Abstract
Introduction
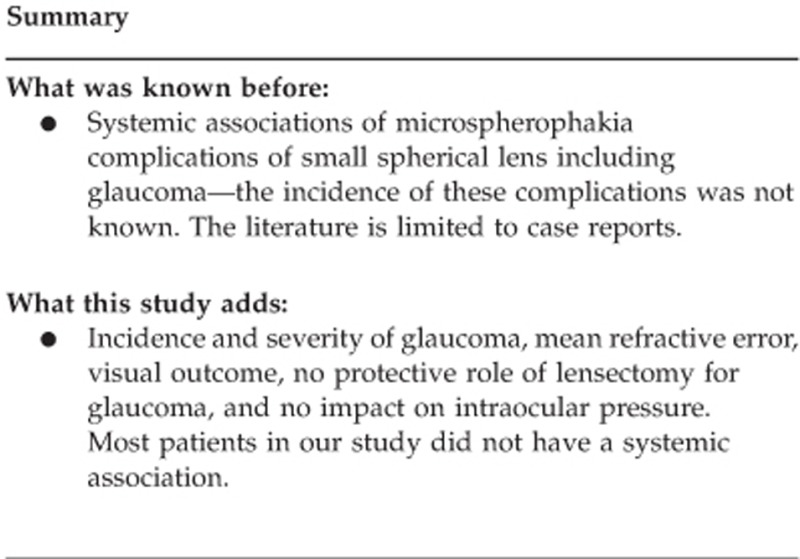
A number of ocular complications have been reported in microspherophakia. The literature however is limited to small case reports and the incidence of these complications is largely unknown. Our study describes a series of patients who presented to our hospital from 1998 to 2008.
Material and methods
Data on the clinical and surgical findings of patients presented to us from 1998 to 2008 with microspherophakia were retrieved from the medical records and the results analyzed.
Results
Thirty-six eyes of 18 patients were reviewed. The mean age at presentation was 16±10 years. All patients had varying degrees of lenticular myopia with a mean of −11.07±5.03 D. Glaucoma developed in 16 eyes (44.4%). Half of them had high IOP at presentation. Despite medical and surgical management IOP remained high in five eyes at the last follow-up. Sixteen eyes (44.4%) required lensectomy for dislocated crystalline lens. Lensectomy did not have any impact on the intraocular pressures. Homocysteinuria was the most common systemic association noted.
Conclusion
Microspherophakia is associated with a high incidence of lenticular myopia, subluxation of the crystalline lens and glaucoma. Management of glaucoma is difficult with the IOP remaining high in spite of combined medical and surgical management.
Introduction
Microspherophakia is an uncommon bilateral condition characterized by abnormally lax zonules, leading to the development of a small spherical lens. It has been reported to be associated with many conditions like Weil–Marchesani syndrome, Marfan's syndrome, Alport's syndrome, Homocysteinuria, Klinefelter's syndrome, and mandibulofacial dystosis.1, 2 Ocular complications of microsperophakia include high myopia, pupillary block and secondary angle closure glaucoma, and complications associated with anterior or posterior dislocation of the lens.3, 4 The Literature is largely limited to isolated case reports/series and the incidence of these complications is unknown. Glaucoma has been reported in microspherophakia associated with Weil–Marschesani syndrome, but is not so well described with other systemic associations.1 Our paper describes a series of 18 patients with microspherophakia, who presented to our hospital from 1998 to 2008.
Material and methods
The surgical and outpatient records of patients who presented to us with microspherophakia from 1998 to 2008 were reviewed. Only patients who had completed a minimum of 6 months of follow-up were included. The study adheres to the tenets of the Declaration of Helsinki and was approved by the institution review board of our hospital. Data with regard to complaints, age at presentation, clinical findings, and surgical findings were collected. As a routine practice in our hospital, all patients with microspherophakia are screened for homocysteinuria by a urine screening test. Serum homocysteine levels are estimated in those who test positive on urine screening. All patients were evaluated for systemic associations by a general physician.
Lensectomy (when indicated) was done by the limbal route in cases of anterior dislocations. Patients with posterior dislocation of the crystalline lens were managed by a pars plana lensectomy. All patients were taken up for surgery under general anesthesia with endotracheal intubation. Those noted to have high intraocular pressures were given intravenous mannitol just before surgery. The surgical area was prepared with 5% povidone iodine and covered by a self-adhesive drape. In cases of anterior dislocations, two side ports were made at 0200 and 1000 hours with an angled side port blade. The anterior capsule was nicked with the side port blade and the cut extended with Vannas scissors. As much of cortical matter as possible was aspirated with a Symcoe's cannula. The remaining bag and cortical matter were removed with automated vitrectomy. Sufficient anterior vitrectomy and a peripheral iridectomy (if not already present) were done with the vitreous cutter. Postoperatively, the patient was treated with a steroid antibiotic combination and cycloplegics for 6 weeks. Anti-glaucoma medications were added when needed. Patients were discharged on the third postoperative day and reviewed at 1 month and 6 monthly intervals thereafter (more frequently if the intraocular pressures were high). Pars plana lensectomy was done in cases of posterior dislocations with 20-G vitrectomy. Patients who did not undergo a lensectomy were treated by a prophylactic Nd : Yag peripheral iridotomy (PI) and followed-up with regular monitoring of intraocular pressures.
Results
Thirty-six eyes of 18 patients were reviewed. The age at presentation ranged from 5 to 35 years with a mean of 16±10 years. The patient details are listed in Table 1. The mean follow-up was 8.55±3.98 years. The commonest presenting complaint was defective vision (n=14), followed by pain in the eye (n=5). One patient was identified as having microspherophakia on a routine ocular examination. Six eyes had anterior dislocation of the crystalline lens at presentation and 10 eyes developed subluxation at subsequent follow ups.
Table 1. Clinical data of patients.
| Sr. No. | Glaucoma Y/N | No. of G. Mx | Age and sex at prtn (years) | Durtn of Follow-up (years) | Complaints | BCVA RE at prtn | BCVA LE at prtn | Refraction RE at prtn* | Refraction LE at prtn* | Lens status | Homocystinuria | Other association | Lensectomy | Trabeculectomy | No. of G. Mx | BCVA RE at f f | BCVA LE at f f | Axial length RE (mm) | Axial length LE (mm) | Tn re at prtn | Tn le at prtn | Tn Rt at f f | Tn Lt.at f f | YAG PI | Gonio at prntn | Fundus at prtn | Fundus at f f |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | BE: Y | RE: 2 LE: 1 | 8/f | 13 | Def. Vn. BE | 6/18 | 6/18 | −20 | −20 | + | BE | RE: 2 LE: 1 | 6/18 | 6/12 | 26.11 | 26.11 | 24 | 24 | 16 | 28 | BE | BE: open | BE: CDR: 0.5 | BE: CDR 0.9 | |||
| 2 | BE: N | 8/f | 8 | Def. Vn. BE 6 months | 5/60 | 4/60 | Phakic −10.5/−7 at 180; aphakic 10.5/1 at 90 | Phakic −11.5/−6 at 180; aphakic | BE subluxation | + | BE | 1/60 | 1/60 | 22.6 | 22.7 | 8 | 16 | LE:D:pale RE: normal | LE:D:pale; RE: normal | ||||||||
| 3 | BE: N | 7/m | 4 | Def. Vn. 1 week | 6/24 | 6/36 | −10 | −11.0/−2.0 at 60 | BE subluxation | + | RE: PPL, LE: limbal | 6/36 | 6/36 | 20.35 | 20.17 | 12 | 9 | 10 | 11 | BE | Normal | Normal | |||||
| 4 | BE: N | 8/f | 5 | Def. Vn. BE | Not | Not coop | −10 | −22 | RE: subluxation; LE: ant. Dislocation at prtn | C | Cerebral palsy | BE | Not coop | Not coop | 14 | 9 | 16 | 13 | LE:pale, RE: fundus not clear | As before | |||||||
| 5 | BE: N | 5/f | 6 | Pain, redness LE 2 days (injury with Finger) | 6/60 | 6/24 | BE: ant. Dislocation LE: at prtn | C | BE | 6/36 | 6/36 | 21.9 | 21.9 | 13 | 12 | 11 | 13 | RE | Normal | Normal | |||||||
| 6 | BE: Y | BE: 2 | 18/f | 5 | Pain BE 6 months | 6/9 | 6/6 | −19 | −15 | BE: subluxation | BE: 2 | 6/9 | 6/9 | 16 | 16 | 14 | 14 | BE | BE>1800 PAS | RE: CDR: 0.9, LE: CDR: 0.85 | RE: CDR:−0.9, LE-CDR: 0.8.50 | ||||||
| 7 | BE: N | 19/m | 12 | Def. Vn. BE | 6/9 | 6/9 | −9.0/−3.0 at 180 | −8.0/−3.0 at 180 | Weil–Marchesani | 6/9 | 6/9 | 17 | 15 | 16 | 16 | BE | Open | RE-CDR: 0.65, LE.CDR: 65 | BE: CDR: 0.6 | ||||||||
| 8 | BE: N | 10/f | 9 | Def. Vn. BE | 6/9 | 6/9 | −5.50/−1.0 at 105 | −5.50/−1.50 at 75 | RE lens subluxation | BE: PPL | 6/9 | 6/9 | 20.7 | 20.56 | 10 | 11 | 20 | 15 | BE | BE: narrow | BE: CDR: 0.4 | BE: CDR:0.40 | |||||
| 9 | BE: Y | BE: 1 | 25/m | 5 | RE pain | No PL | 6/6 | −4/−2.0 at 180 | BE | BE: 1 | No PL | 6/6 | 50 | 28 | 26 | 16 | BE | RE: closed, LE: >1800 PAS | RE-GOA, LE-CDR: 0.4 | RE-GOA, LE-CDR: 0.7 | |||||||
| 10 | RE: Y | RE: 1 | 20/f | 9 | Def. Vn. 7 years | 6/6 | 6/6 | −9 | −7.0/−2.0 at 165 | 6/6 | 6/6 | 18 | 18 | 30 | 18 | BE | RE: closed, LE: narrow | BE: CDR: 0.3 | BE: normal | ||||||||
| 11 | BE: Y | BE: 1 | 14/f | 7 | Def. Vn. BE | 6/18 | 6/12 | −12 | −13 | BE: 1 | 6/12 | 6/12 | 21.6 | 21.27 | 14 | 14 | 18 | 18 | BE | BE: closed angles | BE: CDR: 0.6 | BE: CDR: 0.7 | |||||
| 12 | BE: Y | BE: 1 | 29/f | 14 | Def. Vn. pain LE | 6/6 | 6/6 | −9 | −11 | RE: subluxation | Weil–Marchesani | BE: PPL | BE: 1 | 6/6 | 6/6 | 20.85 | 20.99 | 20 | 26 | 18 | 20 | BE | BE: angles closed | BE: CDR: 0.3 | BE: CDR: 0.6 | ||
| 13 | BE: N | 31/m | 15 | Def. Vn. BE | 6/9 | 6/9 | −8.50/−1.5 at 15 | −8.0/−1.5 at 150 | 6/18 | 6/18 | 23.35 | 23.29 | 14 | 14 | 10 | 10 | BE | Open | RP with disc pallor | RP with COA | |||||||
| 14 | BE: Y | BE: 1 | 6/m | 16 | Check up | 6/12 | 6/12 | −4 | −4 | Tourete syndrome | BE: 1 | 6/9 | 6/9 | 20.75 | 20.65 | 20 | 21 | 16 | 14 | BE | 900 PAS, rest narrow—SL seen | BE: 0.6 | BE: 0.6 | ||||
| 15 | RE: Y | RE: 3 | 6/f | 10 | Def Vn. BE | Able to pick up cake decoration | Able to pick up cake decoration | BE: ant. Dislocation at prtn | BE | RE: AGV implant then BE DLCP | RE: 3 | 2/60 | PL+ | 25.59 | 25.59 | 25 | 31 | 30 | 35 | Gonio not available | RE hypoplastic disc. LE: CDR: 0.8 | RE: 0.8, LE-Goa | |||||
| 16 | BE:Y | BE: 1 | 35/m | 8 | Def. Vn. pain LE 1 week. | 6/60 | No PL | BE: subluxation, RE: cataractus | RE | RE | BE: 1 | 1/60 | NO PL | 21.08 | - | 20 | NVG | 15 | Absolute | RE | Angles closed | RE 0.8; LE: NVG | RE: 0.8; LE: NVG | ||||
| 17 | BE: N | 29/m | 4 | Def. Vn. 20 years | 6/6 | 6/6 | −12 | −12.0/−1.50 at 90 | BE: subluxation | Marfan's syndrome | 6/6 | 6/6 | 16 | 18 | 18 | 18 | BE | Open | 0.3 BE | BE:0.3 | |||||||
| 18 | RE: Y | 10/f | 4 | Def. Vn. BE 2.5 years | 6/36 | 3/60 | −12/−1.0 at 180 | −13 | BE: ant. Dislocation RE: at prtn | + | Marfan's syndrome | BE | 6/60 | 6/12 | 22.72 | 22.72 | 15 | 18 | 30 | 10 | RE: CDR: 0.4; LE: CDR: 0.5 | RE: CDR: 0.6; LE: CDR: 0.6 |
Abbreviations: *, phakic area refraction; ant, anterior; BCVA, best corrected visual acuity; C, homocysteinuria confirmed by estimation of plasma homocysteine levels; CDR, cup disc ratio; COA, consecutive optic atrophy; COOP, co-operative; Def, defective; DLCP, diode laser cyclophotocoagulation; Durtn, duration; f f, final follow-up; G Mx, glaucoma medication; GOA, glaucomatous optic atrophy; Gonio, gonioscopy; NA, not available; NC, not co-operative; PAS, peripheral anterial synechie; PI, peripheral iridectomy; PL, perception of light; PPL, pars plana lensectomy; Prtn, presentation; RP, retinitis pigmentosa; SL, Schwalbe's line; Tn, tension (IOP).
If not specified the lensectomy was performed by the limbal route.
Visual outcome
Snellen Visual acuity was available for 30 eyes. The mean presenting visual acuity was 0.51±0.36. Patient no. 4 had cerebral palsy and did not cooperate for vision testing. He was noted to have good fixation at presentation. Visual acuity≥6/18 at presentation was seen in 58.3% of eyes and in 61.1% of eyes at final follow-up. The mean refractive error at presentation (data available for 30 eyes) was −11.07±5.03 D and mean axial length was 22.33±1.9 mm. Four eyes (11.11%) of two patients had axial length >24.5 mm.
Development of glaucoma
Eight eyes (22.2%) of five patients were noted to have an IOP of >21 mm Hg at presentation. Two eyes had no perception of light at presentation and were noted to have absolute glaucoma. One of these had neovascular glaucoma at presentation. In addition, eight eyes of five patients (22.2%—patients 6, 10, 11, 12 and 14) developed high intraocular pressures during subsequent follow-up. Thus the incidence of glaucoma was 44.4% (16 out of 36 eyes).
No association was noted between lens subluxation and the development of glaucoma (P=0.335 by Fisher's exact test). In patient No. 1, the angles were noted to be open. In all other patients, a closed angle mechanism was responsible for the increase in intraocular pressure.
Time to development of glaucoma
Nine out of 18 patients developed glaucoma. Six patients (6/9=66.7%) had glaucoma at presentation. One patient was diagnosed to have glaucoma after 1 year, one patient was noted to have glaucoma after 2 years of follow-up, and another patient was detected to have glaucoma after 9 years. A statistically significance between age or time to detection and glaucoma was not noted by Fisher's exact test (P=0.347).
Surgical management of glaucoma
Twenty-six eyes underwent YAG PI to prevent/relieve a pupillary block during their review. No association was noted between iridotomy and development of glaucoma (P=0.316 by Fisher's exact test). Five eyes underwent trabeculectomy. Ahmed Glaucoma Valve (AGV) was implanted in one eye of patient No. 15 initially, who then received diode cyclophotocoagulation (CPC) in both eyes for uncontrolled glaucoma. Patient No. 1 (open angles) underwent trabeculectomy in both eyes followed by a repeat trabeculectomy and diode CPC in his right eye for poorly controlled glaucoma. Thus 6 out of 16 glaucomatous eyes (37.5%) underwent glaucoma filtering surgery and 3 eyes needed an additional cyclodestructive procedure.
Medical treatment of glaucoma
All the above patients who underwent surgery for glaucoma also received additional anti-glaucoma medication. Altogether, 12 eyes of 16 (75%) were treated with monotherapy whereas 4 eyes (25%) required more than one medication. Despite medical and surgical treatment the IOP remained high in five eyes of four patients at final follow-up.
Lensectomy
Lensectomy was done in 16 eyes (44.4%). The indication for lensectomy was dislocation of the crystalline lens. In four eyes, lensectomy was done by a pars plana route and in the remaining a limbal route was employed. Glaucoma was noted in 6 of 16 eyes (37.5%)—Table 2. No association was noted between lensectomy and the development of glaucoma (P=0.347 by Fisher's exact test). Four eyes had high intraocular pressures noted at presentation (patients 12 and 15, Table 2). All four eyes needed surgical intervention. Two more eyes (patients 16 OD and 18 OD) developed high IOPs during review. No other patient (11 eyes) developed high intraocular pressures during follow-up. The mean IOP prior to lensectomy was 15.71±7.22 mm Hg and the mean IOP after surgery was 16.64±6.76 mm Hg. The differences were not significant (P=0.614). The mean follow-up after lensectomy was 8.56±4 years. Four eyes required supplemental medication for IOP control. One patient underwent an Ahmed valve implant, but was lost to follow-up after surgery. The patient details are mentioned in Table 2. Four of the 12 eyes who had not undergone lensectomy (and had normal IOP's at presentation) developed high intraocular pressures during review.
Table 2. Intraocular pressure and anti-glaucoma medications in patients who underwent lensectomy.
| Patient No. (as mentioned in Table 1) | IOP prior to lensectomy | IOP at last review after lensectomy | Increase/decrease in anti-glaucoma medication | Follow-up after lensectomy | Comments |
|---|---|---|---|---|---|
| 2 OD | na | 8 | 0 | 7 years | |
| 2 OS | na | 16 | 0 | 7 years | |
| 3 OD | 10 | 10 | 0 | 2 years | |
| 3 OS | 11 | 11 | 0 | 2 years | |
| 4 OD | 14 | 16 | 0 | 4 years | |
| 4 OS | 9 | 13 | 0 | 4 years | |
| 5 OD | 13 | 11 | 0 | 6 years | |
| 5 OS | 10 | 13 | 0 | 6 years | |
| 8 OD | 10 | 20 | 0 | 2 years | |
| 8 OS | 11 | 15 | 0 | 2 years | |
| 12 OD | 22 | 18 | +2 | 8 years | On timolol and brimonidine. IOP had spiked to 54 in the RE immediate postoperative period |
| 12 OS | 34 | 20 | +2 | 8 years | on timolol and brimonidine |
| 15 OD | 25 | Lost to follow upa | |||
| 15 OS | 31 | Lost to follow upa | |||
| 16 OD | 20 | 15 | +1 | 8 years | On timolol after trabeculectomy |
| 16 OS | Absolute eye | ||||
| 18 OD | 15 | 30 | +1 | 2 years | On timolol |
| 18 OS | 16 | 10 |
Patient 15 had undergone Ahmed glaucoma valve implantation in the RE and cyclophotocoagulation in BE, but the patient has been lost to follow-up and no further data is available with us.
No surgical intervention
Eight eyes (22.2%) did not require any surgical/medical intervention other than YAG PI during their follow-up.
Systemic/ocular associations
Six patients tested positive on a urine homocysteinuria screening. The diagnosis was confirmed in two patients with estimation of plasma homocysteine levels. The confirmatory test could not be done in other patients because of poor compliance, financial reasons, and loss of follow-up. Systemic evaluation revealed Weil–Marchesani syndrome in two patients, Marfan's syndrome in two, and Tourette syndrome in one. One patient had mental retardation with delayed milestones. He was noted to have high plasma homocysteine levels and was referred to a pediatrician for further management.
Disscussion
Microspherophakia is a rare condition with multiple systemic associations.1, 2 Eight of our patients had isolated microspherophakia. Homocysteinuria was noted to be the commonest systemic association, though it could be confirmed with estimation of plasma levels in only two patients. The other systemic associations were Marfan's and Weil–Marchesani's syndrome. Tourette syndrome has not been reported with microspherophakia and it is likely that its presence was coincidental. One patient with mental retardation was noted to have high plasma homocysteine levels. Mental retardation is a known association of untreated homocysteinuria.5
All patients presented with a high degree of lenticular myopia. Spontaneous dislocation of the crystalline lens is the commonest presenting feature of Weil–Marchesani syndrome and homocysteinuria3, 4, 5 and the same was noted in our study.
Most patients were managed successfully by a limbal route lensectomy. Studies showing results and complications for lensectomy in microspherophakia are difficult to compare due to small number of patients, different etiologies for lens subluxation, and variable length of follow-up. To the best of our knowledge, we report the largest number of patients with microspherophakia managed by limbal route lensectomy. Our series shows that lensectomy via limbal route is a viable option in these patients. The visual outcome in microspherophakia remains guarded and only 61% of patients in our study attained a vision of 6/18 or better at the final follow-up.
Glaucoma was another important complication in our study. Pupillary block glaucoma leading to angle closure is believed to be frequent in Weil–Marchesani syndrome and Homocysteinuria;4, 5 to the best of our knowledge, the incidence of glaucoma has not been previously reported. Glaucoma in microspherophakia can occur by a number of mechanisms. Chronic pupillary block can result in the formation of peripheral anterior synechiae. Crowding of the angle by the spherophakic lens, chronic pupillary block without complete angle closure, and angle abnormalities with agenesis of the angle structures are the other mechanisms reported.1, 6 The incidence of glaucoma in our study was high (44.4%) despite the presence of patent PI in most patients. It is likely that many of these patients had already developed peripheral anterior synechiae and angle closure before a PI was performed. This is substantiated by the fact that half of these patients had high IOP at presentation. Interestingly, one patient was noted to have open angle glaucoma. No angle abnormality was recorded in this patient and she required multiple procedures to bring the IOP under control in the right eye. Management of glaucoma in general was difficult and most patients required multiple medications in addition to surgical management. Three eyes required cyclodestructive procedures to bring the IOP under control. This is in line with published literature.7 Lensectomy did not have any impact on the intraocular pressures and two eyes developed high IOPs during follow-up.
To sum up, microspherophakia is associated with a high incidence of anterior dislocation, lenticular myopia, and advanced glaucoma. Some patients did not require any surgery other than a Nd : YAG PI during their follow-up. Management of glaucoma is difficult and frequently requires multiple medications in addition to surgery. Despite meticulous management the visual outcome remains guarded. Lensectomy did not appear to have any impact on the intraocular pressures.
Acknowledgments
We wish to acknowledge the assistance of Mrs Chandra Secretary Dept of Pediatric Ophthalmology and Mr Vijay Kumar, Biostatistician, Aravind Eye Hospital, Madurai for their assistance in retrieving and analyzing the medical records.
The authors declare no conflict of interest.
References
- Willoughby CE, Wishart PK. Lensectomy in the management of glaucoma in spherophakia. J Cataract Refract Surg. 2002;28 (6:1061–1064. doi: 10.1016/s0886-3350(01)01226-3. [DOI] [PubMed] [Google Scholar]
- Nelson LB, Maumenee IH. Ectopia lentis. Surv Ophthalmol. 1982;27 (3:143–160. doi: 10.1016/0039-6257(82)90069-8. [DOI] [PubMed] [Google Scholar]
- Jensen AD, Cross HE, Paton D.Ocular complications in the Weill-Marchesani syndrome Am J Ophthalmol 197477(2261–269.192. [DOI] [PubMed] [Google Scholar]
- Cruysberg JR, Boers GH, Trijbels JM, Deutman AF. Delay in diagnosis of homocystinuria: retrospective study of consecutive patients. BMJ. 1996;313 (7064:1037–1040. doi: 10.1136/bmj.313.7064.1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JP, O'Keefe M, Bowell R, Naughten ER. Ocular complications in homocystinuria–early and late treated. Br J Ophthalmol. 1989;73 (6:427–431. doi: 10.1136/bjo.73.6.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feiler-Ofry V, Stein R, Godel V. Marchesani's syndrome and chamber angle anomalies. Am J Ophthalmol. 1968;65:862. doi: 10.1016/0002-9394(68)92211-3. [DOI] [PubMed] [Google Scholar]
- Harasymowycz P, Wilson R. Surgical treatment of advanced chronic angle closure glaucoma in Weill-Marchesani syndrome. J Pediatr Ophthalmol Strabismus. 2004;41 (5:295–299. doi: 10.3928/01913913-20040901-08. [DOI] [PubMed] [Google Scholar]


