Abstract
Aims and Objective:
The objectives of this study were to evaluate the epidemiology, clinical variable of chemical burns, and their outcomes to prevent or reduce the frequency and morbidity of such injuries.
Materials and Methods:
A retrospective analysis was performed on all the patients with chemical burns admitted at author's center between November 2008 and December 2013. All the patients were evaluated in terms of age, sex, total body surface area, etiology, treatment given, morbidity, mortality, final outcome, and then educated regarding specific preventive measures.
Results:
A total of 96 patients (2.4% of total burn admissions) (42 males and 54 females) were admitted to our hospital with chemical burn injuries. Most of the patients were in the age group of 16–30 years. Incidence in females was slightly higher than in males. Acid was found to be the most common cause of injury. We found 55% patients admitted had <10% total body surface area (TBSA) involvement, 35% had burns involving between 11 and 20% TBSA, and 4% had burns involving 21–30% TBSA, and 6% had burns in >30% TBSA. Morbidity was noticed in the form of skin defect in 80% of cases, soft tissue defect with exposed tendon, bone, or vessels in 16% of cases, and 4% of patients developed contracture and hypertrophic scar. Eighty-six percent of patients required operative intervention. A total of three deaths (3%) were recorded.
Conclusion:
It was found that chemical burns, though not very common, are deeper burns and can be accidental or non-accidental, and the high-risk age group is 16–25 years. Chemical burns are largely preventable and if properly managed have a good outcome.
Keywords: Chemical burn, epidemiology, preventive measures
Introduction
Burn injury is very common in developing countries, especially in poor socioeconomic and rural areas. There are various forms of burn injuries including thermal, flame, electrical, scald, and chemical.
In the modern era, chemicals are commonly used due to continuous development in industrialization. Though it is uncommon in poorly developed areas, it could be devastating. The factors influencing chemical burns are geographic areas, types of population, degree of industrialization, and physical and social surroundings.[1] Majority of the chemical burns are due to assault or are accidental.[2,3]
The various agents causing chemical burns are acids, alkalis, urea, and organic substances. Work-related causes of burn injury are very common accounting for 29% of burns requiring admission.[4] Palao et al.[5] described the pathophysiology of chemical burns. Acids act by coagulation necrosis through protein denaturation leading to thick eschar formation. This prevents deeper penetration of the acids. On the other hand, alkalis acts by liquefaction necrosis that allows a deeper penetration leading to more damage compared to acid burns. The various factors influencing severity of chemical burns are its physical characteristics, pH value, time of contact with the agent, and concentration of the chemical substance.
Chemical burn can lead to grievous injury.[6] Ocular burn causes corneal opacification and subsequent loss of vision. Acid ingestion may lead to esophageal stricture which may require complicated reconstruction, thus further increasing the morbidity.[7] However; early management could prevent these morbidities. Furthermore, proper safety measures must be taken at the workplace. Hunt et al. recommended instituting education and prevention measures targeted at workers in high-risk occupation groups.[8]
In this series, we present the epidemiology and outcome of chemical burns in and around Aligarh, Utter Pradesh, India. Different types of chemical burn injuries, their severity, site involved, morbidities, operative procedures, their outcomes, and measures to prevent or reduce the frequency and morbidity of such injuries were evaluated.
Materials and Methods
A retrospective analysis was performed on all the patients with chemical burns admitted at burn unit of our hospital between November 2008 and December 2013. All patients of chemical burns, irrespective of the severity of their injuries, were admitted, assessed, managed accordingly, and then educated regarding specific preventive measures. Sixty percent of the patients presented within 24 h. All these patients were thoroughly irrigated with tap water for 30 min. Patients were properly resuscitated following advanced trauma life support. The medical notes of the patients admitted in the aforementioned period were reviewed. The information regarding age, sex, total body surface area, etiology, treatment given, morbidity, mortality, and final outcome was recorded.
Results
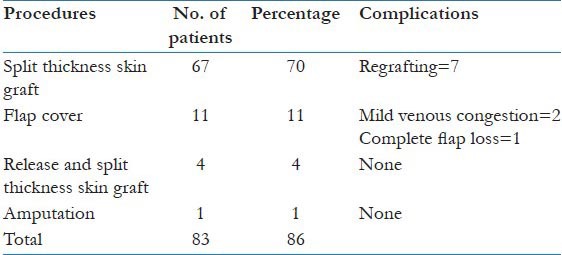
A total of 96 patients (42 males and 54 females) were admitted to our hospital with chemical burn injuries. Most of the patients were in the 16–30 year age group [Table 1]. Incidence in females was slightly higher than in males. Acid was found to be the most common cause of injury [Table 2]. We found that 55% of patients who were admitted had <10% total body surface area (TBSA) burns, 35% had burns involving between 11 and 20% TBSA, 4% had burns involving between 21 and 30% TBSA, and 6% had burns involving >30% TBSA [Table 3]. Accidental injury was the most common mode of injury followed by homicidal and suicidal injuries [Table 4]. Head and neck region was found to be the most common site of injury accounting for 37% of the total injury [Table 5]. Morbidity was noticed in the form of skin defect in 80% of cases, soft tissue defect with exposed tendon, bone, or vessels in 16% of cases, and 4% of patients developed contracture and hypertrophic scar. Also, 86% of patients required operative intervention [Table 6]. Sixty-seven patients (70%) required split thickness skin graft, 11 patients (11%) underwent flap cover, and 1 underwent amputation of hand. Of those who underwent skin graft, seven required regrafting due to complete or partial loss [Table 7]. Of the patients who underwent flap cover, two developed mild venous congestion which subsided by conservative means and one patient had complete flap loss that required split thickness skin graft. A total of three deaths (3%) were recorded.
Table 1.
Age and sex distribution
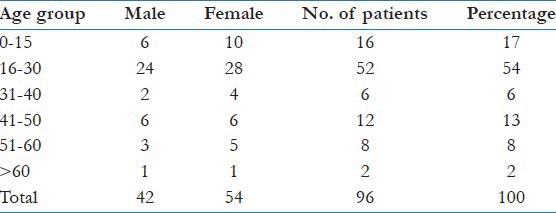
Table 2.
Etiology of chemical burn
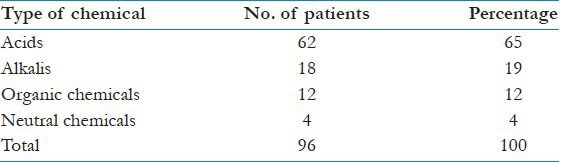
Table 3.
Total body surface area

Table 4.
Nature of chemical burn
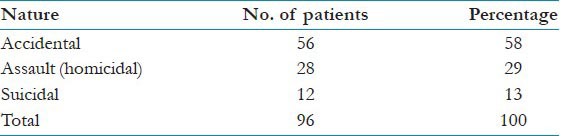
Table 5.
Sites involved

Table 6.
Morbidity and mortality

Table 7.
Operative procedures
Discussion
Burn injury is very common in our country. It can be categorized as thermal, electrical, scald, and chemical burn. Chemical injury, though uncommon, can be devastating and may lead to significant morbidity if not properly managed. The incidence of chemical burn was found to be 2.4% in our study, which corresponds to other studies showing an incidence between 1.4% and 4.8%.[9,10,11]
Common substances that may cause chemical burns are acids, alkalis, and various organic and neutral substances. Out of these, acid burns are most common as described by Ramakrishnan et al.[12] We found similar results as 65% of patients sustained injury due to acids in our study.
As described in various literatures, patients with chemical burns presenting early should be treated by hydrotherapy to dilute and remove the chemicals.[13,14,15] In our series, 60% of the patients presented within 24 h. All these patients underwent irrigation with copious amount of water for 30 min. Industrial chemical burn is most common in western countries.[15] In contrast, our population covers rural catchment area, and therefore, domestic accidental chemical burn was found to be the most common cause of injury accounting for 58% of the patients in this series.
Eschar separation is delayed in chemical burns occurring between 3 and 5 weeks.[11] Split thickness skin graft is one of the commonest operative procedures performed for chemical burns after debridement or spontaneous separation of slough.[11] The same was performed in 70% of patients in this study. Fifteen patients (16%) had soft tissue loss with exposed vital structures (tendon, bone, or vessels). Out of these, 11 required flaps, 1 underwent amputation of hand, and 3 patients expired. These three patients had TBSA of more than 30% and presented late with features of septicemia. Incidence of chemical burn in females was found to be slightly more than in males. This could be due to involvement of females in domestic work more than males. We also observed that injury in the age group of 16–30 years was the most common due to similar reason.
Various factors were found to be responsible for chemical burns, including mishandling of chemicals, lack of awareness regarding action and side effects of specific chemicals, lack of employee's knowledge, and not using appropriate protective measures. Therefore, all the patients in our series were educated regarding specific targeted protective measures. It is also important to make specific laws in industries and make the employee aware of the chemicals used.
A total of 28 patients (29%) in this series were cases of vitriolage (acid attacks); 21 (75%) of them were females. In addition to the medical effects of acid burn, it has various social issues, especially in women. This type of attack may leave the victims handicapped, thus making them dependent on other members of the family for their daily activities. This situation is further aggravated by inability of the victim to find suitable and appropriate work due to impaired vision and physical health. This leads to negative impact on the economic status of the patient and his/her family. The survivors of acid burn are usually excluded from the society, thus causing hurdles in their marriage if they are single.[16]
Vitriolage/acid attack on women in India needs special elaboration and is a matter of concern. This usually occurs as a form of revenge when the woman refuses a man's proposal for marriage. The number is increasing.[17]
The Supreme Court's judgment on regulation of sale of acids came on July 16, 2013 following an incident in which four sisters sustained burns after being attacked with acid. The Supreme Court has directed India's 28 states and 7 union territories to issue licenses to retailers selling acid after the government said it will categorize acid as poison. The court ruled that a person less than 18 years of age cannot purchase acids like hydrochloric acid, sulfuric acid, and nitric acid. Details of buyers and quantity of the acid sold must be recorded by shopkeepers. The Supreme Court said, “Over the counter sale of acid is completely prohibited unless the seller maintains a log/register recording the sale of acid and the retailers will have to declare the amount of acid being stocked to the police.” The Court said that acid attacks become a non-bailable offence and the survivors of the attack should receive 300,000 rupees in compensation, a third of which must be given within 15 days of the attack. India's parliament approved a bill strengthening laws on assaults against women following the gang rape of a 23-year-old student on a bus in Delhi 2 years back. Acid attacks were included in the bill and were made a criminal offence with a minimum 10-year prison term.[18]
Conclusion
It was found that chemical burns, though not very common, are deeper burns, can be accidental or non-accidental, and the high-risk age group is 16–30 years. An early surgical intervention in selected group of patients, targeting all the epileptic patients for education, and instituting specific preventive measures give good outcomes.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Song C, Chua A. Epidemiology of burn injuries in Singapore from 1997 to 2003. Burns. 2005;31(Suppl 1):S18–26. doi: 10.1016/j.burns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 2.Sawhney CP, Kaushish R. Acid and alkali burns: Considerations in management. Burns. 1989;15:132–4. doi: 10.1016/0305-4179(89)90146-0. [DOI] [PubMed] [Google Scholar]
- 3.Sinha J, Sinha S. Chemical burns. In: Sinha J, Sinha S, editors. Handbook of Burns Management. New Delhi: Jaypee Brothers Medical Publisher; 1991. pp. 152–9. [Google Scholar]
- 4.Pruitt VM. Work-related burns. (ix-x).Clin Occup Environ Med. 2006;5:423–33. doi: 10.1016/j.coem.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 5.Palao R, Monge I, Ruiz M, Barret JP. Chemical burns: Pathophysiology and treatment. Burns. 2010;36:295–304. doi: 10.1016/j.burns.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Morgan SJ. Chemical burns of the eye: Causes and management. Br J Ophthalmol. 1987;71:854–7. doi: 10.1136/bjo.71.11.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chandra R, Agarwal R. Chemical burns in children. Paras Medical Publisher; 2011. Total Management of the Burned Child; pp. 240–9. [Google Scholar]
- 8.Hunt JP, Calvert CT, Peck MD, Meyer AA. Occupation-related burn injuries. J Burn Care Rehabil. 2000;21:327–32. doi: 10.1067/mbc.2000.108092. [DOI] [PubMed] [Google Scholar]
- 9.Pegg SP, Gregory JJ, Hogan PG, Mottarelly IW, Walker LF. Epidemiological pattern of adult burn injuries. Burns. 1979;5:326–34. [Google Scholar]
- 10.Leonard LG, Scheulen JJ, Munster AM. Chemical burns: Effect of prompt first aid. J Trauma. 1982;22:420–3. doi: 10.1097/00005373-198205000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Sawhney CP, Kaushish R. Acid and alkali burns: Considerations in management. Burns. 1989;15:132–4. doi: 10.1016/0305-4179(89)90146-0. [DOI] [PubMed] [Google Scholar]
- 12.Ramakrishnan KM, Mathivanan T, Jayaraman V, Babu M, Shankar J. Current scenario in chemical burns in a developing country: Chennai, India. Ann Burns Fire Disasters. 2012;25:8–12. [PMC free article] [PubMed] [Google Scholar]
- 13.Bromberg BE, Song IC, Walden RH. Hydrotherapy of chemical burns. Plast Reconstr Surg. 1965;35:85–95. doi: 10.1097/00006534-196501000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Curreri PW, Asch MJ, Pruitt BA. The treatment of chemical bums: Specialized diagnostic, therapeutic, and prognostic considerations. J Trauma. 1970;10:634–42. [PubMed] [Google Scholar]
- 15.Herbert K, Lawrence JC. Chemical burns. Burns. 1989;15:381–4. doi: 10.1016/0305-4179(89)90103-4. [DOI] [PubMed] [Google Scholar]
- 16.Iranian Woman Blinded by Acid Attack Pardons Assailant as he Faces Same Fate. The Guardian. 2011-07-31. [Google Scholar]
- 17.India's Acid Victims Demand Justice. BBC News. 2008 Apr 9;:XXXX. [Google Scholar]
- 18.India Realtime. New Rules to Curb Acid Attacks. 2013 Jul 19; [Google Scholar]


