Abstract
Introduction:
South Asian population has a particularly high prevalence of thyroid disorders mainly due to iodine deficiency and goitrogen use. There is no data available for prevalence of thyroid disorders in the general population living in nonmountainous regions of Pakistan.
Materials and Methods:
A total of 2335 residents of Pak Pattan, Punjab, Pakistan were interviewed about demographic, dietary, medical and environmental history as well as screened for goiter. Individuals of all ages and either gender were included.
Results:
Median age was 34 (10–88) years and 1164 (49.9%) were males. Median monthly income was 49 (3.9–137) USD. Six hundred and sixty-nine (28.7%) subjects had palpable goiter. 77.5% (n = 462) and 22.5% (n = 133) had World Health Organization Grade I and Grade II goiters respectively, further screened by measuring thyroid-stimulating hormone (TSH). In subjects with TSH <0.4 mg/dL, free T3 and free T4 levels were measured. In 185 goiter subjects when TSH was measured, 50% (n = 93) were euthyroid, 48% (n = 89) were hyperthyroid, and one subject each was hypothyroid and subclinically hyperthyroid. 29/89 hyperthyroid subjects underwent radionuclide scanning. Twelve subjects had heterogeneous uptake consistent with multinodular goiter, 12 subjects had diffuse uptake, two had cold nodules and two had hyperfunctioning single nodules. Goiter was significantly more common among females, unmarried individuals and individuals drinking tube well (subterranean) water. Goiter was less common among those who consumed daily milk, daily ghee (hydrogenated oil), spices, chilies, and turmeric.
Discussion:
In our study population, goiter was endemic with very high prevalence of hyperthyroidism. Turmeric use was association with reduced goitrogenesis. Further studies to assess iodine sufficiency, thiocyanate exposure and autoimmunity need to be conducted. Masses consuming high goitrogen diets should be educated to incorporate turmeric, spices and green chilies in their cooking recipes, to reduce the risk of goiter development. In addition, use of iodized salt in their daily diet cannot be overemphasized.
Keywords: Goiter, Pakistan, iodine deficiency, turmeric, goitrogens
INTRODUCTION
Thyroid disorders affect all ages and either gender. South Asian population has a particularly high prevalence of thyroid disorders mainly due to iodine deficiency[1] and goitrogen use. Many time the sole symptoms prompting patient and physicians to screen for thyroid disorder is a visible goiter. In I972, Chapman et al. first described the prevalence of thyroid disorders in the general population in mountainous northern areas of Pakistan.[2] In a series of studies, Elahi et al. documented the prevalence of iodine deficiency, goiter and thyroid disorders in pregnant females in Lahore, Pakistan.[3,4,5] Palpable goiter prevalence as high as 12% and 23% has been reported in India in adults[6] and children,[7] respectively. There is, however, no data available for prevalence of thyroid disorders in the general population living in nonmountainous regions of Pakistan.
There were anecdotal reports of increased frequency of visible goiter in subjects presenting to a free medical camp conducted in Pak Pattan. Some of them were also clinically hyperthyroid. As a pilot study, we decided to screen the population systematically for thyroid disorders.
MATERIALS AND METHODS
Pak Pattan District has a population of 1,563,000.[8] Rajbah, a belt along the Sutlej river in Pak Pattan District, has an estimated population of 500,000 residents. Pak Pattan district is primarily an agricultural land mass with local crops of wheat, rice, sugar cane and vegetables including potatoes, turnip, cauliflower, cabbage, spinach, garlic, and chilies.[9] Rajbah residents belong to lower socioeconomic class, and their diet mostly consists of locally grown seasonal crops with rare milk and animal protein intake.
After obtaining approval from ethics review board of Allama Iqbal Medical College, Lahore, key opinion leaders, and stakeholders were engaged to ensure adequate subject enrolment in the study. We estimated that about 2500–3000 Rajbah residents were suffering from goiter in the target population. Investigators formed two teams of volunteers and conducted presurvey training. Team A visited the residents of Rajbah area door-to-door ahead of time and reinforced attendance of the screening medical camp. Team B obtained consent from the subject or caregivers in case of minors and recorded data on standardized proforma.
In order to screen the affected population, a free screening cross-sectional study was conducted over 2 days in February 2011. The study was conducted at Outpatient Department of a local hospital in downtown Pak Pattan. Individuals of any age and either gender were included, whereas nonresidents or those residing for <1 year in the village were excluded from the study. Two thousand three hundred and thirty five subjects consented and were recruited in the study. Volunteers interviewed, whereas the investigators examined subjects in tandem. Volunteers collected demographic data (age, sex, occupation, monthly income etc.), dietary history (daily milk, daily ghee, use of spices, use of turmeric, use of chilies etc.), medical history (diagnosed thyroid disorders, current or past medication levothyroxine and anti-thyroid drugs intake history), environmental history (water source, tobacco smoking etc.) and physical examination findings (pulse rate, blood pressure, presence or absence of goiter and size of goiter etc.). Investigators examined and graded goiter according to the World Health Organization (WHO) guidelines.[10] Subjects with goiter were photographed for future reference.
A representative subset of individuals with goiter underwent thyroid function tests (TFTs) and Tc99 radionuclide thyroid scanning. Subjects with goiter were offered TFTs. Thyroid-stimulating hormone (TSH) values between 0.4 and 4 mg/dL were considered normal for the purpose of this study. A TSH value of < 0.1, 0.1–0.4 (with normal free T3 and free T4 values), 4–10.99 and >11 mg/dL was classified as overt hyperthyroidism, subclinical hyperthyroidism, subclinical hypothyroidism and overt hypothyroidism respectively. We offered Tc99 radionuclide thyroid scanning to subjects with TSH below 0.4 mg/dL. Volunteers escorted subjects to nuclear medicine institutes in Lahore and Multan for radionuclide thyroid scanning.
Data were analyzed using Statistical Package for the Social Sciences (SPSS) statistics software version 17 (SPSS Inc., Chicago, IL, USA). Continuous variables (age, income and duration of goiter) were presented as median and range. Nominal data (gender, presence of goiter, exposure to dietary and environmental factors) was presented as percentages. Characteristics of the subjects with and without goiter were compared. Fisher's exact test or the Mantel–Haenszel Chi-square statistic was used for categorical variables, and Mann–Whitney test was used for continuous variables. A multivariate binary logistic regression analysis was performed to determine predictors of the presence of goiter.
RESULTS
Median age of the 2335 participants was 34 years (range 10–88 years), and 1164 (49.9%) were males 51.9% participants were illiterate. Median monthly income was 49 (3.9–137) US dollars. 669 (28.7%) subjects presented with goiter [Figure 1]. 20 and 8 subjects with goiter were on carbimazole and levothyroxine, respectively.
Figure 1.
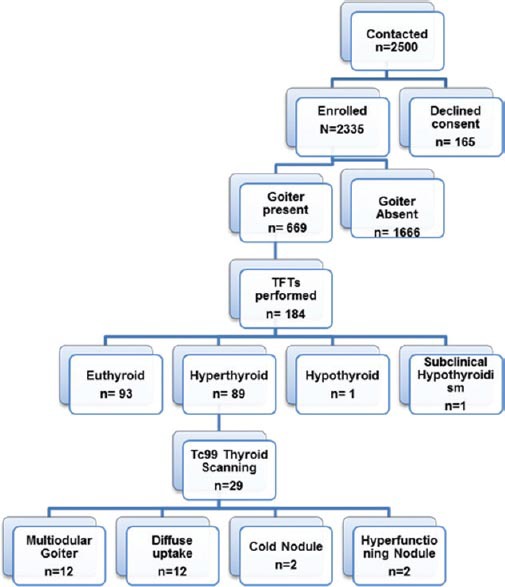
Recruitment and work up algorithm of THYPAK study subjects
77.5% (n = 462) and 22.5% (n = 133) had WHO Grade I and Grade II goiters respectively. Serum TSH was used as a screening test for thyroid status in goiter subjects. In subjects in whom TSH was <0.4 mg/dL, Free T3 and free T4 levels were measured. TSH was measured in 185 goiter subjects of which 50% (n = 93) were euthyroid, 48% (n = 89) were hyperthyroid, and one subject each was hypothyroid and subclinically hyperthyroid.
29/89 hyperthyroid subjects underwent radionuclide scanning. Twelve subjects had multinodular goiter (MNG) with heterogeneous uptake in both lobes. Twelve subjects had diffuse uptake in both lobes of the thyroid gland, two had cold nodules and two had hyperfunctioning single nodules.
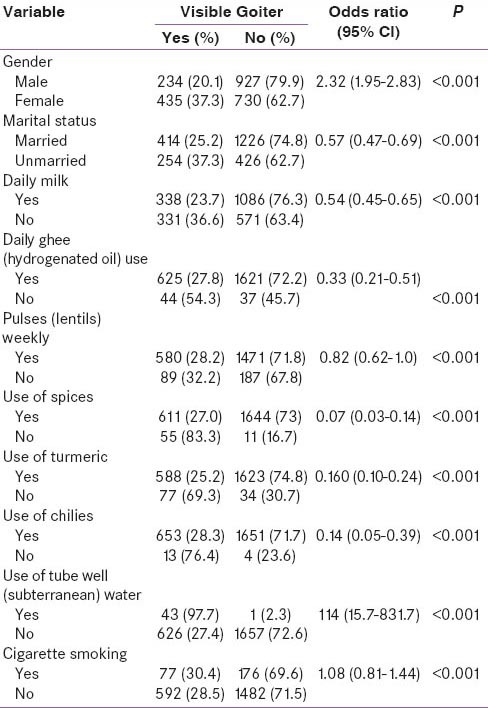
Goiter was significantly more common among females, unmarried individuals and individuals drinking tube well (subterranean) water. Goiter was less common among those who consumed daily milk, daily ghee (hydrogenated oil), spices, chilies and turmeric [Table 1].
Table 1.
Characteristics of study subjects with and without goiter
DISCUSSION
Our study is the first systemically conducted study to assess the prevalence of thyroid disorders in the Plains of Pakistan. People living in the rural areas of Pakistan understandably rely on locally grown vegetables for their daily sustenance. In our population, like other rural areas of Pakistan, the consumption of known goitrogens was very high. Turmeric is one of the commonly used spices in local dishes of Pakistan. Turmeric use is advocated by herbalists for the treatment of a variety of ailments including symptomatic relief of skin cancers,[11] wound healing, gastrointestinal disorders, de-worming, and rheumatic disorders.[12] Our finding of turmeric use association with reduced goitrogenesis was unexpected. This finding supports the local belief that turmeric is useful in goiter treatment. The other factors associated with reduced goiter development included female sex, unmarried, and those who consumed daily milk, ghee, green chilies and spices. Future studies should focus on quantity of turmeric consumed, and prospective follow up study to see effects of turmeric use on the incidence of goiter.
In our study, almost one in every four subjects (28%) had a goiter. This frequency of goiter is higher than both previously reported prevalences in adults and children in India.[6,7] This increased goiter prevalence suggests compounding effect of goitrogen use to underlying iodine deficiency, as observed by Marwaha et al.[7]
In our study, we used presence of goiter as a screening test, a suboptimal indicator of thyroid disorder at best. The number of subjects could have been higher if biochemical testing were also incorporated in the screening process. Despite this shortcoming, nearly one in two subjects (48%) with goiter who underwent TFT were hyperthyroid. Thyroid scanning results showed a near equal split between Graves’ disease and MNG. These results are very alarming, indicating endemicity of thyroid disorders in Pak Pattan, most likely due to a combination of goitrogen use and iodine deficiency. These findings reinforce the need to conduct a nationwide study to assess the prevalence of thyroid disorders in not only other contiguous areas of Punjab but also the rest of the nonmountainous and mountainous areas of Pakistan.
Owing to the limitation of resources, we did not asses iodide sufficiency, thiocyanate exposure and autoimmunity in this study. The underlying assumption is that there is significant iodine deficiency among the subjects screened. However, we need objective data in the populace, including children and pregnant women. It would be interesting to see the urinary iodide thiocyanate excretion and autoimmunity state in subjects in future studies.
Our study findings have important real life implications. Advising people to avoid goitrogen containing food is impractical. However, if we can educate them to incorporate turmeric, spices and green chilies in their cooking recipes, we can reduce the risk of goiter development. In addition, use of iodized salt in their daily diet cannot be overemphasized.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Zimmermann MB. Iodine deficiency. Endocr Rev. 2009;30:376–408. doi: 10.1210/er.2009-0011. [DOI] [PubMed] [Google Scholar]
- 2.Chapman JA, Grant IS, Taylor G, Mahmud K, Mulk SU, Shahid MA. Endemic goitre in the Gilgit Agency, West Pakistan with an appendix on dermatoglyphics and taste-testing. Philos Trans R Soc Lond B Biol Sci. 1972;263:459–90. doi: 10.1098/rstb.1972.0007. [DOI] [PubMed] [Google Scholar]
- 3.Elahi S, Hussain Z. A Longitudinal study of changes in thyroid related hormones among pregnant women residing in an iodine deficient Urban Area. ISRN Endocrinol 2013. 2013 doi: 10.1155/2013/234031. 234031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Elahi S, Nagra SA. Low maternal iodine intake and early pregnancy hypothyroxinemia: Possible repercussions for children. Indian J Endocrinol Metab. 2014;18:526–30. doi: 10.4103/2230-8210.137513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Elahi S, Rizvi NB, Nagra SA. Iodine deficiency in pregnant women of Lahore. J Pak Med Assoc. 2009;59:741–3. [PubMed] [Google Scholar]
- 6.Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Nair V, Kumar H. High prevalence of undetected thyroid disorders in an iodine sufficient adult south Indian population. J Indian Med Assoc. 2009;107:72–7. [PubMed] [Google Scholar]
- 7.Marwaha RK, Tandon N, Gupta N, Karak AK, Verma K, Kochupillai N. Residual goitre in the postiodization phase: Iodine status, thiocyanate exposure and autoimmunity. Clin Endocrinol (Oxf) 2003;59:672–81. doi: 10.1046/j.1365-2265.2003.01895.x. [DOI] [PubMed] [Google Scholar]
- 8.Pakpattan-Economic and Social Indicators. 2009-2010. [Last accessed on 2014 Dec 01]. Available from: http://www.pakpattanpolice.gov.pk/soci.Eco%20Statistics.html .
- 9.Pre-Investment Study, District Pakpattan, G.o.P. Department of Industries and Mineral development, Editor. 2009:7–8. [Google Scholar]
- 10.WHO; 2007. WHO_iodine deficiency disorder screening_2007, in Thyroid size; p. 36. [Google Scholar]
- 11.Kuttan R, Sudheeran PC, Josph CD. Turmeric and curcumin as topical agents in cancer therapy. Tumori. 1987;28(73):29–31. doi: 10.1177/030089168707300105. [DOI] [PubMed] [Google Scholar]
- 12.Krishnaswamy K. Traditional Indian spices and their health significance. Asia Pac J Clin Nutr. 2008;17(Suppl 1):265–8. [PubMed] [Google Scholar]


