Abstract
We investigated the effects of weekend admission on adverse cardiac events in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). Patients with NSTE-ACS treated with percutaneous coronary intervention (PCI) were divided into a "weekend group" and a "weekday group" according to the emergency room arrival time. The primary outcome was 30-day major adverse cardiac events (MACE) including cardiac death, recurrent myocardial infarction, repeat revascularization, and urgent PCI. Of 577 patients, 168 patients were allocated to the weekend and 409 patients to the weekday group. The incidence of 30-day MACE was significantly higher in the weekend group (Crude: 15.5% vs. 7.3%, P = 0.005; propensity score matched: 12.8% vs. 4.8%, P = 0.041). After adjustment for all the possible confounding factors, in Cox proportional hazard regression analysis, weekend admission was associated with a 2.1-fold increased hazard for MACE (HR, 2.13; 95% CI, 1.26-3.60, P = 0.005). These findings indicate that weekend admission of patients with NSTE-ACS is associated with an increase in 30-day adverse cardiac event.
Graphical Abstract
Keywords: Coronary Artery Disease, Acute Coronary Syndrome, Percutaneous Coronary Intervention
INTRODUCTION
It has been well established that the immediate reperfusion therapy lowers mortality in patients with ST-segment elevation myocardial infarction (STEMI) (1). In contrast, for patients presenting with non-ST-segment elevation acute coronary syndrome (NSTE-ACS), guidelines do not recommend an immediate revascularization (2, 3). Instead, in patients with NSTE-ACS, revascularization is typically performed 12-72 hr after medical stabilization, except in those with hemodynamic instability, electrical instability, or refractory ischemia who require urgent revascularization (4).
With regard to the hospital arrival time, during the weekend, invasive revascularization procedures can be delayed inappropriately (5, 6, 7). Hospitals have reduced staffing levels on the weekend and an interventional cardiologist may not be immediately available, possibly leading to a delay in the revascularization procedure for patients with NSTE-ACS (8, 9, 10, 11).
Therefore, we sought to examine the effects of weekend admission on clinical outcomes in patients with NSTE-ACS undergoing percutaneous coronary intervention (PCI). The hypothesis was that the incidence of major adverse cardiac events (MACE) is increased in patients who are admitted to the hospital during the weekend than those admitted during the weekday.
MATERIALS AND METHODS
Study design and study population
Patients who were admitted to the coronary care unit (CCU) via the emergency room (ER) from January 2007 to December 2010 in Seoul National University Bundang Hospital were retrospectively identified for the inclusion in this study. The inclusion criteria included the diagnosis of unstable angina pectoris (UA) or non-ST-segment elevation myocardial infarction (NSTEMI). The exclusion criteria were patients diagnosed with STEMI or stable angina, patients admitted to the general ward or via an outpatient clinic, and patients experiencing UA or NSTEMI during hospitalization for other medical conditions. Patients who had undergone coronary artery bypass graft surgery (CABG) after diagnostic coronary angiography (CAG) were also excluded. Since medically-managed ACS patients comprised a heterogeneous population including patients without severe coronary stenosis, those with coronary artery spasm, and patients who refused PCI or CABG due to economic reason, those patients were also excluded from the study.
The patient's demographic and clinical characteristics, laboratory tests and angiographic characteristics were reviewed. Cardiac biomarkers including creatine kinase-myocardial band (CK-MB) and Troponin-I were checked every 8 hr from the admission until PCI, and twice a day after PCI for one day, and daily until their normalization. In addition, we collected the exact time, day, and date of symptom onset, admission to ER and then CCU, and the first balloon inflation time during PCI. In our hospital, NSTE-ACS patients visiting ER from Sunday to Thursday after 6 p.m. undergo PCI in the next-day morning and those who visit ER between Friday 6 p.m. to Sunday 5:59 p.m. undergo PCI in coming Monday morning. The enrolled patients were divided into two groups according to ER admission time. Patients who were admitted to the ER from Friday 6 p.m. to Sunday 5:59 p.m. or from the day before holiday 6 p.m. to holiday 5:59 p.m. were allocated to the 'weekend group'. Patients who were admitted to the ER during all other time periods were classified as the 'weekday group'. Event adjudication was done by two experienced reviewers. If the two reviewers' opinions disagree, then a third reviewer evaluated the clinical events and established the adjudication.
Definition
Patients were diagnosed as NSTE-ACS if there were appropriate clinical manifestations including chest discomfort or angina-equivalent suggesting UA with or without positive biomarkers of necrosis in the absence of electrocardiographic ST-segment elevation (12). UA was defined as angina pectoris with at least one of three features: 1) chest pain occurring at rest and usually lasting >20 min; 2) chest pain being severe and usually described as frank pain; or 3) chest pain occurring with a crescendo pattern. We differentiated between NSTEMI and UA based on cardiac troponin I with at least one value above the 99th percentile of the upper reference level (13, 14). The risk stratification was done using thrombolysis in myocardial infarction (TIMI) risk scores and the scores classified as low (TIMI risk score 0-2), intermediate (TIMI risk score 3-4), and high risk (TIMI risk score 5-7) (15, 16). We defined symptom-to-admission time as the time from current angina symptom onset to admission to the ER. Also, admission-to-PCI time referred to the time interval between admission to the ER and time of the first balloon inflation to culprit lesion.
Study outcomes
The primary outcome was the incidence of MACE during the 30-day follow-up period after admission to the ER, including cardiac death, recurrent myocardial infarction (MI), repeat revascularization and urgent PCI. MI was defined according to the universal definition of myocardial infarction, and recurrent MI was defined to MI which occurred after an incident event with 20% or greater increase of the cardiac troponin I in the second sample compared to the sample at the time of suspected recurrent MI (13). Repeat revascularization included target or non-target vessel revascularization including CABG. We also examined the incidence of urgent PCI which was performed in cases of refractory angina, hemodynamic instability, or electrical instability, during the period of medical stabilization.
To determine whether the PCI was urgent one or not, for patients who experienced unstable clinical condition during the period of medical stabilization, we reviewed the vital sign chart, nursing records, doctors' records including physical examination, and the test results including electrocardiogram for ST-segment change or ventricular tachyarrhythmia and cardiac enzymes. The secondary outcomes included the incidence of cardiac death, recurrent MI, repeat revascularization, urgent PCI, peak CK-MB level during hospital stay, and peak troponin-I level during hospital stay. Also, we investigated the daily distribution of MACE according to ER admission day. Moreover, we evaluated the clinical outcomes including cardiac death, myocardial infarction, and repeat revascularization at 18 months.
Statistical analysis
All categorical data were summarized as frequencies and percentages, whereas statistics for continuous variables are presented as means and standard deviations. The Pearson's chi-square test was used for comparison of categorical variables and the Fisher's exact test was used for comparison of categorical variables with 20% or more of the expected cell frequencies below 5. The Student's t-test was used for comparison of continuous variables and the Mann-Whitney U-test was used for sample sizes below 30 in at least one group. Linear-by-linear association was used to extract trend of clinical characteristics and MACE according to ER admission day. The time interval trend according to ER admission day was evaluated using ANOVA. In addition, we selected a propensity score matched population to adjust for uneven distribution of baseline characteristics; a 1:1 matched analysis without replacement was performed using propensity score. Logistic regression model was conducted to generate propensity score which was probability that a patient admitted in weekend. The adjusted variables were as follows: age, sex, height, body weight, body mass index, hypertension, diabetes mellitus, hyperlipidemia, smoking, previous MI history, previous CABG history, symptom-to-admission time, admission-to-PCI time, hemoglobin, estimated glomerular filtration rate, total cholesterol, triglyceride, HDL-cholesterol, LDL-cholesterol, NT-proBNP, hsCRP, elevation of CK-MB, elevation of troponin-I, ischemic change of ECG, left ventricular ejection fraction, TIMI risk scores, culprit artery, and extent of coronary artery disease. The Greedy 5→1 digit match algorithm was used for matching. We were able to match 125 patients in weekend group to 125 patients in weekday group. McNemar's test and marginal homogeneity test were used for comparison of categorical variables between the matched patient groups, paired t-test for continuous variables. Multivariate Cox proportional hazards regression analyses were performed to evaluate the risk of 30-day MACE with adjustment for individual risk factors. We obtained hazard ratio of weekend admission for MACE with the adjustment of sequentially-added potential confounding factors, including clinical characteristics, time factors, and severity factors. In addition, survival analyses and the log-rank test were used to compare 30-day MACE-free survival. A P value of less than 0.05 was considered statistically significant. All analyses were performed with SPSS v. 18.0 (SPSS Inc., Chicago, IL, USA).
Ethics statement
The study was approved by the institutional review board of the Seoul National University Bundang Hospital (No. B-1111-139-105), and was conducted according to the Declaration of Helsinki. Informed consent for study enrollment was waived by the board.
RESULTS
Baseline patients characteristics
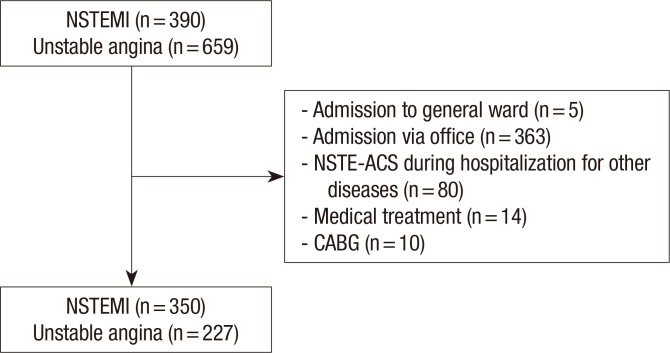
Among 1,049 patients screened, 577 patients with NSTE-ACS who had been admitted via ER and managed with PCI were finally enrolled in the study (Fig. 1). Study subjects were classified into the weekend group (n=168) or the weekday group (n=409) based on the ER admission day and time (Table 1). The weekend group showed significantly higher baseline cardiac enzyme, shorter symptom-to-admission time, and longer admission-to-PCI time compared to the weekday group. In addition, patients of weekend group had more intermediate to high TIMI risk scores than weekday group, with borderline statistical significance (66.1% vs. 57.5%, P=0.055). Concomitant medications were not significantly different except that heparin was administered more often in the weekend group. In the weekday group, the admission-to-PCI time did not differ between patients who arrive at ER after 6 p.m. on Sunday or holiday and those who arrive after 6 p.m. on weekdays excluding Friday (36.9±41.9 hr vs. 34.7±55.7 hr, P=0.741).
Fig. 1. Selection of patients. NSTEMI, non-ST-segment elevation myocardial infarction; NSTE-ACS, non-ST-segment elevation acute coronary syndrome; CABG, coronary artery bypass grafting.
Table 1. Baseline patient characteristics.
| Parameters | All (n = 577) | Weekend group (n = 168) | Weekday group (n = 409) | P value |
|---|---|---|---|---|
| Age (yr) | 63.7 ± 12.8 | 63.3 ± 13.1 | 64.0 ± 12.6 | 0.586 |
| Sex (male) | 412 (71.4%) | 123 (73.2%) | 289 (70.7%) | 0.537 |
| Height (cm) | 163.5 ± 8.8 | 164.3 ± 8.8 | 163.1 ± 8.8 | 0.128 |
| Body weight (kg) | 65.2 ± 11.6 | 66.3 ± 11.3 | 64.7 ± 11.7 | 0.130 |
| Body mass index (kg/m2) | 24.3 ± 3.3 | 24.5 ± 3.1 | 24.2 ± 3.4 | 0.382 |
| Hypertension | 358 (62.0%) | 107 (63.7%) | 251 (61.4%) | 0.602 |
| Diabetes mellitus | 186 (32.2%) | 53 (31.5%) | 133 (32.5%) | 0.821 |
| Hyperlipidemia | 171 (29.6%) | 55 (32.7%) | 116 (28.4%) | 0.296 |
| Smoking, current | 193 (33.4%) | 65 (38.7%) | 128 (31.3%) | 0.087 |
| Previous myocardial infarction | 82 (14.2%) | 24 (14.3%) | 58 (14.2%) | 0.974 |
| Previous CABG | 16 (2.8%) | 6 (3.6%) | 10 (2.4%) | 0.454 |
| Hemoglobin (g/dL) | 13.9 ± 2.1 | 13.9 ± 2.0 | 13.8 ± 2.2 | 0.688 |
| eGFR (mL/min/m2) | 66.0 ± 30.4 | 67.7 ± 32.5 | 65.3 ± 29.5 | 0.382 |
| Total cholesterol (mg/dL) | 190.7 ± 45.6 | 190.1 ± 41.9 | 190.9 ± 47.1 | 0.848 |
| Triglyceride (mg/dL) | 119.8 ± 85.6 | 124.2 ± 91.7 | 118.1 ± 83.0 | 0.440 |
| HDL-cholesterol (mg/dL) | 44.0 ± 10.7 | 43.9 ± 11.5 | 44.0 ± 10.4 | 0.929 |
| LDL-cholesterol (mg/dL) | 99.0 ± 33.8 | 98.4 ± 34.1 | 99.7 ± 33.7 | 0.687 |
| NT-proBNP (pg/mL) | 2,285.6 ± 6,431.9 | 2,117.9 ± 5,678.5 | 2,356.3 ± 6,730.2 | 0.695 |
| hsCRP (mg/dL) | 1.07 ± 2.54 | 1.29 ± 3.13 | 0.99 ± 2.24 | 0.255 |
| CK-MB elevation* | 208 (36.0%) | 73 (43.5%) | 135 (33.0%) | 0.018 |
| Troponin-I elevation* | 350 (60.7%) | 119 (70.8%) | 231 (56.5%) | 0.001 |
| Ischemic ECG change | 0.143 | |||
| ST depression | 169 (29.3%) | 59 (35.1%) | 110 (26.9%) | |
| T-wave inversion | 141 (24.4%) | 38 (22.6%) | 103 (25.2%) | |
| Echocardiographic LV EF (%) | 55.9 ± 11.1 | 55.2 ± 11.0 | 56.2 ± 11.2 | 0.362 |
| TIMI risk score | 0.136 | |||
| Low (0-2) | 231 (40.0%) | 57 (33.9%) | 174 (42.5%) | |
| Intermediate (3-4) | 277 (48.0%) | 87 (51.9) | 190 (46.5%) | |
| High (5-7) | 69 (12.0%) | 24 (14.3%) | 45 (11.0%) | |
| Culprit artery | 0.864 | |||
| Left main coronary artery | 19 (3.3%) | 5 (3.0%) | 14 (3.4%) | |
| Left anterior descending artery | 290 (50.3%) | 84 (49.4%) | 206 (50.6%) | |
| Left circumflex artery | 137 (23.7%) | 43 (25.6%) | 94 (23.0%) | |
| Right coronary artery | 129 (22.4%) | 37 (22.0%) | 92 (22.5%) | |
| CAD extent | 0.726 | |||
| 1 vessel disease | 198 (34.3%) | 60 (35.1%) | 138 (34.0%) | |
| 2 vessel disease | 182 (31.6%) | 49 (29.2%) | 133 (32.5%) | |
| 3 vessel disease | 197 (34.1%) | 60 (35.7%) | 137 (33.5%) | |
| Symptom-to-admission time (hr, median) | 133.2 ± 348.0 (10.0) | 82.7 ± 260.5 (6.0) | 154.0 ± 378.0 (12.0) | 0.010 |
| Admission to-PCI time (hr, median) | 38.1 ± 50.9 (25.0) | 45.3 ± 44.9 (37.6) | 35.2 ± 53.0 (21.7) | 0.030 |
| Concomitant medication | ||||
| Heparin | 531 (92.0%) | 163 (97.0%) | 368 (90.0%) | 0.005 |
| UFH | 471 (81.6%) | 149 (88.7%) | 322 (78.7%) | 0.070 |
| Enoxaparin | 60 (10.4%) | 14 (8.3%) | 46 (11.2%) | 0.070 |
| GpIIb/IIIa R antagonists | 117 (20.3%) | 38 (22.6%) | 79 (19.3%) | 0.370 |
| Tirofiban | 19 (3.3%) | 3 (1.8%) | 16 (3.9%) | 0.303 |
| Abciximab | 100 (17.3%) | 35 (20.8%) | 65 (15.9%) | 0.154 |
| Aspirin | 577 (100.0%) | 168 (100.0%) | 409 (100.0%) | 1.000 |
| Clopidogrel | 577 (100.0%) | 168 (100.0%) | 409 (100.0%) | 1.000 |
| Beta-blocker | 372 (64.5%) | 111 (66.1%) | 261 (63.8%) | 0.633 |
| ACEI | 341 (59.2%) | 107 (63.7%) | 234 (57.4%) | 0.163 |
| ARB | 93 (16.1%) | 27 (16.1%) | 66 (16.1%) | 1.000 |
| DHP CCB | 79 (13.7%) | 24 (14.3%) | 55 (13.4%) | 0.791 |
| Non-DHP CCB | 36 (6.2%) | 12 (7.1%) | 24 (5.9%) | 0.573 |
| Nitrates | 97 (16.8%) | 26 (15.5%) | 71 (17.4%) | 0.626 |
| Statin | 474 (82.3%) | 140 (83.3%) | 334 (81.9%) | 0.720 |
*>1×upper reference limit; CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NT-proBNP, N-terminal-proB-type natriuretic peptide; hsCRP, high-sensitivity C-reactive protein; CK-MB, creatine kinase-myocardial band; ECG, electrocardiography; LV EF, left ventricular ejection fraction; TIMI, thrombolysis in myocardial infarction; CAD, coronary artery disease; PCI, percutaneous coronary intervention; UFH, unfractionated heparin; GpIIb/IIIa R, glycoprotein IIb/IIIa receptor; ACEI, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker; DHP CCB, dihydropyridine-calcium channel blocker.
Clinical outcomes at 30 days of follow-up
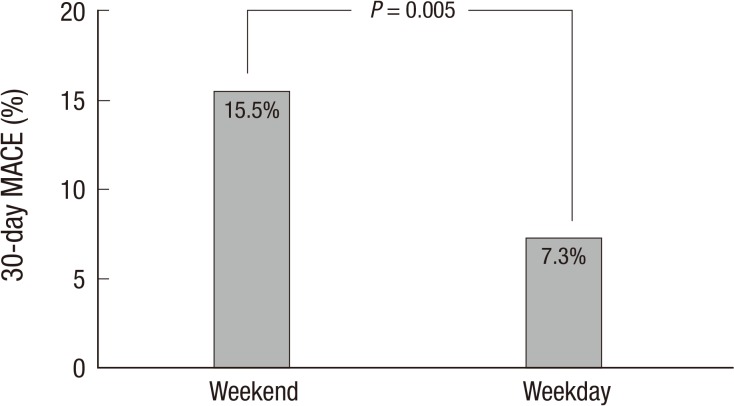
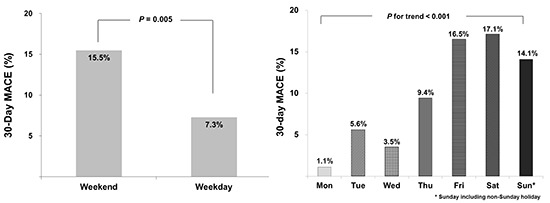
The weekend group had higher 30-day MACE rate than the weekday group (15.5% vs. 7.3%, P=0.005) (Fig. 2). The incidence of cardiac death (3.0% vs. 0.5%, P=0.025) and that of urgent PCI (12.5% vs. 6.8%, P=0.033) were also significantly higher in the weekend group (Table 2). Overall cardiac enzyme elevation was more frequent in the weekend group. When the whole patients were subgrouped into NSTEMI (n=350) and UA (n=227), there were similar results. The incidence rate of MACE was significantly higher in the weekend group in comparison with the weekday group in patients with NSTEMI (16.8% vs. 9.5%, P=0.047) and in patients with UA (12.2% vs. 4.5%, P=0.046).
Fig. 2. Thirty-day major adverse cardiac events (MACE) for patients with NSTE-ACS who were admitted on weekday or weekend. Of 577 patients, 26 patients in the weekend group (15.5%) and 30 patients in the weekday group (7.3%) had MACE within 30 days. The difference between the two groups was statistically significant (P = 0.005).
Table 2. Thirty-day clinical outcomes.
| Outcomes | All (n = 577) | Weekend group (n = 168) | Weekday group (n = 409) | P value |
|---|---|---|---|---|
| MACE* | 56 (9.7%) | 26 (15.5%) | 30 (7.3%) | 0.005 |
| Cardiac death | 7 (1.2%) | 5 (3.0%) | 2 (0.5%) | 0.025 |
| Recurrent MI | 2 (0.3%) | 2 (1.2%) | 0 (0.0%) | 0.084 |
| Repeat revascularization | 4 (0.7%) | 2 (1.2%) | 2 (0.5%) | 0.584 |
| Urgent PCI | 49 (8.5%) | 21 (12.5%) | 28 (6.8%) | 0.033 |
| CK-MB elevation, overall | 320 (55.5%) | 117 (69.6%) | 203 (49.6%) | < 0.001 |
| Peak CK-MB level | 62.2 ± 142.3 | 74.0 ± 108.6 | 57.4 ± 153.9 | 0.080 |
| Troponin-I elevation, overall | 454 (78.7%) | 149 (88.7%) | 305 (74.6%) | < 0.001 |
| Peak Troponin-I level | 22.5 ± 67.8 | 30.3 ± 78.8 | 19.4 ± 62.6 | 0.203 |
*MACE (major adverse cardiac event) including cardiac death, recurrent MI, repeat revascularization, and unplanned urgent PCI. MI, myocardial infarction; PCI, percutaneous coronary intervention; CK-MB, creatine kinase-myocardial band.
Most MACE occurred within 5 days after PCI in both groups, and the distribution patterns were similar between the two groups (Table 3). Seven patients died of cardiac causes, five in the weekend group and 2 in the weekday group. In the weekend group, four had cardiogenic shocks and one ventricular tachyarrhythmia, while in the weekday group one had cardiogenic shock and one ventricular tachyarrhythmia. There was no significant difference in the incidence of MACE among eight PCI operators (P=0.100) and between four senior operators and four junior operators (7.9% vs. 12.2%, P=0.082).
Table 3. Distribution of the occurrence of MACE.
| MACE duration | All | Weekend group (n = 26) | Weekday group (n = 30) | P value |
|---|---|---|---|---|
| Day 1-5 | 52 (92.9%) | 23 (88.4%) | 29 (96.7%) | 0.490 |
| Day 6-10 | 2 (3.6%) | 1 (3.8%) | 1 (3.3%) | - |
| Day 11-20 | 1 (1.8%) | 1 (3.8%) | 0 (0%) | - |
| Day 21-30 | 1 (1.8%) | 1 (3.8%) | 0 (0%) | - |
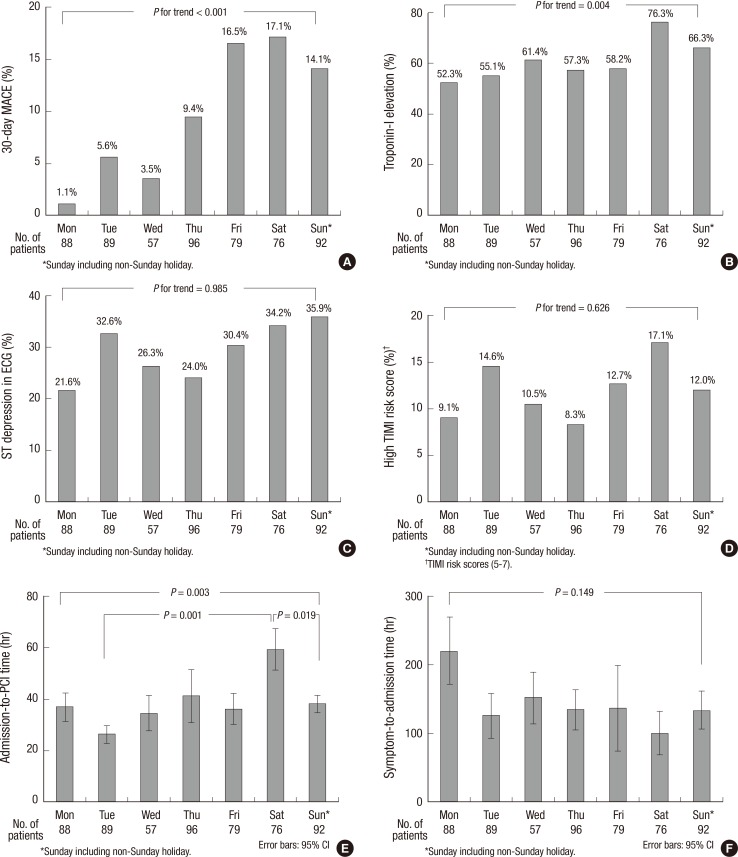
Interestingly, there was a trend of gradual increase in MACE from the start of a week toward the weekend with a highest incidence on Saturday followed by Friday (Fig. 3A). With regard to the potential factors that can contribute to the occurrence of MACE (Fig. 3B-F), baseline Troponin-I elevation and the admission-to-PCI time showed similar distribution pattern as the MACE distribution with a peak on Saturday, suggesting some causal role in the increase of MACE in the weekend group. The distribution of symptom-to-admission time showed a reverse pattern of MACE, showing a trend of longest time on Monday and gradual decrease toward the weekend, without statistical significance.
Fig. 3. Outcomes and baseline characteristics according to ER admission day. (A) Thirty-day major adverse cardiac events (MACE) according to ER admission day. The incidence of MACE shows a trend of increase from Monday to Sunday. (B) Baseline Troponin-I elevation according to ER admission day. Distribution of patients with elevated baseline troponin-I shows a trend of gradual increase from Monday to Sunday. (C) Baseline electrocardiographic ST-segment depression according to ER admission day. Distribution of patients with baseline ECG change does not show statistically significant trend. (D) Baseline high TIMI risk score according to ER admission day. Distribution of patients with high TIMI risk score did not get statistically significant trend. (E) Admission to-PCI time according to ER admission day. The admission-to-PCI time has a trend of gradual increase from Monday to Saturday, revealing significantly longer time on Saturday than Tuesday or Sunday. (F) Symptom to-admission time according to ER admission day. The distribution of symptom-to-admission time shows a trend of longest time on Monday and gradual decrease toward the weekend, without statistical significance.
However, there was no significant difference in MACE between the weekend group and the weekday group at 18 months (19.0% vs. 19.6%, P=0.888) (Table 4).
Table 4. Eighteen-month cumulative clinical outcomes.
| Outcomes | All (n = 577) | Weekend group (n = 168) | Weekday group (n = 409) | P value |
|---|---|---|---|---|
| MACE* | 111 (19.2%) | 32 (19.0%) | 79 (19.3%) | 0.941 |
| Cardiac death | 12 (2.1%) | 6 (3.7%) | 6 (1.5%) | 0.110 |
| MI | 8 (1.4%) | 3 (1.8%) | 5 (1.3%) | 0.605 |
| Repeat revascularization | 69 (12.3%) | 8 (4.9%) | 61 (15.4%) | 0.001 |
| Urgent PCI | 49 (8.5%) | 21 (12.5%) | 28 (6.8%) | 0.033 |
*MACE (major adverse cardiac event) including cumulative cardiac death, MI, repeat revascularization, and unplanned urgent PCI. MI, myocardial infarction; PCI, percutaneous coronary intervention.
Clinical outcomes in propensity score matched population
After propensity score matching, 125 of 168 patients in the weekend group were successfully matched to an equal number of patients in the weekday group. Baseline characteristics showed no significant differences between the groups after propensity score matching (Table 5). The clinical outcomes of the matched population also showed significantly higher rate of MACE in the weekend group (12.8% vs. 4.8%, P=0.041) (Table 6).
Table 5. Baseline characteristics in propensity-score matched population.
| Parameters | All (n = 250) | Weekend group (n = 125) | Weekday group (n = 125) | P value |
|---|---|---|---|---|
| Age (yr) | 62.9 ± 13.4 | 62.64 ± 13.7 | 63.14 ± 13.12 | 0.761 |
| Sex (male) | 183 (73.2%) | 91 (72.8%) | 92 (73.6%) | 1.000 |
| Height (cm) | 164.6 ± 8.9 | 164.5 ± 9.0 | 164.7 ± 8.8 | 0.828 |
| Body weight (kg) | 67.0 ± 11.9 | 66.8 ± 11.8 | 67.2 ± 12.1 | 0.764 |
| Body mass index (kg/m2) | 24.6 ± 3.3 | 24.6 ± 3.2 | 24.7 ± 3.4 | 0.821 |
| Hypertension | 155 (62.0%) | 80 (64.0%) | 75 (60.0%) | 0.596 |
| Diabetes mellitus | 73 (29.2%) | 37 (29.6%) | 36 (28.8%) | 1.000 |
| Hyperlipidemia | 82 (32.8%) | 44 (35.2%) | 38 (30.4%) | 0.488 |
| Smoking, current | 94 (37.6%) | 51 (40.8%) | 43 (34.4%) | 0.366 |
| Previous myocardial infarction | 41 (16.4%) | 20 (16.0%) | 21 (16.8%) | 1.000 |
| Previous CABG | 8 (3.2%) | 5 (4.0%) | 3 (2.4%) | 0.687 |
| Hemoglobin (g/dL) | 14.0 ± 2.2 | 14.1 ± 1.9 | 14.0 ± 2.4 | 0.778 |
| eGFR (mL/min/m2) | 69.8 ± 31.7 | 70.0 ± 33.4 | 70.0 ± 30.1 | 0.913 |
| Total cholesterol (mg/dL) | 192.1 ± 45.8 | 193.0 ± 42.2 | 191.2 ± 49.3 | 0.766 |
| Triglyceride (mg/dL) | 124.5 ± 87.4 | 126.3 ± 87.4 | 122.7 ± 87.6 | 0.749 |
| HDL-cholesterol (mg/dL) | 44.6 ± 10.9 | 44.6 ± 11.7 | 44.6 ± 10.1 | 0.968 |
| LDL-cholesterol (mg/dL) | 101.3 ± 35.0 | 101.1 ± 34.1 | 101.5 ± 36.1 | 0.928 |
| Baseline NT-proBNP (pg/mL) | 2,072.4 ± 5,975.7 | 2,024.4 ± 5,937.7 | 2,120.4 ± 6,037.1 | 0.895 |
| Baseline hsCRP (mg/dL) | 1.0 ± 2.2 | 0.9 ± 1.9 | 1.1 ± 2.4 | 0.508 |
| CK-MB elevation* | 101 (40.4%) | 50 (40.0%) | 51 (40.8%) | 1.000 |
| Troponin-I elevation* | 174 (69.6%) | 84 (67.2%) | 90 (72.0%) | 0.440 |
| Ischemic ECG change | 0.113 | |||
| ST depression | 74 (29.6%) | 36 (28.8%) | 38 (30.4%) | |
| T-wave inversion | 60 (24.0%) | 32 (25.6%) | 28 (22.4%) | |
| Echocardiographic LV EF (%) | 56.1 ± 10.7 | 55.9 ± 11.0 | 56.2 ± 10.4 | 0.801 |
| TIMI risk score | 1.000 | |||
| Low (0-2) | 93 (37.2%) | 47 (37.6%) | 46 (36.8%) | |
| Intermediate (3-4) | 122 (48.8%) | 60 (48.0%) | 62 (49.6%) | |
| High (5-7) | 35 (14.0%) | 18 (14.4%) | 17 (13.6%) | |
| Culprit artery | 0.783 | |||
| Left main coronary artery | 5 (2.0%) | 2 (1.6%) | 3 (2.4%) | |
| Left anterior descending artery | 135 (54.0%) | 66 (52.8%) | 69 (55.2%) | |
| Left circumflex artery | 58 (23.2%) | 28 (22.4%) | 30 (24.0%) | |
| Right coronary artery | 51 (20.4%) | 29 (23.2%) | 22 (17.6%) | |
| CAD extent | 0.807 | |||
| 1 vessel disease | 88 (35.2%) | 44 (35.2%) | 44 (35.2%) | |
| 2 vessel disease | 73 (29.2%) | 35 (28.0%) | 38 (30.4%) | |
| 3 vessel disease | 89 (35.6%) | 46 (36.8%) | 43 (34.4%) | |
| Symptom-to-admission time (hr, median) | 58.8 ± 132.0 (7.0) | 50.9 ± 125.7 (5.2) | 66.7 ± 138.0 (12.0) | 0.151 |
| Admission to-PCI time (hr, median) | 43.3 ± 42.3 (29.5) | 43.6 ± 33.5 (39.2) | 43.1 ± 49.6 (24.0) | 0.915 |
| Concomitant medication | ||||
| Heparin | 239 (95.6%) | 123 (98.4%) | 116 (92.8%) | 0.065 |
| GpIIb/IIIa R antagonists | 54 (21.6%) | 29 (23.2%) | 25 (20.0%) | 0.651 |
| Tirofiban | 9 (3.6%) | 2 (1.6%) | 7 (5.6%) | 0.180 |
| Abciximab | 46 (18.4%) | 27 (21.6%) | 19 (15.2%) | 0.256 |
| Aspirin | 250 (100.0%) | 125 (100.0%) | 125 (100.0%) | 1.000 |
| Clopidogrel | 250 (100.0%) | 125 (100.0%) | 125 (100.0%) | 1.000 |
| Beta-blocker | 17 (69.6%) | 83 (66.4%) | 91 (72.8%) | 0.341 |
| ACEI | 153 (61.2%) | 79 (63.2%) | 74 (59.2%) | 0.603 |
| ARB | 40 (16.0%) | 19 (15.2%) | 21 (16.8%) | 0.864 |
| DHP CCB | 39 (15.6%) | 21 (16.8%) | 18 (14.4%) | 0.728 |
| Non-DHP CCB | 19 (7.6%) | 9 (7.2%) | 10 (8.0%) | 1.000 |
| Nitrates | 45 (18.0%) | 20 (16.0%) | 25 (20.0%) | 0.486 |
| Statin | 217 (86.8%) | 107 (85.6%) | 110 (88.0%) | 0.728 |
*>1×upper reference limit; CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NT-proBNP, N-terminal-proB-type natriuretic peptide; hsCRP, high-sensitivity C-reactive protein; CK-MB, creatine kinase-myocardial band; ECG, electrocardiography; LV EF, left ventricular ejection fraction; TIMI, thrombolysis in myocardial infarction; CAD, coronary artery disease; PCI, percutaneous coronary intervention; GpIIb/IIIa R, glycoprotein IIb/IIIa receptor; ACEI, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker; DHP CCB, dihydropyridine-calcium channel blocker.
Table 6. Thirty-day clinical outcomes in propensity-score matched population.
| Outcomes | All (n = 250) | Weekend group (n = 125) | Weekday group (n = 125) | P value |
|---|---|---|---|---|
| MACE | 22 (8.8%) | 16 (12.8%) | 6 (4.8%) | 0.041 |
| Cardiac death | 1 (0.4%) | 1 (0.8%) | 0 (0.0%) | 1.000 |
| Recurrent MI | 2 (0.8%) | 2 (1.6%) | 0 (0.0%) | 0.500 |
| Repeat revascularization | 2 (0.8%) | 2 (1.6%) | 0 (0.0%) | 0.500 |
| Urgent PCI | 20 (8.0%) | 14 (11.2%) | 6 (4.8%) | 0.064 |
| CK-MB elevation, overall | 157 (63.6%) | 85 (68.0%) | 72 (59.0%) | 0.120 |
| Peak CK-MB level | 52.0±92.4 | 62.6±95.1 | 41.5±88.8 | 0.072 |
| Troponin-I elevation, overall | 213 (86.2%) | 109 (87.2%) | 104 (52.2%) | 0.690 |
| Peak Troponin-I level | 17.3±34.5 | 23.0±43.7 | 11.6±20.5 | 0.009 |
MACE, major adverse cardiac event; MI, myocardial infarction; PCI, percutaneous coronary intervention; CK-MB, creatine kinase-myocardial band.
Survival analysis
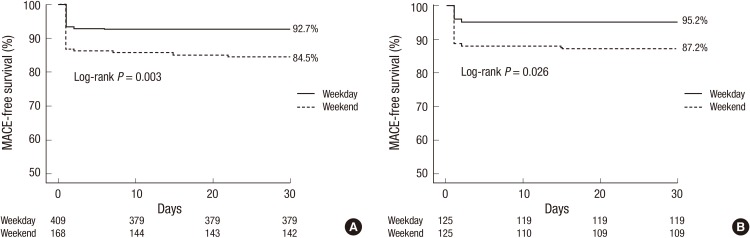
The cumulative 30-day MACE-free survival rate was significantly lower in the weekend group compared to the weekday group (92.7% vs. 84.5%, P=0.003) (Fig. 4A), as well as in the propensity-score matched population (87.2% vs. 95.2%, P=0.026) (Fig. 4B). In Cox proportional hazard regression analysis, weekend admission was associated with a 2.1-fold increased hazard for MACE (HR, 2.13; 95% CI, 1.26-3.60, P=0.005) (Table 7) after sequential adjustment of potential confounding factors including clinical characteristics, time factors such as symptom-to-admission time and admission-to-PCI, and severity factors such as Troponin-I elevation, ECG change and TIMI score. Interestingly, admission-to-PCI time appeared to be a weak, but an independent protective factor of MACE.
Fig. 4. Thirty-day MACE-free survival. (A) MACE-free survival in all patients. The cumulative 30-day MACE-free survival rate is significantly lower in patients admitted during the weekend (dotted line) compared to patients admitted during the weekday (solid line). Survival curves begin to diverge at day 1 and continue to separate throughout the 30-day follow-up period. (B) MACE-free survival in propensity-matched population. The cumulative 30-day MACE-free survival rate is significantly lower in the weekend group in the propensity score-matched population, too. MACE, major adverse cardiac events.
Table 7. Adjusted risk of 30-day MACE in sequential Cox models.
| Variable in Cox model | Hazard ratio (95% confidence interval)* | |||
|---|---|---|---|---|
| Weekend admission only | Weekend + clinical characteristics | Weekend + clinical + time factors | Weekend + clinical + time + severity factors | |
| Weekend admission | 2.13 (1.26-3.60) | 2.20 (1.29-3.73) | 3.01 (1.73-5.23) | 2.84 (1.61-5.00) |
| Age | 1.00 (0.98-1.03) | 1.01 (0.98-1.03) | 1.00 (0.98-1.03) | |
| Male sex | 1.46 (0.74-2.87) | 1.25 (0.63-2.45) | 1.14 (0.57-2.58) | |
| Hypertension | 0.68 (0.37-1.22) | 0.81 (0.44-1.46) | 0.85 (0.47-1.55) | |
| Diabetes mellitus | 0.89 (0.49-1.63) | 0.88 (0.48-1.61) | 0.89 (0.48-1.65) | |
| Hyperlipidemia | 0.79 (0.42-1.48) | 0.79 (0.42-1.49) | 0.80 (0.42-1.50) | |
| Smoking, current | 0.76 (0.40-1.45) | 0.78 (0.41-1.52) | 0.73 (0.38-1.42) | |
| Previous myocardial infarction | 1.67 (0.87-3.21) | 1.44 (0.75-2.79) | 1.66 (0.78-3.52) | |
| Previous CABG | 1.20 (0.28-5.06) | 1.33 (0.32-5.55) | 1.57 (0.35-6.93) | |
| Symptom-to-admission time | 1.00 (1.00-1.00) | 1.00 (1.00-1.00) | ||
| Admission-to-PCI time | 0.97 (0.95-0.98) | 0.97 (0.95-0.98) | ||
| Baseline Troponin-I elevation | 1.79 (0.94-3.41) | |||
| Ischemic ECG change | 0.68 (0.38-1.20) | |||
| TIMI scores | 1.01 (0.76-1.34) | |||
*The hazard ratios are derived from sequential Cox proportional-hazard models that included variables that may affect 30-day MACE.
Analysis of urgent PCI subgroup
The weekend group had higher unplanned, urgent PCI rate than the weekday group. Considering the possibility of inappropriately performed urgent PCI during the weekend period, we underwent further analysis. Of the 49 patients with urgent PCI, 57.1% had refractory angina, 20.4% had hemodynamic instability, and 22.4% had electrical instability as the reason for urgent PCI (Table 8). There were no significant differences in the reasons for urgent PCI (refractory angina, 71.4% vs. 46.4%; hemodynamic instability, 14.3% vs. 25.0%; electrical instability, 14.3% vs. 28.6%, P=0.215) between the weekend and the weekday group. More importantly, the time interval from unstable clinical condition to urgent PCI (107.4±42.2 min vs. 127.4±48.8 min, P=0.139) were not significantly different between the two groups. In addition, the time interval between unstable clinical condition and urgent PCI did not differ between MACE (+) group (n=3) and MACE (-) group (n=46) (104.0±30.3 vs. 120.0±47.7 min, P=0.661).
Table 8. Analysis of subgroup of patients with urgent PCI.
| Parameters | All (n = 49) | Weekend group (n = 21) | Weekday group (n = 28) | P value |
|---|---|---|---|---|
| Reason for urgent PCI | 0.215 | |||
| Refractory angina | 28 (57.1%) | 15 (71.4%) | 13 (46.4%) | |
| Hemodynamic instability | 10 (20.4%) | 3 (14.3%) | 7 (25.0%) | |
| Electrical instability | 11 (22.4%) | 3 (14.3%) | 8 (28.6%) | |
| Time interval from reason to urgent PCI (min, median) | 118.8 ± 46.7 (109.0) | 107.4 ± 42.2 (95.0) | 127.4 ± 48.8 (119.0) | 0.139 |
| Age | 62.1 ± 12.5 | 59.9 ± 13.5 | 63.8 ± 11.7 | 0.287 |
| Sex (male) | 38 (77.6%) | 18 (85.7%) | 20 (71.4%) | 0.311 |
| Height (cm) | 163.9 ± 9.0 | 165.0 ± 8.3 | 163.1 ± 9.6 | 0.472 |
| Body weight (kg) | 64.6 ± 12.2 | 64.8 ± 12.1 | 64.4 ± 12.4 | 0.926 |
| Body mass index (kg/m2) | 23.9 ± 3.3 | 23.6 ± 3.1 | 24.0 ± 1.8 | 0.641 |
| Hypertension | 26 (53.1%) | 8 (38.1%) | 18 (64.3%) | 0.069 |
| Diabetes mellitus | 11 (22.4%) | 5 (23.8%) | 6 (21.4%) | 0.843 |
| Hyperlipidemia | 12 (24.5%) | 5 (23.8%) | 7 (25.0%) | 0.924 |
| Smoking, current | 16 (32.7%) | 7 (33.3%) | 9 (32.1%) | 0.930 |
| Previous myocardial infarction | 12 (24.5%) | 6 (28.6%) | 6 (21.4%) | 0.565 |
| Previous CABG | 2 (4.1%) | 1 (4.8%) | 1 (3.6%) | 1.000 |
| Hemoglobin, g/dL | 13.9 ± 2.0 | 13.6 ± 2.3 | 14.0 ± 1.8 | 0.509 |
| eGFR (mL/min/m2) | 63.0 ± 30.2 | 70.3 ± 36.1 | 57.7 ± 24.1 | 0.148 |
| Total cholesterol (mg/dL) | 200.5 ± 43.4 | 191.3 ± 41.6 | 207.3 ± 44.2 | 0.206 |
| Triglyceride (mg/dL) | 121.2 ± 84.5 | 143.4 ± 114.3 | 105.6 ± 52.0 | 0.137 |
| HDL-cholesterol (mg/dL) | 42.4 ± 7.2 | 41.4 ± 5.8 | 43.0 ± 8.1 | 0.485 |
| LDL-cholesterol (mg/dL) | 101.1 ± 36.7 | 100.4 ± 37.8 | 101.6 ± 36.8 | 0.918 |
| NT-proBNP (pg/mL) | 2,489.4 ± 6,157.8 | 1,560.2 ± 3,617.1 | 3,168.5 ± 7,495.4 | 0.393 |
| hsCRP (mg/dL) | 1.3 ± 3.4 | 2.4 ± 5.1 | 0.6 ± 0.6 | 0.128 |
| CK-MB elevation* | 26 (53.1%) | 9 (42.9%) | 17 (60.7%) | 0.215 |
| Troponin-I elevation* | 36 (73.5%) | 16 (76.2%) | 20 (71.4%) | 0.709 |
| Ischemic ECG change | 0.480 | |||
| ST depression | 19 (38.8%) | 10 (47.6%) | 9 (32.1%) | |
| T-wave inversion | 4 (8.2%) | 1 (4.8%) | 3 (10.7%) | |
| Echocardiographic LV EF (%) | 54.6 ± 10.3 | 55.9 ± 9.2 | 53.6 ± 11.3 | 0.502 |
| TIMI risk score | 0.409 | |||
| Low (0-2) | 17 (34.7%) | 6 (28.6%) | 11 (39.3%) | |
| Intermediate (3-4) | 26 (53.1%) | 11 (52.4%) | 15 (53.6%) | |
| High (5-7) | 6 (12.2%) | 4 (19.0%) | 2 (7.1%) | |
| Culprit artery | 0.310 | |||
| Left main coronary artery | 2 (4.1%) | 1 (4.8%) | 1 (3.6%) | |
| Left anterior descending artery | 23 (46.9%) | 10 (47.6%) | 13 (46.4%) | |
| Left circumflex artery | 13 (26.5%) | 8 (38.1%) | 5 (17.9%) | |
| Right coronary artery | 10 (20.4%) | 2 (9.5%) | 8 (28.6%) | |
| CAD extent | 0.607 | |||
| 1 vessel disease | 22 (44.9%) | 8 (38.1%) | 14 (50.0%) | |
| 2 vessel disease | 11 (22.4%) | 6 (28.6%) | 5 (17.9%) | |
| 3 vessel disease | 16 (32.7%) | 7 (33.3%) | 9 (32.1%) | |
| Symptom-to-admission time (hr, median) | 37.3 ± 116.2 (5.5) | 32.2 ± 103.3 (5.2) | 41.1 ± 126.8 (6.0) | 0.793 |
| Admission-to-PCI time (hr, median) | 7.6 ± 7.6 (4.8) | 7.2 ± 8.6 (4.4) | 7.9 ± 7.0 (6.6) | 0.742 |
| Concomitant medications | ||||
| Heparin | 43 (87.8%) | 19 (90.5%) | 24 (85.7%) | 0.688 |
| GpIIb/IIIa R antagonists | 17 (34.7%) | 8 (38.1%) | 9 (32.1%) | 0.665 |
| Tirofiban | 2 (4.1%) | 0 (0.0%) | 2 (7.1%) | 0.500 |
| Abciximab | 15 (30.6%) | 8 (38.1%) | 7 (25.0%) | 0.325 |
| Aspirin | 49 (100%) | 21 (100%) | 28 (100%) | 1.000 |
| Clopidogrel | 49 (100%) | 21 (100%) | 28 (100%) | 1.000 |
| Beta-blocker | 32 (65.3%) | 17 (81.0%) | 15 (53.6%) | 0.070 |
| ACEI/ARB | 33 (67.3%) | 17 (81.0%) | 16 (57.1%) | 0.079 |
| Statin | 37 (75.5%) | 15 (71.4%) | 22 (78.6%) | 0.565 |
*>1×upper reference limit; PCI, percutaneous coronary intervention; CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NT-proBNP, N-terminal-proB-type natriuretic peptide; hsCRP, high-sensitivity C-reactive protein; CK-MB, creatine kinase-myocardial band; ECG, electrocardiography; LV EF, left ventricle ejection fraction; TIMI, thrombolysis in myocardial infarction; CAD, coronary artery disease; GpIIb/IIIa R, glycoprotein IIb/IIIa receptor; ACEI, angiotensin-converting-enzyme inhibitor; ARB, angiotensin receptor blocker.
DISCUSSION
This study shows that admission on weekends has an adverse influence on clinical outcomes in patients with NSTE-ACS. Weekend admission was associated with a higher incidence of 30-day MACE, which maintained after adjusting the difference in baseline characteristics with propensity score matching and Cox proportional hazard model regression analysis. In addition, there was a trend of gradual increase of MACE from Monday toward the weekend peaking on Saturday with similar patterns in cardiac biomarker elevation and time delay to PCI. In subgroup of patients with urgent PCI, the causes of and the time delay to the urgent PCI were not significantly different between the two groups.
In this study, the patients in the weekend group had higher cardiac markers than those in the weekday group indicating they are a "riskier" patients group. Cram et al. (8) showed that patients who were admitted during the weekend were older and had higher in-hospital mortality. Ryan et al. (10) also showed that patients admitted during the weekend tended to have high-risk characteristics including older age, more prior CABG and more positive cardiac markers. Consistent with previous studies, our study also showed that patients in the weekend group had more high-risk characteristics.
MACE occurred more often in the weekend group in the present study. Previously, the MIDAS study showed that patients with acute MI admitted during the weekend had significantly higher 30-day mortality compared to patients admitted during the weekday, supporting the results of our study (5). However, the study population comprised all acute MI patients without differentiating between STEMI and NSTE-ACS. Cram et al. (8) showed that risk-adjusted mortality was higher in patients with ACS admitted during weekend compared patients admitted during weekday. In contrast, Ryan et al. (10) showed in their registry that weekend admission did not have an adverse effect on clinical outcome in patients with NSTE-ACS. However, in that registry, only high-risk patients who were admitted to the ER within 24 hr of symptoms onset were enrolled. Another trial revealed that next-working day intervention did not worsen cardiac event compared to immediate intervention in patients with NSTE-ACS (17). In the ABOARD trial, immediate intervention with 70 min of delay did not show significant difference in the composite of death, MI, or urgent revascularization at 1-month follow-up in comparison with the next-working day intervention with 21 hr of delay. However, there were some differences between the ABOARD trial and our study. First, the two comparator groups in our study were determined by the admission date and time of the patients not by the delay in intervention. Second, the time delays to intervention of both the weekday group (mean admission to PCI time, 35.2 hr) and the weekend group (45.3 hr) in our study were different from those of ABOARD trial. Third, the proportion of patients who underwent PCI within 2 hr of admission in our study, who could be classified as immediate intervention group in ABOARD trial, was quite low (3.5%) and showed no significant difference between the weekend and the weekday group (3.0% vs. 3.7%, P=0.680, data not shown). We think that the differences in the group classification and the study population may be responsible for the discrepancies between the two studies. In addition, in another study with acute MI patients showing no significant difference between the weekend and weekday group (18), only highly-selected patients with early onset of MI were enrolled. Overall, in previous studies with positive results, the population comprised all acute MI or ACS patients without differentiating between NSTEMI and STEMI, therefore the result is not easily applicable to the current practice guidelines for UA/NSTEMI (19) or STEMI (20). The present study enrolled NSTE-ACS patients only, which was more consistent with the practice guidelines, and revealed that patients with NSTE-ACS in the weekend had a significantly higher rate of MACE, even after adjustment for differences in baseline characteristics.
In order to find factors contributing to the worse outcome in the weekend group, we first compared the daily-distribution pattern of the most possible contributing factors for MACE. Second, we conducted Cox proportional hazard analysis by putting possible contributing factors step-by-step. In the analysis of daily-distribution pattern, baseline cardiac enzyme elevation and admission-to-PCI time showed similar pattern with that of MACE. However, Cox proportional hazard model analysis showed that the worse outcome in the weekend group was significant even after adjusting with those two factors. Moreover, it revealed the admission-to-PCI time as an independent predictor of MACE, in contrast to the result of baseline characteristics and daily-distribution pattern. This discrepancy was probably due to the relatively short admission-to-PCI time in patients with urgent revascularization which was one of the main components of the MACE. Therefore, we can speculate that there might be other, hidden contributing factors which were not measured in the present study. Finally, among other possible contributing factors, time delay from development of patient's instability to urgent PCI was not significantly different in the two groups, either.
One of the reasons why weekend admission was associated with worse outcome is that more severe patients visit hospitals during weekends, because of the difference in accessibility to the hospital between the weekend and the weekdays. Two previous studies showed that patients admitted during the weekend tended to be older and have more positive cardiac markers (8, 10). Another study reported that patient presented with more complex and critical conditions on the weekend than on the weekdays (21). Further prospective study with much detailed variable setting on baseline and therapeutic characteristics would be needed in order to find the hidden contributing factors.
This study has several limitations. The main limitation of this study is the relatively small sample size and enrollment from a single study center during a 4-yr period, although the reason for enrolling from a single center during a relatively short period was to avoid inter-institutional differences in detailed technique of PCI and choices among various anti-thrombotic agents. Second, the enrollment was confined to patients who underwent PCI, excluding patients treated medically or with CABG. Although routine invasive treatment is highly recommended for most patients with NSTE-ACS (22, 23, 24), this can be an important limitation of our study. Third, we used composite endpoint of MACE as the primary endpoint. Hence, large portion of the MACE comprised of urgent revascularization, which could be classified as 'soft' endpoint. Finally, this study was not a prospective study, rather a retrospective analysis. Therefore, unknown confounding factors could have affected the results. Further large-scale prospective analyses would be required to assess the effect of weekend admission on clinical outcomes in patients with NSTE-ACS.
In conclusion, patients with NSTE-ACS admitted during the weekends have an increased MACE rate. The similarity of daily-distribution pattern of baseline cardiac enzyme elevation and admission-to-PCI with that of MACE suggested those factors as underlying contributing factors to worse outcome with the weekend admission. However, weekend admission still remains an independent risk factor of MACE, suggesting the possibility of hidden, unmeasured contributing factor.
Footnotes
The authors have no conflicts of interest to disclose.
Guarantor of integrity of the study: Cho YS. Study concepts and coordination: Cho YS. Literature research: Kim HJ, Cho YS. Design of ethical issues: Kim HJ, Cho YS. Data acquisition and interpretation: Cho YS, Park JJ, Oh IY, Yoon CH, Suh JW, Youn TJ, Chae IH, Choi DJ. Data review and analysis: Kim HJ, Cho YS, Kang J. Manuscript preparation: Kim HJ, Kim KI, Cho YS. Statistical analysis: Kim HJ, Cho YS, Kang J, Park JJ. Manuscript editing: Kim HJ, Cho YS, Park JJ. Manuscript revision: Kim HJ, Cho YS, Park JJ. Manuscript approval: all authors.
References
- 1.Angeja BG, Gibson CM, Chin R, Frederick PD, Every NR, Ross AM, Stone GW, Barron HV Participants in the National Registry of Myocardial Infarction 2-3. Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol. 2002;89:1156–1161. doi: 10.1016/s0002-9149(02)02296-8. [DOI] [PubMed] [Google Scholar]
- 2.Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, Caso P, Dudek D, Gielen S, Huber K, et al. ESC Committee for Practice Guidelines. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: the Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2999–3054. doi: 10.1093/eurheartj/ehr236. [DOI] [PubMed] [Google Scholar]
- 3.Jneid H, Anderson JL, Wright RS, Adams CD, Bridges CR, Casey DE, Jr, Ettinger SM, Fesmire FM, Ganiats TG, Lincoff AM, et al. American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2012;126:875–910. doi: 10.1161/CIR.0b013e318256f1e0. [DOI] [PubMed] [Google Scholar]
- 4.Yui Y, Hirayama A, Nonogi H, Kimura K, Kodama K, Hosoda S, Kawai C. Unstable angina and non-ST elevation acute coronary syndrome: epidemiology and current management in Japan (Japan Multicenter Investigation for Cardiovascular Disease-D (JMIC-D) Committee) Circ J. 2007;71:1335–1347. doi: 10.1253/circj.71.1335. [DOI] [PubMed] [Google Scholar]
- 5.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 6.Magid DJ, Wang Y, Herrin J, McNamara RL, Bradley EH, Curtis JP, Pollack CV, Jr, French WJ, Blaney ME, Krumholz HM. Relationship between time of day, day of week, timeliness of reperfusion, and in-hospital mortality for patients with acute ST-segment elevation myocardial infarction. JAMA. 2005;294:803–812. doi: 10.1001/jama.294.7.803. [DOI] [PubMed] [Google Scholar]
- 7.Garot P, Juliard JM, Benamer H, Steg PG. Are the results of primary percutaneous transluminal coronary angioplasty for acute myocardial infarction different during the "off" hours? Am J Cardiol. 1997;79:1527–1529. doi: 10.1016/s0002-9149(97)00186-0. [DOI] [PubMed] [Google Scholar]
- 8.Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117:151–157. doi: 10.1016/j.amjmed.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 9.Matsui K, Kojima S, Sakamoto T, Ishihara M, Kimura K, Miyazaki S, Yamagishi M, Tei C, Hiraoka H, Sonoda M, et al. Weekend onset of acute myocardial infarction does not have a negative impact on outcome in Japan. Circ J. 2007;71:1841–1844. doi: 10.1253/circj.71.1841. [DOI] [PubMed] [Google Scholar]
- 10.Ryan JW, Peterson ED, Chen AY, Roe MT, Ohman EM, Cannon CP, Berger PB, Saucedo JF, DeLong ER, Normand SL, et al. CRUSADE Investigators. Optimal timing of intervention in non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) Registry. Circulation. 2005;112:3049–3057. doi: 10.1161/CIRCULATIONAHA.105.582346. [DOI] [PubMed] [Google Scholar]
- 11.Hong JS, Kang HC, Lee SH. Comparison of case fatality rates for acute myocardial infarction in weekday vs weekend admissions in South Korea. Circ J. 2010;74:496–502. doi: 10.1253/circj.cj-09-0678. [DOI] [PubMed] [Google Scholar]
- 12.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, 2nd, Fesmire FM, Hochman JS, Levin TN, et al. American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction); American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions; Society of Thoracic Surgeons; American Association of Cardiovascular and Pulmonary Rehabilitation; Society for Academic Emergency Medicine. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50:e1–e157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, Thygesen K, Alpert JS, White HD, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33:2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 14.Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernández-Avilés F, Fox KA, Hasdai D, Ohman EM, Wallentin L, et al. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1598–1660. doi: 10.1093/eurheartj/ehm161. [DOI] [PubMed] [Google Scholar]
- 15.Antman EM, Cohen M, Bernink PJ, McCabe CH, Horacek T, Papuchis G, Mautner B, Corbalan R, Radley D, Braunwald E. The TIMI risk score for unstable angina/non-ST elevation MI: A method for prognostication and therapeutic decision making. JAMA. 2000;284:835–842. doi: 10.1001/jama.284.7.835. [DOI] [PubMed] [Google Scholar]
- 16.Sabatine MS, Antman EM. The thrombolysis in myocardial infarction risk score in unstable angina/non-ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2003;41:89s–95s. doi: 10.1016/s0735-1097(02)03019-x. [DOI] [PubMed] [Google Scholar]
- 17.Montalescot G, Cayla G, Collet JP, Elhadad S, Beygui F, Le Breton H, Choussat R, Leclercq F, Silvain J, Duclos F, et al. ABOARD Investigators. Immediate vs delayed intervention for acute coronary syndromes: a randomized clinical trial. JAMA. 2009;302:947–954. doi: 10.1001/jama.2009.1267. [DOI] [PubMed] [Google Scholar]
- 18.Malmberg K, Yusuf S, Gerstein HC, Brown J, Zhao F, Hunt D, Piegas L, Calvin J, Keltai M, Budaj A. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) Registry. Circulation. 2000;102:1014–1019. doi: 10.1161/01.cir.102.9.1014. [DOI] [PubMed] [Google Scholar]
- 19.Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Jr, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff AM, et al. 2011 ACCF/AHA Focused Update of the Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction (Updating the 2007 Guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011;123:2022–2060. doi: 10.1161/CIR.0b013e31820f2f3e. [DOI] [PubMed] [Google Scholar]
- 20.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, Chambers CE, Ellis SG, Guyton RA, Hollenberg SM, et al. 2011 ACCF/AHA/SCAI Guideline for Per cutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2011;124:e574–e651. doi: 10.1161/CIR.0b013e31823ba622. [DOI] [PubMed] [Google Scholar]
- 21.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 22.Fox KA, Poole-Wilson P, Clayton TC, Henderson RA, Shaw TR, Wheatley DJ, Knight R, Pocock SJ. 5-year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomised trial. Lancet. 2005;366:914–920. doi: 10.1016/S0140-6736(05)67222-4. [DOI] [PubMed] [Google Scholar]
- 23.Damman P, Hirsch A, Windhausen F, Tijssen JG, de Winter RJ ICTUS Investigators. 5-year clinical outcomes in the ICTUS (Invasive versus Conservative Treatment in Unstable coronary Syndromes) trial a randomized comparison of an early invasive versus selective invasive management in patients with non-ST-segment elevation acute coronary syndrome. J Am Coll Cardiol. 2010;55:858–864. doi: 10.1016/j.jacc.2009.11.026. [DOI] [PubMed] [Google Scholar]
- 24.Fox KA, Clayton TC, Damman P, Pocock SJ, de Winter RJ, Tijssen JG, Lagerqvist B, Wallentin L FIR Collaboration. Long-term outcome of a routine versus selective invasive strategy in patients with non-ST-segment elevation acute coronary syndrome a meta-analysis of individual patient data. J Am Coll Cardiol. 2010;55:2435–2445. doi: 10.1016/j.jacc.2010.03.007. [DOI] [PubMed] [Google Scholar]