nursing at Virginia Commonwealth University in Richmond.
AnnMarie Lee Walton, College of Nursing at the University of Utah in Salt Lake City.
Ashley Leak Bryant, School of Nursing at the University of North Carolina (UNC) in Chapel Hill..
References
- Allen RS. The Legacy Project intervention to enhance meaningful family interactions: Case examples. Clinical Gerontologist. 2009;32:164–176. doi: 10.1080/07317110802677005. doi:10.1080/07317110802677005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown JC, Huedo-Medina TB, Pescatello LS, Ryan SM, Pescatello SM, Moker E, Johnson BT. The efficacy of exercise in reducing depressive symptoms among cancer survivors: A meta-analysis. PLOS ONE. 2012;7:e30955. doi: 10.1371/journal.pone.0030955. doi:10.1371/journal.pone.0030955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant AL, Walton A, Albrecht TA. Management of febrile neutropenia in a patient with acute leukemia. Journal of Emergency Nursing. 2014;40:377–381. doi: 10.1016/j.jen.2013.07.021. doi:10.1016/j.jen.2013.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Button E, Chan RJ. Palliative care provision for patients with a hematological malignancy: Can we do more? Cancer Nursing. 2014;37:239–240. doi: 10.1097/NCC.0000000000000164. doi:10.1097/NCC.0000000000000164. [DOI] [PubMed] [Google Scholar]
- Compas BE, Worsham NL, Epping-Jordan JE, Grant KE, Mireault G, Howell DC, Malcarne VL. When Mom or Dad has cancer: Markers of psychological distress in cancer patients, spouses, and children. Health Psychology. 1994;13:507–515. doi:10.1037/0278-6133.13.6.507. [PubMed] [Google Scholar]
- Danhauer SC, Russell GB, Tedeschi RG, Jesse MT, Vishnevsky T, Daley K, Powell BL. A longitudinal investigation of posttraumatic growth in adult patients undergoing treatment for acute leukemia. Journal of Clinical Psychology in Medical Settings. 2013;20:13–24. doi: 10.1007/s10880-012-9304-5. doi:10.1007/s10880-012-9304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freifeld AG, Bow EJ, Sepkowitz KA, Boeckh MJ, Ito JI, Mullen CA, Wingard JR. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the Infectious Diseases Society of America. Clinical Infectious Diseases. 2011;52:e56–e93. doi: 10.1093/cid/cir073. doi:10.1093/cid/cir073. [DOI] [PubMed] [Google Scholar]
- Galvão DA, Newton RU. Review of exercise intervention studies in cancer patients. Journal of Clinical Oncology. 2005;23:899–909. doi: 10.1200/JCO.2005.06.085. doi:10.1200/JCO.2005.06.085. [DOI] [PubMed] [Google Scholar]
- Galway K, Black A, Cantwell M, Cardwell CR, Mills M, Donnelly M. Psychosocial interventions to improve quality of life and emotional wellbeing for recently diagnosed cancer patients. Cochrane Database of Systematic Reviews. 2012;11:CD007064. doi: 10.1002/14651858.CD007064.pub2. doi:10.1002/14651858.CD007064.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helseth S, Ulfsaet N. Parenting experiences during cancer. Journal of Advanced Nursing. 2005;52:38–46. doi: 10.1111/j.1365-2648.2005.03562.x. doi:10.1111/j.1365-2648.2005.03562.x. [DOI] [PubMed] [Google Scholar]
- Holland J. Psychological aspects of oncology. Medical Clinics of North America. 1977;61:737–748. doi: 10.1016/s0025-7125(16)31293-7. [DOI] [PubMed] [Google Scholar]
- Mishra SI, Scherer RW, Geigle PM, Berlanstein DR, Topaloglu O, Gotay CC, Snyder C. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database of Systematic Reviews. 2012;8:CD007566. doi: 10.1002/14651858.CD007566.pub2. doi:10.1002/14651858.CD007566.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nerenz DR, Leventhal H, Love RR. Factors contributing to emotional distress during cancer chemotherapy. Cancer. 1982;50:1020–1027. doi: 10.1002/1097-0142(19820901)50:5<1020::aid-cncr2820500534>3.0.co;2-j. doi:10.1002/1097-0142 (19820901) 50:5 <1020 ::AID-CNCR2820500534>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- Piet J, Würtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: A systematic review and meta-analysis. Journal of Consulting and Clinical Psychology. 2012;80:1007–1020. doi: 10.1037/a0028329. doi:10.1037/a0028329. [DOI] [PubMed] [Google Scholar]
- Pulte D, Gondos A, Brenner H. Expected long-term survival of patients diagnosed with acute myeloblastic leukemia during 2006–2010. Annals of Oncology. 2010;21:335–341. doi: 10.1093/annonc/mdp309. doi:10.1093/annonc/mdp309. [DOI] [PubMed] [Google Scholar]
- Weisman AD, Worden JW. The existential plight in cancer: Significance of the first 100 days. International Journal of Psychiatry in Medicine. 1976;7:1–15. doi: 10.2190/uq2g-ugv1-3ppc-6387. doi:10.2190/uq2g-ugv1-3ppc-6387. [DOI] [PubMed] [Google Scholar]
- Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: A systematic review. Explore: The Journal of Science and Healing. 2007;3:585–591. doi: 10.1016/j.explore.2007.08.003. doi:10.1016/j.explore.2007.08.003. [DOI] [PubMed] [Google Scholar]