Abstract
Purpose
To determine the morphologic features of the optic disc and the location of visual field (VF) defect in relation to posterior staphyloma in normal tension glaucoma (NTG) eyes with myopia.
Methods
One hundred and thirty-four NTG patients with myopia were enrolled. B-scan ultrasonography was performed in enrolled patients. Disc tilt ratio, disc torsion, and area of peripapillary atrophy were measured from disc photographs. Patients were classified according to the presence of posterior staphyloma and its location: staphyloma involving the optic disc, staphyloma involving either the supero-temporal side of the optic disc or the infero-temporal side of the optic disc. The relationship between the location of the posterior staphyloma and that of the VF defect was analyzed.
Results
Among 134 eyes, 74 eyes (55.2%) had posterior staphyloma on B-scan ultrasonography. Mean torsion degree was significantly greater in eyes with staphyloma involving the temporal side of the optic disc (19.78±18.00°) compared with eyes with staphyloma involving the optic disc (4.65±4.92°, P=0.001). The frequency of the location of VF damage differed significantly between eyes with staphyloma involving the supero-temporal side and those involving the infero-temporal side of the optic disc (P=0.008), which was not significant in eyes with staphyloma involving the optic disc (P=0.813).
Conclusions
Optic disc torsion was a prominent finding in myopic NTG eyes when posterior staphyloma was located temporal to the optic disc. The location of posterior staphyloma was related to the direction of disc torsion and the location of VF defect.
Introduction
Myopia is thought to be a risk factor for glaucoma development.1, 2, 3 In myopia, the optic disc undergoes morphological changes, such as optic disc tilt, torsion, and peripapillary atrophy (PPA).4, 5, 6 Optic disc tilt and torsion represent the skewed insertion of the optic nerve into the globe and can be acquired during eyeball elongation as myopia develops.7, 8 A recent study observed serial changes in the optic disc of children who developed myopia and showed that optic nerve head (ONH) changes such as disc tilting and development or enlargement of PPA were related to the degree of myopic shift.9 The study proposed that scleral stretching in the peripapillary region may drive these changes of the optic disc in myopia. A previous study analyzing the development of visual field (VF) defects in highly myopic eyes showed that an abrupt change in scleral curvature due to posterior staphyloma is the only factor significantly associated with VF defect progression, suggesting that stretching and distortion of the optic nerve fibers from scleral changes may contribute to cause optic nerve damage.10 In the previous study, we demonstrated that the direction of optic disc torsion is related to the location of glaucomatous damage in normal tension glaucoma (NTG) with myopia.11 We proposed that optic disc torsion and its relationship with the location of the VF defect in myopic NTG eyes may be related to eyeball growth in myopia. However, our previous study did not use direct observation of the posterior part of the eye.
Posterior staphyloma, a protrusion of the posterior shell of the eye globe, is a common characteristic of highly myopic eyes.12, 13 The development of posterior staphyloma is thought to be accompanied by stretching of the posterior fundus, resulting in various retinal lesions.14, 15 Our observations revealed that not only the retina but also the optic disc could be affected by stretching of the posterior fundus when the posterior staphyloma is close to the ONH. To determine the effect of the posterior shape of the globe to glaucomatous optic disc changes and the location of VF defect, we analyzed the relationship between the morphological features of the optic disc and the location of VF damage according to the location of posterior staphyloma in NTG eyes with myopia.
Materials and methods
Subjects
We enrolled 260 consecutive NTG patients with myopia who were seen by a glaucoma specialist (CKP) from March 2012 to September 2012 at the glaucoma clinic of the Seoul St Mary's Hospital, Seoul, Korea. Each patient received a complete ophthalmologic examination, which included a medical history review, measurement of best-corrected visual acuity and refraction, slit-lamp biomicroscopy, gonioscopy, Goldmann applanation tonometry, dilated stereoscopic examination, disc and red-free fundus photography (Canon, Tokyo, Japan), Humphrey VF examination using the Swedish interactive threshold algorithm (SITA) Standard 24-2 test (Carl Zeiss Meditec, Dublin, CA, USA), Heidelberg retina tomography (HRT, Heidelberg Engineering GmbH, Heidelberg, Germany), Cirrus spectral-domain optical coherence tomography (Carl Zeiss Meditec), central corneal thickness measurement using ultrasound pachymetry (Tomey Corp., Nagoya, Japan), axial length measurement using ocular biometry (IOL Master; Carl Zeiss Meditec), and B-scan ultrasonography. Using stereoscopic fundus observations by retinal specialists, the presence of posterior staphyloma and any type of myopic macular and peripheral lesions were recorded.
For NTG diagnosis, patients had to fulfill the following criteria: the presence of glaucomatous optic disc changes (such as diffuse or localized rim thinning, disc hemorrhage, a notch in the rim, or a vertical cup-to-disc ratio higher than that of the other eye by more than 0.2), and glaucomatous VF loss, with both criteria confirmed and agreed on by two glaucoma specialists (HYP and CKP); best-corrected visual acuity better than 20/30; maximum IOP less than 22 mm Hg (without glaucoma medications) during repeated measurements obtained on different days; and an open angle on gonioscopic examination. On the basis of the refractive error and axial length, myopia was defined as a spherical equivalent of greater than −2.00 D or axial length greater than 24.0 mm.
Patients were excluded for any of the following criteria: mean deviation (MD) less than −20.00 dB, a history of any retinal disease, including diabetic or hypertensive retinopathy; a history of eye trauma or surgery, with the exception of uncomplicated cataract surgery; optic nerve disease besides glaucoma; a history of systemic or neurological diseases that could affect the VF; any type of myopic macular or peripheral lesions that could cause VF defects; and a spherical equivalent between −0.50 and −2.00 D. When both eyes of a patient had NTG and met the inclusion and exclusion criteria, one eye was randomly chosen for the study.
The Institutional Review Board of the Seoul St Mary's Hospital approved the study, and the study adhered to the principles of the Declaration of Helsinki.
B-scan ultrasonography and the location of posterior staphyloma
B-scan ultrasonography was performed in all enrolled patients. Axial ultrasonography was performed in a supine position, with both eyes closed in a primary gaze position. A B-scan ultrasound probe was lightly applied with coupling gel to the closed eyelid and centered on the cornea. Horizontal and vertical axial scans passing through the optic nerve were obtained. The probe marker was placed nasally on the horizontal scan (Figure 1a-1, upper right) and superiorly on vertical scans (Figure 1a-2, upper right). To ensure that the B-scan passed through the deepest part of the staphyloma, B-scans were performed until five well-defined images were obtained from each eye.
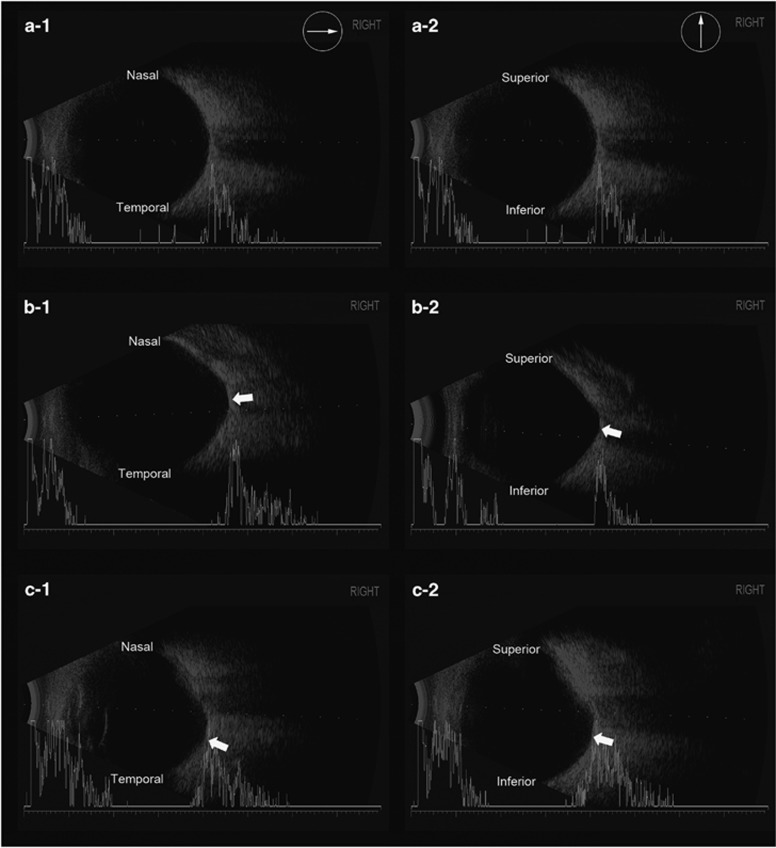
Figure 1.
Images of B-scan ultrasonography. Axial scans passing through the optic nerve were obtained in both horizontal and vertical directions. The probe marker was placed nasally for the horizontal scans and superiorly for the vertical scans, for both right and left eyes. Thus, the upper part of the scan is nasal in the horizontal scan and superior in the vertical scan. The posterior part of an eye without staphyloma shows a uniformly round and regular shape in the both horizontal (a-1) and vertical scans (a-2). The posterior part of an eye with staphyloma involving the optic disc shows conical elongation with the deepest part of the staphyloma at the optic nerve in both the horizontal (b-1) and vertical scans (b-2). The posterior part of an eye with staphyloma involving the temporal side of the optic disc has an irregular protrusion. In the horizontal scan (c-1), the staphyloma is located at the temporal side of the optic nerve. In vertical scan (c-2), the staphyloma is located either superior or inferior to the optic nerve.
The presence and location of posterior staphyloma was determined by both stereoscopic fundus examination and B-scan ultrasonographic findings. The presence of posterior staphyloma by stereoscopic fundus examination was recorded by retinal specialists without knowing the results of VF. The presence of posterior staphyloma was examined by two masked observer (HYP and YJ) without knowing other information about the patient. When no staphyloma was detected on both the stereoscopic fundus examination and B-scan ultrasonography, eyes were classified as having no staphyloma (Figure 1a). When staphyloma was detected only by B-scan ultrasonography, its location was determined by the orientation of both the horizontal and vertical scans. Eyes with posterior staphyloma were further classified by involvement of the optic disc or involvement of the temporal side of the optic disc. Posterior staphyloma involving the optic disc was defined as that centered on the optic disc; the deepest part of the staphyloma was at the optic nerve in both horizontal (Figure 1b-1) and vertical B-scans (Figure 1b-2). A posterior staphyloma involving the temporal side of the optic disc was defined as a staphyloma centered on the fovea with or without inclusion of the temporal side of the optic disc; the deepest part of the staphyloma was at the temporal side of the optic nerve in the horizontal B-scan (Figure 1c-1). In eyes with a staphyloma involving the temporal side of the optic disc, the deepest part of the staphyloma was at either the superior or the inferior side of the optic nerve in the vertical B-scan (Figure 1c-2).
Measurement of optic disc tilt, torsion, and PPA area
Details of measurements have been explained elsewhere.11 Digital retinal photographs centered on the optic disc and macula were obtained using standardized settings with a non-mydriatic retinal camera (Canon). Optic disc tilt, torsion, and PPA area were measured from these photographs by a glaucoma specialist (HYP) using National Institutes of Health image analysis software (ImageJ 1.40; available from http://rsb.info.nih.gov/ij/index.html; developed by Wayne Rasband, National Institutes of Health, Bethesda, MD, USA). Optic disc tilt was identified by the tilt ratio, defined as the ratio between the longest (LD) and shortest (SD) diameters of the optic disc (tilt ratio =LD/SD).16, 17, 18 Optic disc torsion was defined as the deviation of the long axis of the optic disc from the vertical meridian.4, 5 The vertical meridian was identified as a vertical line 90° from a horizontal line connecting the fovea, which is 2° to 6° below the optic disc, to the center of the optic disc. The degree between the vertical meridian and the long axis of the optic disc was named the torsion degree. The β-zone PPA (an inner crescent of chorioretinal atrophy with visible sclera and choroidal vessels) was plotted by using a mouse-driven cursor to trace the disc and PPA margins directly onto the image. The pixel area of the β-zone PPA was then calculated using the ImageJ software (http://imagej.nih.gov/ij/).
Identification of the VF defect locations
VF testing was performed with optical correction using either trial lenses or disposable hydrophilic contact lenses. Glaucomatous VF was defined as one with three or more contiguous points on the pattern deviation plot depressed at the P<5% level with at least one point depressed at the P<1% level, and/or an abnormal corrected pattern SD with P<5% occurring in the normal population in a consistent pattern in the Bjerrum area on two qualifying VFs. consistently reliable VFs (defined as false negative <15%, false positive <15%, and fixation losses <20%).
The pattern deviation plot from the SITA Standard 24-2 test was used to identify the location of the VF defects that occurred in less than 5% of age-matched controls. Eyes with defects within the 26 points of the superior hemifield were classified as the superior defect group. Eyes with defects within the 26 points of the inferior hemifield were classified as the inferior defect group. Eyes with defects involving both the superior and inferior hemifields were classified as having VF defects in both hemifields.
Statistical analysis
The independent t-test and chi-squared test for independent samples were used to assess differences between groups. A P-value of <0.05 was considered to indicate statistical significance. SPSS for Windows (ver. 16.0; SPSS Inc., Chicago, IL, USA) was used for the statistical analyses.
Results
From the 260 eyes of 260 NTG patients, 220 eyes met the inclusion and exclusion criteria. Among those eyes, 76 eyes were further excluded due to unreliable VF that did not met the VF reliability criteria and 10 eyes were excluded due to misaligned B-scan ultrasonography. Remaining of 134 eyes of 134 NTG patients with myopia was further analyzed. Among them, 74 eyes (55.2%) had posterior staphyloma on B-scan ultrasonography. Eyes with staphyloma did not differ from the eyes without staphyloma in terms of age (P=0.301), gender (P=0.477), central corneal thickness (P=0.913), IOP (P=0.508), RNFL thickness measured by Cirrus spectral-domain optical coherence tomography (P=0.394), VF MD (P=0.070), or pattern SD (P=0.089). However, the eyes with staphyloma had a longer axial length (29.55±3.05 mm) than eyes without staphyloma (26.68±1.05, P<0.001).
On HRT, eyes with staphyloma had a significantly larger optic disc (2.55±1.48 mm2) compared with eyes without staphyloma (1.71±0.73 mm2, P=0.002). The mean tilt ratio was 1.39±0.26 in eyes with staphyloma, and this was significantly greater than the mean tilt ratio of 1.30±0.27 in eyes without staphyloma (P=0.016). The mean torsion degree was 17.68±17.57° in eyes with staphyloma and 7.99±11.28° in eyes without staphyloma (P=0.037), which were significantly different. The mean PPA area was significantly larger in eyes with staphyloma (36 874.44±23 286.67 pixel areas) compared with eyes without staphyloma (21 811.74±20 436.54 pixel area, P<0.001; Table 1).
Table 1. Demographic data and optic disc morphology between eyes with and without posterior staphyloma in normal tension glaucoma patients with myopia.
| Without staphyloma (n=74) | With staphyloma (n=60) | P-value | |
|---|---|---|---|
| Age, years | 49.78±8.68 | 50.16±12.06 | 0.301a |
| Gender, male : female | 30 : 44 | 24 : 36 | 0.477b |
| Spherical equivalent, diopters | −8.07±2.67 | −8.87±4.48 | 0.479a |
| Axial length, mm | 26.68±1.05 | 29.55±3.05 | <0.001a |
| Central corneal thickness, μm | 527.05±38.79 | 525.89±43.74 | 0.913a |
| Intraocular pressure, mm Hg | 15.46±2.45 | 16.08±2.08 | 0.508a |
| RNFL thickness, μm | 67.93±10.10 | 65.82±14.03 | 0.394a |
| Visual field MD, dB | −8.99±5.51 | −12.06±8.84 | 0.070a |
| Visual field PSD, dB | 8.71±4.23 | 6.97±3.85 | 0.089a |
| Disc area, mm2 | 1.71±0.73 | 2.55±1.48 | 0.002a |
| Disc ovality ratio | 1.30±0.27 | 1.39±0.26 | 0.016a |
| Torsion degree | 7.99±11.28 | 17.68±17.57 | 0.037a |
| PPA area | 21 811.74±20 436.54 | 36 874.44±23 286.67 | <0.001a |
All data are expressed as mean±SD.
Independent t-test.
Chi-square test.
Eyes with staphyloma were further divided into staphyloma involving the optic disc and eyes (39 eyes, 65%) and staphyloma involving the temporal side of the optic disc (21 eyes, 35%). The two groups did not differ in terms of age (P=0.277), gender (P=0.380), central corneal thickness (P=0.387), IOP (P=0.416), RNFL thickness (P=0.084), VF MD (P=0.193), or pattern SD (P=0.969). However, the eyes with staphyloma involving the optic disc had a longer axial length (30.21±2.98 mm) than eyes with staphyloma involving the temporal side of the optic disc (27.10±1.87 mm, P<0.001).
HRT revealed a significantly larger optic disc in eyes with staphyloma involving the optic disc (3.45±1.03 mm2) compared with eyes with staphyloma involving the temporal side of the optic disc (2.23±0.81 mm2, P=0.045). The mean tilt ratio was similar between the two groups (1.32±0.19 in eyes with staphyloma involving the optic disc and 1.39±0.27 in eyes with staphyloma involving the temporal side of the optic disc, P=0.269). The mean torsion degree showed that eyes with staphyloma involving the temporal side of the optic disc had significantly greater disc torsion (19.78±18.00°) than eyes with staphyloma involving the optic disc (4.65±4.92°, P=0.001). The mean PPA area was significantly larger in eyes with staphyloma involving the optic disc (23 437.46±20 155.80 pixel area) than in eyes with staphyloma involving the temporal side of the optic disc (11 730.42±21 444.62 pixel area, P=0.028; Table 2).
Table 2. Demographic data and optic disc morphology by the location of posterior staphyloma in normal tension glaucoma patients with myopia.
| Staphyloma involving the optic disc (n=39) | Staphyloma involving the temporal side of the optic disc (n=21) | P-value | |
|---|---|---|---|
| Age, years | 51.20±11.78 | 46.10±12.93 | 0.277a |
| Sex, male : female | 14 : 25 | 10 :11 | 0.380b |
| Spherical equivalent, diopters | −9.40±4.76 | −8.68±4.55 | 0.767a |
| Axial length, mm | 30.21±2.98 | 27.10±1.87 | <0.001a |
| Central corneal thickness, μm | 529.17±42.92 | 514.40±46.93 | 0.387a |
| Intraocular pressure, mm Hg | 16.54±2.57 | 15.84±2.34 | 0.416a |
| RNFL thickness, μm | 63.64±13.37 | 74.25±14.25 | 0.084a |
| Visual field MD, dB | −13.09±9.03 | −7.99±7.06 | 0.193a |
| Visual field PSD, dB | 6.96±3.50 | 7.03±5.23 | 0.969a |
| Disc area, mm2 | 3.45±1.03 | 2.23±0.81 | 0.045a |
| Ovality ratio | 1.32±0.19 | 1.39±0.27 | 0.269a |
| Torsion degree | 4.65±4.92 | 19.78±18.00 | 0.001a |
| PPA area | 23 437.46±20 155.80 | 11 730.42±21 444.62 | 0.028a |
All data are expressed as mean±SD.
Independent t-test.
Chi-square test.
Among the eyes with staphyloma involving the optic disc, 2 eyes (5.1%) had superior disc torsion, 14 eyes (35.8%) had inferior disc torsion, and 23 eyes (59.0%) had no optic disc torsion. Among the eyes with staphyloma involving the temporal side of the optic disc, 13 eyes (92.9%) had inferior disc torsion when the staphyloma was located inferiorly, and 6 eyes (85.7%) had superior disc torsion when the staphyloma was located superiorly (Table 3). To determine the relationship between the location of posterior staphyloma and the location of damage, NTG eyes were divided into superior defect, inferior defect, and both defect groups. The frequency and location of the VF defect were not different between eyes with and without staphyloma (P=0.257). Between eyes with staphyloma involving the optic disc and eyes with staphyloma involving the temporal side of the optic disc, the location of VF defect showed a difference that was borderline significant (P=0.065). When eyes with staphyloma involving the temporal side of the optic disc were further divided into inferior and superior staphyloma groups, the location of VF defect was significantly different (P=0.008). Ten eyes (71.4%) from the inferior staphyloma group had superior VF defects, and five eyes (71.4%) from the superior staphyloma group had inferior VF defects (Table 4). In eyes with staphyloma involving the optic disc, there was no significant relationship between the direction of disc torsion and the location of VF damage (P=0.813, Table 5).
Table 3. Frequency of the direction of optic disc torsion by the location of posterior staphyloma.
| Staphyloma involving the optic disc (n=39) |
Staphyloma involving the temporal side of the optic disc (n=21) |
||
|---|---|---|---|
| Inferior staphyloma | Superior staphyloma | ||
| Superior disc torsion | 2 (5.1%) | 0 (0%) | 6 (85.7%) |
| Inferior disc torsion | 14 (35.9%) | 13 (92.9%) | 0 (0%) |
| No disc torsion | 23 (59.0%) | 1 (7.1%) | 1 (14.3%) |
All data are expressed as number of eyes (%).
Table 4. Frequency of the location of visual field defect by the presence and location of posterior staphyloma.
| Without staphyloma (n=74) | With staphyloma (n=60) | P-valuea | Staphyloma involving the optic disc (n=39) |
Staphyloma involving the temporal side of the optic disc (n=21) |
P-valuea | |||
|---|---|---|---|---|---|---|---|---|
| Total | Inferior staphyloma | Superior staphyloma | ||||||
| Superior VF defect | 37 (50.0%) | 23 (38.3%) | 0.257 | 12 (30.8%) | 11 (52.4%) | 10 (71.4%) | 1 (14.3%) | 0.065b/0.008c |
| Inferior VF defect | 18 (24.3%) | 14 (23.3%) | 8 (20.5%) | 6 (28.6%) | 1 (7.1%) | 5 (71.4%) | ||
| Both VF defect | 19 (25.7%) | 23 (38.3%) | 19 (48.7%) | 4 (19.0%) | 3 (21.4%) | 1 (14.3%) | ||
All data are expressed as number of eyes (%).
Chi-square test.
Comparison between eyes with staphyloma involving the optic disc and temporal side of the optic disc.
Comparison between eyes with inferior and superior staphyloma involving the temporal side of the optic disc.
Table 5. Frequency of the location of visual field defect related to the direction of disc torsion in eyes with staphyloma involving the optic disc.
|
Staphyloma involving the optic disc (n=39) |
P Valuea | |||
|---|---|---|---|---|
| Inferior VF defect | Superior VF defect | Both VF defect | ||
| Superior disc torsion (n=2) | 1 (50%) | 0 (0%) | 1 (50%) | 0.813 |
| Inferior disc torsion (n=14) | 3 (21.4%) | 4 (28.6%) | 7 (50.0%) | |
| No disc torsion (n=23) | 4 (17.4%) | 7 (30.4%) | 12 (52.2%) | |
All data are expressed as number of eyes (%).
Chi-square test.
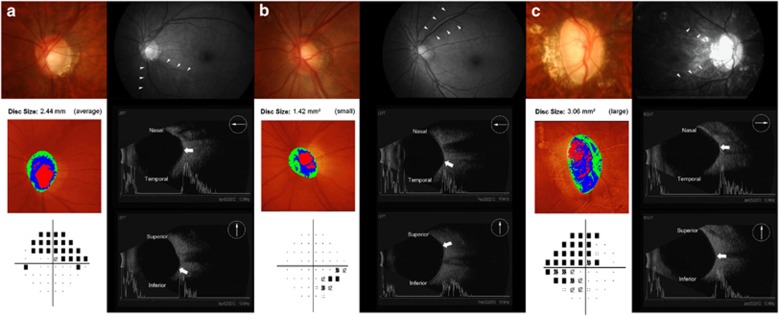
As shown in the representative cases in Figure 2, optic disc morphology and related glaucomatous VF defect differ according to the location of the posterior staphyloma in NTG eyes with myopia.
Figure 2.
Representative cases showing the relationship between optic disc morphology and the location of posterior staphyloma. (a) A 42-year-old male with NTG and myopia (spherical equivalent, −7.5 diopters (D); axial length, 26.75 mm). The mean deviation (MD) on static automated perimetry was −11.55 decibel (dB) with a superior arcuate defect. The optic disc showed a tilt ratio of 1.41 and torsion degree of 22.38°, the direction of the optic disc torsion was inferior, and the damage was at the infero-temporal region. The location of posterior staphyloma was infero-temporal to the optic nerve by B-scan ultrasonography. (b) A 47-year-old male with NTG and myopia (spherical equivalent, −6.75 D; axial length, 25.52 mm). The MD on perimetry was −6.24 dB with an inferior arcuate defect. The optic disc shows a tilt ratio of 1.33 and torsion degree of 29.53°, the direction of the optic disc torsion was superior, and the damage appears at the supero-temporal region. The location of posterior staphyloma was supero-temporal to the optic nerve by B-scan ultrasonography. (c) A 40-year-old male with NTG and myopia (spherical equivalent, −17.00 D; axial length, 27.72 D; a The MD on perimetry was −11.25 dB with a superior and inferior arcuate defect. The optic disc shows a tilt ratio of 1.63 and torsion degree of 8.13°, there was significant disc tilt, but minimal disc torsion, and the damage was in both superior and inferior regions. The location of posterior staphyloma was at the optic disc by B-scan ultrasonography.
Discussion
In this study, we analyzed 134 NTG patients with myopia. Approximately 55.2% of these patients had posterior staphyloma detected by B-scan ultrasonography. The posterior staphyloma involved either the optic disc (65%) or the temporal side of the optic disc (35%) with or without involvement of the optic disc. The optic disc morphology and location of glaucomatous VF damage differed according to the location of the posterior staphyloma.
By analyzing posterior staphyloma in myopic NTG patients, we aimed to examine the effect of posterior scleral stretching or expansion on the ONH. As myopia develops, the globe elongates axially.12, 19, 20 However, elongation of the globe is not symmetrical throughout the posterior part of the eye. As reported by Moriyama et al,21 highly myopic eyes are not simply elongated, but can have out-pouchings, and the shape of eyes with pathological myopia has several types of axial elongation observed by three-dimensional magnetic resonance imaging. Approximately 36% of highly myopic eyes with a chronic VF defect had posterior staphyloma, compared with 15% of eyes without a VF defect.10 Approximately 55% of NTG eyes with myopia had posterior staphyloma in the present study, which is a higher frequency than that previously reported for myopic eyes or highly myopic eyes with a VF defect.10, 22, 23 However, because the study population was different and had various means of axial length, direct comparison is difficult. Importantly, changes in the sclera may influence the morphology and structure of the ONH. Posterior staphyloma is an extreme change in the posterior sclera. Identifying the relationship between posterior staphyloma and features of glaucoma may shed light on the importance of the sclera in the pathogenesis of glaucoma.
Moriyama et al21 showed that temporal protrusion of the posterior part of the eye is more related to VF defects than distortions in other areas. The hypothesis for this observation was that lamina cribrosa deformation from asymmetric stretching of the eyes around the optic disc and the RNFL could disturb the axoplamic flow, leading to VF defects. Additionally, our study shows that posterior staphyloma temporally related to the disc, which could be either supero-temporally or infero-temporally located, predicts the location of glaucomatous damage. This supero- or infero-location of posterior staphyloma leads to asymmetric scleral stretching during axial elongation of the globe when myopia develops. As the morphology of the optic disc also changes during axial elongation of the globe,9 asymmetric elongation of the globe superiorly or inferiorly may drive optic disc torsions in different directions. The present study shows that the driving force behind the direction of optic disc torsion is the location of posterior staphyloma, where the scleral stretching is greatest during myopia development. However, further investigation is needed to clearly state the relationship between disc torsion and staphyloma, which could be a process that occurs simultaneously.
Disc area was significantly different between eyes with posterior staphyloma including the optic disc (3.45±1.03 mm2) and eyes with temporally located posterior staphyloma (2.23±0.81 mm2). When posterior staphyloma included the optic disc, extensive disc enlargement with less disc torsion was apparent. When the posterior staphyloma was located temporally to the optic disc with or without inclusion of part of the optic disc, a small myopic disc with apparent disc tilt or torsion was present. Myopic discs also had PPA, which is thought to be caused by excessive elongation of the eye.24 When the posterior extension of the eyeball includes the optic disc, a larger PPA surrounding the ONH develops. Temporally located staphyloma leads to temporally located PPA (11 730.42 pixel area), which has a smaller area than PPA in eyes with staphyloma including the optic disc (23 437.46 pixel area). Eyes with staphyloma involving the temporal side of the optic disc had a small optic disc with tilt and torsion. The superior or inferior location of the posterior staphyloma relative to the optic disc determined the direction of optic disc torsion and location of the RNFL and VF damage. However, eyes with staphyloma including the optic disc had an extensively enlarged optic disc with PPA surrounding the ONH. There was apparent optic disc tilt; however, optic disc torsion was not a characteristic. RNFL damage occurred both superiorly and inferiorly, with extensive VF damage in eyes with staphyloma involving the optic disc and there was no significant relationship between the direction of disc torsion and the location of VF damage. Recently, our group reported that eyes with both superior and inferior VF damage had characteristics of disc tilt rather than disc torsion in these eyes.25
The present study had some limitations. The subjects of our study were recruited from a referral clinic-based practice and not via a population-based screening. Thus, they may represent a subgroup of Korean individuals who do not reflect the characteristics of individuals in other populations. We gave our effort to include only patients with typical VF defects located at the Bjerrum area. All temporal field loss that is not typical for glaucoma was excluded. The pattern deviation map was used in the analysis of VF rather than total deviation plot since this may in part excluded the generalized depression due to myopia itself or defocus during VF performance. Pathologic myopia with other retinal lesions was carefully examined with the assistance of retinal specialists and patients were excluded. However, it is known that myopic discs result in a variety of stationary field defects other than temporal field loss, and the potential for misclassification must be considered in this situation. A longitudinal study to confirm our findings is needed. Finally, we only could use B-scan ultrasonography to determine posterior protrusion of the eye at this present study. There are several other methods that could image the posterior part of the eye including magnetic resonance imaging. Recently, swept-source optical coherence tomography that could visualize the contour of the posterior part of the eye with a deep scan window is available.22 Further studies using other methods to confirm our findings may be valuable.
In summary, 55.2% of NTG patients with myopia had posterior staphyloma, showing that asymmetric elongation of the globe is present in these patients. Optic disc torsion was a prominent finding in small myopic discs, when the location of the posterior staphyloma was temporal to the optic disc. Also, the location of the posterior staphyloma was related to the direction of disc torsion and the location of the VF defect. This shows that change in the posterior shape of the globe influences the optic disc morphological change and related to the location of RGC damage in myopic eyes with glaucoma.
Acknowledgments
This research was supported by Seoul St. Mary's Hospital Clinical Medicine Research Program year of 2013 through the Catholic University of Korea.
The authors declare no conflict of interest.
References
- Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999;106 (10:2010–2015. doi: 10.1016/s0161-6420(99)90416-5. [DOI] [PubMed] [Google Scholar]
- Xu L, Wang Y, Wang S, Jonas JB. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology. 2007;114 (2:216–220. doi: 10.1016/j.ophtha.2006.06.050. [DOI] [PubMed] [Google Scholar]
- Wong TY, Klein BE, Klein R, Knudtson M, Lee KE. Refractive errors, intraocular pressure, and glaucoma in a white population. Ophthalmology. 2003;110 (1:211–217. doi: 10.1016/s0161-6420(02)01260-5. [DOI] [PubMed] [Google Scholar]
- Samarawickrama C, Mitchell P, Tong L, Gazzard G, Lim L, Wong TY, et al. Myopia-related optic disc and retinal changes in adolescent children from Singapore. Ophthalmology. 2011;118:2050–2057. doi: 10.1016/j.ophtha.2011.02.040. [DOI] [PubMed] [Google Scholar]
- How AC, Tan GS, Chan YH, Wong TT, Seah SK, Foster PJ, et al. Population prevalence of tilted and torted optic discs among an adult Chinese population in Singapore: the Tanjong Pagar Study. Arch Ophthalmol. 2009;127 (7:894–899. doi: 10.1001/archophthalmol.2009.134. [DOI] [PubMed] [Google Scholar]
- Doshi A, Kreidl KO, Lombardi L, Sakamoto DK, Singh K. Nonprogressive glaucomatous cupping and visual field abnormalities in young Chinese males. Ophthalmology. 2007;114 (3:472–479. doi: 10.1016/j.ophtha.2006.07.036. [DOI] [PubMed] [Google Scholar]
- Rada JA, Shelton S, Norton TT. The sclera and myopia. Exp Eye Res. 2006;82 (2:185–200. doi: 10.1016/j.exer.2005.08.009. [DOI] [PubMed] [Google Scholar]
- McBrien NA, Gentle A. Role of the sclera in the development and pathological complications of myopia. Prog Retin Eye Res. 2003;22 (3:307–338. doi: 10.1016/s1350-9462(02)00063-0. [DOI] [PubMed] [Google Scholar]
- Kim TW, Kim M, Weinreb RN, Woo SJ, Park KH, Hwang JM. Optic disc change with incipient myopia of childhood. Ophthalmology. 2012;119 (1:21–26 e21-23. doi: 10.1016/j.ophtha.2011.07.051. [DOI] [PubMed] [Google Scholar]
- Ohno-Matsui K, Shimada N, Yasuzumi K, Hayashi K, Yoshida T, Kojima A, et al. Long-term development of significant visual field defects in highly myopic eyes. Am J Ophthalmol. 2011;152 (2:256–265 e251. doi: 10.1016/j.ajo.2011.01.052. [DOI] [PubMed] [Google Scholar]
- Park HY, Lee K, Park CK. Optic disc torsion direction predicts the location of glaucomatous damage in normal-tension glaucoma patients with myopia. Ophthalmology. 2012;119 (9:1844–1851. doi: 10.1016/j.ophtha.2012.03.006. [DOI] [PubMed] [Google Scholar]
- Hsiang HW, Ohno-Matsui K, Shimada N, Hayashi K, Moriyama M, Yoshida T, et al. Clinical characteristics of posterior staphyloma in eyes with pathologic myopia. Am J Ophthalmol. 2008;146 (1:102–110. doi: 10.1016/j.ajo.2008.03.010. [DOI] [PubMed] [Google Scholar]
- Curtin BJ. Posterior staphyloma development in pathologic myopia. Ann Ophthalmol. 1982;14 (7:655–658. [PubMed] [Google Scholar]
- Pruett RC. Complications associated with posterior staphyloma. Curr Opin Ophthalmol. 1998;9 (3:16–22. doi: 10.1097/00055735-199806000-00004. [DOI] [PubMed] [Google Scholar]
- Steidl SM, Pruett RC. Macular complications associated with posterior staphyloma. Am J Ophthalmol. 1997;123 (2:181–187. doi: 10.1016/s0002-9394(14)71034-7. [DOI] [PubMed] [Google Scholar]
- Giuffre G. Chorioretinal degenerative changes in the tilted disc syndrome. Int Ophthalmol. 1991;15 (1:1–7. doi: 10.1007/BF00150971. [DOI] [PubMed] [Google Scholar]
- Vongphanit J, Mitchell P, Wang JJ. Population prevalence of tilted optic disks and the relationship of this sign to refractive error. Am J Ophthalmol. 2002;133 (5:679–685. doi: 10.1016/s0002-9394(02)01339-9. [DOI] [PubMed] [Google Scholar]
- Tay E, Seah SK, Chan SP, Lim AT, Chew SJ, Foster PJ, et al. Optic disk ovality as an index of tilt and its relationship to myopia and perimetry. Am J Ophthalmol. 2005;139 (2:247–252. doi: 10.1016/j.ajo.2004.08.076. [DOI] [PubMed] [Google Scholar]
- Cheng HM, Singh OS, Kwong KK, Xiong J, Woods BT, Brady TJ. Shape of the myopic eye as seen with high-resolution magnetic resonance imaging. Optom Vis Sci. 1992;69 (9:698–701. doi: 10.1097/00006324-199209000-00005. [DOI] [PubMed] [Google Scholar]
- Atchison DA, Pritchard N, Schmid KL, Scott DH, Jones CE, Pope JM. Shape of the retinal surface in emmetropia and myopia. Invest Ophthalmol Vis Sci. 2005;46 (8:2698–2707. doi: 10.1167/iovs.04-1506. [DOI] [PubMed] [Google Scholar]
- Moriyama M, Ohno-Matsui K, Hayashi K, Shimada N, Yoshida T, Tokoro T, et al. Topographic analyses of shape of eyes with pathologic myopia by high-resolution three-dimensional magnetic resonance imaging. Ophthalmology. 2011;118 (8:1626–1637. doi: 10.1016/j.ophtha.2011.01.018. [DOI] [PubMed] [Google Scholar]
- Ohno-Matsui K, Akiba M, Modegi T, Tomita M, Ishibashi T, Tokoro T, et al. Association between shape of sclera and myopic retinochoroidal lesions in patients with pathologic myopia. Invest Ophthalmol Vis Sci. 2012;53 (10:6046–6061. doi: 10.1167/iovs.12-10161. [DOI] [PubMed] [Google Scholar]
- Fledelius HC, Goldschmidt E. Eye shape and peripheral visual field recording in high myopia at approximately 54 years of age, as based on ultrasonography and Goldmann kinetic perimetry. Acta Ophthalmol. 2010;88 (5:521–526. doi: 10.1111/j.1755-3768.2009.01550.x. [DOI] [PubMed] [Google Scholar]
- Curtin BJ, Karlin DB. Axial length measurements and fundus changes of the myopic eye. I. The posterior fundus. Trans Am Ophthalmol Soc. 1970;68:312–334. [PMC free article] [PubMed] [Google Scholar]
- Choi JA, Park HY, Shin HY, Park CK. Optic disc characteristics in patients with glaucoma and combined superior and inferior retinal nerve fiber layer defects. JAMA Ophthalmol. 2014;132:1068–1075. doi: 10.1001/jamaophthalmol.2014.1056. [DOI] [PubMed] [Google Scholar]