Abstract
Objective This study investigated self-awareness of peer-rated social attributes and its relations to executive function (EF), theory of mind (TOM), and psychosocial adjustment in children with traumatic brain injury (TBI). Methods Self- and peer perceptions of classroom social behavior were assessed for 87 children 8–13 years of age: 15 with severe TBI, 40 with complicated mild/moderate TBI, and 32 with orthopedic injury. Participants completed measures of EF and TOM, and parents rated children’s psychosocial adjustment. Results Self-ratings of classroom social behavior did not differ between injury groups. Self- and peer ratings generally agreed, although children with severe TBI rated themselves as less rejected/victimized than did their peers. Higher EF predicted better self- and peer ratings and smaller self–peer discrepancies, which in turn predicted better adjustment. Conclusions Children with TBI show variable social self-awareness, which relates to EF and adjustment. Future studies should identify additional factors that contribute to limited insight.
Keywords: neurological disorders, neuropsychology, peers, psychosocial functioning
Traumatic brain injury (TBI) is a prominent cause of morbidity and mortality in children. In the United States, over 700,000 youth seek medical attention for TBI each year, leading to around 50,000 hospitalizations and 6,000 deaths (Faul, Xu, Wald, & Coronado, 2010). Survivors of childhood TBI often struggle with long-term difficulties including cognitive, emotional, social, and behavioral problems (Yeates, 2010). Problems with social functioning in particular have been identified as a major concern for parents and children with TBI, and are characterized, in part, by difficulties forming and maintaining peer relationships. Mutual friendship is associated with higher rates of peer acceptance, lower rates of peer victimization, and increased white matter volumes in children with TBI (Yeates et al., 2013, 2014). However, children with TBI have lower rates of mutual friendship and experience more peer rejection compared with healthy children (Yeates et al., 2013; see Rosema, Crowe, & Anderson, 2012, for a review).
The reasons for poor peer relationships following childhood TBI remain unclear. Deficits in social cognitive skills, such as theory of mind (TOM; i.e., the ability to attribute mental states to oneself and others and to understand that others have thoughts, desires, and intentions that are different from one's own) and executive function (EF; i.e., an umbrella term for cognitive processes involved in goal-directed behavior, including working memory, cognitive flexibility, and inhibitory control), may play a role (Yeates et al., 2007). Another possibility is that children with TBI possess inadequate awareness of their deficits and therefore are unable to alter or compensate for inappropriate behavior in social situations. In other populations, a lack of awareness is related to both cognitive skills and adjustment. For example, inaccurate self-ratings of skill predict lower social and academic competence in healthy children (Gresham, Lane, MacMillan, Bocian, & Ward, 2000). Furthermore, aggressive children who are rejected by their peers tend to think more positively about themselves and to underestimate how disliked they are compared with nonaggressive-rejected and withdrawn children (Boivin, Poulin, & Vitaro, 1994; Zakriski & Coie, 1996). Similarly, children with attention deficit/hyperactivity disorder (ADHD) tend to systematically overestimate their prowess across a variety of domains, and this so-called “positive illusory bias” in turn predicts more conduct problems and fewer peer-nominated friendships (Mikami, Calhoun, & Abikoff, 2010).
Similar to the aforementioned research in child populations, in adults with TBI, lack of awareness is related to EF deficits and predicts difficulties with self-regulation, reduced motivation to engage in rehabilitation, and less willingness to use assistive or compensatory devices (Bivona et al., 2008, Fleming & Strong, 1995; Sherer et al., 1998). Moreover, self-awareness helps predict vocational success in adults with TBI because a lack of awareness can lead to vocational pursuits that exceed actual abilities, as well as to socially inappropriate workplace behavior (Bogod, Mateer, & MacDonald, 2003; Trudel, Tryon, & Purdum, 1998). In one study of children with TBI, participants were asked to gauge their own performance after completing a fluency task; more accurate self-appraisal was related to fewer parent-reported real-world EF difficulties (Kruger et al., 2011). Nevertheless, the nature and implications of awareness of social deficits in children with TBI has received scant attention to date.
In previous studies of self-awareness, researchers have often used discrepancies between self-ratings and those of other informants (e.g., parent, spouse) to operationalize self-awareness, with larger discrepancies between self- and other ratings taken to reflect poorer awareness, and vice versa. However, statistical objections have arisen regarding the use of discrepancy scores as predictors of adjustment or other outcomes (De Los Reyes, Thomas, Goodman, & Kundey, 2013; Laird & De Los Reyes, 2013). De Los Reyes and colleagues (2013) outlined an alternative methodology to assess the implications of interrater differences while circumventing the statistical drawbacks of using discrepancy scores as independent variables. In this approach, self- and other ratings are entered as independent predictors before an interaction term of self-rating X other ratings to determine whether the discrepancy between self- and other ratings adds to prediction, over and above the independent effects of self- and other ratings. Notably, the use of discrepancy scores as outcomes rather than predictors has not been a focus of concern, and no alternative methodologies have been proposed to treating discrepancy scores as dependent variables.
In the present study, we sought to examine peer–self discrepancies in ratings of social attributes to better understand the nature and correlates of social self-awareness in children with TBI as compared with peers with history of orthopedic injury (OI). An OI comparison group was recruited to control for the experience of acute injury and hospitalization, as well as for preexisting factors that might increase the risk of injury. We previously reported on peer classmate ratings in children with TBI compared with children with OI, but did not report on self-ratings (Yeates et al., 2013, 2014). Our previous studies showed that children with TBI were rated higher in rejection-victimization than peers with OI and were less likely to have a mutual friendship in their classroom. Greater rejection-victimization was related to reduced brain volumes and poorer TOM, in addition to lower peer acceptance, fewer friendships, more social withdrawal, and higher levels of general psychopathology. Here we expand on this work by investigating three specific hypotheses. First, we sought to characterize the degree of concordance between self- and peer ratings of classroom social attributes. We hypothesized that self- and peer ratings of children would differ more for children with TBI than those with OI, implying less self-awareness. Second, as shown in Figure 1, we examined whether discrepancies between self- and peer ratings could be accounted for by social cognitive abilities, specifically EF and TOM skills. We hypothesized that better EF and TOM would predict greater self-awareness (i.e., less overestimation of desirable social attributes by self relative to peers). Third, we used De Los Reyes and colleagues’ (2013) statistical approach to investigate whether self–peer discrepancies in ratings of social attributes predicted children’s psychosocial adjustment as rated by parents. We hypothesized that greater overestimation of social attributes (i.e., higher self-ratings than peer ratings) would predict maladjustment over and above self- and peer ratings when considered as independent predictors.
Figure 1.
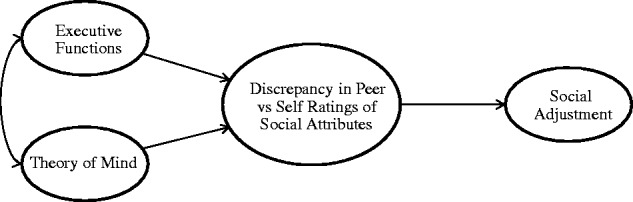
Conceptual model for the present study. Executive functions and theory of mind skills influence the nature of discrepancies between participant and peer ratings of participants’ social attributes (e.g., popularity, rejection), such that children with poorer social-cognitive skills overestimate desirable attributes and underestimate undesirable attributes. In turn, peer/self-discrepancies regarding social attributes affect parent-reported social adjustment, with overestimation of skills relative to peers predicting poorer adjustment.
Methods
Participants
Participants were a subset of a larger group of children included in a multisite study examining social outcomes among children with TBI. Recruitment occurred at three metropolitan children’s hospitals, including Nationwide Children’s Hospital in Columbus, Ohio (US), Rainbow Babies and Children’s Hospital and MetroHealth Medical Center in Cleveland, Ohio (US), and the Hospital for Sick Children in Toronto, Ontario (Canada). Children from 8 to 13 years of age who had been hospitalized for either TBI or OI after 3 years of age and injured between 12 and 63 months before the time of the study were eligible to participate. Within the TBI group, injury severity ranged from complicated mild to severe TBI. Complicated mild TBI was defined by a Glasgow Coma Scale (GCS) score of 13–15 combined with trauma-related abnormalities on neuroimaging or a depressed skull fracture at the time of hospitalization. Moderate TBI was defined by a GCS score of 9–12, and severe TBI was defined by a GCS score of ≤8. For the purposes of the current study, children with complicated mild and moderate TBI were combined into one group for analyses because they tend to display similar outcomes (Williams, Levin, & Eisenberg, 1990) and to increase statistical power. The OI group included children who sustained fractures without loss of consciousness or any indication of brain injury (e.g., facial or skull fractures).
Exclusion criteria included (a) history of any prior injury requiring medical attention; (b) injury related to child abuse or assault; (c) premorbid neurological disorder, intellectual disability, or any sensory/motor impairment that precluded valid administration of study measures; (d) history of severe psychiatric disorder requiring hospitalization; and (e) not fluent in English. Additionally, children placed in full-time special education classrooms were excluded because of the lack of established psychometric properties for classroom data in these settings. Premorbid learning or attention problems did not warrant exclusion; six children had a premorbid diagnosis of ADHD and four had a premorbid learning disability based on parent report. The proportion of children with these difficulties did not differ across groups.
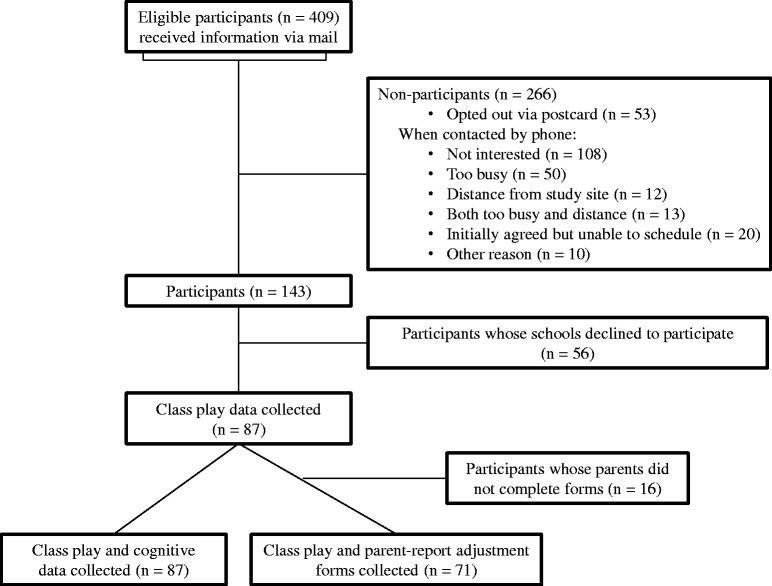
Of all eligible participants who approached for the study, 61 (27%) of those with OI and 82 (47%) of those with TBI agreed to enroll. Although the participation rate was significantly higher for TBI, participants and nonparticipants did not differ on age at injury or at the time of study recruitment, race, sex, census tract measures of socioeconomic status (SES; mean family income, percentage of minority heads of household, and percentage of households below the poverty line), or injury severity (i.e., mean length of hospital stay, or GCS score for the TBI group). The most common reasons given for nonparticipation in both groups included the family being uninterested in participating, not having time to participate, and not wanting to travel the distance to the study site to participate (see Figure 2).
Figure 2.
Participant recruitment and attrition. Participants and nonparticipants did not differ on age at injury or at study recruitment, race, sex, census tract measures of socioeconomic status, or injury severity (i.e., mean length of hospital stay, or Glasgow Coma Scale score for the traumatic brain injury group).
The present study included the 87 of 143 children from the larger study for whom classroom data were obtained (Figure 2). Participants with and without classroom data did not differ by injury group, race, sex, SES (measured using a standardized composite based on parental education, parent occupational status, and census tract mean family income), age at injury or at the time of study participation. Classroom data were obtained from 1,598 children (i.e., the participants and their classmates) in 87 classrooms. An average of 18.4 students per class (79%) took part; the remaining students were either absent or their parents did not give consent for their participation. EF and TOM test scores were available for all 87 participants with classroom data, and parent questionnaires were obtained from 71 of those 87 participants (81%). Participants with and without parent-report data did not differ by injury group, sex, SES, or age at injury or at the time of study participation. They did differ by race, with children of minority status being more likely to be missing parent-report data.
Participant demographic information, injury-related characteristics, and other descriptive data are presented in Table I. The groups differed significantly in SES and intelligence quotient (IQ), with the severe TBI group having the lowest SES and IQ. The groups also differed in mechanism of injury. When injury mechanism was taken into account, group differences in SES were no longer significant. This is consistent with epidemiological research showing that the risk of TBI, especially in the context of motor vehicle incidents, is highest for children of lower SES and minority status (Brown, 2010; Howard, Joseph, & Natale, 2005; Langlois, Rutland-Brown, & Thomas, 2005). Therefore, SES was not treated as a covariate, as the SES differences appeared to be intrinsic to the injury groups (Dennis et al., 2009). Groups also differed significantly in the expected direction on the EF and TOM composite scores, with the poorest performances in the severe TBI group.
Table I.
Demographic Information, Injury Characteristics, Cognitive Measures, and Adjustment Measures by Injury Group
| OI (n = 32) | Mild/Moderate TBI (n = 40)a | Severe TBI (n = 15) | |
|---|---|---|---|
| Demographic information | |||
| Age in years at injury (mean, SD) | 7.84 (1.97) | 8.08 (1.82) | 7.17 (2.14) |
| Age in years at assessment (mean, SD) | 10.57 (1.62) | 10.57 (1.30) | 9.68 (1.40) |
| Years from injury to assessment (mean, SD) | 2.73 (1.07) | 2.48 (1.20) | 2.51 (1.18) |
| Gender (male/female) | 20/12 | 25/15 | 8/7 |
| Caucasian/African–American/Multiracial | 29/0/2 | 34/1/3 | 9/3/0 |
| SES composite standard score (mean, SD)** | 0.44 (0.94) | −0.10 (1.06) | −0.60 (0.50) |
| Injury characteristics | |||
| Mechanism of Injury** | |||
| Motor vehicle related (n, %) | 2 (6%) | 12 (30%) | 10 (67%) |
| Fall (n, %) | 6 (19%) | 12 (30%) | 2 (13%) |
| Sports/recreational/bicycle/other (n, %) | 24 (75%) | 16 (40%) | 3 (20%) |
| Lowest Glasgow Coma Scale (GCS) score (mean, SD)b,** | n/a | 14.05 (1.68) | 3.730 (1.75) |
| Abnormal brain CT scan at time of injury (n, %) | n/a | 38 (95%) | 12 (80%) |
| Cognitive measures | |||
| Full-Scale intelligence quotient (IQ)c (mean, SD)** | 112.25 (12.74) | 99.70 (14.58) | 92.87 (12.48) |
| Executive Function Composite (mean, SD)** | 97.18 (16.40) | 85.39 (20.90) | 71.14 (18.89) |
| Theory of Mind Composite (mean, SD)** | 67.29 (14.58) | 60.33 (17.64) | 43.99 (18.28) |
| Adjustment Measures | |||
| Adjustment Composite (mean, SD) | 102.61 (9.53) | 101.17 (13.51) | 95.14 (11.36) |
Note. OI = orthopedic injury; TBI = traumatic brain injury; SES = socioeconomic status.
aModerate TBI, n = 7; complicated mild TBI, n = 33.
bThe GCS has a range of 3–15.
cIQ measured using two-subtest form of Wechsler Abbreviated Scale of Intelligence.
**p < .01.
Procedure
Institutional review boards from each site approved all study procedures. Parents provided informed consent, and children informed assent, before participation. Participants completed measures of general cognitive ability, EF, and TOM at an initial visit, while parents completed questionnaires regarding children’s psychosocial adjustment. Following this visit, participants’ school principals were contacted for permission to contact each participant’s teacher. Study staff met with teachers to explain the study and provide parental consent forms for peers, which were distributed and collected by teachers. To protect confidentiality, the study was described to students as a general study of friendships, with no mention of injury or the participant’s name. Measures were administered at a single time in the primary classroom for elementary school students or during a required academic subject for middle school students. Classroom data were not collected until after the first 2 months of the school year to ensure peer familiarity. Groups did not differ in the average number of months that had passed into the school year before classroom data collection (M = 6.30; SD = 2.09). All data collection for the study occurred from 2007 to 2011.
Measures
Extended Class Play
Participants and their classmates completed an extended version of the Revised Class Play (Masten, Morison, & Pellegrini, 1985) to assess peer and self-perceptions of social behavior in the school environment. During this paper and pencil task, all participating students in a classroom are asked individually to act as director of an imaginary class play and to write the name of one boy and one girl from the class who would best play 31 hypothetical “roles,” each of which loads on one of five subscales derived from previous factor analyses: Aggressive (e.g., “A person who gets into fights a lot”), Popular-Sociable (e.g., “Someone who has many friends”), Prosocial (e.g., “Someone who plays fair”), Rejected-Victimized (e.g., “Someone who is often left out”), and Shy-Withdrawn (e.g., “Someone who is very shy”). Self-nominations were not allowed. To account for different class sizes, gender ratios, and participation rates, the number of nominations that each study participant received for each role were tallied and standardized within gender in each class, and then summed within each subscale. Subscale scores were then standardized within gender in each class (M = 0, SD = 1). Thus, scores reflect ratings of the participant relative to same-gender peers in his or her class for the five subscales. Self-ratings were obtained by asking each participant to rate how well they thought they could play each role on a Likert scale of 1–5, with 5 being the best fit. These scores also were standardized by gender within each class (M = 0, SD = 1). The five subscales of the Extended Class Play (ECP) demonstrated acceptable reliability in the current study (peer rating Cronbach’s αs = .87–.94; self-rating Cronbach’s αs = .65–.82), and have demonstrated substantial validity in other studies (Rubin, Wojslawowicz, Burgess, Rose-Krasnor, & Booth-LaForce, 2006; Salley, Vannatta, Gerhardt, & Noll, 2010; Wojslawowicz Bowker, Rubin, Burgess, Rose-Krasnor, & Booth-LaForce, 2006).
Intelligence
Intellectual ability was assessed using the Wechsler Abbreviated Scale of Intelligence (WASI) two-subtest IQ, which includes the Vocabulary and Matrix Reasoning subtests (Wechsler, 1999). The WASI is a shortened version of the Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV; Wechsler, 2003) and has shown excellent validity and reliability in child populations.
Executive Functions
Inhibitory control, working memory, and cognitive flexibility were assessed using the Walk/Don’t Walk, Code Transmission, and Creature Counting subtests of the TEA-Ch (Manly et al., 2001), respectively. The TEA-Ch is a norm-referenced measure with high reliability and construct validity in assessing various aspects of EFs (Heaton et al., 2001; Manly et al., 2001). In the Walk/Don’t Walk subtest, children take one step along a path each time they hear a tone (“go tone”), at regular intervals. Different tones occur occasionally to signal the child not to take a step (“no-go tones”). The total standard score reflects the number of correct responses to both tones. The Code Transmission subtest is akin to an n-back task, and requires children to monitor a stream of monotonous digits for a particular target; the total standard score reflects the number of correctly identified targets. In the Creature Counting subtest, children must count creatures depicted in a burrow, switching between counting forwards and backwards when they encounter arrows pointing up or down. The total standard score reflects speed as well as accuracy.
Theory of Mind
Several measures assessing TOM were administered. Cognitive TOM (i.e., understanding false beliefs) was assessed using the Jack and Jill task (Dennis et al., 2012), in which children observed cartoon scenes of Jack and Jill characters involving Jack switching the location of a ball; sometimes Jill saw the ball’s location being switched, and sometimes she did not. Participants were asked to respond from Jill’s perspective where the ball would be located in each scenario. Percent accuracy for switched, unwitnessed trials was the primary measure of cognitive TOM.
Affective TOM (i.e., understanding of displayed versus felt emotions) was assessed using the Emotional and Emotive Faces Task (Dennis, Agostino, et al., 2013). Participants listened to short narratives about a character that were designed to evoke one of five emotions: happiness, sadness, fear, disgust, or anger. In each situation, children were asked to identify both the character’s true emotion and facial expression, which were discrepant. The percent accuracy for displayed emotion was used to assess affective TOM.
Conative TOM (i.e., social communication meant to influence the emotions of others) was assessed using the Literal Truth, Ironic Criticism, and Empathetic Praise task (Dennis, Simic, et al., 2013). In this task, children were presented with pictures and background information about six scenarios; they then listened to audiotaped utterances with neutral, ironic, or empathetic implied meanings. In each scenario, children were asked two factual questions, two belief questions, and two intent questions. The percent accuracy for indirect speech (i.e., belief and intent for empathetic praise and ironic criticism) was the primary measure of conative TOM.
Psychosocial Adjustment
Parents’ ratings of their children’s social and behavioral adjustment were elicited using the Adaptive Behavior Assessment System-Second Edition (ABAS-II; Harrison & Oakland, 2003). The ABAS-II includes Likert-scale ratings of various skills important for daily functioning, is standardized by age, and has shown good reliability and internal consistency as well as sensitivity to developmental differences and clinical disorders. We used several subscales that tap aspects of social interaction in the current paper: Social, Communication, and Self-Direction (M = 10, SD = 3), for which higher scores reflect better functioning.
Parents’ reports of their children’s emotional and behavioral adjustment were elicited using the Behavior Assessment System for Children-Second Edition (BASC-2; Reynolds & Kamphaus, 2004). This measure provides multiple subscales assessing aspects of emotional and behavioral functioning, standardized by age and gender. The BASC-2 has shown good reliability and internal consistency. Measures included in the current paper include the Social Skills Index, for which higher scores indicate better functioning, and the Behavior Symptoms Index, for which higher scores indicate more emotional and behavioral problems (both M = 50, SD = 10).
Data Analysis
All statistical analyses were completed in SPSS version 21 for Windows.
Composite Scores
Because the standard scores for the three EF measures were significantly correlated with one another (rs = .34–.50), they were averaged together to create an EF composite for analyses. Similarly, the three TOM outcome variables were also significantly correlated (rs = .23–.35), and were averaged together to create a TOM composite. A principal components analysis with varimax rotation using the six measures confirmed a two-factor solution, with the three EF variables loading highly onto Factor 1 (factor loadings .52–.88) and three TOM variables loading highly onto Factor 2 (factor loadings .47–.83). Communalities ranged from .40 to .78.
Correlations among the five parent-reported adjustment variables also were high (rs = .44–.76). Thus, the five adjustment variables were converted to a standard score metric, with higher scores reflecting better functioning, and averaged to create a single adjustment composite. Principal components analysis with varimax rotation using the five adjustment variables revealed one factor that accounted for 71% variance in adjustment, with high loadings (.77–.89) and communalities (.57–.80) for all variables.
Peer and Self-Ratings
Self-ratings on the ECP were compared across injury groups. Peer ratings on the ECP have been previously published (Yeates et al., 2013). We examined agreement between raters using bivariate, two-tailed correlations between self- and peer ratings. Differences between peer and self-ratings across the OI, mild/moderate TBI, and severe TBI groups were examined using repeated measures analysis of variance, with group as a between-subjects variable and self- versus peer ratings as a within-subjects variable. A power analysis showed that our sample size was sufficient to detect medium to large effect sizes (power = .80 for N = 87, ƒ = .34, p < .05) (Faul, Erdfelder, Lang & Buchner, 2007).
EF and TOM as Predictors of Rater Discrepancies
Interrater discrepancy scores were calculated by subtracting self-rating from peer ratings on each subscale of the ECP. Hierarchical linear regression analyses examined whether EF and TOM composite scores predicted interrater discrepancies for each of the five ECP subscales, after accounting for group (all TBI versus OI), for five regression analyses. Group X EF and group X TOM interaction terms were entered as a third step in the regression equations; none reached statistical significance, and they are not reported here. A power analysis demonstrated that our sample size was sufficient to detect medium to large effect sizes (power = .80 for N = 87, ƒ = .15, two-tailed p < .05) (Faul, Erdfelder, Buchner, & Lang, 2009).
Rater Discrepancies as Predictors of Psychosocial Adjustment
We conducted hierarchical linear regression analyses as recommended by De Los Reyes and colleagues (2013) to determine whether interrater discrepancies on the ECP predicted parent-rated psychosocial adjustment. As mentioned above, discrepancy scores are problematic when treated as independent variables. De Los Reyes and colleagues (2013) showed that scores from two informants’ reports that have equivalent variances and equivalent correlations with an outcome variable cannot yield a difference score that is significantly associated with that outcome variable. Furthermore, using a directional difference score as a predictor is equivalent to constraining the coefficients on child and parent reports to be equal in magnitude but opposite in valence (+/−) (Laird & De Los Reyes, 2013). Based on Laird & De Los Reyes’ recommendation, we therefore entered predictors in the following order: (1) group (all TBI vs. OI); (2) self- and peer ratings on the ECP subscale; (3) quadratic effects terms (i.e., squared self- and peer ratings); (4) group X self-rating and group X peer rating interactions; (5) the self-rating X peer rating interaction (representing the effect of peer–self discrepancies across groups); and (6) the self-rating X peer rating X group interaction. Quadratic effects (i.e., squared self- and peer ratings) were tested in initial models, per the recommendations of Laird & De Los Reyes (2013), to ensure that a significant interaction did not actually reflect quadric effects of self- or peer ratings; quadratic effects were eliminated from the final model when not significant. Thus, five distinct multiple regression analyses were conducted, examining each of the five ECP subscales as predictors of the parent-reported adjustment composite. We graphed significant self-rating X peer rating interactions using Hayes’ (2013) PROCESS macro for SPSS to facilitate their interpretation. Power analysis indicated that our sample size was again sufficient to detect medium to large effect sizes (N = 71, power = .80 for ƒ = .24, p < .05) (Faul et al., 2009).
Results
Peer and Self-Ratings
Group means on the five subscales of the ECP for self- and peer ratings are presented in Table II. Self-ratings did not differ between groups on any of the subscales. Peer ratings have been previously reported (Yeates et al., 2013); peers rated the severe TBI group as more rejected/withdrawn than the OI group.
Table II.
Self-Report and Peer-Report on the Extended Class Play Subscales
| Aggressive |
Popular-Sociable |
Prosocial |
Rejected-Victimized |
Shy-Withdrawn |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Injury group | Rater | M | SD | M | SD | M | SD | M | SD | M | SD |
| Severe TBI | Self | −0.10 | 1.03 | −0.21 | 0.94 | 0.05 | 0.92 | −0.26** | 1.26 | −0.22 | 0.97 |
| (n = 15) | Peer | −0.19 | 0.68 | −0.25 | 0.98 | 0.07 | 1.26 | 0.58a | 1.16 | 0.17 | 0.78 |
| Mild/Moderate TBI | Self | −0.11 | 0.82 | −0.05 | 1.03 | 0.00 | 1.02 | −0.02 | 0.99 | −0.26 | 0.83 |
| (n = 40) | Peer | 0.03 | 0.98 | 0.19 | 1.07 | 0.14 | 1.08 | 0.02 | 1.15 | −0.02 | 1.03 |
| OI | Self | −0.04 | 1.04 | −0.23 | 0.79 | −0.43** | 1.00 | −0.08* | 0.78 | 0.00 | 0.77 |
| (n = 32) | Peer | −0.24 | 0.65 | 0.25 | 1.08 | 0.34 | 1.14 | −0.28 | 0.74 | −0.21 | 0.77 |
Note. For all subscales, higher scores indicate greater frequency of nominations in that category; that is, higher scores on Aggressive, Rejected-Victimized, and Shy-Withdrawn subscales indicate undesirable traits, whereas higher scores on Popular-Sociable and Prosocial indicate desirable traits. TBI = traumatic brain injury; OI = orthopedic injury.
*Self- versus Peer Ratings, p < .05.
**Self- versus Peer Ratings, p < .01.
aSevere TBI Peer versus OI Peer Rating, p < .01.
Peer and Self-Rating Agreement
Across the sample as a whole, self- and peer ratings on each ECP subscale were significantly positively correlated (rs = .24–.42). Additionally, a number of subscales correlated significantly with one another in expected directions across self- and peer ratings (e.g., higher self-ratings of aggression correlated with lower peer ratings of popular-sociable and prosocial attributes).
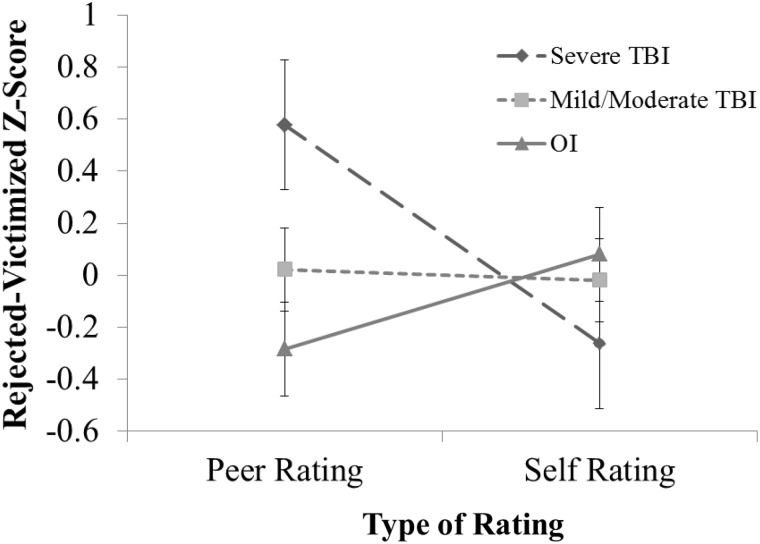
Despite the significant correlations between peer and self-ratings, repeated-measures analyses showed that the group X self/peer interaction was significant for rejection/victimization, F(2,80) = 7.39, p = .001, partial η2 = 0.16. Post hoc analyses showed that self-ratings of rejection/victimization were significantly lower than peer ratings in the severe TBI group (p = .002; d = .69), indicating that children with severe TBI viewed themselves as less rejected/victimized than did their peers (Figure 3). In contrast, within the OI group, self-ratings of rejection/victimization were significantly higher than peer ratings (p = .047; d =−.45), indicating that children with OI viewed themselves less favorably than their peers. Additionally, the group X self/peer interaction for prosocial attributes was marginally significant (p = .095, partial η2 = 0.06). Post hoc analyses revealed that the children with OI rated themselves as less prosocial than did their peers (p = .002; d = .69).
Figure 3.
Extended Class Play Rejected-Victimized Scores by Group and Rater. Error bars represent standard error. Higher scores reflect greater levels of rejection-victimization. The interaction was significant, with follow-up analysis indicating a significant difference between peer and self-rating for the Severe TBI (p = .002, d = 0.69) and the OI (p = .047, d = −.45) groups. TBI = traumatic brain injury; OI = orthopedic injury.
EF and TOM as Predictors of Rater Discrepancies
Table III presents the results of hierarchical linear regression analyses predicting discrepancies between peer and self-ratings on each of the ECP subscales from EF and TOM composites, after accounting for group. As predicted, higher EF scores were significantly associated with positive discrepancies (i.e., peer ratings greater than self-ratings) on the popular-sociable subscale and negative discrepancies (i.e., peer ratings lower than self-ratings) on the rejection/victimization subscale, and marginally associated with positive discrepancies on the prosocial subscale. Higher TOM scores unexpectedly predicted positive discrepancies on the aggression subscale and were marginally related to positive discrepancies on the rejection/victimization subscale.
Table III.
EF and TOM as Predictors of Interrater Discrepancies on the ECP Subscales
| Aggressive |
Popular-Sociable |
Prosocial |
Rejected-Victimized |
Shy-Withdrawn |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | r | β | ΔR2 | r | β | ΔR2 | r | β | ΔR2 | r | β | ΔR2 | r | β | ΔR2 |
| Step 1 | 0.02 | 0.05 | 0.06 | .13** | 0.05 | ||||||||||
| Group (TBI vs. OI) | 0.1 | 0.1 | −.20 | −.20 | −.24 | −.24 | 0.32 | 0.32 | 0.23 | 0.23 | |||||
| Age at testing | −.07 | −.07 | −.15 | −.15 | −.02 | −.02 | −.16 | −.15 | 0.02 | 0.02 | |||||
| Step 2 | .12** | .10* | 0.06 | .10* | 0.03 | ||||||||||
| EF | −.19 | −.22 | 0.32 | .39** | 0.22 | .26† | −.35 | −.40** | −.09 | −.11 | |||||
| TOM | 0.35 | .50** | −.12 | −.16 | 0 | 0 | 0.2 | .25*** | 0.18 | 0.25 | |||||
Note. EF = executive function composite; TOM = theory of mind composite. ECP = Extended Class Play. Interrater discrepancies = peer–self report. r = partial correlation.
N = 87; df (2, 84).
*p < .05, **p < .01, ***p < .10.
Rater Discrepancies as Predictors of Psychosocial Adjustment
Table IV summarizes the results of five different hierarchical regression analyses examining the prediction of parent-rated adjustment, one for each of the five ECP subscales. Predictors included self- and peer ratings on the respective ECP subscale, as well as the interactions between them, after controlling for group membership.
Table IV.
Peer and Self-Ratings on ECP Subscales as Predictors of Parent-Reported Adjustment Composite
| ECP Subscale Predicting Adjustment Composite |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Aggressive |
Popular-Sociable |
Prosocial |
Rejected-Victimized |
Shy-Withdrawn |
|||||||||||
| Predictor | r | β | ΔR2 | r | β | ΔR2 | r | β | ΔR2 | r | β | ΔR2 | r | β | ΔR2 |
| Step 1 | .02 | .02 | .02 | .02 | .02 | ||||||||||
| Group (TBI vs. OI) | −.15 | −.15 | −.15 | −.15 | −.15 | −.15 | −.15 | −.15 | −.15 | −.15 | |||||
| Step 2 | .09* | .09* | .21** | .05 | .02 | ||||||||||
| Peer rating | .08 | .08 | .25 | .26* | .21 | .20*** | −.15 | −.17 | −.01 | −.01 | |||||
| Self-rating | −.30 | −.32* | .08 | .08 | .37 | .38** | −.09 | −.10 | −.14 | −.15 | |||||
| Step 3a | .07* | .07* | – | – | – | ||||||||||
| Peer rating squared | .28 | .41* | −.28 | −.40* | – | – | – | – | – | – | |||||
| Self-rating squared | – | – | – | – | – | – | – | – | – | – | |||||
| Step 4 | .04 | .00 | .01 | .01 | .00 | ||||||||||
| Group X peer rating | .04 | .14 | .05 | .14 | −.02 | −.05 | .12 | .39 | −.03 | −.09 | |||||
| Group X self-rating | .18 | .56 | .02 | .07 | −.12 | −.35 | −.08 | −.26 | .06 | .19 | |||||
| Step 5 | .00 | .05* | .01 | .01 | .07* | ||||||||||
| Peer X self-rating | .01 | .01 | .25 | .31* | −.08 | −.08 | .11 | .15 | .27 | .32* | |||||
| Step 6 | .00 | .00 | .00 | .01 | .00 | ||||||||||
| Group X peer X self-rating | .05 | .16 | −.03 | −.08 | −.00 | −.01 | −.10 | −.50 | −.03 | −.11 | |||||
Note. Five distinct regression analyses are reported in this table, one for each of the ECP subscales. ECP = Extended Class Play, TBI = traumatic brain injury. r = partial correlation.
N = 71; df (6, 65).
*p < .05; **p < .01; ***p < .10.
aStep 3 terms represent the quadratic effects of peer and self-ratings.
Higher self-ratings of aggression predicted lower parent-reported adjustment. Peer ratings of aggression did not predict adjustment, nor did the peer-rating X self-rating interaction.
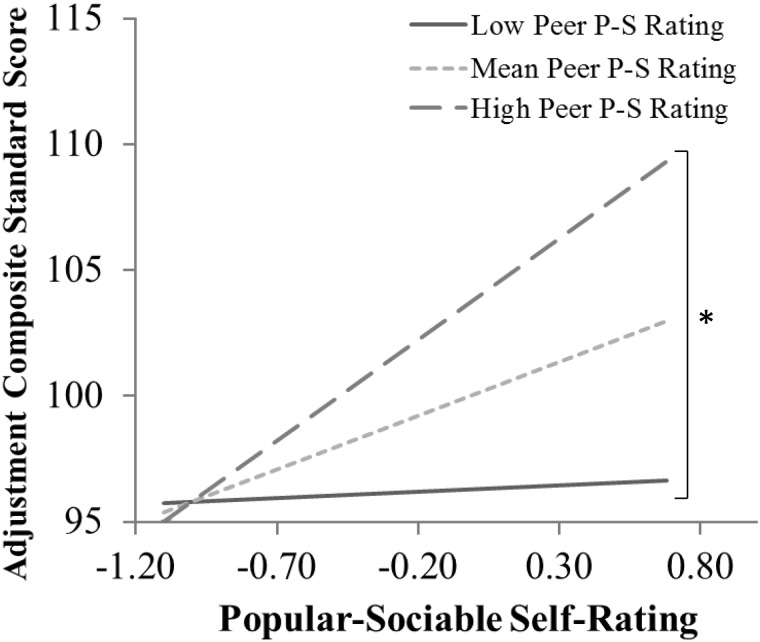
Higher peer ratings of popular-sociable behavior predicted higher parent-reported adjustment, but self-ratings did not. The self- X peer-rating interaction for popular-sociable behavior was also a significant predictor, such that the higher self than peer ratings (i.e., overestimation of popular-sociable behavior) predicted poorer adjustment (see Figure 4). Children who rated themselves positively and also were rated positively by peers had the best parent-reported adjustment. This interaction remained significant after controlling for the significant quadratic effect of peer ratings.
Figure 4.
Adjustment composite standard scores by Extended Class Play Popular-Sociable self-rating at different levels of Popular-Sociable peer ratings. P-S = Popular-Sociable. Higher Popular-Sociable scores reflect greater popularity-sociability. Higher adjustment composite scores reflect better adjustment. The Peer rater by Self-rater interaction was significant, with follow-up analysis indicating significant differences in adjustment scores between those with low versus high peer P-S ratings only at higher levels of self P-S ratings (i.e., the right side of the graph). The findings indicate that adjustment is poorer in children who rate themselves high on popular-sociable behavior, but whose peers rate them low; in other words, children who overestimate their popularity-sociability have poorer adjustment. *p < .05.
Higher self-ratings of prosocial behavior predicted higher parent-reported adjustment, and a similar marginal effect was found for peer ratings. The self-rating X peer rating interaction for prosocial behavior was not significant.
Neither self- nor peer ratings of rejection-victimization nor their interaction predicted adjustment.
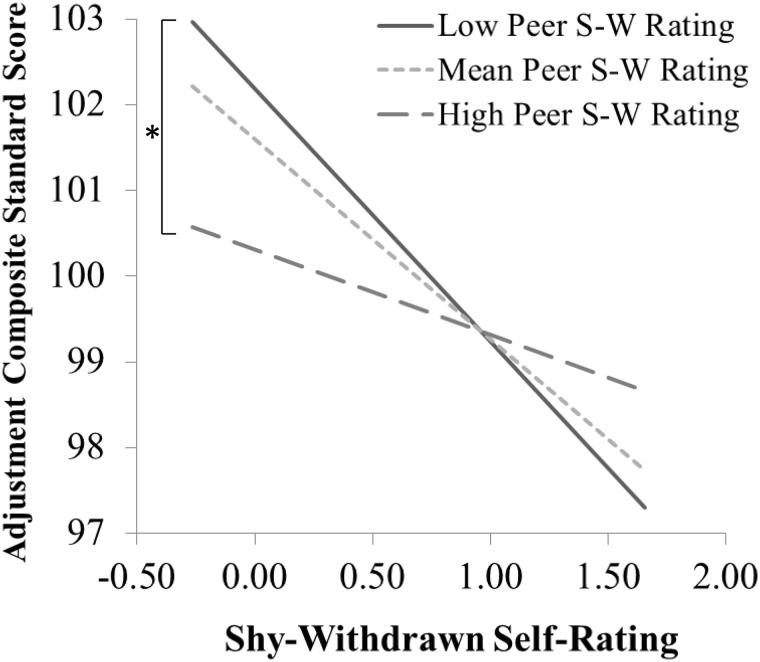
Neither self- nor peer ratings of shy-withdrawn behavior predicted adjustment. However, the self-rating X peer rating interaction for shy-withdrawn behavior was a significant predictor, such that lower self- than peer ratings (i.e., underestimation of shy-withdrawn behavior) predicted poorer adjustment (Figure 5). Children who rated themselves as low in shy-withdrawn behavior and also were rated low by peers had the best parent-rated adjustment.
Figure 5.
Adjustment composite standard scores (M = 100, SD = 15) by Extended Class Play Shy-Withdrawn self-rating z-scores at different levels of Shy-Withdrawn peer ratings. S-W=Shy-Withdrawn. Higher Shy-Withdrawn scores reflect greater shyness-withdrawal. Higher adjustment composite scores reflect better adjustment. The interaction effect was significant, with follow-up analysis indicating significant differences in adjustment scores between those with low versus high peer S-W ratings only at lower levels of self S-W ratings (i.e., the left side of the graph). The findings indicate that adjustment is poorer in children who rate themselves low for shy-withdrawn behavior, but whose peers rate them high; in other words, children who underestimate their shyness-withdrawal have poorer adjustment. *p < .05.
None of the three-way interactions of group X self-rating X peer rating reached statistical significance across the five ECP subscales, indicating that the effects of peer–self discrepancies were consistent across the TBI and OI groups.
Discussion
Overall, our findings suggest that children with TBI demonstrate significant agreement with peers’ perceptions of their social attributes. A notable exception is that children with severe TBI underestimate the extent to which they are rejected-victimized according to peers. Inaccurate self-perceptions of rejection-victimization may be associated with the poor quality of peer relationships and fewer mutual friendships of children with TBI (Yeates et al., 2013), consistent with research in community samples with aggressive children (Orobio deCastro, Brendgen, Van Boxtel, Vitaro, & Schaepers, 2007). Unexpectedly, we found that children with OI tend to overestimate the degree to which they are rejected-victimized and underestimate their prosocial behavior relative to their peers’ rating. We conceptualized this as a “modesty” effect.
EF abilities helped to predict discrepancies between self- and peer ratings of popular/sociable, prosocial, and rejected/victimized scales on the ECP. Better EF predicted more “humble” discrepancies (i.e., self-underestimation); conversely, poorer EF predicted overestimation of positive social attributes and underestimation of negative social attributes by children relative to peers. In contrast, TOM was only predictive of discrepancies in ratings of aggression, and in an unexpected direction, such that better TOM predicted higher peer than self-ratings of aggression. This finding is generally inconsistent with previous research; one potential explanation is that children with higher TOM in our sample may have been better able to rationalize their aggressive behaviors. Regardless, the current findings suggest that EF may be more important or consistent as a predictor of children’s social self-awareness than TOM. In adults, however, lack of awareness has been linked to difficulties with both social information processing and EF (Bivona et al., 2008, 2014; Bogod, Mateer, & MacDonald, 2003); thus, further research is needed to examine other aspects of social information processing (e.g., social problem solving) as potential predictors of self-awareness in children with TBI.
When a discrepancy occurs between peer and self-ratings of certain social attributes (specifically, popularity/sociability and shyness/withdrawal), parent-rated adjustment is poorest for children who show an “immodest” response style (i.e., rate themselves more positively than their peers rate them). This finding is consistent with research on childhood ADHD (Mikami, Calhoun, & Abikoff, 2010). Substantial research has investigated interventions for improving awareness of deficits in adults with TBI (see Fleming & Ownsworth, 2006, for a review), but very few studies have attempted to foster awareness in children with TBI. Our findings provide preliminary support for the development of empirical approaches to increasing awareness of social difficulties for children with TBI, given that lack of awareness in some domains is associated with poorer psychosocial adjustment.
On the other hand, self- and peer ratings of social attributes were also independent predictors of parent-reported adjustment. This finding emphasizes the importance of incorporating multiple perspectives in assessing social competence in children with TBI. Previously, researchers have found substantial discrepancies in the reports of children with TBI and their parents on measures of quality of life and metacognitive difficulties (Green, Godfrey, Soo, Anderson, & Catroppa, 2012; Stancin et al., 2002; Wilson, Donders, & Nguyen, 2011). Furthermore, children with TBI are less accurate than healthy children on tasks of cognitive self-appraisal (Hanten, Bartha, & Levin, 2000), and greater discrepancies between actual and perceived cognitive performance predict higher levels of parent-reported behavior difficulties (Kruger et al., 2011). To our knowledge, however, ours is the first study in which self- and peer perceptions of social attributes in children with TBI were compared. Notably, the percent of variance accounted for by peer and self-ratings, as well as by interrater discrepancies, were generally small to medium in size. Other child characteristics, such as social problem solving, are also likely to contribute to explaining adjustment in children with history of TBI (Yeates et al., 2007).
To assess discrepancies between peer and self-ratings of social attributes as predictors of psychosocial adjustment, we used a novel regression-based framework (De Los Reyes et al., 2013; Laird & De Los Reyes, 2013) instead of the more traditional approach of treating discrepancy scores as independent variables. We found the model to be useful in better delineating the roles of peer and self-ratings, and discrepancies between them, as predictors of adjustment. We encourage investigators exploring the consequences of interrater discrepancies to consider using this regression-based approach in future research. Furthermore, future methodological research should explore whether the use of discrepancy scores as dependent variables presents its own statistical drawbacks, and if so, explore alternative approaches to this form of analysis.
Limitations of the present study include the small sample size, especially in the severe TBI group. Unfortunately, classroom data were not available for all children in the larger parent study, and the small group sizes limited our ability to compare severe with mild/moderate TBI groups, for example, and reduced the statistical power of our study more generally. The relation between SES and injury severity is also a potential problem because it may confound our findings given that the effect of SES cannot be entirely accounted for. However, the lack of group differences in SES after accounting for injury mechanism, in addition to the lack of evidence for recruitment bias, suggests that group differences in SES are intrinsically related to TBI severity.
In the future, researchers should explore why some children with TBI display accurate self-perceptions of peer relationships relative to peers, while others show a lack of awareness of how peers perceive their social attributes. Identifying cognitive, environmental, family, and injury-related variables that contribute to limited insight among children with TBI will be an important precursor to the development of intervention programs that can enhance awareness and improve social outcomes in children with TBI.
Funding
This work was supported by the National Institute of Child Health and Human Development at the National Institutes of Health (grant number 5 R01 HD048946 to K.O.Y.).
Conflicts of interest: None declared.
References
- Bivona U, Ciurli P, Barba C, Onder G, Azicnuda E, Silvestro D, Mangano R, Rijon J, Formisano R. Executive function and metacognitive self-awareness after severe traumatic brain injury. Journal of the International Neuropsychological Society. 2008;14:862–868. doi: 10.1017/S1355617708081125. doi:10.10170S1355617708081125. [DOI] [PubMed] [Google Scholar]
- Bivona U, Riccio A, Ciurli P, Carlesimo G A, Donne V D, Pizzonia E, Caltagirone C, Formisano R, Costa A. Low self-awareness of individuals with severe traumatic brain injury can lead to reduced ability to take another person’s perspective. Journal of Health Trauma Rehabilitation. 2014;29:157–171. doi: 10.1097/HTR.0b013e3182864f0b. [DOI] [PubMed] [Google Scholar]
- Bogod N M, Mateer C A, MacDonald S W S. Self-awareness after traumatic brain injury: A comparison of measures and their relationship to executive functions. Journal of the International Neuropsychological Society. 2003;9:450–458. doi: 10.1017/S1355617703930104. doi:10.10170S1355617703930104. [DOI] [PubMed] [Google Scholar]
- Boivin M, Poulin F, Vitaro F. Depressed mood and peer rejection in childhood. Development and Psychopathology. 1994;6:483–498. [Google Scholar]
- Brown R L. Epidemiology of injury and the impact of health disparities. Current Opinion in Pediatrics. 2010;22:321–325. doi: 10.1097/MOP.0b013e3283395f13. doi:10.1097/MOP.0b013e3283395f13. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas S A, Goodman K L, Kundey S M A. Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology. 2013;9:123–149. doi: 10.1146/annurev-clinpsy-050212-185617. doi:10.1146/annurev-clinpsy-050212-185617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Agostino A, Taylor H G, Bigler E D, Rubin K H, Vannatta K, Gerhardt C A, Stancin T, Yeates KO. Emotional expression and socially modulated emotive communication in children with traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:34–43. doi: 10.1017/S1355617712000884. doi:10.1017/S1355617712000884. [DOI] [PubMed] [Google Scholar]
- Dennis M, Francis D J, Cirino P T, Schachar R, Barnes M A, Fletcher J M. Why IQ is not a covariate in cognitive studies of neurodevelopmental disorders. Journal of the International Neuropsychological Society. 2009;15:331–343. doi: 10.1017/S1355617709090481. doi:10.1017/S1355617709090481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis M, Simic N, Agostino A, Taylor H G, Bigler E D, Rubin K R, Vannatta K, Gerhardt C A, Stancin T, Yeates K O. Irony and empathy in children with traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:338–348. doi: 10.1017/S1355617712001440. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, Lang A G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Faul M, Xu L, Wald M M, Coronado V G. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- Fleming J M, Ownsworth T. A review of awareness interventions in brain injury rehabilitation. Neuropsychological Rehabilitation. 2006;16:474–500. doi: 10.1080/09602010500505518. doi:10.1080/09602010500505518. [DOI] [PubMed] [Google Scholar]
- Fleming J M, Strong J. Self-awareness of deficits following acquired brain injury: Considerations for rehabilitation. British Journal of Occupational Therapy. 1995;58:55–60. [Google Scholar]
- Green L, Godfrey C, Soo C, Anderson V, Catroppa C. Agreement between parent-adolescent ratings on psychosocial outcome and quality-of-life following childhood traumatic brain injury. Developmental Neurorehabilitation. 2012;15:105–113. doi: 10.3109/17518423.2011.638331. doi:10.3109/17518423.2011.638331. [DOI] [PubMed] [Google Scholar]
- Gresham F M, Lane K L, MacMillan D L, Bocian K M, Ward S L. Effects of positive and negative illusory biases: Comparisons across social and academic self-concept domains. Journal of School Psychology. 2000;38:151–175. doi:10.1016/S0022-4405(99)00042-4. [Google Scholar]
- Hanten G, Bartha M, Levin H S. Metacognition following pediatric traumatic brain injury: A preliminary study. Developmental Neuropsychology. 2000;18:383–398. doi: 10.1207/S1532694206Hanten. [DOI] [PubMed] [Google Scholar]
- Harrison P L, Oakland T. ABAS-II: Adaptive behavior assessment system. 2nd ed. San Antonio, TX: Harcourt Assessment; 2003. [Google Scholar]
- Hayes A F. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press; 2013. [Google Scholar]
- Heaton S C, Reader S K, Preston A S, Fennell E B, Puyana O E, Gill N, Johnson J H. The Test of Everyday Attention for Children (TEA-Ch): Patterns of performance in children with ADHD and clinical controls. Child Neuropsychology. 2001;7:251–264. doi: 10.1076/chin.7.4.251.8736. doi:10.1076/chin.7.4.251.8736. [DOI] [PubMed] [Google Scholar]
- Howard I, Joseph J G, Natale J E. Pediatric traumatic brain injury: Do racial/ethnic disparities exist in brain injury severity, mortality, or medical disposition? Ethnicity & Disease. 2005;15(Suppl. 5):51–56. [PubMed] [Google Scholar]
- Kruger C E, Rosen H J, Taylor H G, Espy K A, Schatz J, Rey-Casserly C, Kramer J H. Know thyself: Real-world correlates of self-appraisal accuracy. Clinical Neuropsychology. 2011;25:741–756. doi: 10.1080/13854046.2011.569759. doi:10.1080/13854046.2011.569759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laird R D, De Los Reyes A. Testing informant discrepancies as predictors of early adolescent psychopathology: Why difference scores cannot tell you what you want to know and how polynomial regression may. Journal of Abnormal Child Psychology. 2013;41:1–14. doi: 10.1007/s10802-012-9659-y. doi:10.1007/s10802-012-9659-y. [DOI] [PubMed] [Google Scholar]
- Langlois J A, Rutland-Brown W, Thomas K E. The incidence of traumatic brain injury among children in the United States: Differences by race. Journal of Head Trauma Rehabilitation. 2005;20:229–238. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- Manly T, Anderson V, Nimmo-Smith I, Turner A, Watson P, Robertson I H. The differential assessment of children’s attention: The Test of Everyday Attention for Children (TEA-Ch), normative sample and ADHD performance. Journal of Child Psychology and Psychiatry. 2001;42:1065–1081. doi: 10.1111/1469-7610.00806. [DOI] [PubMed] [Google Scholar]
- Masten A S, Morison P, Pellegrini D S. A revised class play method of peer assessment. Developmental Psychology. 1985;21:523–533. [Google Scholar]
- Mikami A Y, Calhoun C D, Abikoff H B. Positive illusory bias and response to behavioral treatment among children with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2010;39:373–385. doi: 10.1080/15374411003691735. doi:10.1080/15374411003691735. [DOI] [PubMed] [Google Scholar]
- Orobio de Castro B, Brendgen M, Van Boxtel H, Vitaro F, Schaepers L. ‘Accept me, or else’: Disputed overestimation of social competence predicts increases in proactive aggression. Journal of Abnormal Child Psychology. 2007;35:165–178. doi: 10.1007/s10802-006-9063-6. [DOI] [PubMed] [Google Scholar]
- Reynolds C R, Kamphaus R W. BASC-2: Behavior assessment system for children. 2nd ed. Minneapolis, MN: Psychological Corporation; 2004. [Google Scholar]
- Rosema S, Crowe L, Anderson V. Social function in children and adolescents after traumatic brain injury: A systematic review. Journal of Neurotrauma. 2012;29:1277–1291. doi: 10.1089/neu.2011.2144. doi:10.1089/neu.2011.2144. [DOI] [PubMed] [Google Scholar]
- Rubin K H, Wojslawowicz J, Burgess K, Rose-Krasnor L, Booth-LaForce C. The friendships of socially withdrawn and competent young adolescents. Journal of Abnormal Child Psychology. 2006;34:139–153. doi: 10.1007/s10802-005-9017-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salley C G, Vannatta K, Gerhardt C A, Noll R B. Social self-perception accuracy: Variations as a function of child age and gender. Self and Identity. 2010;9:209–223. doi:10.1080/15298860902979224. [Google Scholar]
- Sherer M, Bergloff P, Levin E, High W M, Jr, Oden K E, Nick T G. Impaired awareness and employment outcome after traumatic brain injury. Journal of Head Trauma Rehabilitation. 1998;13:52–61. doi: 10.1097/00001199-199810000-00007. [DOI] [PubMed] [Google Scholar]
- Stancin T, Drotar D, Taylor H G, Yeates K O, Wade S L, Minich N M. Health-related quality of life of children and adolescents after traumatic brain injury. Pediatrics. 2002;109:e34. doi: 10.1542/peds.109.2.e34. [DOI] [PubMed] [Google Scholar]
- Trudel T M, Tryon W W, Purdum C M. Awareness of disability and long-term outcome after a traumatic brain injury. Rehabilitation Psychology. 1998;43:267–281. doi:10.1037/0090-5550.43.4.267. [Google Scholar]
- Wechsler D. Wechsler abbreviated scale of intelligence (WASI) San Antonio, TX: Harcourt Assessment; 1999. [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children—4th Edition (WISC-IV) San Antonio, TX: Harcourt Assessment; 2003. [Google Scholar]
- Williams D H, Levin H S, Eisenberg H M. Mild head injury classification. Neurosurgery. 1990;27:422–428. doi: 10.1097/00006123-199009000-00014. [DOI] [PubMed] [Google Scholar]
- Wilson K R, Donders J, Nguyen L. Self and parent ratings of executive functioning after adolescent traumatic brain injury. Rehabilitation Psychology. 2011;56:100–106. doi: 10.1037/a0023446. doi:10.1037/a0023446. [DOI] [PubMed] [Google Scholar]
- Wojslawowicz Bowker J C, Rubin K H, Burgess K B, Rose-Krasnor L, Booth-LaForce C L. Behavioral characteristics associated with stable and fluid best friendship patterns in middle childhood. Merrill-Palmer Quarterly. 2006;52:671–693. doi:10.1353/mpq.2006.0000. [Google Scholar]
- Yeates K O. Traumatic brain injury. In: Yeates K O, Ris M D, Taylor H G, Pennington B F, editors. Pediatric neuropsychology: Research, theory, and practice. 2010. (2nd ed., pp. 112–146). New York, NY: Guilford. [Google Scholar]
- Yeates K O, Bigler E D, Abildskov T, Dennis M, Gerhardt C A, Vannatta K, Rubin K H, Stancin T, Taylor H G. Social competence in pediatric traumatic brain injury: From brain to behavior. Clinical Psychological Science. 2014;2:97–107. doi:10.1177/2167702613499734. [Google Scholar]
- Yeates K O, Bigler E D, Dennis M, Gerhardt C A, Rubin K H, Stancin T, Taylor H G, Vannatta K. Social outcomes in childhood brain disorder: A heuristic integration of social neuroscience and developmental psychology. Psychological Bulletin. 2007;133:535–556. doi: 10.1037/0033-2909.133.3.535. doi:10.1037/0033-2909.133.3.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates K O, Gerhardt C A, Bigler E, Abildskov T, Dennis M, Rubin K H, Stancin T, Taylor H G, Vannatta K. Peer relationships of children with traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:518–527. doi: 10.1017/S1355617712001531. doi:10.1017/S1355617712001531. [DOI] [PubMed] [Google Scholar]
- Zakriski A L, Coie J D. A comparison of aggressive-rejected and nonaggressive-rejected children’s interpretations of self-directed and other-directed rejection. Child Development. 1996;67:1048–1070. [PubMed] [Google Scholar]