Abstract
The objective of this study was to conduct a meta-analysis to determine risk factors that may facilitate patient selection for radical resections or additional resections after a polypectomy. Eligible articles were identified by searches of PUBMED, Cochrane Library and Korean Medical Database using the terms (early colorectal carcinoma [ECC], lymph node metastasis [LNM], colectomy, endoscopic resection). Thirteen cohort studies of 7,066 ECC patients who only underwent radical surgery have been analysed. There was a significant risk of LNM when they had submucosal invasion (≥ SM2 or ≥ 1,000 µm) (odds Ratio [OR], 3.00; 95% confidence interval [CI], 1.36-6.62, P = 0.007). Moreover, it has been found that vascular invasion (OR, 2.70; 95% CI, 1.95-3.74; P < 0.001), lymphatic invasion (OR, 6.91; 95% CI, 5.40-8.85; P < 0.001), poorly differentiated carcinomas (OR, 8.27; 95% CI, 4.67-14.66; P < 0.001) and tumor budding (OR, 4.59; 95% CI, 3.44-6.13; P < 0.001) were significantly associated with LNM. Furthermore, another analysis was carried out on eight cohort studies of 310 patients who underwent additional surgeries after an endoscopic resection. The major factors identified in these studies include lymphovascular invasion on polypectomy specimens (OR, 5.47; 95% CI, 2.46-12.17; P < 0.001) and poorly or moderately differentiated carcinomas (OR, 4.07; 95% CI, 1.08-15.33; P = 0.04). For ECC patients with ≥ SM2 or ≥ 1,000 µm submucosal invasion, vascular invasion, lymphatic invasion, poorly differentiated carcinomas or tumor budding, it is deemed that a more extensive resection accompanied by a lymph node dissection is necessary. Even if the lesion is completely removed by an endoscopic resection, an additional surgical resection should be considered in patients with poorly or moderately differentiated carcinomas or lymphovascular invasion.
Graphical Abstract
Keywords: Colorectal Neoplasms, Lymph Nodes, Endoscopy, Colectomy
INTRODUCTION
The incidence of colorectal cancer in Korea has increased dramatically over the past few decades, but fortunately the detection rate of early stage colon cancer has also risen with the advent of screening colonoscopy. Early colorectal cancer (ECC) is defined as carcinoma with invasion limited to the mucosa (Tis) and submucosa (T1), regardless of the presence of lymph node metastasis (LNM) (1).
Like other cancers, early detection is of utmost importance. The 5-yr survival rate for patients who have colorectal cancer treated at Stage I exceeds 74%, whereas the rates fall to 67% and 6% for stage II and IV tumors, respectively.
Advances in colonoscopic instrumentation and techniques have made it possible to resect colorectal neoplasms endoscopically, including mucosal and submucosal invasive cancers. Once the cancer invades the submucosal layer, lymph node metastasis is reported to occur in 3.6% to 16.2% of patients, requiring additional surgery and lymphadenectomy (2, 3, 4, 5).
However, operative treatments are relatively invasive and costly, and the postoperative mortality rate of colon and rectal cancer procedures is approximately 3% to 6% (6, 7). Therefore, over- and under-treatments should be avoided by selecting patients through careful histological analyses of local excision specimens. Despite the importance of accurate discrimination between low and high risk T1 cases, an adequate literature review that could quantify the influences of individual risk factors has been rarely investigated. This study will provide a meta-analysis of the risk factors for the presence of LNM in pT1 colorectal cancer.
MATERIALS AND METHODS
Literature search strategy and criteria for inclusion
A systematic review was conducted using PubMed, Medline and Korean Medical Database, to identify studies published between 1980 and May 2013 in each database. We also investigated reference lists of relevant articles and review articles. Only published studies written in English or Korean were included, and the following keywords were used in various forms and combinations for the search: colorectal carcinoma, lymph node metastasis, lymph nodes, colectomy, surgical resection, and endoscopic resection.
We included studies that evaluate the association between LNM and specific risk factors in patients with ECC who underwent radical surgeries or additional surgeries after an endoscopic resection. The factors include sex, age, tumor location, lymphatic invasion, vascular invasion, lymphovascular invasion, gross types of carcinoma, depths of submucosal invasion, tumor budding, and differentiation. The percentage or number of patients with lymph node involvement was reported separately. To avoid overlapping data that may result from duplications, only the articles with the largest sample size were included. Studies of advanced colorectal carcinomas were excluded.
Data extraction
Data were extracted and analyzed by a single investigator. The following characteristics have been extracted from the selected studies: the first author, publication date, study design, size of the study group, number of patients with nodal involvement, treatments, analyzed risk factors for LNM, reasons for additional surgical resection, definitions of deep submucosal invasion, and histopathologic analysis.
Measuring submucosal invasion depth
The literature described various methods of dividing patients into a low risk group and a high risk group based on the depths of submucosal invasion. For the purpose of this meta-analysis, the patients are divided into two groups: the superficial invasion group (SM1 or <1,000 µm) and intermediate invasion group (SM2 or ≥1,000 µm).
Lymphatic, vascular, and lymphovascular invasion
Most studies considered lymphatic or vascular (sometimes called venous) invasion as separate variables or categorized them collectively under lymphovascular invasion. Definitions, additional staining techniques or immunohistochemical stains were often not provided.
Statistical analysis
If a specific factor was reported in at least three studies and supported by comparable methodologies, a meta-analysis was performed to summarize its prognostic effect in terms of the odds ratios (ORs) for developing LNM. That is, the meta-analysis was limited to a pooled analysis of the ORs for developing LNM, while risk factors, incidences, and events stated in individual studies were entered into Review Manager 5.1 (RevMan, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011). A pooled OR greater than one indicated a worse prognosis in the research group compared to the other group. We used a fixed-effects model and performed a sensitivity analysis of the chosen model. Heterogeneity between the studies is assessed with the I2 statistic. P values less than 0.05 were considered statistically significant and 95% confidence intervals (CI) were reported. Moreover, a funnel plot analysis was conducted to evaluate any publication bias. The data presented as pooled estimates do not take account of the heterogeneity between the studies and are used for exploratory purposes only. The extracted ORs for LNM were pooled by using the generic inverse variance method in Review Manager.
RESULTS
Search results and characteristics of included studies
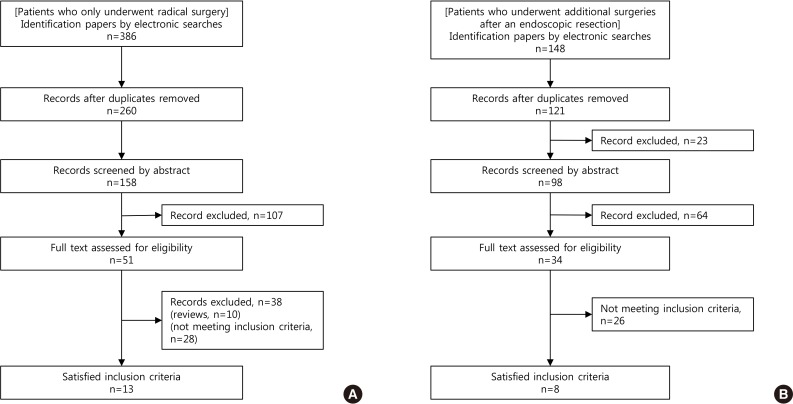
Among 386 and 148 potentially relevant studies, only 13 and 8 studies met the inclusion criteria. The flow chart of the study selection process is shown in Fig. 1. The main characteristics of the studies included in the meta-analysis are summarized in Table 1. The total number of participants was 7,376 (7,066 patients with ECC who underwent radical surgeries only, and 310 patients who underwent additional surgeries after an endoscopic resection).
Fig. 1. Flowchart of patient selection. (A) Patients with radical surgery. (B) Patients with additional surgeries after an endoscopic resection.
Table 1. Basic information for the included trials.
| First author (yr) (Ref. No.) | Country | No. of patients | Type of therapy | Reason for additional surgery | LNM (%) | Analyzed risk factors of LNM |
|---|---|---|---|---|---|---|
| Akishima-Fukasawa Y (2011) (8) | Japan | 111 | Radical surgery | - | 32.4 | Lymphatic invasion |
| Kitajima K (2004) (9) | Japan | 865 | Radical surgery | - | 10.1 | Depth of invasion (SM depth ≥ 1,000 µm), Lymphatic invasion, Tumor budding |
| Nascimbeni R (2002) (10) | United States of America | 353 | Radical surgery | - | 13.0 | Depth of invasion (SM3), Lymphovascular invasion, Location (Lower rectum) |
| Okabe S (2004) (11) | United States of America, Japan | 428 | Radical surgery | - | 10.0 | Depth of invasion (SM depth > 3 mm), Lymphovascular invasion |
| Pan W (2006) (12) | Japan | 166 | Radical surgery | - | 6.6 | Depth of invasion, Lymphovascular invasion |
| Sakuragi M (2003) (13) | Japan | 278 | Radical surgery | - | 7.6 | Depth of invasion (SM depth ≥ 2,000 µm), Lymphatic invasion |
| Shimomura T (2004) (14) | Japan | 171 | Radical surgery | - | 10.5 | Depth of invasion (SM2, SM depth > 1,500 µm), Lymphatic invasion, Tumor budding |
| Sohn DK (2007) (15) | Korea | 48 | Radical surgery | - | 14.6 | Tumor budding |
| Son HJ (2008) (16) | Korea | 3,557 | Radical surgery | - | 17.0 | Depth of invasion (SM2 or SM3), Lymphatic invasion, Sex (Male), Location (Left side), Gross type (Depressed), Differentiation (Moderately or poorly differentiated carcinomas) |
| Suh JH (2012) (17) | Korea | 435 | Radical surgery | - | 13.0 | Lymphovascular invasion, Tumor budding, Differentiation (Undifferentiated carcinomas) |
| Tanaka S (1995) (4) | Japan | 177 | Radical surgery | - | 12.0 | Depth of invasion (SM depth > 400 µm), Lymphatic invasion, Gross type (Depressed), Differentiation (Undifferentiated carcinomas) |
| Tateishi Y (2010) (18) | Japan | 322 | Radical surgery | - | 14.3 | Lymphatic invasion, Differentiation (Undifferentiated carcinomas), Tumor budding |
| Tominaga K (2005) (19) | Japan | 155 | Radical surgery | - | 12.3 | Lymphatic invasion, Dedifferentiation (High-grade focal dedifferentiation) |
| Colacchio TA (1981) (20) | United States of America | 24 | Additional surgeries following polypectomy | Penetration of carcinoma into submucosa | 25.0 | - |
| Kodaira Sa (1981) (21) | Japan | 5 | Additional surgeries following polypectomy | Submucosally invasive carcinomas | 40.0 | - |
| Kodaira Sb (1981) (22) | Japan | 6 | Additional surgeries following polypectomy | Submucosally invasive carcinomas | 33.3 | - |
| Choi DH (2009) (23) | Korea | 38 | Additional surgeries following polypectomy | Poorly or undifferentiated carcinomas, Lymphovascular or venous invasion, Presence of tumor budding | 15.8 | Tumor budding |
| Rossini FP (1988) (24) | Italy | 10 | Additional surgeries following polypectomy | Poorly differentiated carcinomas, Lymphatic or vascular permeation, Resection margin involved with carcinoma | 40.0 | Lymphovascular invasion |
| Sugihara K32 (1989) (25) | Japan | 16 | Additional surgeries following polypectomy | Invasive carcinoma infiltrated within 1,000 µm from the edge, Venous invasion, Carcinoma infiltrating into more than 1/3 of the depth of the submucosa, Poorly differentiated adenocarcinoma | 6.3 | - |
| Butte JM (2012) (26) | United States of America | 143 | Additional surgeries following polypectomy | 6.9 | Young age, Lymphovascular invasion | |
| Kobayashi H (2012) (27) | Japan | 68 | Additional surgeries following polypectomy | Positive margin | 8.2 | Differentiation (Moderately or poorly differentiated carcinomas) |
| Lymphovascular invasion | ||||||
| Submucosally invasion (≥ 1,000 µm) |
LNM, lymph node metastasis; SM, depth, depth of submucosal invasion.
The detection rate of lymph node metastasis ranged from 6.6% to 32.4% in the surgery-only group and from 6.3% to 40.0% in the additional-surgery group. The independent predictors of LNM include sex (male), age (young), tumor location (lower rectum, left side colon), lymphatic and lymphovascular invasion, gross type (depressed type), depth of submucosal invasion (SM2 or ≥1,000 µm), tumor budding, and poor differentiation. The factors that were investigated in at least three studies are included in the meta-analysis.
Factors predictive of LNM in surgery-only group
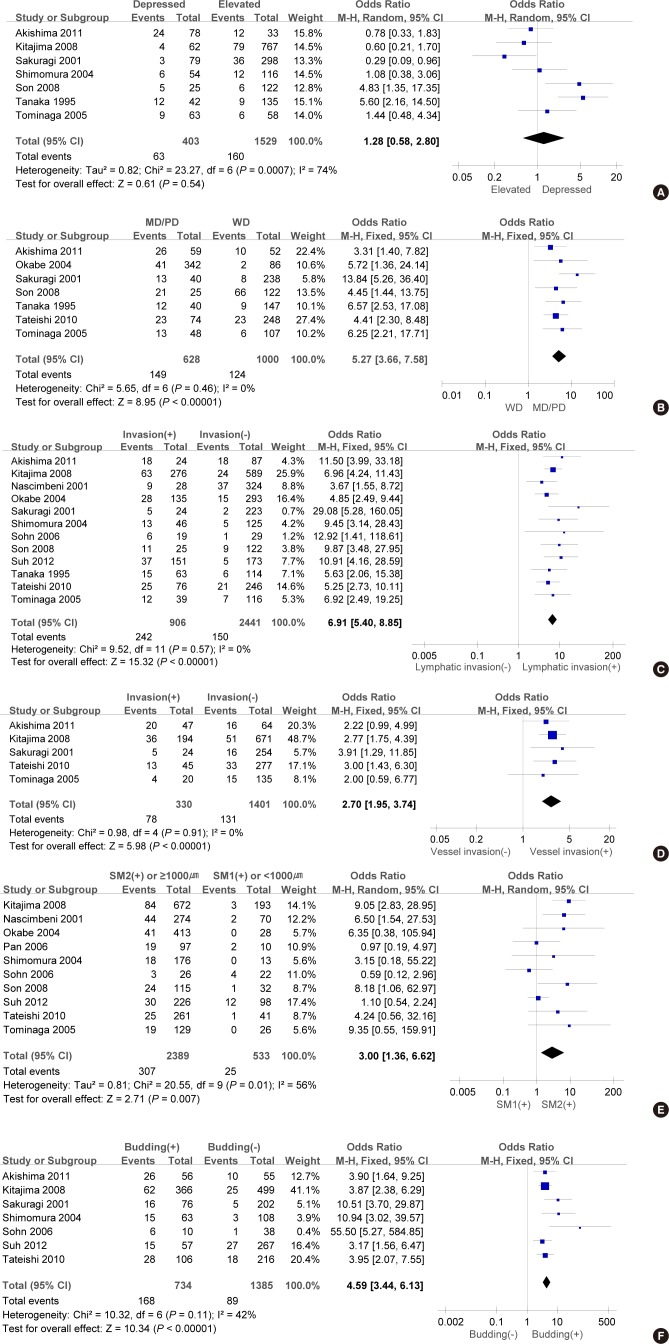
The results of the pooled analyses of the LNM rates of the group of early colorectal carcinoma patients who only underwent radical surgeries are presented in Fig. 2. Eight factors that were investigated in at least three studies included sex, carcinoma location, gross type of carcinoma, differentiation, depth of invasion, lymphovascular invasion and tumor budding.
Fig. 2. Forest plots for lymph node metastasis in early colorectal carcinoma patients who underwent radical surgery. Categorized by (A) grossly depressed carcinoma vs. elevated carcinoma, (B) poorly or moderately differentiation vs. well differentiation, (C) lymphatic invasion vs. absence of lymphatic invasion, (D) vascular invasion vs. absence of vascular invasion. (E) SM2 or ≥ 1,000 µm vs. SM1 or < 1,000 µm, and (F) tumor budding vs. absence of tumor budding.
Poorly or moderately differentiated carcinoma was a predictor of LNM in the surgery-only group (poorly or moderately vs. well differentiated adenocarcinoma, OR, 5.27; 95% CI, 3.66-7.58; P<0.001). When poorly differentiated adenocarcinoma was classified as an unfavorable histologic factor, poorly differentiated carcinoma was the most powerful predictor of LNM (poorly vs. moderately or well differentiated adenocarcinoma, OR, 8.27; 95% CI, 4.67-14.66; P<0.001). There is a clear difference between the LNM rate of deep invasion (>SM2, ≥1,000 µm) and that of SM1 or invasion of less than 1,000 µm (OR, 3.00; 95% CI, 1.36-6.62). Furthermore, compared to the patients without lymphatic invasion or vascular invasion, the patients with detected lymphatic invasion (OR, 6.91; 95% CI, 5.40-8.55) or vascular invasion (OR 2.70; 95% CI 1.95-3.74) showed a significant association with LNM. Tumor budding was also associated with a statistically significant increased risk of LNM (OR, 4.59 and 95% CI, 3.44-6.13).
In contrast, sex (male vs. female; OR, 0.89; 95% CI, 0.65-1.22) and location of carcinoma (left side colon vs. right side colon; OR, 1.65; 95% CI, 0.58-4.69) had no statistically significant association with the risk of LNM. In addition, the meta-analyses of seven studies did not find any association between the gross type of carcinoma and LNM (depressed type vs. elevated type; OR, 1.28; 95% CI, 0.58-2.80).
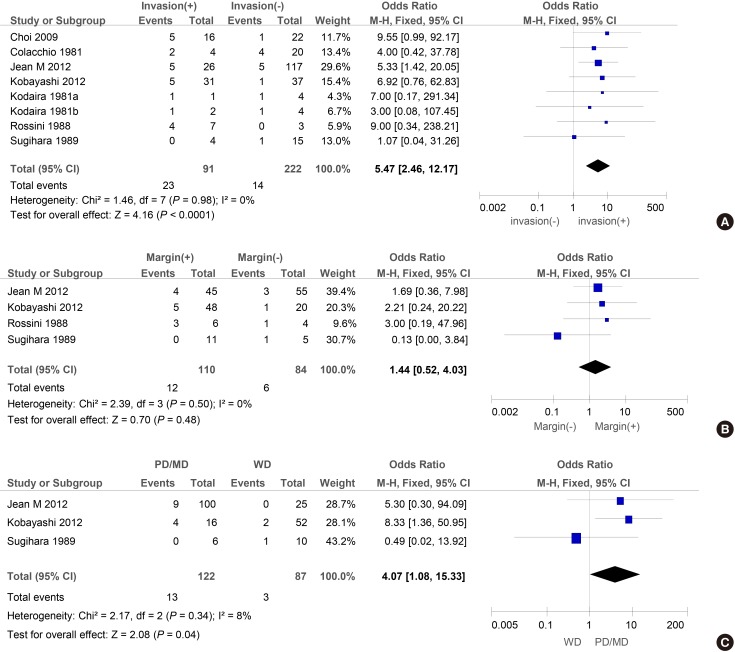
Factors predictive of LNM in additional surgeries after an endoscopic resection
Fig. 3 illustrates the OR of the risk of LNM in ECC patients who underwent additional surgeries after an endoscopic resection. Four calculated factors include gross type, lymphovascular invasion, margin status at the time of endoscopic resection, and differentiation. For instance, lymphovascular invasion was significantly associated with the risk of LNM (OR, 5.47; 95% CI, 2.46-12.17). Furthermore, compared to well-differentiated carcinoma, poorly or moderately differentiated carcinoma was significantly associated with LNM (OR, 4.07; 95% CI, 1.08-15.33). However, no risk was observed with the factors such as gross type (depressed or sessile type vs. elevated type; OR, 2.40; 95% CI, 0.56-10.18) and positive margin (OR, 1.44; 95% CI, 0.52-4.03).
Fig. 3. Forest plots for lymph node metastasis in early colorectal carcinoma patients who underwent additional surgeries after an endoscopic resection. Categorized by (A) lymphovascular invasion vs. absence of lymphovascular invasion, (B) positive margin vs. clear margin at the time of endoscopic resection, and (C) poorly or moderately differentiation vs. well differentiation.
DISCUSSION
Endoscopic resection safely and effectively removed most colorectal cancers in the mucosa or with superficial invasion of the submucosa (28). However, careful histological examinations of the resected specimens are required to determine any indications of subsequent surgical colectomy. Insufficient treatment and overtreatment in the management of colorectal cancer greatly influence patients' outcome. Many studies have explored the effectiveness of endoscopic treatment of ECC. The complete cure rate of EMR for ECC is known to be between 68.6% and 79%, and the local recurrence rate was 0.8% among completely cured cases (29, 30). Surgery is recommended for SM deep cancer or deeper invasion and when lymphovascular invasion or poorly differentiated cancer is diagnosed histologically (5, 9). The complete cure rate of submucosal carcinoma (37.5%) was significantly lower than that of intramucosal carcinoma (87.5%), although in some case we did not find any residual tumor in the surgically resected specimens collected from the patients who underwent additional surgeries after an endoscopic resection. Furthermore, colectomy and total mesorectal excision are believed to be associated with considerable surgery-related morbidity. The mortality after surgery for rectal cancer is reported to be 1.9%-6.5% and 3.2%-9.8% after surgery for colon cancer (6, 7).
We investigated the pathological risk factors for LNM in ECC which can provide data for an evidence-based decision regarding follow-up or additional radical surgeries after an endoscopic resection. We found that the frequency of LNM is 20.7% in patients with ECC. The strongest predictors of LNM for ECC sorted by OR in descending order are poor histological differentiation, lymphatic invasion, tumor budding, depth of submucosal invasion (SM2 or ≥1,000 µm), and vascular invasion. Several guidelines such as American (National Cancer Institute), British, Japanese and Dutch national guidelines have already included some of the characteristics discussed above as the indicators for high-risk lesions that necessitate additional radical surgery (31, 32, 33, 34).
Meanwhile, poorly or moderately differentiated carcinoma was a predictor of LNM in the surgery-only group. The OR of poorly differentiated adenocarcinoma was greater than that of poorly or moderately differentiated carcinoma. In line with the results of this study, many studies have asserted that an unfavorable histologic grade such as poorly differentiated carcinoma is a risk factor for LNM of colorectal cancer (35, 36). Most of the studies whose data are included in the additional surgery group compare well differentiated adenocarcinoma against poorly and moderately differentiated adenocarcinoma by classifying them together as an unfavorable histologic factor. Therefore, the OR of poorly differentiated adenocarcinoma could not be analyzed independently for the analysis of the additional surgery group. Regardless of this, the unfavorable histologic group did present a high OR. It is important to recognize that well differentiated submucosal adenocarcinomas are more associated with a lower risk of LNM than a moderately differentiated one. For example, one study pointed out that 44% (30/68) of patients who received additional resection with en bloc removal of regional lymph nodes had well differentiated adenocarcinomas without any evidence of lymphovascular invasion or LNM. That is, additional surgical treatment after endoscopic resection might be unnecessary in patients who have well differentiated T1 adenocarcinomas without lymphovascular invasion (27).
Moreover, vascular or lymphatic channel invasion has long been recognized as a risk factor for metastatic disease. Coverlizza et al. (37) reported that 45% of patients with lymphatic invasion also had lymph node metastases. In our series, detection of lymphatic or vascular invasion is significantly associated with LNM in patients with ECC who underwent radical surgery only compared to the ones who underwent additional surgeries after an endoscopic resection. The studies that are used to provide the data for the additional surgery groups argue that lymphovascular invasion is the most powerful predictor for LNM, and they listed lymphatic or vascular (sometimes called venous) invasion collectively as lymphovascular invasion. Many other studies also state that lymphatic invasion is one of the most powerful predictors of LNM. On the other hand, as the two factors are combined into a single factor called lymphovascular invasion, an intermediate relative risk is generated logically and becomes less informative (38). Therefore, lymphatic invasion and vascular invasion should be described and investigated as separate variables in order for them to be more useful in predicting LNM.
Tumor budding is usually described as foci of isolated cancer cells or a cluster of fewer than five cancer cells at the invasive front of the lesion (38). All seven studies that produced data on tumor budding view that budding can be a risk factor for LNM, and show that its OR is minimum 3.17. Only few authors provided a cut-off value or definition, whilst the rest preferred various definitions. Moreover, as most studies that are included for the additional surgery group lack data on budding, it was impossible to analyze the relevant data.
Various methods of dividing patients into a low or high risk group based on the depths of submucosal invasion are described in the literature (38). For the purpose of the current meta-analysis, the studies were divided into two groups: high risk group (SM2 or ≥1,000 µm) and relatively low risk group (SM1 or <1,000 µm). High risk group showed a sharp increase in the relative risk for LNM. Most studies included for the additional surgery group used different definitions of invasion, and thus it was impossible to analyze the data on deep invasion.
Clinical factors (sex, gross type of carcinoma, and polyp location) did not differ between the patients with LNM and the ones without LNM. This study was able to confirm that microscopic margin status at the time of polypectomy is not associated with LNM. There are other studies that appear to agree with this finding, and they suggest that residual disease in the colon wall is the one that is associated with LNM (26). Several guidelines recommend additional curative surgery, if the margin of excision cannot be assessed or if it is pathologically involved (27). However, the result of our study suggests that a minimally invasive approach such as regional lymph node dissection alone should be carefully considered in patients who do not satisfy the criterion complete resection margins. In particular, considering the fact that surgeries could potentially impair the quality of life in patients with rectal cancer, additional endoscopic resection of the remnant lesion might be effective enough to treat rectal cancer (39). In terms of the length of hospital stay and time to oral intake after the procedures, both periods were shorter for the ESD group than for the laparoscopic-assisted colorectal (LAC) surgery group (40). ESD and LAC have quite different indications, however, so if the primary indications are a noninvasive colorectal lesion diagnosed preoperatively as intramucosal to SM1, the patient's quality of life following treatment for such an early colorectal cancer would probably be better with ESD (40).
The limitations of the current study are that we were only able to evaluate a small number of factors because of the limited number of studies available, used various definitions and classifications, and were unable to present relevant data. Furthermore, we could not investigate different combinations of the factors.
In conclusion, deep submucosal invasion (>SM2 or ≥1,000 µm), poorly or moderately differentiated tumor, vascular invasion, lymphatic invasion and tumor budding are risk factors of lymph node metastasis in ECC. In addition, poorly or moderately differentiated tumors, or lymphovascular invasion on polypectomy specimens were also associated with lymph node metastasis after endoscopic resection for early colorectal cancer. However, more studies are needed to investigate every single factor discussed above and they should aim to standardize the detection of these powerful markers, preferably by using a unified definition of each factor.
Footnotes
The authors have no potential conflicts of interest to disclose.
Conception and design of the study: Jung SA, Cho WY. Acquisition of data: Choi JY, Cho WY. Analyzed the data: Kong KA. First draft of manuscript: Choi JY, Jung SA, Cho WY. Revision and critical review of the manuscript: Jung SA, Shim KN, Keum B, Byeon JS, Huh KC, Jang BI, Chang DK, Jung HY. ICMJE criteria for authorship read and met: Choi JY, Jung SA, Cho WY, Shim KN, Keum B, Byeon JS, Huh KC, Jang BI, Chang DK, Jung HY, Kong KA. Agree with manuscript results and conclusions: Choi JY, Jung SA, Cho WY, Shim KN, Keum B, Byeon JS, Huh KC, Jang BI, Chang DK, Jung HY, Kong KA.
References
- 1.Sobin LH, Wittekind C International Union against Cancer. TNM : classification of malignant tumours. 6th ed. New York: Wiley-Liss; 2002. [Google Scholar]
- 2.Kyzer S, Bégin LR, Gordon PH, Mitmaker B. The care of patients with colorectal polyps that contain invasive adenocarcinoma. Endoscopic polypectomy or colectomy? Cancer. 1992;70:2044–2050. doi: 10.1002/1097-0142(19921015)70:8<2044::aid-cncr2820700805>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 3.Minamoto T, Mai M, Ogino T, Sawaguchi K, Ohta T, Fujimoto T, Takahashi Y. Early invasive colorectal carcinomas metastatic to the lymph node with attention to their nonpolypoid development. Am J Gastroenterol. 1993;88:1035–1039. [PubMed] [Google Scholar]
- 4.Tanaka S, Haruma K, Teixeira CR, Tatsuta S, Ohtsu N, Hiraga Y, Yoshihara M, Sumii K, Kajiyama G, Shimamoto F. Endoscopic treatment of submucosal invasive colorectal carcinoma with special reference to risk factors for lymph node metastasis. J Gastroenterol. 1995;30:710–717. doi: 10.1007/BF02349636. [DOI] [PubMed] [Google Scholar]
- 5.Morson BC, Whiteway JE, Jones EA, Macrae FA, Williams CB. Histopathology and prognosis of malignant colorectal polyps treated by endoscopic polypectomy. Gut. 1984;25:437–444. doi: 10.1136/gut.25.5.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iversen LH, Nielsen H, Pedersen L, Harling H, Laurberg S. Seasonal variation in short-term mortality after surgery for colorectal cancer? Colorectal Dis. 2010;12:e31–e36. doi: 10.1111/j.1463-1318.2009.01888.x. [DOI] [PubMed] [Google Scholar]
- 7.Paulson EC, Mitra N, Sonnad S, Armstrong K, Wirtalla C, Kelz RR, Mahmoud NN. National Cancer Institute designation predicts improved outcomes in colorectal cancer surgery. Ann Surg. 2008;248:675–686. doi: 10.1097/SLA.0b013e318187a757. [DOI] [PubMed] [Google Scholar]
- 8.Akishima-Fukasawa Y, Ishikawa Y, Akasaka Y, Uzuki M, Inomata N, Yokoo T, Ishii R, Shimokawa R, Mukai K, Kiguchi H, et al. Histopathological predictors of regional lymph node metastasis at the invasive front in early colorectal cancer. Histopathology. 2011;59:470–481. doi: 10.1111/j.1365-2559.2011.03964.x. [DOI] [PubMed] [Google Scholar]
- 9.Kitajima K, Fujimori T, Fujii S, Takeda J, Ohkura Y, Kawamata H, Kumamoto T, Ishiguro S, Kato Y, Shimoda T, et al. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol. 2004;39:534–543. doi: 10.1007/s00535-004-1339-4. [DOI] [PubMed] [Google Scholar]
- 10.Nascimbeni R, Burgart LJ, Nivatvongs S, Larson DR. Risk of lymph node metastasis in T1 carcinoma of the colon and rectum. Dis Colon Rectum. 2002;45:200–206. doi: 10.1007/s10350-004-6147-7. [DOI] [PubMed] [Google Scholar]
- 11.Okabe S, Shia J, Nash G, Wong WD, Guillem JG, Weiser MR, Temple L, Sugihara K, Paty PB. Lymph node metastasis in T1 adenocarcinoma of the colon and rectum. J Gastrointest Surg. 2004;8:1032–1039. doi: 10.1016/j.gassur.2004.09.038. discussion 9-40. [DOI] [PubMed] [Google Scholar]
- 12.Pan W, Terai T, Abe S, Sakamoto N, Nagahara A, Ohkusa T, Ogihara T, Sato N. Location of early colorectal cancers at fold-top may reduce the risk of lymph node metastasis. Dis Colon Rectum. 2006;49:579–587. doi: 10.1007/s10350-006-0508-3. [DOI] [PubMed] [Google Scholar]
- 13.Sakuragi M, Togashi K, Konishi F, Koinuma K, Kawamura Y, Okada M, Nagai H. Predictive factors for lymph node metastasis in T1 stage colorectal carcinomas. Dis Colon Rectum. 2003;46:1626–1632. doi: 10.1007/BF02660767. [DOI] [PubMed] [Google Scholar]
- 14.Shimomura T, Ishiguro S, Konishi H, Wakabayashi N, Mitsufuji S, Kasugai T, Manou M, Kodama T. New indication for endoscopic treatment of colorectal carcinoma with submucosal invasion. J Gastroenterol Hepatol. 2004;19:48–55. doi: 10.1111/j.1440-1746.2004.03261.x. [DOI] [PubMed] [Google Scholar]
- 15.Sohn DK, Chang HJ, Park JW, Choi DH, Han KS, Hong CW, Jung KH, Kim DY, Lim SB, Choi HS, et al. Histopathological risk factors for lymph node metastasis in submucosal invasive colorectal carcinoma of pedunculated or semipedunculated type. J Clin Pathol. 2007;60:912–915. doi: 10.1136/jcp.2006.043539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Son HJ, Song SY, Lee WY, Yang SS, Park SH, Yang MH, Yoon SH, Chun HK. Characteristics of early colorectal carcinoma with lymph node metastatic disease. Hepatogastroenterology. 2008;55:1293–1297. [PubMed] [Google Scholar]
- 17.Suh JH, Han KS, Kim BC, Hong CW, Sohn DK, Chang HJ, Kim MJ, Park SC, Park JW, Choi HS, et al. Predictors for lymph node metastasis in T1 colorectal cancer. Endoscopy. 2012;44:590–595. doi: 10.1055/s-0031-1291665. [DOI] [PubMed] [Google Scholar]
- 18.Tateishi Y, Nakanishi Y, Taniguchi H, Shimoda T, Umemura S. Pathological prognostic factors predicting lymph node metastasis in submucosal invasive (T1) colorectal carcinoma. Mod Pathol. 2010;23:1068–1072. doi: 10.1038/modpathol.2010.88. [DOI] [PubMed] [Google Scholar]
- 19.Tominaga K, Nakanishi Y, Nimura S, Yoshimura K, Sakai Y, Shimoda T. Predictive histopathologic factors for lymph node metastasis in patients with nonpedunculated submucosal invasive colorectal carcinoma. Dis Colon Rectum. 2005;48:92–100. doi: 10.1007/s10350-004-0751-4. [DOI] [PubMed] [Google Scholar]
- 20.Colacchio TA, Forde KA, Scantlebury VP. Endoscopic polypectomy: inadequate treatment for invasive colorectal carcinoma. Ann Surg. 1981;194:704–707. doi: 10.1097/00000658-198112000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kodaira S, Teramoto T, Ono S, Takizawa K, Katsumata T, Abe O. Lymph node metastases from carcinomas developing in pedunculated and semipedunculated colorectal adenomas. Aust N Z J Surg. 1981;51:429–433. doi: 10.1111/j.1445-2197.1981.tb05977.x. [DOI] [PubMed] [Google Scholar]
- 22.Kodaira S, Ono S, Purri P, Takizawa K, Kotake K, Tsuyuki A, Okuda M, Abe O. Endoscopic polypectomy of the large bowel: management of cancer-bearing polyps. Int Surg. 1981;66:311–314. [PubMed] [Google Scholar]
- 23.Choi DH, Sohn DK, Chang HJ, Lim SB, Choi HS, Jeong SY. Indications for subsequent surgery after endoscopic resection of submucosally invasive colorectal carcinomas: a prospective cohort study. Dis Colon Rectum. 2009;52:438–445. doi: 10.1007/DCR.0b013e318197e37f. [DOI] [PubMed] [Google Scholar]
- 24.Rossini FP, Ferrari A, Coverlizza S, Spandre M, Risio M, Gemme C, Cavallero M. Large bowel adenomas containing carcinoma--a diagnostic and therapeutic approach. Int J Colorectal Dis. 1988;3:47–52. doi: 10.1007/BF01649684. [DOI] [PubMed] [Google Scholar]
- 25.Sugihara K, Muto T, Morioka Y. Management of patients with invasive carcinoma removed by colonoscopic polypectomy. Dis Colon Rectum. 1989;32:829–834. doi: 10.1007/BF02554549. [DOI] [PubMed] [Google Scholar]
- 26.Butte JM, Tang P, Gonen M, Shia J, Schattner M, Nash GM, Temple LK, Weiser MR. Rate of residual disease after complete endoscopic resection of malignant colonic polyp. Dis Colon Rectum. 2012;55:122–127. doi: 10.1097/DCR.0b013e3182336c38. [DOI] [PubMed] [Google Scholar]
- 27.Kobayashi H, Higuchi T, Uetake H, Iida S, Ishikawa T, Ishiguro M, Sugihara K. Resection with en bloc removal of regional lymph node after endoscopic resection for T1 colorectal cancer. Ann Surg Oncol. 2012;19:4161–4167. doi: 10.1245/s10434-012-2471-7. [DOI] [PubMed] [Google Scholar]
- 28.Larghi A, Waxman I. State of the art on endoscopic mucosal resection and endoscopic submucosal dissection. Gastrointest Endosc Clin N Am. 2007;17:441–469. v. doi: 10.1016/j.giec.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 29.Tung SY, Wu CS. Clinical outcome of endoscopically removed early colorectal cancer. J Gastroenterol Hepatol. 2003;18:1175–1179. doi: 10.1046/j.1440-1746.2003.03134.x. [DOI] [PubMed] [Google Scholar]
- 30.Bergmann U, Beger HG. Endoscopic mucosal resection for advanced non-polypoid colorectal adenoma and early stage carcinoma. Surg Endosc. 2003;17:475–479. doi: 10.1007/s00464-002-8931-6. [DOI] [PubMed] [Google Scholar]
- 31.National Cancer Institute. Rectal Cancer Treatment (PDQ®) [accessed on 19 March 2014]. Available at http://www.cancer.gov/cancertopics/pdq/treatment/rectal/HealthProfessional/page4/page5.
- 32.The Association of Coloproctology of Great Britain and Ireland. Guidelines for the management of colorectal cancer. 3rd ed. London: Association of Coloproctology of Great Britain & Ireland; 2007. [accessed on 19 March 2014]. p. 117. Available at http://acpgbi.mixd.co.uk/content/uploads/2007-CC-Management-Guidelines.pdf. [Google Scholar]
- 33.Labianca R, Nordlinger B, Beretta GD, Brouquet A, Cervantes A ESMO Guidelines Working Group. Primary colon cancer: ESMO Clinical Practice Guidelines for diagnosis, adjuvant treatment and follow-up. Ann Oncol. 2010;21:v70–v77. doi: 10.1093/annonc/mdq168. [DOI] [PubMed] [Google Scholar]
- 34.Japanese Society for Cancer of the Colon and Rectum. Japanese guidelines for the treatment of colorectal carcinoma. Tokyo: Kanehara Shuppan Co; 2010. pp. 42–43. [Google Scholar]
- 35.Kobayashi H, Mochizuki H, Morita T, Kotake K, Teramoto T, Kameoka S, Saito Y, Takahashi K, Hase K, Oya M, et al. Characteristics of recurrence after curative resection for T1 colorectal cancer: Japanese multicenter study. J Gastroenterol. 2011;46:203–211. doi: 10.1007/s00535-010-0341-2. [DOI] [PubMed] [Google Scholar]
- 36.Cooper HS, Deppisch LM, Gourley WK, Kahn EI, Lev R, Manley PN, Pascal RR, Qizilbash AH, Rickert RR, Silverman JF, et al. Endoscopically removed malignant colorectal polyps: clinicopathologic correlations. Gastroenterology. 1995;108:1657–1665. doi: 10.1016/0016-5085(95)90126-4. [DOI] [PubMed] [Google Scholar]
- 37.Coverlizza S, Risio M, Ferrari A, Fenoglio-Preiser CM, Rossini FP. Colorectal adenomas containing invasive carcinoma. Pathologic assessment of lymph node metastatic potential. Cancer. 1989;64:1937–1947. doi: 10.1002/1097-0142(19891101)64:9<1937::aid-cncr2820640929>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 38.Bosch SL, Teerenstra S, de Wilt JH, Cunningham C, Nagtegaal ID. Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy. 2013;45:827–834. doi: 10.1055/s-0033-1344238. [DOI] [PubMed] [Google Scholar]
- 39.Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Hölzel D. Quality of life in rectal cancer patients: a four-year prospective study. Ann Surg. 2003;238:203–213. doi: 10.1097/01.sla.0000080823.38569.b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saito Y, Otake Y, Sakamoto T, Nakajima T, Yamada M, Haruyama S, So E, Abe S, Matsuda T. Indications for and technical aspects of colorectal endoscopic submucosal dissection. Gut Liver. 2013;7:263–269. doi: 10.5009/gnl.2013.7.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]