Abstract
Background
The prevalence of angina from 1971 to 1994 was relatively flat for whites and blacks. We ask whether the prevalence and medical history of angina have changed during 1988 to 2012.
Methods and Results
We used the National Health and Nutrition Examination Survey data from 1988 to 2004 and the data from the six 2-year surveys from 2001 to 2012. We calculated trends in both crude and standardized prevalence rates for the Rose questionnaire on angina (symptomatology) and a question asking whether the respondent had ever been told by a medical professional that they had angina (medical history). In 2009 to 2012, there were on average 3.4 million (95% confidence interval, 2.8–4.0 million) people aged ≥40 years in the United States each year with angina (Rose questionnaire) and 4.5 million (95% confidence interval, 3.5–5.1 million) people with a medical history of angina. The burden of angina varied across age, race, and sex categories, and the pattern of variation differed by whether symptomatology or medical history was assessed. Statistically significant declines in the rates for both outcomes were noted, for the most part, in people aged ≥65 years. Age and sex standardized rates declined significantly for whites but not for blacks.
Conclusions
Rates of angina symptoms and medical history of angina have declined among non-Hispanic whites and among adults aged ≥65 years. Blacks have not experienced these same declines. Clearly, additional study is required to understand these declines and to track the future cost and burden of angina in the US population.
Keywords: epidemiology, medical history, prevalence, trends
Recent data that formally test the presence of secular changes in the prevalence of angina are lacking for the United States. Most epidemiological surveillance of angina has focused on hospitalization, emergency room, and outpatient visit data. Visit rates have declined in all 3 of these settings1–5 Based on observing increasing rates of hospitalization for coronary atherosclerosis and increased use of coronary angiography from 1992 to 1999, ≥1 researcher has suggested that declines in angina hospitalization rates reflect trends in more aggressive diagnosis of coronary atherosclerosis, which has led to angina being replaced with a different discharge diagnosis.1
It is not clear whether the prevalence of angina (as distinguished from the visit rates for angina) has also been declining, which might help explain the drop in inpatient and outpatient visit rates found in recent studies. However, because the most recent study that formally tested for secular trends in angina prevalence was published >10 years ago,6 it sheds little light on this relatively recent phenomenon. In fact, the prevalence of angina from 1971 to 1994 was relatively flat for whites and blacks, and the rate for Mexican Americans actually increased from 1982 to1994.6
The purpose of this study is to describe the population of people who self-reported angina using the Rose questionnaire and who self-reported a medical history of angina, to provide up-to-date findings related to secular trends in rates of these 2 outcomes, and to describe these trends by race.
Methods
Data Source and Definitions
We obtained population-based data from the National Health and Nutrition Examination Surveys (NHANES) that included data from 1988 to 2004 (NHANES III) and the 2-year surveys from 2001 to 2002, 2003 to 2004, 2005 to 2006, 2007 to 2008, 2009 to 2010, and 2011 to 2012.7 We did not include the 1999 to 2000 survey because it was missing key information on angina for our analysis. All surveys were conducted by the National Center for Health Statistics and includes both an interview and an examination component.7 All research activities related to the surveys were reviewed and approved by the National Center for Health Statistics Research Ethics Review Board in accordance with 45 Code of Federal Regulations 46. NHANES are stratified probability-designed surveys. NHANES are complex, multistage stratified clustered sample surveys of the civilian, noninstitutionalized population for the purpose of assessing the health and nutrition status of the population aged ≥2 months. NHANES have 4 stages of sampling. At the first stage of sampling, primary sampling units are selected that consist of counties or groups of counties. At the second stage, segments (blocks or groups of blocks) are selected within primary sampling units. The third stage consists of households within segments, and the final stage involves selecting ≥1 participants within each household.
Based on data from NHANES III and the 5 surveys that were administered from 2001 through 2010, response rates ranged from 78% to 84% for the interview and 73% to 80% for the examination. A surveyed individual can be considered a nonrespondent to either the NHANES interview or the NHANES examination. A person is considered a nonrespondent to the interview if he/she was selected to be in the sample but did not agree to be interviewed. An individual who completes the interview but not the examination is considered a nonrespondent to the examination. Responders tend to be younger than nonresponders and vary in other ways. However, we used the weighted data that adjust for survey nonresponse. By using the weighted data, we are using analytic tools to ensure that our results represent the total sampled population (ie, the civilian noninstitutionalized US population).
The presence of angina was defined using 2 methods. First, we considered anyone answering yes to the question “Has a doctor or other health professional ever told {you/SP} that {you/s/he}…had angina, also called angina pectoris?” to be a person with a medical history of an angina diagnosis. Those who said no were considered to not have a medical history of a diagnosis of angina. Respondents who refused or did not answer the question or said they did not know (<1% overall, with a range from 0.22% to 0.47% depending on the time period) were eliminated from the calculation of angina prevalence rates. This question was part of the Medical Conditions Questionnaire that was administered to all sampled people or their proxy respondent in NHANES III and all later surveys. The question measures the lifetime medical history of angina and does not measure only recent history (eg, the previous year or the past 5 years). Second, we used the Rose questionnaire8,9 to determine which respondents have angina symptomatology, whether diagnosed or not. These questions were part of the Cardiovascular Disease Questionnaire that was administered to people aged ≥40 years in NHANES III and in all subsequent surveys, except for the 1999 to 2000 survey. The questions that were used and the scoring of the answers to the questions are presented in Appendix A in the Data Supplement. If a person failed to answer one of the questions (<1% overall, with a range from 0.14% to 0.34% depending on the time period), he/she was eliminated from the analysis. Because both methods are based on self-report and neither can be considered a gold standard, we treated them as independent estimates and did not combine them when calculating the prevalence of angina. Appendix B in the Data Supplement provides a cross-tabulation of the 2 measures and the resulting Cohen’s κ statistic of 0.15 that supports our decision to analyze the measures separately. To allow comparisons, we calculated prevalence rates using only the population aged ≥40 years because the Rose questionnaire was only administered to people in that age group.
In describing the characteristics of people with angina, we used 3 categories for race/ethnicity: non-Hispanic white, non-Hispanic black, and other. Hispanics were included in the other category and could not be studied separately because of insufficient numbers leading to large SEs around the point estimates.
Statistical Analysis
Characteristics of Those With Angina, Angina Prevalence Rates, and Time Trends
We estimated the total weighted number of people aged ≥40 years with angina (using the 2 methods described above) in the United States by multiplying the crude prevalence of angina for people aged ≥40 years within each time period by population survey estimates for those aged ≥40 years in the United States.10 We calculated the prevalence over time; however, because angina is relatively rare (<5% of the population), we need to combine surveys to obtain reliable estimates. We used NHANES III (1988–1994) as is, but then combined 2 continuous surveys in the later years to obtain 3 additional time periods: 2001 to 2004, 2005 to 2008, and 2009 to 2012.
We first examined the demographic characteristics among people with angina defined by the 2 methods. We stratified the population with angina by age (40–64 years and ≥65 years), sex, and race/ethnicity (as defined above) and then calculated the percentage of people in each stratum for each of the time periods. We used only 2 age strata because using more resulted in large SEs around the percentages. Second, we calculated the crude percentages of the US population with angina (again, using both methods for defining angina) by the same categories described above. Finally, we calculated the age- and sex-standardized percentages of people with angina in the United States—we did this for the total US population aged ≥40 years and within racial categories using the 2000 US Census population11 as the standard. We calculated the standardized percentages across time so that we could assess whether there was a secular trend in the percentages.
Because of the complex sampling design, we used Survey Data Analysis12 to calculate 95% confidence intervals (CIs) around the estimates. We tested differences between subgroups using t tests, with α=0.05 as a measure of statistical significance; however, this testing was only performed for estimates that were considered reliable according to National Center for Health Statistics standards (ie, estimates based on ≥30 visits and those where the relative SE is ≤30%). We used the ANOVA-type Cochran–Mantel–Haenszel test in Survey Data Analysis to test for trend in each study subgroup.12
Results
Population Distribution of Angina
Symptomatology From the Rose Questionnaire
In 1988 to 1994, an average of 4 million (95% CI, 3.6–4.6 million) people aged ≥40 years in the United States reported symptoms of angina each year (Figure 1). Recent estimates from 2009 to 2012 indicate that the number of people reporting such symptoms in this same age category is 3.4 million (95% CI, 2.8–4.0 million) people each year.
Figure 1.
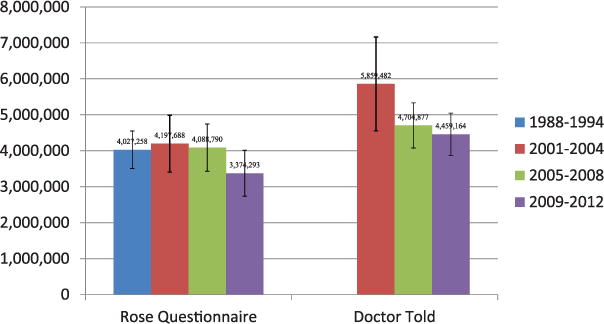
Total population of people aged ≥40 years with angina symptoms or with a medical history of angina.
In every time period, angina symptoms were more often reported by people aged 40 to 64 years (from 60% to 72%) than by people aged ≥65 years (Table 1). Women were more likely than men to report angina symptoms (≈60% and 40%, respectively). Approximately 80% of people with symptoms were white. However, by 2009 to 2012, this had dropped significantly to 59%.
Table 1.
Demographic Characteristics of People Aged ≥40 Years With Angina Symptomatology (Rose Questionnaire) by Time Period: NHANES, 1988 to 2012
| NHANES III
|
2001–2004
|
2005–2008
|
2009–2012
|
|||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) |
| Age, y | ||||||||
| 40–64 | 275 | 60.1 (54.2–65.7) | 134 | 65.4 (56.1–73.6) | 159 | 65.8 (60.5–70.7) | 163 | 71.7 (64.9–77.6) |
| 65+ | 297 | 39.9 (34.3–45.8) | 125 | 34.6 (26.4–43.9) | 108 | 34.2 (29.3–39.5) | 91 | 28.3 (22.4–35.1) |
| Total | 572 | 100.00 | 259 | 100.00 | 267 | 100.00 | 254 | 100.00 |
| Sex | ||||||||
| Women | 339 | 61.2 (53.7–68.1) | 146 | 58.9 (50.7–66.7) | 164 | 63.8 (56.3–70.7) | 141 | 60.7 (51.1–69.5) |
| Men | 233 | 38.8 (31.9–46.3) | 113 | 41.1 (33.3–49.3) | 103 | 36.2 (29.3–43.7) | 113 | 39.3 (30.5–48.9) |
| Total | 572 | 100.00 | 259 | 100.00 | 267 | 100.00 | 254 | 100.00 |
| Race | ||||||||
| Non-Hispanic | 294 | 79.2 (74.3–83.3) | 156 | 75.1 (67.0–81.8) | 134 | 70.3 (62.4–77.2) | 96 | 58.8 (47.8–68.9) |
| white | ||||||||
| Non-Hispanic | 142 | 11.4 (9.1–14.1) | 58 | 15.4 (11.2–20.8) | 75 | 16.1 (12.1–21.1) | 78 | 19.0 (13.7–25.6) |
| black | ||||||||
| Other | 136 | 9.4 (6.7–13.1) | 45 | 9.5 (5.5–16.1) | 58 | 13.6 (9.0–20.2) | 80 | 22.3 (14.3–33.0) |
| Total | 572 | 100.00 | 259 | 100.00 | 267 | 100.00 | 254 | 100.00 |
CI indicates confidence interval; and NHANES, National Health and Nutrition Examination Survey.
Medical History of Angina
In 2001 to 2004, an average of 5.9 million (95% CI, 5.0–7.2 million) people aged ≥40 years in the United States reported a medical history of angina each year (Figure 1). More recent estimates from 2009 to 2012 indicate that the number of people aged ≥40 years reporting such a history is 4.5 million (95% CI, 3.5–5.1 million) each year.
A medical history of angina was reported more frequently by people aged ≥65 years; however, this difference between those aged 40 to 64 years and those aged ≥65 years was only significant in 2005 to 2008 (Table 2). Women and men were equally likely to have such a medical history. As expected, given the distribution of race in the US population, whites make up the vast majority of people with a medical history of angina (80%–85% depending on time period).
Table 2.
Demographic Characteristics of People Aged ≥40 Years With a Medical History of Angina (Doctor Told They Had Angina), Weighted Number of People With Angina, Percentage, and 95% CIs by Time Period: NHANES, 1988 to 2012
| NHANES-III
|
2001–2004
|
2005–2008
|
2009–2012
|
|||||
|---|---|---|---|---|---|---|---|---|
| Characteristics | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) |
| Age, y | ||||||||
| 40–64 | … | … | 117 | 44.0 (36.7–51.6) | 123 | 41.2 (34.9–47.9) | 104 | 44.8 (35.4–54.5) |
| 65+ | … | … | 285 | 56.0 (48.4–63.3) | 187 | 58.8 (52.1–65.1) | 172 | 55.2 (45.5–64.6) |
| Total | … | … | 402 | 100.00 | 310 | 100.00 | 276 | 100.00 |
| Sex | ||||||||
| Women | … | … | 196 | 49.6 (43.2–56.1) | 144 | 47.9 (40.9–55.0) | 126 | 48.1 (40.2–56.1) |
| Men | … | … | 206 | 50.4 (44.0–56.8) | 166 | 52.1 (45.0–59.1) | 150 | 51.9 (43.9–59.8) |
| Total | … | … | 402 | 100.00 | 310 | 100.00 | 276 | 100.00 |
| Race | ||||||||
| Non-Hispanic white | … | … | 289 | 84.6 (79.4–88.7) | 198 | 79.7 (72.2–85.7) | 155 | 79.5 (71.9–85.5) |
| Non-Hispanic black | … | … | 35 | 4.8 (3.2–7.2) | 45 | 8.0 (5.3–11.8) | 48 | 8.5 (5.6–12.7) |
| Other | … | … | 78 | 10.6 (6.8–16.1) | 67 | 12.2 (8.0–18.3) | 73 | 12 (8.1–17.4) |
| Total | … | … | 402 | 100.00 | 310 | 100.00 | 276 | 100.00 |
CI indicates confidence interval; and NHANES, National Health and Nutrition Examination Survey.
Age- and Sex-Stratified Prevalences
Symptomatology From the Rose Questionnaire
Crude prevalence rates for those aged 40 to 64 years ranged from 2% to 3% for men and 3% to 4% for women (Table 3). Neither men nor women in this age category showed statistically significant declines in angina symptomatology over time. Prevalence rates for those aged ≥65 years ranged from 3% to 5% for men and 2% to 6% for women. However, among people in this age category, the decline in rates was significant from the first time period (1988–1994) to the most recent time period (2009–2012) for both men and women. The absolute rate for women aged ≥65 years dropped in half during the study period.
Table 3.
Age- and Sex-Stratified Percentage of People With Angina Symptoms or a Medical History of Angina and 95% Confidence Intervals Among Those Aged ≥40 Years by Time Period: NHANES, 1988 to 2012 (United States)
| NHANES III | 2001–2004 | 2005–2008 | 2009–2012 | |
|---|---|---|---|---|
| Angina symptoms (Rose questionnaire) | ||||
| 40–64 y | ||||
| Men | 2.9 (2.1–4.1) | 2.6 (1.7–3.8) | 2.2 (1.6–2.9) | 1.9 (1.3–2.7) |
| Women | 4.4 (3.5–5.6) | 3.5 (2.7–4.6) | 3.6 (2.8–4.5) | 3.2 (2.4–4.1) |
| ≥65 y | ||||
| Men | 5.1 (4.1–6.2) | 4.1 (2.9–5.9) | 3.3 (2.2–4.9) | 2.9 (2.1–4.0)* |
| Women | 5.6 (4.7–6.6) | 4.6 (3.4–6.2) | 4.6 (3.6–5.8) | 2.4 (1.7–3.2)* |
| Medical history (doctor told them they had angina) | ||||
| 40–64 y | ||||
| Men | … | 3.3 (2.3–4.8) | 2.1 (1.5–2.8) | 2.0 (1.3–3.2) |
| Women | … | 2.6 (1.7–3.8) | 2.0 (1.4–2.8) | 2.0 (1.4–2.8) |
| ≥65 y | ||||
| Men | … | 11.0 (9.5–12.8) | 9.7 (7.2–13.0) | 7.8 (5.8–10.4) |
| Women | … | 9.4 (7.4–11.8) | 6.3. (4.7–8.3) | 5.1 (4.2–6.4)* |
NHANES indicates National Health and Nutrition Examination Survey.
Rates dropped significantly (P<0.05) from the first time period to the last time period.
Medical History of Angina
Crude prevalence rates of a medical history of angina for those aged 40 to 64 years ranged from 2% to 3% for men and women (Table 3). Neither men nor women in this age category showed statistically significant declines in having been told by a doctor that they have angina during the study period. Prevalence rates for those aged ≥65 years ranged from 8% to 11% for men and 5% to 9% for women. However, among people in this age category, the decline in rates was significant from 2001 to 2004 through 2009 to 2012 only for women. The rate for women declined from 9.4% in 2001 to 2004 to 5.1% in 2009 to 2012.
Secular Trends
Symptomatology From the Rose Questionnaire
For non-Hispanic whites, a test of linear trend showed that age- and sex-standardized rates for angina symptomatology (Table 4; Figure 2) declined in a statistically significant linear fashion (P<0.0001) from the first (1988–1994) to the final (2009–2012) period. During those years, the actual rate declined by ≈50%, from 4.0% to 2.1%. The rates for non-Hispanic blacks remained relatively flat during the same time period (Table 4; Figure 2).
Table 4.
Age- and Sex-Standardized Rates of Angina and 95% Confidence Intervals Among Adults Aged ≥40 Years by Time Period: NHANES, 1988 to 2012 (United States)
| Angina | NHANES III | 2001–2004 | 2005–2008 | 2009–2012 |
|---|---|---|---|---|
| Angina symptoms (Rose questionnaire) | ||||
| Non-Hispanic White | 4.0 (3.5–4.7) | 3.3 (2.7–4.1) | 3.0 (2.4–3.6) | 2.1 (1.6–2.7)* |
| Non-Hispanic Black | 4.9 (4.1–5.9) | 5.0 (3.7–6.9) | 5.0 (4.1–6.0) | 4.4 (3.6–5.4) |
| Medical history (doctor told them they had angina) | ||||
| Non-Hispanic White | … | 5.2 (4.4–6.3) | 3.7 (3.0–4.5) | 3.4 (2.7–4.2)† |
| Non-Hispanic Black | … | 2.6 (1.9–3.4) | 2.8 (2.1–3.8) | 2.7 (1.9–3.8) |
NHANES indicates National Health and Nutrition Examination Survey.
Percentages declined in a statistically significant linear fashion over time (P<0.0001).
Percentages declined in a statistically significant linear fashion over time (P<0.01).
Figure 2.
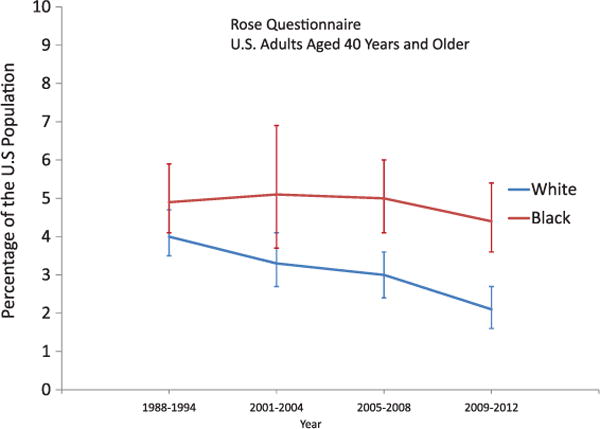
Secular trends in age- and sex-standardized prevalence rates of angina for adults aged ≥40 years in the United States, by race, for angina symptoms defined using the Rose questionnaire. Source: National Health and Nutrition Examination Surveys, 1988 to 2012. Note: The linear decline for whites is statistically significant at P<0.0001, and the vertical lines indicate 95% confidence intervals for each point estimate.
Medical History of Angina
For non-Hispanic whites, a test of linear trend showed that age- and sex-standardized rates for a medical history of angina (Table 4; Figure 3) declined in a statistically significant linear fashion (P<0.001) from 2001 to 2004 through 2009 to 2012. During those years, the actual rate declined by about one third, from 5.2% to 3.4%. The rates for non-Hispanic blacks remained relatively flat during the same time period (Table 4; Figure 2).
Figure 3.
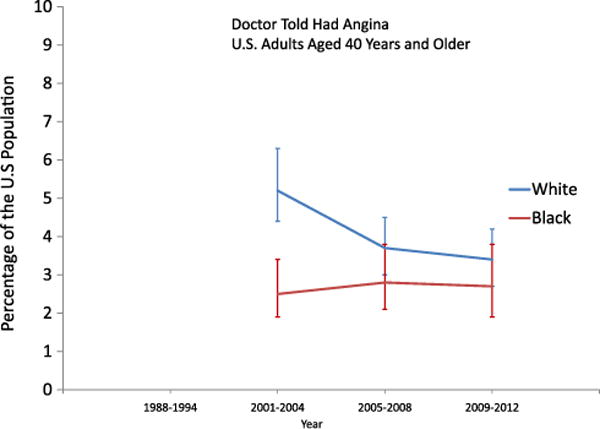
Secular trends in age- and sex-standardized prevalence of a medical history of angina for adults aged ≥40 years in the United States, by race, for angina defined according to whether a doctor had ever told the respondent that they had angina. Source: National Health and Nutrition Examination Surveys, 1988 to 2012. Note: The declining linear trend for whites is statistically significant at P<0.01, and the vertical lines indicate 95% confidence intervals for the point estimates.
Discussion
Our results address an important gap in the epidemiology of cardiovascular disease by showing that the prevalence of angina symptoms among US adults aged 40 to 64 years has declined significantly among non-Hispanic whites and most adults aged ≥65 years during the past 2 decades. Unfortunately, the prevalence of such symptoms has stayed relatively flat for non-Hispanic blacks during this same time period. This same racial disparity is observed for medical history of angina: rates for whites declined during the past decade but rates for blacks remained flat.
The results of the present study are consistent with data showing a decline in the rates of hospitalizations and emergency department visits for angina from 1995 to 2010.4 In that study, rates of emergency department visits for angina declined significantly among patients aged ≥65 years, a finding that is consistent with the present study.
A decline in the prevalence of angina for non-Hispanic whites could be the result of a declining incidence of angina, increased mortality among patients with angina, a changing healthcare system that is less likely to diagnose angina and report to patients that they have angina, or a combination of these factors. There are no national data about trends in incident angina, and therefore other data may offer some insights. Trends in cardiovascular risk factors present a mixed picture. The prevalence of smoking and mean concentration of total cholesterol have declined.13–15 Furthermore, the prevalence of meeting 2008 physical activity recommendations has increased from 1998 to 2010.16 The prevalence of hypertension increased from 1988 to 1994 through 1999 to 2000 but has since remained stable.17,18 In addition, control of hyperlipidemia and hypertension has also improved.19 In contrast, the prevalence of obesity and diabetes mellitus has increased substantially.20–23 Despite this, predicted 10-year cardiovascular risk has declined since 1988 to 1994.24,25 Furthermore, regional studies have shown that incident coronary heart disease has declined.26–30 Although the trends of risk factors present inconclusive supportive evidence, the studies concerning incident coronary heart disease suggest the possibility that incident angina may have declined.
Little is known about mortality rates among people with angina pectoris. Mortality rates from coronary heart disease in the United States have declined precipitously since the late 1960s.31 Thus, mortality among adults with angina pectoris could have conceivably declined as well, which would lead to more people living longer with angina. Such a scenario would run counter to our observation of a lowering prevalence of angina for whites. However, it could possibly explain why rates are not declining for blacks.
Another possible explanation for the relatively flat rates for blacks is that risk factors are not declining as much for blacks as for whites. This is supported by the results of a recent analysis of trends of 10-year predicted cardiovascular disease risk showing that risk has declined significantly for non-Hispanic whites but not for non-Hispanic Blacks.25 The more favorable trends in risk factor evolution among non-Hispanic whites than non-Hispanic Blacks—principally, systolic blood pressure, total cholesterol, and diabetes mellitus—likely influenced the divergent trajectories of prevalent angina.25 To jump start a decline in angina prevalence among non-Hispanic Blacks, underlying health disparities in cardiovascular risk factors will need to be addressed.
Despite a growing population, the number of adults with angina has not increased, which indicates that the prevalence of angina has not kept up with the growth in the US population. These numbers have implications for the healthcare sector and suggest that fewer resources may be needed to treat angina in the future.
The results of this study are subject to several limitations. First, both angina symptomatology and medical history definitions were based on self-reported information and, consequently, are subject to error. In fact, a recent study showed that being black, having lower education, being women, and not having had a healthcare visit in the past year are associated with undiagnosed angina (ie, having symptoms but not having been told by a doctor that you have angina).32 The authors of the study suggest that these findings point to problems with awareness of disease and health communication issues for these subgroups of the population. Consequently, rates of medical history of angina may be underestimated for these groups. However, the validity and reliability of the Rose questionnaire have been evaluated and are generally thought to be reasonable.9 The questionnaire has been used widely in cardiovascular epidemiological studies, including in many countries, in various subpopulations and races, and in various educational and occupational groups.32 Second, the numbers of participants with angina were insufficient to allow examination by detailed demographic subgroups. Third, the numbers necessitated the aggregation of survey cycles to improve the stability of the estimates. Finally, the surveys did not include information allowing estimates on incident angina to be calculated.
In conclusion, both the prevalence rates of angina symptoms and the prevalence rates of the medical history of angina have declined among non-Hispanic whites and among adults aged ≥65 years. Disturbingly, however, blacks have not experienced these declines in either outcome. This disparity needs to be addressed, most likely through the delivery of more intensive public health interventions aimed at addressing the cardiovascular needs of black Americans. The present study was unable to provide data to explain the possible reasons for the apparent decline in the prevalence of angina symptoms and medical history, and, therefore, studies that investigate possible contributing factors to these declines are needed. Continued surveillance efforts will be critical to monitoring the future course of the costs and burden of angina in the US population.
Supplementary Material
WHAT IS KNOWN
Hospitalizations, emergency department visits, and outpatient visits for angina have declined substantially since the late 1980s, and previous research suggests that physician behavior in response to changes in coding guidelines may have played an important role in explaining these declines.
Another possible contribution to these decreasing visit rates is that the prevalence of angina may have declined since the late 1980s; however, the most recent analyses of secular trends of angina prevalence were conducted from 1971 to 1994.
WHAT THE STUDY ADDS
This epidemiological research, which spans from 1988 to 2012, shows that the prevalence of self-reported angina symptoms (as measured by the Rose questionnaire) has declined in people aged ≥65 years in the United States.
Declines in the prevalence of both angina symptoms and medical history have declined for whites aged ≥40 years but not for their black counterparts.
Although it is likely that early diagnosis and treatment of risk factors for angina may have played a role in these declines, more research is needed to confirm this, to better understand why racial disparities exist, and to develop appropriate strategies to reduce these disparities.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The Data Supplement is available at http://circoutcomes.ahajournals.org/lookup/suppl/doi:10.1161/CIRCOUTCOMES.113.000779/-/DC1.
Disclosures
None
References
- 1.Saver BG, Dobie SA, Green PK, Wang CY, Baldwin LM. No pain, but no gain? The disappearance of angina hospitalizations, 1992–1999. Med Care. 2009;47:1106–1110. doi: 10.1097/MLR.0b013e31819e1f53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis SK, Liu Y, Gibbons GH. Disparities in trends of hospitalization for potentially preventable chronic conditions among African Americans during the 1990s: implications and benchmarks. Am J Public Health. 2003;93:447–455. doi: 10.2105/ajph.93.3.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bertoni AG, Bonds DE, Thom T, Chen GJ, Goff DC., Jr Acute coronary syndrome national statistics: challenges in definitions. Am Heart J. 2005;149:1055–1061. doi: 10.1016/j.ahj.2004.10.040. [DOI] [PubMed] [Google Scholar]
- 4.Will JC, Valderrama A, Yoon PW. Preventable hospitalizations and emergency room visits for angina. Prev Chronic Dis. 2013;10:E126. doi: 10.5888/pcd10.120322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Will JC, Loustalot F, Hong Y. National trends in visits to physician offices and outpatient clinics for angina 1995 to 2010. Circ Cardiovasc Qual Outcomes. 2014;7:110–117. doi: 10.1161/CIRCOUTCOMES.113.000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ford ES, Giles WH. Changes in prevalence of nonfatal coronary heart disease in the United States from 1971–1994. Ethn Dis. 2003;13:85–93. [PubMed] [Google Scholar]
- 7.National Health and Nutrition Examination Survey questionnaires, datasets, and related documents. US Department of Health and Human Services, Centers for Disease Control and Prevention; 2013. http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. Accessed September 17, 2013. [Google Scholar]
- 8.Rose GA. ischemic heart disease. Chest pain questionnaire. Milbank Mem Fund Q. 1965;43:32–39. [PubMed] [Google Scholar]
- 9.Sorlie PD, Cooper L, Schreiner PJ, Rosamond W, Szklo M. Repeatability and validity of the Rose questionnaire for angina pectoris in the Atherosclerosis Risk in Communities Study. J Clin Epidemiol. 1996;49:719–725. doi: 10.1016/0895-4356(96)00022-4. [DOI] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. NHANES response rates and CPS totals. http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. Accessed October 29, 2013.
- 11.Census 2000 Brief Series. Washington, DC: US Census Bureau; 2000. http://www.census.gov/population/www/cen2000/briefs.html. Accessed October 29, 2013. [Google Scholar]
- 12.SUDAAN (release 10.0) Language Manual. Research Triangle Park (NC): Research Triangle Institute; 2008. http://www.rti.org/sudaan. Accessed October 29, 2013. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Trends in current cigarette smoking among high school students and adults, United States. 1965–2010 http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/index.htm. October 29, 2013.
- 14.Carroll MD, Lacher DA, Sorlie PD, Cleeman JI, Gordon DJ, Wolz M, Grundy SM, Johnson CL. Trends in serum lipids and lipoproteins of adults, 1960–2002. JAMA. 2005;294:1773–1781. doi: 10.1001/jama.294.14.1773. [DOI] [PubMed] [Google Scholar]
- 15.Carroll MD, Kit BK, Lacher DA, Shero ST, Mussolino ME. Trends in lipids and lipoproteins in US adults, 1988–2010. JAMA. 2012;308:1545–1554. doi: 10.1001/jama.2012.13260. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2011: With Special Feature on Socioeconomic Status and Health. Hyattsville, MD: US Deptartment of Health and Human Services; 2012. [PubMed] [Google Scholar]
- 17.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 18.Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol. 2012;60:599–606. doi: 10.1016/j.jacc.2012.04.026. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Vital signs: prevalence, treatment, and control of hypertension—United States, 1999–2002 and 2005–2008. Morb Mortal Wkly Rep. 2011;60:103–108. [PubMed] [Google Scholar]
- 20.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 21.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 23.Cowie CC, Rust KF, Ford ES, Eberhardt MS, Byrd-Holt DD, Li C, Williams DE, Gregg EW, Bainbridge KE, Saydah SH, Geiss LS. Full accounting of diabetes and pre-diabetes in the U.S. population in 1988–1994 and 2005–2006. Diabetes Care. 2009;32:287–294. doi: 10.2337/dc08-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lopez-Jimenez F, Batsis JA, Roger VL, Brekke L, Ting HH, Somers VK. Trends in 10-year predicted risk of cardiovascular disease in the United States, 1976 to 2004. Circ Cardiovasc Qual Outcomes. 2009;2:443–450. doi: 10.1161/CIRCOUTCOMES.108.847202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ford ES. Trends in predicted 10-year risk of coronary heart disease and cardiovascular disease among U.S. adults from 1999 to 2010. J Am Coll Cardiol. 2013;61:2249–2252. doi: 10.1016/j.jacc.2013.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Floyd KC, Yarzebski J, Spencer FA, Lessard D, Dalen JE, Alpert JS, Gore JM, Goldberg RJ. A 30-year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parikh NI, Gona P, Larson MG, Fox CS, Benjamin EJ, Murabito JM, O’Donnell CJ, Vasan RS, Levy D. Long-term trends in myocardial infarction incidence and case fatality in the National Heart, Lung, and Blood Institute’s Framingham Heart study. Circulation. 2009;119:1203–1210. doi: 10.1161/CIRCULATIONAHA.108.825364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 29.Roger VL, Weston SA, Gerber Y, Killian JM, Dunlay SM, Jaffe AS, Bell MR, Kors J, Yawn BP, Jacobsen SJ. Trends in incidence, severity, and outcome of hospitalized myocardial infarction. Circulation. 2010;121:863–869. doi: 10.1161/CIRCULATIONAHA.109.897249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosamond WD, Chambless LE, Heiss G, Mosley TH, Coresh J, Whitsel E, Wagenknecht L, Ni H, Folsom AR. Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987–2008. Circulation. 2012;125:1848–1857. doi: 10.1161/CIRCULATIONAHA.111.047480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2012 Chart Book on Cardiovascular, Lung, and Blood Diseases. Bethesda, MD: National Institutes of Health; 2012. [Google Scholar]
- 32.McKee MM, Winters PC, Fiscella K. Low education as a risk factor for undiagnosed angina. J Am Board Fam Med. 2012;25:416–421. doi: 10.3122/jabfm.2012.04.110282. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


