Abstract
In the recent years, outbreaks of blood-borne infections have been reported from assisted living facilities, which were traced back to improper blood glucose monitoring practices. Needle-stick injuries have been implicated in many such cases. This directly raises concerns over sharp disposal practices of diabetic patients self-managing their condition in home care settings. With India being home to a huge diabetic population, this issue, if neglected, can cause substantial damage to the health of the population and a marked economic loss. This article discusses the sharp disposal practices prevalent among diabetes patients, the importance of proper sharp disposal, barriers to safe disposal of sharps, and the options available for doing the same. For adopting an environmentally safe wholesome approach, disposal of plastics generated as a result of diabetes self-care at home is important as well. The article also looks at the possible long-term solutions to these issues that are sustainable in an Indian context.
Keywords: Diabetes, disposal, needle, sharps, waste
INTRODUCTION
It is estimated that out of around 3 billion injections administered annually in India, 83% were for curative purpose, and 63% injections were administered in an unsafe manner.[1] Kalra et al. recently came up with recommendations for proper injection techniques, which have come at a time when it was most needed.[2] Proper way of disposing sharps is one of the important, but often neglected component of proper injection techniques.
Recently, lot of importance is being given to diabetes self-care. This involves self-administration of insulin and/or self-monitoring of blood glucose (SMBG). As a part of self-care, various kinds of medical devices and instruments like insulin pens, needles, syringes, lancets, etc., are used by diabetes patients at home. These are either sharps or contain plastic material. Sharps have been defined by World Health Organization as “items that could cause cuts or puncture wounds, including needles, hypodermic needles, scalpel and other blades, knives, infusion sets, saws, broken glass, and nails.”[3] Though proper disposal of both sharps and plastics is important, this article will focus more on sharps, mainly because of the more immediate and devastating consequences it can have on human health.
Incorrect sharp disposal practices among diabetes patients and members of their family lead to needle-stick injuries (NSIs) among rag pickers, domestic waste handlers, and the community. The lancets used for SMBG are often loosely recapped and are vulnerable to be broken/detached when subjected to minimal force. Similarly, not using puncture proof containers for disposed lancets and insulin syringes is equally hazardous. NSIs could lead to epidemics of blood-borne infections such as HIV/AIDS, hepatitis B and hepatitis C. According to the Centre for Disease Control, Atlanta, already outbreaks of hepatitis B have been reported in home and assisted living care settings due to improper blood glucose monitoring practices.[4]
MAGNITUDE OF THE PROBLEM
A multi-country study among diabetics showed that proportion of various kinds of sharps thrown into the household bin varied from 46.9% to 67.6%.[5] Only in <10% of cases, specific containers were used.[5] Other developed countries have also showed improper sharp disposal practices among diabetes patients to be as high as 80–90%.[6,7] A study from Pakistan showed that more than 90% patients discarded them into the household bin.[8]
As per the Indian Council of Medical Research, India Diabetes study published in 2011, 62.4 million people in India were suffering from diabetes.[9] Though India has one of the highest number of diabetes patients in the world, there has been a lack of research on this issue. As far as we know, only one study has been conducted so far in New Delhi, which showed that 84.1% diabetes patients discarded the sharps directly into their household waste bins.[10]
The New Delhi study also reported that 71% patients disposed at least 7 needles/week; 89% patients disposed at least 7 lancets/week.[10] SMBG is becoming a popular method for patients due to its simplicity and low cost. In India, SMBG was found to be practiced by 26.8% and 10.8% of diabetes patients registered at diabetes specialty centers and private clinics, respectively.[11] All these figures suggest that the absolute number of diabetes patients involved in improper sharp disposal practices is bound to be very high in India.
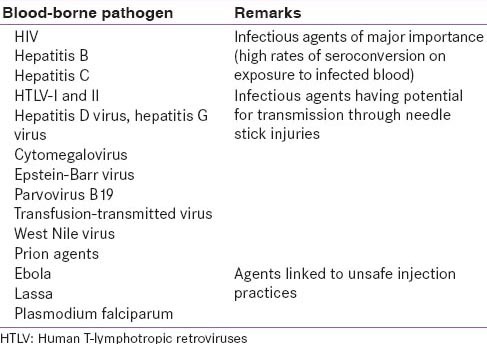
Association of unsafe sharp disposal practices with blood borne infections
The association between diabetes mellitus and hepatitis B virus, hepatitis C virus and HIV has been proved earlier.[12,13,14,15] Diabetes is a lifelong condition that needs long-term care. The strong association between diabetes and these infections implies that a diabetic with any of these, and not following proper sharp disposal practices, via NSIs, will continue to infect others for a significant period of time. A grave problem is that most of these infections have a chronic form, which often remains undetected and thus, is more dangerous for the community. Table 1 enlists common blood-borne infections that can result due to NSIs and unsafe injection practices.[16,17]
Table 1.
Blood-borne infectious agents that can spread as a result of needle-stick injuries and unsafe injection practices
Barriers to safe disposal of sharps by diabetes patients
Some of the barriers identified include lack of information about how and where to dispose, lack of proper advice by doctors and nurses, wrong perception that sharp disposal information is meant only for illegal drug users, and that using community sharp disposal services by patients might result in revelation of their diabetes status.[18] Lack of awareness and wrong perceptions are thus major factors determining sharp disposal practices. Even in developed countries, it was found that diabetes patients did not perceive that “insulin pen needles” and lancets required proper disposal methods.[6] In the New Delhi study, it was found that only 14.1% diabetes patients received education from their healthcare provider regarding proper sharp disposal.[10] Physicians in India either lack time or are unsure of how and what to counsel to patients. Furthermore, diabetes educators are literally nonexistent in India.
Whereas lack of awareness remains a major issue, practically there exist no legislations, national guidelines or local municipality rules regarding disposal of home-generated sharps in India. The Bio-Medical Waste (Management and Handling) Draft rules, 2011 issued by Ministry of Forest and Environment, Government of India, though talk of responsibility regarding disposal of wastes at an approved common biomedical waste treatment facility, are applicable only to occupiers of health care establishments.[19] The National Program for Prevention and Control of Cancer, Diabetes, Cardiovascular disease and Stroke (NPCDCS), the pilot phase of which was launched in January 2008 has also not given any clear recommendations on proper waste disposal.[20]
Some developed countries like the United States of America (USA) have separate laws and rules guiding sharp disposal by residents of each state.[21] Though this kind of policy initiative has had a fair success in ensuring good sharp disposal practices by the residents, ambiguity and lack of uniformity between laws of various states is a problem. For instance, in an assessment of laws, regulations, and guidelines concerned with sharp disposal in 16 states of USA, it was found that several discrepancies existed between the states leading to confusion.[22]
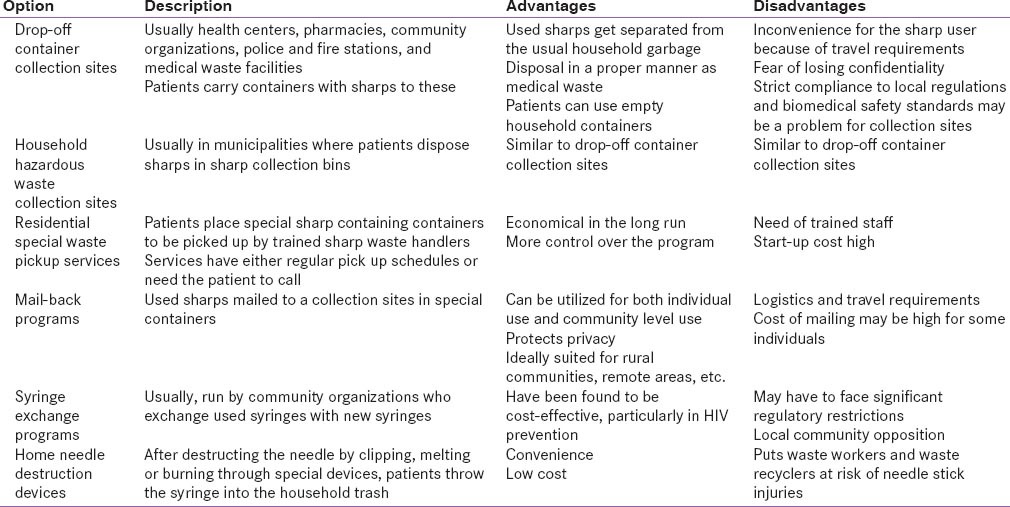
What can be learnt from other countries dealing with home-generated wastes?
Some of the options tried in developed countries with varying success are discussed in Table 2.[23,24,25,26] In some countries, safe sharps website has been created for guidance of patients in finding the location of safe disposal services.[27] Furthermore, smartphone-based applications have been developed to make the services user-friendly.[27]
Table 2.
Various sharp waste disposal options adopted by countries
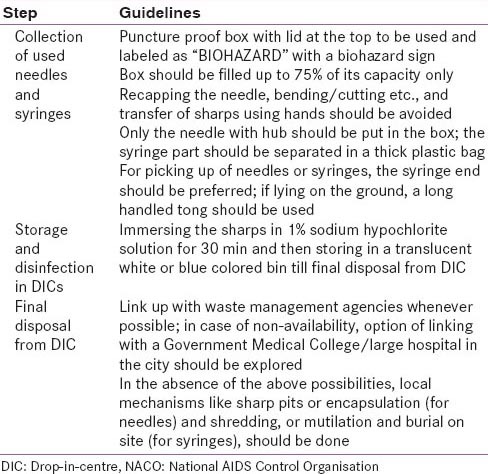
What can be learnt from other national programs running in India?
National AIDS Control Organization (NACO) has issued certain guidelines for disposal of waste needles and syringes as a part of “harm reduction” strategy under targeted intervention (TI) approach for intravenous drug users (IDUs).[28] These guidelines are primarily meant for staff of TIs handling IDUs. Needle syringe exchange programme is the essence of this harm reduction strategy in TI sites, in which used needles and syringes are taken back from IDUs by TI staff after initial distribution. Important guidelines issued by NACO in this regard are highlighted in Table 3.
Table 3.
NACO guidelines for disposal of needles and syringes
Toward “green diabetes care” and “green injection techniques”
While the management of sharps is important, the disposal of the home generated solid plastic wastes resulting from syringes, insulin pens, gloves, blood glucose test strips, catheters, etc., used by diabetes patients cannot be neglected. On one hand, the advent of the single–use disposable medical devices had a great impact on decreasing the transmission of blood-borne infections. On the other hand, it has created the problem of safe disposal of the hundreds of tons of plastics and metals generated in this process. In a study estimating the amount of contents before incineration of six different used products of insulin infusion sets, it was found that amount of plastic content of four products were almost twice the amount of plastics in a typical disposable paper coffee cup.[29] Burning of these plastics leads to the generation of greenhouse gases, further affecting the environment. Thus, there is a need for adopting the environment-friendly wholesome approach to diabetes care at all levels, that is, at the individual, community, and the population level.
Recently, endocrine disrupting chemicals (EDCs) have attracted the attention of many researchers. EDCs are naturally occurring or manmade organic compounds found in hormones, pesticides, plant constituents, compounds used in the plastics industry, consumer products, and various industrial by-products, which, on gaining exposure to human body, interfere with the hormonal system, thus resulting in various endocrine abnormalities.[30] Medical devices and polyvinyl chloride containing medical tubing have been found to contain EDCs.[31] Evidence suggests that EDCs have adverse effects on reproductive health, neuroendocrinology, cardiovascular endocrinology, thyroid function, obesity, diabetes type 2, metabolic diseases, and have roles in breast cancer and prostate cancer.[32,33] More research is needed in this regard to firm up advocacy measures such as the use of EDC-free plastics in insulin pens and syringes, etc.
Need for solutions that fit the Indian scenario best
Spreading awareness among healthcare personnel and diabetes patients
The need for developing local guidelines and educating the community about safe injection use has been realized through research conducted earlier.[34] It is known that patients who receive information regarding safe disposal of sharps are more likely to do the same.[7,8,10] Thus, awareness needs to be spread among general practitioners, physicians dealing with diabetes, diabetes patients, and their family members.
Generating evidence-based guidelines for safe sharps disposal
In the absence of any existing laws, an immediate step could be creation of a dedicated sharp disposal task force under the NPCDCS, consisted of representatives from local Public Health Departments, diabetes researchers, pollution control boards, nongovernmental organizations (NGOs), and pharmaceutical companies involved in diabetes care. This task force can then generate national level estimates of sharp disposal practices by diabetes patients. Furthermore, the same can create guidelines for proper sharp disposal for general public to follow, as well as educate the community on these issues. Guidelines should focus on types of sharps containers that can be used, proper labeling and securing lid of sharps containing containers, any manner of disinfection of sharps, and whether sharps could be disposed off in common household garbage. In this regard, guidance can be taken from the already available guidelines from the NACO.
Finding newer more innovative and cost-effective solutions for source reduction
Development of more sophisticated needle-free insulin injection techniques can significantly lower the generation of sharps. However, the development of such technology has been slow.[35]
Learning from successful waste disposal strategies of other countries
A review of 12 community-based programs for safe disposal of sharps among diabetes patients showed that most of them followed either drop boxes, puncture-proof containers disposed in the trash, and sharps container disposal at designated sites.[36] Whereas India could follow any of the already tested strategies enlisted in Table 2, there is a need to identify cost-effective need-based solutions which are easily implementable as well as sustainable in the Indian context.
Advocacy measures and policy initiatives following a multisectoral approach and involving multiple stakeholders
Intersectoral collaboration is the key to tackle such a complex issue. Government should involve local NGOs, pharmaceutical companies, self-help groups, community volunteers like Accredited Social Health Activists (ASHA) workers, etc., to spread awareness among people regarding the need for safe sharps disposal. ASHA workers could be incentivized for sharp disposal activities under the National Health Mission. Pharmacists are also in an excellent position to educate people. Financial incentives to medical shops could help in motivating them to actively participate. It is important to involve the trash removal companies as a part of public-private partnership. Pharmaceutical companies involved in diabetes care industry could also take up waste disposal activities as a part of their corporate social responsibility. Similarly in villages, Panchayati Raj Institutions can be involved for advocacy measures and to spread awareness regarding sharp disposal. Different strategies may have to be adopted in urban and rural areas owing to the inherent differences in the sociodemographic, economic, and cultural practices.
On the legislation front, stricter and clear laws should be enforced for increasing the accountability of individuals, community, organizations, and the private sector involved in diabetes care. It may be better to have a common law for all states to avoid confusion. While certain companies manufacturing glucometers, lancets, and syringes do mention about sharp disposal on the packets, steps should be taken toward making it mandatory for these companies to explain clearly on the packets the proper method of sharp disposal.
CONCLUSION
Sharp disposal practices among diabetes patients receiving care in home care settings have been found to be unsatisfactory in many countries. Though there is scarcity of literature regarding this issue from India, owing to the huge burden of diabetes, it is imperative that waste workers and the community are at great risk of acquiring blood borne infections via NSIs. Whereas India could adopt strategies already used in other countries, or take guidance from NACO guidelines for sharps disposal, barriers to good sharp disposal practices need to be kept in mind while designing programs. Whereas safe sharps disposal has been a problem, the disposal of plastics (especially those containing EDCs) has come up as an emerging threat. Evidence-based guidelines and legislations in this regard are the need of the hour. Implementation of programs for safe disposal of biomedical waste at home by diabetic patients will not only require a great amount of planning, logistics requirement and advocacy measures, but also significant political commitment as well.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chaturvedi S, Arora NK, Lakshman M, Pandey RM IPEN Study Group. Injection practices in India. South East Asia J Public Health. 2012;1:189–200. doi: 10.4103/2224-3151.206931. [DOI] [PubMed] [Google Scholar]
- 2.Kalra S, Balhara YP, Baruah MP, Chadha M, Chandalaia HB, Chowdhury S, et al. Addendum 2: Forum for injection technique, India. Indian J Endocrinol Metab. 2014;18:800–3. doi: 10.4103/2230-8210.152762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.2nd ed. Geneva: World Health Organisation; 2014. [Last accessed on 2014 Dec14]. Safe management of wastes from health-care. Available from: http://apps.who.int/iris/bitstream/10665/85349/1/9789241548564_eng.pdf?ua=1 . [Google Scholar]
- 4.Atlanta: CDC; [Last accessed on 2014 Dec 20]. Healthcare-Associated Hepatitis B and C Outbreaks Reported to the Centers for Disease Control and Prevention (CDC) in 2008-2013. Available from: http://www.cdc.gov/hepatitis/Outbreaks/PDFs/HealthcareInvestigationTable.pdf . [Google Scholar]
- 5.Bouhanick B, Hadjadj S, Weekers L. What do the needles, syringes, lancets and reagent strips of diabetic patients become in the absence of a common attitude? About 1070 questionnaires in diabetic clinics. Diabetes Metab. 2000;26:288–93. [PubMed] [Google Scholar]
- 6.Costello J, Parikh A. The sticking point: Diabetic sharps disposal practices in the community. J Gen Intern Med. 2013;28:868–9. doi: 10.1007/s11606-013-2350-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Govender D, Ross A. Sharps disposal practices among diabetic patients using insulin. S Afr Med J. 2012;102:163–4. doi: 10.7196/samj.5085. [DOI] [PubMed] [Google Scholar]
- 8.Ishtiaq O, Qadri AM, Mehar S, Gondal GM, Iqbal T, Ali S, et al. Disposal of syringes, needles, and lancets used by diabetic patients in Pakistan. J Infect Public Health. 2012;5:182–8. doi: 10.1016/j.jiph.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 9.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 10.Singh AP, Chapman RS. Knowledge, Attitude and Practices (KAP) on disposal of sharp waste, used for home management of type-2 diabetes mellitus, in New Delhi, India. J Health Res. 2011;25:135–40. [Google Scholar]
- 11.Tharkar S, Devarajan A, Barman H, Mahesh U, Viswanathan V. How far has translation of research been implemented into clinical practice in India? Are the recommended guidelines adhered to? Int J Diabetes Mellit. [Last accessed on 2014 Dec 21]. Available from: http://www.sciencedirect.com/science/article/pii/S1877593411000038 .
- 12.Antonelli A, Ferrari SM, Giuggioli D, Di Domenicantonio A, Ruffilli I, Corrado A, et al. Hepatitis C virus infection and type 1 and type 2 diabetes mellitus. World J Diabetes. 2014;5:586–600. doi: 10.4239/wjd.v5.i5.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Memon MS, Arain ZI, Naz F, Zaki M, Kumar S, Burney AA. Prevalence of type 2 diabetes mellitus in hepatitis C virus infected population: A Southeast Asian study. J Diabetes Res 2013. 2013 doi: 10.1155/2013/539361. 539361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schillie SF, Xing J, Murphy TV, Hu DJ. Prevalence of hepatitis B virus infection among persons with diagnosed diabetes mellitus in the United States, 1999-2010. J Viral Hepat. 2012;19:674–6. doi: 10.1111/j.1365-2893.2012.01616.x. [DOI] [PubMed] [Google Scholar]
- 15.Tien PC, Schneider MF, Cox C, Karim R, Cohen M, Sharma A, et al. Association of HIV infection with incident diabetes mellitus: Impact of using hemoglobin A1C as a criterion for diabetes. J Acquir Immune Defic Syndr. 2012;61:334–40. doi: 10.1097/QAI.0b013e31826bfc32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. [Last accessed on 2014 Dec 17]. Available from: http://www.patient.co.uk/doctor/needlestick-injury .
- 17.Simonsen L, Kane A, Lloyd J, Zaffran M, Kane M. Unsafe injections in the developing world and transmission of bloodborne pathogens: A review. Bull World Health Organ. 1999;77:789–800. [PMC free article] [PubMed] [Google Scholar]
- 18.Community Sharps Management Guidelines for NSW Councils. NSW Department of Health, Sydney. 2004. [Last accessed on 2014 Dec 10]. Available from: http://www0.health.nsw.gov.au/pubs/2004/pdf/sharps.pdf .
- 19.Draft Bio-Medical Waste (Management and Handling) rules, 2011. Ministry of Forest and Environment, Government of India. 2011. [Last accessed on 2014 Nov 28]. Available from: http://www.moef.nic.in/downloads/public-information/salient-features-draft-bmwmh.pdf .
- 20.National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS). Operational Guidelines. Directorate General of Health Services, Ministry of Health and Family welfare, Government of India. p. 61. Available from: http://health.bih.nic.in/Docs/Guidelines/Guidelines-NPCDCS.pdf .
- 21.Atlanta: [Last accessed on 2014 Dec 02]. Safe community needle disposal. Centers for Disease Control and Prevention (CDC) Available from: http://www.cdc.gov/needledisposal/index.htm . [Google Scholar]
- 22.Turnberg WL, Jones TS. Community syringe collection and disposal policies in 16 states. J Am Pharm Assoc (Wash) 2002;42(6 Suppl 2):S99–104. doi: 10.1331/1086-5802.42.0.s99.turnberg. [DOI] [PubMed] [Google Scholar]
- 23.Washington: 2004. [Last accessed on 2014 Dec 03]. Community options for safe needle disposal. United States Environmental Protection Agency. Available from: http://www.epa.gov/wastes/nonhaz/industrial/medical/med-govt.pdf . [Google Scholar]
- 24.Safe community needle disposal. [Last accessed on 2014 Dec 17]. Available from: http://www.cdc.gov/needledisposal/mt/index.htm#standards .
- 25.Atlanta: 2005. [Last accessed on 2014 Dec 19]. Syringe Exchange Programs. Centers for Disease Control and Prevention (CDC) Available from: http://www.cdc.gov/IDU/facts/AED_IDU_SYR.pdf . [Google Scholar]
- 26.Household hazardous waste collection. A program guide for tribal governments. United States Environmental Protection Agency. 2009. [Last accessed on 2014 Dec 14]. Available from: http://www.epa.gov/region9/waste/tribal/pdf/final-hhw-guide-oct-2007.pdf .
- 27. [Last accessed on 2014 Dec 26]. Available from: https://www.safesharps.org.au/
- 28.Guidelines on safe disposal of Used Needles and Syringes in the Context of Targeted Intervention for Injecting Drug Users. National AIDS Control Organisation Department of AIDS Control Ministry of Health and Family Welfare, Government of India. 2009. [Last accessed on 2014 Dec 03]. Available from: http://www.naco.gov.in/upload/NGO%20 and %20Targeted/waste%20disposal%20 guideline%20for%20IDU%20TI.pdf .
- 29.Pfützner A, Musholt PB, Malmgren-Hansen B, Nilsson NH, Forst T. Analysis of the environmental impact of insulin infusion sets based on loss of resources with waste. J Diabetes Sci Technol. 2011;5:843–7. doi: 10.1177/193229681100500403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Global assessment of the state-of-the-science of endocrine disruptors. International Programme on Chemical Safety. World Health Organisation. 2002. [Last accessed on 2014 Dec 25]. Available from: http://www.who.int/ipcs/publications/en/toc.pdf .
- 31.Olujimi OO, Fatoki OS, Odendaal JP, Okonkwo JO. Endocrine disrupting chemicals (phenol and phthalates) in the South African environment: A need for more monitoring. Water SA. 2010;36:671–82. [Google Scholar]
- 32.Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM, et al. Endocrine-disrupting chemicals: An Endocrine Society scientific statement. Endocr Rev. 2009;30:293–342. doi: 10.1210/er.2009-0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chevalier N, Fénichel P. Endocrine disruptors: New players in the pathophysiology of type 2 diabetes? Diabetes Metab. 2014. [Last accessed on 2014 Dec 30]. Available from: http://dx.doi.org/10.1016/j.diabet. 2014.09.005 . [DOI] [PubMed]
- 34.Pandit NB, Choudhary SK. Unsafe injection practices in Gujarat, India. Singapore Med J. 2008;49:936–9. [PubMed] [Google Scholar]
- 35.Needle Free Injecting. [Last accessed on 2014 Dec 21]. Available from: http://www.diabetes.co.uk/insulin/needle-free-injecting.html .
- 36.Macalino GE, Springer KW, Rahman ZS, Vlahov D, Jones TS. Community-based programs for safe disposal of used needles and syringes. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18(Suppl 1):S111–9. doi: 10.1097/00042560-199802001-00019. [DOI] [PubMed] [Google Scholar]


