Abstract
Background:
The incidence of difficult intubation in patients undergoing general anaesthesia is estimated to be approximately 1-18% whereas that of failure to intubate is 0.05-0.35%.1,2,3 Various methods have been used for prediction of difficult laryngoscopy. Although, upper lip bite has been shown to be a promising test in its introductory article, repeated validation in various populations is required for any test to be accepted as a routine test. We have compared upper lip bite test (ULBT), modified Mallampati test (MMC) and thyromental distance (TMD) individually and in various combinations to verify which of these predictor tests are significantly associated with difficult glottic exposure.
Methods:
After obtaining institutional ethics committee approval, 402 ASA I and II adult patients undergoing elective surgical procedures requiring endotracheal intubation were included. All the three test were performed in all the patients preoperatively and their glottic exposure was recorded by Cormack-Lehane classification during intubation. Sensitivity, specificity, positive predictive value and negative predictive value were used for comparison.
Results:
In our study, the incidence of difficult laryngoscopy was 11.4% and failure to intubate 0.49%. None of the three are a suitable predictive test when used alone. Combination of tests added incremental diagnostic value.
Conclusion:
We conclude that all three screening tests for difficult intubation have only poor to moderate discriminative power when used alone. Combinations of individual tests add some incremental diagnostic value.
Keywords: Difficult airway, Mallampati classification, thyromental distance, upper lip bite test
Introduction
Airway management, including the ability to intubate, is a basic skill required in the repertoire of any doctor especially in a setting of primary care center at remote locations. Inability to maintain a patent airway results in inadequate ventilation and oxygenation leading to hypoxic brain damage and death. The incidence of difficult intubation in surgical patients undergoing general anesthesia is estimated to be approximately 1–18%, whereas that of failure to intubate is 0.05–0.35%.[1,2,3] Various methods have been used for prediction of difficult laryngoscopy comparing either individual parameters or by using scoring systems.[4,5,6,7] Although, upper lip bite has been shown to be a promising test in its introductory article,[5] repeated validation in various populations is required for any test to be accepted as a routine test.
In our study, the two most commonly used tests, namely “Modified Mallampati classification” (MMC) and “Thyromental distance” (TMD) are compared with “Upper lip bite test” (ULBT), both individually as well as in combination, in an attempt to verify which of these predictor tests are significantly associated with difficult glottic exposure.
Materials and Methods
After obtaining institutional ethics committee approval and written informed consent from 402 patients (sample size calculated according to Raosoft sample size calculator with 95% confidence limits), a prospective, comparative, double-blind study of three predictive tests-ULBT, MMC, TMD for prediction of ease of laryngoscopy and intubation was conducted.
American Society of Anaesthesiologists (ASA) I and II patients above 18 years undergoing elective surgical procedures requiring endotracheal intubation were included in the study. Patients with a history of previous surgery, burns or trauma, tumors/mass in the airways or the cranial, cervical and facial regions, patients with restricted mobility of the neck and mandible (rheumatoid arthritis, cervical disc disorders, or temporomandibular joint disorders), edentulous patients, pregnant patients, and body mass index (BMI) >26 kg/m2 were excluded from the study.
All patients were subjected to a thorough preoperative airway assessment a day prior to surgery. All the three predictive tests were assessed by a single anesthetist to avoid inter-observer bias.
ULBT tests the range of mandibular movement and dental morphology. Patients were asked to bite their upper lip with lower incisors as high as they could, in sitting position with head in neutral position. The anesthetist also demonstrated the test to the patient, thereby enabling patient compliance as instructed by the original authors.[5] ULBT was assessed-Class I: Lower incisors can bite the upper lip above the vermilion line. Class II: Lower incisors can bite the upper lip below the vermilion line. Class III: Lower incisors cannot bite the upper lip. Classes I and II were considered to be predictive of easy intubation and class III of difficult intubation.
The MMC test was done with the aid of a torch, with the patients in sitting position, head in neutral position, the mouth wide open with the tongue fully protruding and without phonating “ah.”[8,9,10] Classification was assigned into four classes.[11] Class I: Soft palate, fauces, entire uvula, anterior and posterior tonsillar pillars visible, Class II: Soft palate, fauces, uvula visible. Class III: Soft palate and base of uvula visible. Class IV: Only hard palate visible. Classes I and II were considered predictive of easy intubation whereas classes III and IV were considered predictive of difficult intubations.
TMD is defined as the distance from the mentum to the superior notch on the thyroid cartilage when the patient's neck is fully extended. It was measured with a ruler in the upright sitting position.[8,12,13] A TMD less than 6 cm was considered to be predictive of difficult intubation.[4,14] To maintain blinding, only one anesthetist assessed the predictive tests while other blinded anesthetists performed the patients’ intubation.
On the day of surgery, after confirming the nil per oral status, monitors were attached (electrocardiogram, automated blood pressure, pulse oximetry, end tidal carbon dioxide). Lactated ringer was started at 2 ml/kg/hr through a 20G intravenous cannula. Patients were sedated 5 minutes prior to induction with midazolam (0.05 mg/kg) and fentanyl (2 mcg/kg) and pre-oxygenation for 3–4 minutes with 100% oxygen.
General anesthesia was induced with thiopentone sodium (5 mg/kg) and vecuronium (0.1 mg/kg) and the patient was ventilated with oxygen, nitrous oxide (50%), and isoflurane (0.6–0.8%) for 3 minutes, followed by only oxygen and isoflurane for another one minute. At the end of 4 minutes, the head of the patient was placed in the optimum sniffing position, (neck flexed on the chest by head elevation with a head ring and head extension at atlanto-occipital joint by tilting the head backward with the hand of the operator to bring oral, pharyngeal, and laryngeal axes in line for proper glottis visualization).
After fully opening the mouth, laryngoscopy was done with Macintosh 3 blade by an anesthesiologist with minimum one year experience. Laryngoscopic view was graded without the use of external laryngeal maneuver. Cormack-Lehane (CL) grading system was used to determine the glottis view.[15] Grade 1: Most of the glottis visible. Grade 2: Only the posterior part of glottis and epiglottis visible. Grade 3: Only epiglottis visible. Grade 4: Not even epiglottis seen. CL grade 1 and 2 were considered easy laryngoscopy, whereas CL grade 3 and 4 difficult laryngoscopy. The patients were intubated with sizes 7, 7.5 cuffed endotracheal tubes for females and sizes 8.5, 9 tubes for males. In the event of CL grade 3 or 4, intubation with external laryngeal maneuver was tried. In the event of an unsuccessful attempt, intubation was taken over by the senior most anesthetist in the operation theater (OT). Proseal laryngeal mask airway was kept as standby in the event of failure to intubate.
All collected data was entered in an excel worksheet. Statistics were analyzed with Statistical Package for the Social Sciences (SPSS) 16.0 software. Statistical tools in excel sheet were used. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated and used for comparison.
Results
The youngest patient in our study was 18 years old and oldest was 80 years old. The mean age was 41.89 years with standard deviation of 14.356. Male and female patients were 108 and 294, respectively. This female preponderance can be explained by the inclusion of gynecological patients and general surgery patients posted for mastectomy. The mean BMI in our study was 22.1689 with a standard deviation of 1.63.
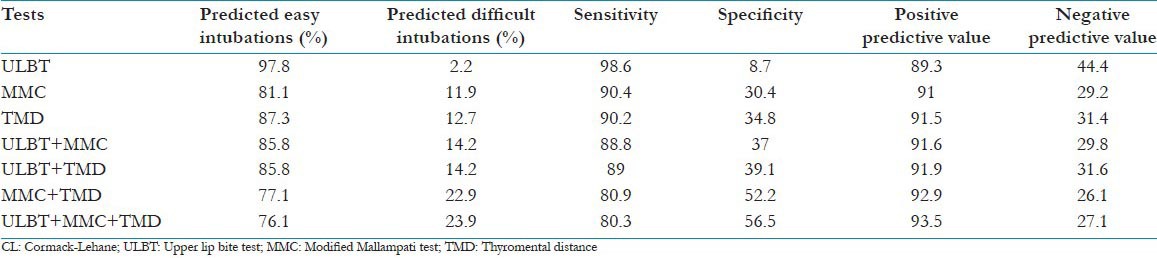
The airway predictive indices were studied independently, in combination of two and all three tests together. The sensitivity, specificity, PPV and NPVs calculated for the groups are as shown in Table 1.
Table 1.
Predictive values of upper lip bite test, modified Mallampati classification and thyromental distance and their combinations to predict the occurrence of CL grade 3 or 4 laryngoscopic view
In our study, 46 out of 402 patients were difficult laryngoscopies and all but two could easily be intubated with the help of the external laryngeal maneuver, indicating that difficult laryngoscopy need not always be a difficult intubation. [Table 2]
Table 2.
Cormack-Lehane classification of glottic exposure
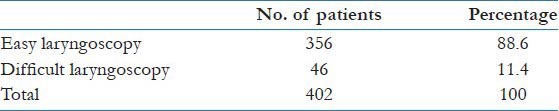
Only two patients could not be intubated despite repeated attempts by seniormost personnel and had to be ventilated with proseal laryngeal mask airway. Of these two cases, only one was correctly predicted and the other one was unanticipated. No incidence of desaturation was encountered in our study.
Although ULBT is not a suitable predictive test for difficult intubation when used alone, its combination with either modified Mallampati classification or thyromental distance has superior sensitivity, specificity, PPV, and NPV for prediction of difficult laryngoscopy and intubation. The combination of all three tests produced the highest specificity with an acceptable sensitivity, a NPV at the lower range of all tests and a PPV in the same range as other tests. This shows that a combination of individual tests add some incremental diagnostic value and is best suited for prediction of difficult intubation.
Discussion
Difficult tracheal intubation accounted for approximately 17% of adverse respiratory events in an American Society of Anesthesiologists Closed Claims analysis. In 85% of these cases, the outcome was either death or hypoxic brain damage.[16] Difficult tracheal intubation also increases the incidence of critical nonfatal events such as desaturation, hypertension, esophageal intubation, upper airway and dental trauma, postponing the surgery, increased hospital stay, and an increased intensive care unit admission. Pre-operative prediction of difficult airway allows sufficient time for formulation of a proper plan for difficult airway.
Various tests have been used in the past for prediction of difficult laryngoscopy and intubation. Unanticipated difficult intubations are probably the result of a lack of accurate predictive tests for difficult intubation. In addition, the ability of the person performing the intubation cannot be easily incorporated into a standardized assessment. Eighteen colleagues with clinical experience ranging from 1 to 35 years performed the intubations in our study. In our view, this heterogeneity is essential in validation of a clinical tool designed as a screening method for routine use.
Although unanticipated difficult intubation has been the subject of many studies, a wide variation has been reported in the sensitivity of different tests used for prediction of this problem. The ideal method for preoperative airway assessment should have high sensitivity and specificity and result in minimal false positive and false negative predictions.
Our study shows a good sensitivity (98.6%) for ULBT when used alone but a very low specificity 8.7%. Sensitivity and specificity being dependent on each other, an increase in one of them usually results in a decrease in the other. As compared to ULBT used alone, MMC or TMD is a better predictive test. Combination of tests further increases their diagnostic value.
In 2005, Eberhart et al. assessed ULBT in a sample size of 1,425 and could not reproduce the high predictive properties of the ULBT as reported by the original authors.[17] They found MMC to be a better predictor than ULBT but concluded that both ULBT and MMC were poor predictors of difficult laryngoscopy and intubation as single screening tests.
Cattano et al. in the Italian population concluded that the Mallampati score by itself is insufficient for predicting difficult endotracheal intubation.[2] Huh et al. in univariate analysis found MMC to be inferior to TMD as a predictor test but on comparison with other tests in combinations, found combination of tests to add an incremental diagnostic value.[18] Krobbuaban et al. found a Mallampati class 3 or 4 was a major factor for predicting difficult laryngoscopy but interestingly, found no correlation between TMD <6.5 cm and difficult laryngoscopy.[19]
The original study by Khan et al. and a subsequent study in 2011 found ULBT to be a very good predictor as compared to other indices as a single screening test.[5,20] They found that a higher ULBT score had a strong positive correlation to higher CL grade of laryngoscopic view. But unlike in our study, the pre-operative airway assessment was done by 2 evaluators, introducing inter-observer bias. Hester et al. in a study published in 2007 found ULBT to be a superior predictor test as compared to MMC.[21] Safavi et al. reported that ULBT when used alone is a better predictor of difficult laryngoscopy than MMC as a single test or in combination with ULBT as a bedside screening test.[22] Chohedri et al. found ULBT to have a higher specificity and accuracy than MMC and TMD but found TMD to be the most sensitive test as compared to ULBT and MMT for prediction of difficult laryngoscopy.[23] Gupta et al. in a study in the Kashmiri population, simply arranged the predictor tests in an order based on the strength of association with difficult intubation instead of trying to find “ideal” predictor(s), scores, or models.[24] They found that poor Mallampati class and a TMD <6 cm are significantly associated with difficult intubation.
Shiga et al. in their meta-analysis found MMC to have a higher discriminative power than TMD as predictors of difficult intubation. Combination of these two tests further increased the discriminative power.[14] They also showed that the positive likelihood ratio of TMD improved from 3.4 to 4.1 when a stricter cut-off criterion (<6.0 cm) was applied.
Although other studies have compared ULBT with TMD, none have studied their combined predictive value.
The increasing specificity of MMC + TMD demonstrates a greater diagnostic value of this combination of tests. Frek et al. also reported a high sensitivity and specificity of 81.2% and 97.8%, respectively for the this combination of tests.[3]
Some of the above studies have included the original Mallampati test with only three classes in their study, whereas we have included the Samsoon and Young's modified Mallampati test, which has been found to have a better predictive value.[25,26]
In our study, the combination of all three tests has the highest specificity for prediction of difficult intubation. Since no single independent criteria or combination of criteria can uniformly predict all cases of difficult glottic exposure, we must acknowledge the dynamic relationship between sensitivity and specificity. Application of multiple preoperative predictor tests, for anticipating difficult airway, can reduce the frequency of both unanticipated failure to visualize laryngeal structures as well as potentially unnecessary interventions related to over-prediction of airway difficulty.
Some of the challenges that we faced during our study are as follows. In spite of demonstrating ULBT to the patients during airway examination, we found that there was indeed a difficulty in following the instructions by the patients who got flustered by their repeated attempts to get the correct position.
Another limitation of this test is that it is not appropriate for edentulous patients, who had to be excluded from the study. Also the review of dental literature shows that there are significant racial variation in morphology of human mandible and maxillary bones.[22] Tham et al. confirmed that prevention of phonation while grading MMC was a critical factor in accomplishing a reliable score.[10] Almost 25% of patients phonate spontaneously, leading to inter-observer variability.[27] Also, there are many sources of error in measurement techniques for TMD such as digital preference, rounding off to closest number, different landmarks, different head positions leading to inter-observer variation.[25] All observations in our study were done by one anesthetist to avoid inter-observer variability.[8,12,13] Various studies have included numerous cut-off values of thyromental distance ranging from 4–7 cm for prediction of difficult intubation.[1,2,19,28,29] In our study, a TMD less than 6 cm was considered to be predictive of difficult intubation as determined by the original article by Patil et al. and a meta-analysis by Shiga et al.[4,14] It is essential that clinicians understand the limitations of all predictive tests and remain prepared to follow appropriate algorithms to avoid morbidity and mortality due to mismanagement of difficult airway.[30]
Variations in the incidence of difficult laryngoscopy have been attributed to different factors such as different anthropomorphic features among populations, lack of uniformity in describing laryngeal views, use of external laryngeal maneuver, head position, degree of muscle relaxation, and type or size of laryngoscope blade.[22]
Research has mainly been directed at predicting difficult laryngoscopy as it is the most common cause of difficult intubation. Although difficult laryngoscopy is a major determinant of difficult intubation, it is not synonymous with difficult intubation. In many clinical situations the application of external laryngeal pressure facilitates a laryngoscopic view and intubation can be performed without difficulty. In addition, direct laryngoscopy is not the only way to secure and maintain an airway, although it is the most common means of facilitating intubation.[18]
Wilson stated, “No test is likely to be perfect, therefore, it remains essential that every anesthetist must be trained and equipped to deal with the now much less common, unexpected failure to intubate.”[14] We realized that attempts at prediction are much less important than knowing what to do when difficulty is encountered.
In conclusion, currently available screening tests for difficult intubation have only poor to moderate discriminative power when used alone. Combinations of individual tests add some incremental diagnostic value. However, the clinical value of these bedside screening tests for predicting difficult intubation remains inadequate. Our search for the “Holy Grail” of a predictive test for difficult intubation continues.
In this scenario, our efforts must not only be directed at finding that elusive predictor test but must be intensified towards training of physicians in appropriate algorithms as per the Difficult Airway Society guidelines so as to prevent any morbidity and mortality due to mismanaged difficult airway.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Tse JC, Rimm EB, Hussain A. Predicting difficult endotracheal intubation in surgical patients scheduled for general anesthesia: A prospective blind study. Anesth Analg. 1995;81:254–8. doi: 10.1097/00000539-199508000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Cattano D, Panicucci E, Paolicchi A, Forfori F, Giunta F, Hagberg C. Risk factors assessment of the difficult airway: An Italian survey of 1956 patients. Anesth Analg. 2004;99:1774–9. doi: 10.1213/01.ANE.0000136772.38754.01. [DOI] [PubMed] [Google Scholar]
- 3.Frerk CM. Predicting difficult intubation. Anaesthesia. 1991;46:1005–8. doi: 10.1111/j.1365-2044.1991.tb09909.x. [DOI] [PubMed] [Google Scholar]
- 4.Patil VU, Stehling LC. Predicting the difficulty of intubation utilizing an intubation guide. Anaesthesiology. 1983;10:32. [Google Scholar]
- 5.Khan ZH, Kashfi A, Ebrahimkhani E. A comparison of the upper lip bite test (a Simple New Technique) with modified mallampati classification in predicting difficulty in endotracheal intubation: A prospective blinded study. Anesth Analg. 2003;96:595–9. doi: 10.1097/00000539-200302000-00053. [DOI] [PubMed] [Google Scholar]
- 6.el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: Predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197–204. doi: 10.1097/00000539-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Arné J, Descoins P, Fusciardi J, Ingrand P, Ferrier B, Boudigues D, et al. Preoperative assessment for difficult intubation in general and ENT surgery: Predictive value of a clinical multivariate risk index. Br J Anaesth. 1998;80:140–6. doi: 10.1093/bja/80.2.140. [DOI] [PubMed] [Google Scholar]
- 8.Lewis M, Keramati S, Benumof JL, Berry CC. What is the best way to determine oropharyngeal classification and mandibular space length to predict difficult laryngoscopy? Anesthesiology. 1994;81:69–75. doi: 10.1097/00000542-199407000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Oates JD, Macleod AD, Oates PD, Pearsall FJ, Howie JC, Murray GD. Comparison of two methods for predicting difficult intubation. Br J Anaesth. 1991;66:305–9. doi: 10.1093/bja/66.3.305. [DOI] [PubMed] [Google Scholar]
- 10.Tham EJ, Gildersleve CD, Sanders LD, Mapleson WW, Vaughan RS. Effects of posture, phonation and observer on Mallampati classification. Br J Anaesth. 1992;68:32–8. doi: 10.1093/bja/68.1.32. [DOI] [PubMed] [Google Scholar]
- 11.Samsoon GL, Young JR. Difficult tracheal intubation: A retrospective study. Anaesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 12.Kiser M, Wakim JA, Hill L. Accuracy of fingerbreadth measurements for thyromental distance estimates: A brief report. AANA J. 2011;79:15–8. [PubMed] [Google Scholar]
- 13.Baker PA, Depuydt A, Thompson JM. Thyromental distance measurement--fingers don’t rule. Anaesthesia. 2009;64:878–82. doi: 10.1111/j.1365-2044.2009.05985.x. [DOI] [PubMed] [Google Scholar]
- 14.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: A meta-analysis of bedside screening test performance. Anesthesiology. 2005;103:429–37. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 15.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–11. [PubMed] [Google Scholar]
- 16.Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–33. doi: 10.1097/00000542-199005000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Eberhart LH, Arndt C, Cierpka T, Schwanekamp J, Wulf H, Putzke C. The reliability and validity of the upper lip bite test compared with the Mallampati classification to predict difficult laryngoscopy: An external prospective evaluation. Anesth Analg. 2005;101:284–9. doi: 10.1213/01.ANE.0000154535.33429.36. [DOI] [PubMed] [Google Scholar]
- 18.Huh J, Shin HY, Kim SH, Yoon TK, Kim DK. Diagnostic predictor of difficult laryngoscopy: The hyomental distance ratio. Anesth Analg. 2009;108:544–8. doi: 10.1213/ane.0b013e31818fc347. [DOI] [PubMed] [Google Scholar]
- 19.Krobbuaban B, Diregpoke S, Kumkeaw S, Tanomsat M. The predictive value of the height ratio and thyromental distance: Four predictive tests for difficult laryngoscopy. Anesth Analg. 2005;101:1542–5. doi: 10.1213/01.ANE.0000181000.43971.1E. [DOI] [PubMed] [Google Scholar]
- 20.Khan ZH, Maleki A, Makarem J, Mohammadi M, Khan RH, Zandieh A. A comparison of the upper lip bite test with hyomental/thyrosternal distances and mandible length in predicting difficulty in intubation: A prospective study. Indian J Anaesth. 2011;55:43–6. doi: 10.4103/0019-5049.76603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hester CE, Dietrich SA, White SW, Secrest JA, Lindgren KR, Smith T. A comparison of preoperative airway assessment techniques: The modified Mallampati and the upper lip bite test. AANA J. 2007;75:177–82. [PubMed] [Google Scholar]
- 22.Safavi M, Honarmand A, Zare N. A comparison of the ratio of patient's height to thyromental distance with the modified Mallampati and the upper lip bite test in predicting difficult laryngoscopy. Saudi J Anaesth. 2011;5:258–63. doi: 10.4103/1658-354X.84098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chohedri AH, Tabari M. The upper lip bite test to predict difficult intubation. Prof Med J. 2005;12:440–5. [Google Scholar]
- 24.Gupta AK, Mohamad O, Showkat N, Imtiyaz N, Anjali M. Predictors of difficult intubation: Study in kashmiri population. Br J Med Pract. 2010;3:307. [Google Scholar]
- 25.Karkouti K, Rose DK, Ferris LE, Wigglesworth DF, Meisami-Fard T, Lee H. Inter-observer reliability of ten tests used for predicting difficult tracheal intubation. Can J Anaesth. 1996;43:554–9. doi: 10.1007/BF03011765. [DOI] [PubMed] [Google Scholar]
- 26.Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006;102:1867–78. doi: 10.1213/01.ane.0000217211.12232.55. [DOI] [PubMed] [Google Scholar]
- 27.Bilgin H, Ozyurt G. Screening tests for predicting difficult intubation. A clinical assessment in Turkish patients. Anaesth Intensive Care. 1998;26:382–6. doi: 10.1177/0310057X9802600407. [DOI] [PubMed] [Google Scholar]
- 28.Tripathi M, Pandey M. Short thyromental distance: A predictor of difficult intubation or an indicator for small blade selection? Anesthesiology. 2006;104:1131–6. doi: 10.1097/00000542-200606000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Schmitt HJ, Kirmse M, Radespiel-Troger M. Ratio of patient' s height to thyromental distance improves prediction of difficult laryngoscopy. Anaesth Intensive Care. 2002;30:763–5. doi: 10.1177/0310057X0203000607. [DOI] [PubMed] [Google Scholar]
- 30.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: An updated report by the american society of anesthesiologists task force on management of the difficult airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]


