Abstract
Background:
Psychiatric disorders including anxiety, depression, somatization, obsessive compulsive, and bipolar disorders are recognized as causing the biggest burden of disease worldwide.
Aim:
In this study, we aimed to assess the prevalence and burden of common mental disorders at Primary Health Care Centers (PHCC) using the World Health Organization Composite International Diagnostic Interview (WHO-CIDI) in the Qatari population, aged 18–65 who attended Primary Health Care (PHC) settings.
Design:
A prospective cross-sectional study conducted during November 2011 to October 2012.
Setting:
Primary Health Care Centers of the Supreme Council of Health, Qatar.
Subjects:
A total of 2,000 Qatari subjects aged 18–65 years were approached; 1475 (73.3%) agreed to participate.
Methods:
Prevalence and severity of International Classification of Disease-10 disorders were assessed with the WHO-CIDI (Version 3.0).
Results:
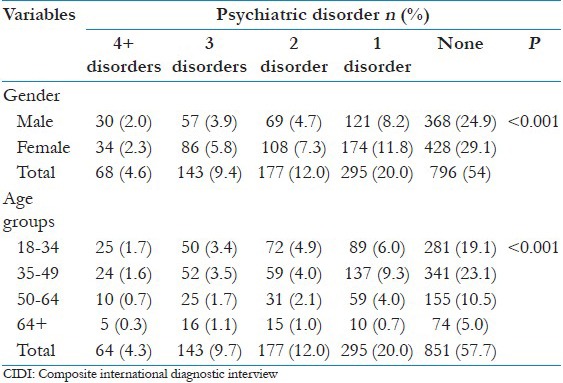
Of the 1475 participants, 830 (56.3%) were females and 645 (43.7%) was males. One-third were aged 35–49 years 558 (37.8%). The three most common disorders were major depression disorders (18.31%), any anxiety disorders (17.3%), any mood disorders (16.95%), followed by separation anxiety disorders (15.25%), personality disorder (14.1%). In the present study, prevalence in women was significantly higher than men for the most common psychiatric disorders, specifically generalized anxiety disorder, panic disorder, social phobia, specific phobias, obsessive compulsive disorders, posttraumatic disorder, somatization, major depressive disorder, bipolar disorder, dysthymia, and oppositional defiant disorder. Of the total 20% had only one psychiatric diagnosis and 12% had two disorders, 9.7% respondents with three diagnoses, and finally 4.3% of respondents had four or more diagnoses.
Conclusion:
One-fifth of all adults who attended the PHCC (20%) had at least one psychiatric diagnosis. The CIDI is a useful instrument for psychiatric diagnosis in community settings such as PHC clinics, clinical research and intervention studies. There is an urgent need to not only assess prevalence, but also risk factors, burden, treatment gaps and outcomes to obtain evidence for policy making.
Keywords: Composite International Diagnostic Interview, prevalence, Primary Health Care visits, psychiatric disorders, Qatar, size and burden disorders
Introduction
Recent cross-national epidemiologic studies have demonstrated a wide variation in the prevalence of common mental disorders across countries.[1,2,3,4] Mental disorders are widely recognized as a major contributor (14%) to the global burden of disease worldwide.[1] Patients often present to their family physician as their first contact with health services, depression and anxiety disorders remain the most common conditions in primary care. Yet, symptoms are commonly undetected.[5] Although potentially treatable, lack of early detection and the subsequent nontreatment results in substantial morbidity and contributes to the higher social burden of disease.[5,6,7] Psychiatrists in the Middle East are well accustomed to patients with psychiatric problems presenting late to health services, often under pressure from family.[6,7,8,9]
Internationally, the public health burden of anxiety and depression are well recognized, ranking fourth among global burden of diseases. By 2020, their impact is estimated to rise to second.[10,11] In previously published studies from Qatar depression was the most common; second only to heart disease as a cause of disability in this country.[6,7] Depression is also the most common mental health presentation at Primary Health Care Centre (PHCC) level, often presenting with multiple somatic complaints and co-morbid anxiety disorders.[6,7,8] Lack of awareness and high levels of stigma related to mental health is a barrier to accessing mental health services at an early stage, resulting in impairments in social functioning, employment, and quality of life. Furthermore, it is well-established that prevalence rates of common mental disorders are higher in women in most countries.[12,13]
In primary care setting, the high prevalence of anxiety and depressive disorders increases use of health services, and delays response to effective treatments.[14,15] Certain demographic and psychosocial risk factors for anxiety-depression appear to be universal, in particular,[16,17,18,19] female gender;[16] unemployment;[17] lower levels of education;[18] young (vs. older) adulthood;[19] co-morbid substance use disorder (SUD);[20] physical ill-health;[21] and exposure to potentially traumatic events or postpartum depression.[22,23]
Structured psychiatric diagnostic tools have been developed by the World Health Organization (WHO) of which the Composite International Diagnostic Interview (CIDI) has been used worldwide.[3,4,14,24,25,26] The CIDI ascertains diagnoses based on WHO International Classification of Disease (ICD) criteria facilitating cross-national comparative epidemiological studies of mental disorders.[8]
The aim of this study was to assess the prevalence and burden of common psychiatric disorders at PHCC using the WHO-CIDI in the Qatari population, aged 18–65, and examine their symptom patterns and co-morbidity.
Methods
This is a prospective cross-sectional study that included Qatari patients aged 18–65 years who attended the Primary Health Care (PHC), during the period from November 2011 to October 2012, using WHO-CIDI instrument.[3,4,14,24,25,26,27] The field of psychiatric epidemiology has made considerable progress in the last few decades, with the expansion and refinement of the definitions and criteria for mental disorders in the main diagnostic systems: The WHO's ICD,[28] and the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM),[29] allowing the use of operationalized diagnostic criteria within fully structured research questionnaires that can be administered by trained nonclinical interviewers. Using such procedures, community epidemiological surveys have started to be carried out in many countries, leading over time to the refinement of survey methods design and questionnaire development.
Design
A multistage stratified sampling design was developed, using an administrative division of Qatar into 23 PHCs in terms of number of inhabitants. Only 13 health centers were visited mostly by Qatari nationals and other Arab expatriates, the remaining 10 health centers were excluded from our survey. The selected 13 health centers represented the Arab population mostly geographically, in Qatar.
Ethical approval
Institutional review board approval was obtained from Weill Cornell Medical College and Hamad Medical Corporation, MRC for conducting this research in Qatar.
Subjects
The subjects were selected by simple random sampling among population who visited the 13 health centers (10 urban and 3 semi-urban). Qualified nurses and health educators were trained to interview structurally and complete a questionnaire for randomly selected Qatari and Arab expatriates population of age 20 years and above. Assuming the prevalence rates of depression and anxiety disorders in Qatar to be similar to rates found in other Arabian Gulf countries and the Eastern Mediterranean,[6,8,9] with reported prevalence of 20% with the 99% confidence interval (CI) for an error of 3% at the level of significance, a sample size of 1500 subjects would be required to meet the objectives of the study. Allowing an error of 2.5%, level of significance (type 1 error) of 1%, and 99% CI, the computer program indicated that a sample size of 2000 subjects was required to achieve the objective of our study.
A random sample of Qatari nationals aged 18–65 years old was drawn from the primary care registry. A total of 2000 Qatari subjects were approached; 1475 (73.3%) agreed to participate. The study was conducted during the period from March 2011 to December 2012.
Questionnaires
The data were collected through a validated self-administered questionnaire with the help of physicians and qualified nurses. The questionnaire had three parts. The first part included the sociodemographic details of the patients, the second part with the medical and family history of the patients, and the third part was the diagnostic screening questionnaire.
Disorder severity
Cases were classified with an ad hoc three-category severity rating. Cases were classified as serious if they had any of the following: Bipolar I disorder; substance dependence with a physiological dependence syndrome; suicide attempt within the previous 12 months; severe impairment in at least two areas of role functioning assessed in the Sheehan Disability Scales (SDS),[19] or role functioning at a level consistent with a Global Assessment of Functioning[9] score of 50 or less. Cases not classified as serious were judged to be moderate if the individual had either substance dependence without a physiological dependence syndrome or at least moderate role impairment in two or more SDS domains. Remaining cases were classified mildly.
The World Mental Health (WMH)-CIDI instrument in Arabic language was used by the trained 12 interviewers to administer the instrument. The interviewers were all nurses working at the psychiatry department of Hamad Medical Corporation and PHCC. The psychiatric diagnoses reported were based on ICD-10 criteria[27,28] and generated with the Arabic WMH-CIDI version 3.0. The participants completed the Arabic WMH-CIDI which was previously validated[9] although some Arabic words had to be replaced due to a different dialect. Paper and pencil Personal Interview version 6 was utilized to bridge the data into BLAISE survey software for professionals; Blaise 4.8.4 version, 1888, The Netherland 2014. Blaise® is a registered trademark of Statistics Netherlands, a third party computer program customized to capture ICD-10 diagnoses and generate statistical data into SPSS statistical analysis software. The ICD-10 diagnoses[27,28] generated in this study included generalized anxiety disorders, major depressive disorder, social phobia, obsessive-compulsive disorder (OCD), psychosis and personality disorder. Chronic conditions section was also included. Functional disability section was randomized to every 10th interview. The original WMH-CIDI[24,25,26,30] includes 41 sections and takes an average of 1, 5 h to administer. The WHO field trials of the CIDI have documented good inter-rate reliability, test-retest reliability and validity for almost all diagnostic categories.
Student's t-test was used to ascertain the significance of differences between mean values of two continuous variables and confirmed by nonparametric Mann–Whitney test. Chi-square and Fisher's exact test were performed to test for differences in proportions of categorical variables between two or more groups. Multivariate logistic regression analysis using the forward inclusion and backward deletion method was used to determine for potential confounders and importance of risk factors. The level P < 0.05 was considered to be the cut-off value for significance.
Results
Of the 1475 participants, 830 (56.3%) were females, and 645 (43.7%) was males. One-third were aged 35–49 years 558 (37.8%). Majority of them were married (75.10%).
Table 1 gives the prevalence and severity of ICD-10 disorders by severe, moderate and mild condition. The three most common disorders were major depression disorders (18.3%), any anxiety disorders (17.3%), any mood disorders (17%), followed by separation anxiety disorders (15.3%), personality disorder (14.1%). The majority of subjects were in the mild to moderate range of symptom severity. In addition, the most common co-morbid chronic physical conditions were ischemic heart disease, followed by diabetes than hypertension.
Table 1.
Prevalence and severity of Qatari CIDI disorders of studied subject (n=1475)
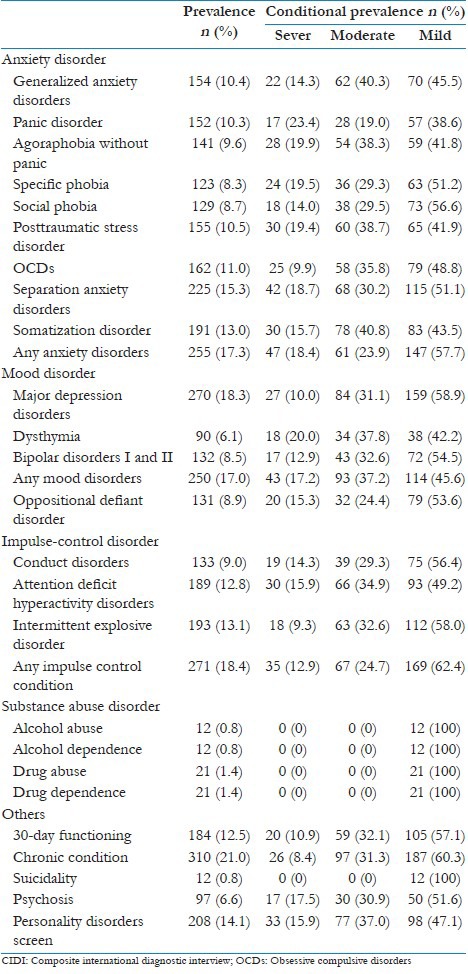
Table 2 presents the prevalence and severity of DSM-IV disorders by age group. More than one-third of the participants were in the age group 35–49 years (37.8%), followed by 18–34 years (34%), then 50–64 years (19.6%) and above aged 65 years old (8.5%). Across the diagnostic categories covered in this study, the most affected were the 35–49 years age group with a high statistical significance (P < 0.001). This was also the age group most impaired as assessed by the 30-day functioning.
Table 2.
CIDI disorders of studied subject by age group (n=1475)
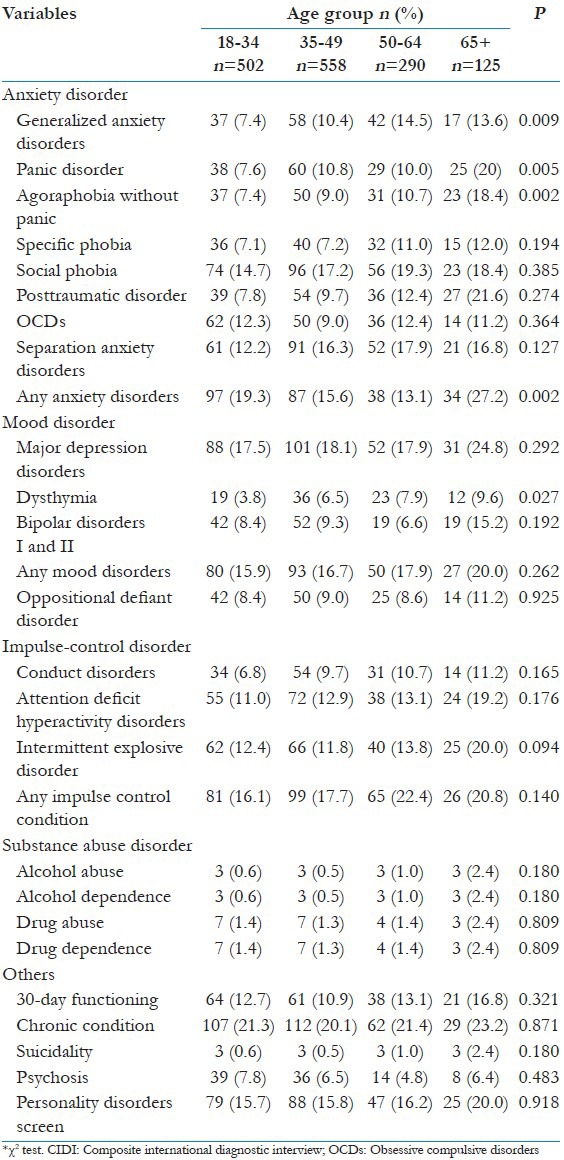
Table 3 shows the prevalence and severity of disorders by gender. Not surprisingly, prevalence rates in women were significantly higher than men for the most common mental disorders. In the present study, prevalence in women was significantly higher than men for the most common psychiatric disorders, specifically generalized anxiety disorder, panic disorder, social phobia, specific phobias, OCDs, posttraumatic disorder, somatization, major depressive disorder, bipolar disorder, dysthymia, and oppositional defiant disorder.
Table 3.
Multivariate logistic regression analysis results of CIDI disorders by gender (n=1475)
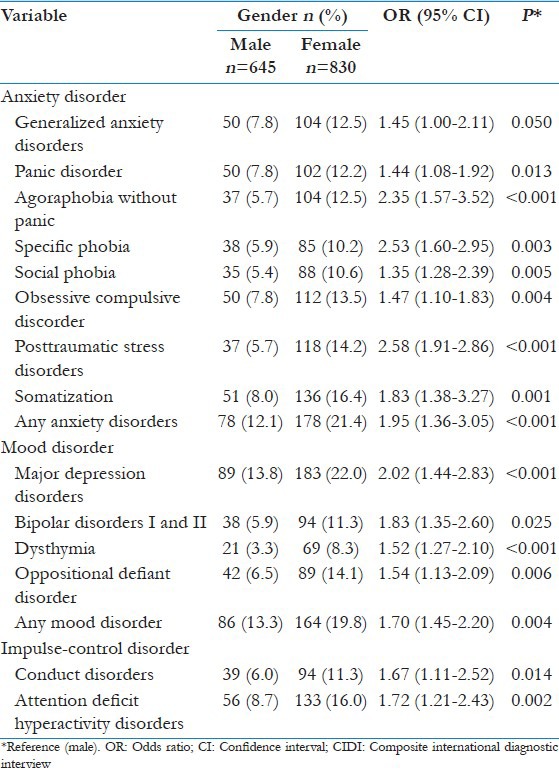
Table 4 shows the prevalence rate of CIDI psychiatric disorders by degree of co-morbidity be gender and age groups. Of the total sample of 1475, 20% had at least one psychiatric diagnosis, and 12% had two disorders, 9.7% respondents with three diagnoses, finally 4.3% of respondents had four or more diagnoses.
Table 4.
The prevalence of rate CIDI psychiatrics disorders by degree of co-morbidity be gender and age groups (n=1475)
Discussion
The prevalence of current psychiatric disorders was found to be relatively high in primary care clinics in Qatar. Major depression disorders, any anxiety disorder, any impulse control condition, and mood disorder were the most common disorders, afflicting, respectively, one patient out of five. These estimates are amongst the highest reported in the world.[2,3,4,10,11] Higher levels of psychiatric morbidity may be associated with higher consanguineous marriages, rapid urbanization, heterogeneous population as social groups living in adverse situations under chronic stress would be more likely to present mental disorders as previously reported.[8,31,32,33]
We found advantages in using the CIDI, such as standardization of data collection, widening and extending investigation field of the physician,[3,4,9,21,24,25,26,30] standardization of the communication between different professionals, and utilization of nonmedical interviewers as a way to increase capacity and capability for psychiatric assessment and to reduce costs in population studies. Our results confirm previous findings that the rates of common mental disorders are higher in women.[2,3,8,9,10,14,21,24,25,26]
Major depression is a serious, recurrent disorder linked to diminished role functioning and quality of life, medical comorbidity, and mortality.[2,3,4,10,14,30,31,32] In the present study, prevalence of any anxiety disorders in women was significantly higher than men (21.4% vs. 12.1%) and major depression disorders (22.0% vs. 13.8%). Prince et al.,[1] noted that women are at higher risk for common mental disorders with a higher female to male sex ratio of 1.5:1. Culturally, the role of women in this society is changing. The level of education for Qatari women is higher than men.[6,7] More women are now working in leadership positions while the cultural expectation of them as wives and mothers remains unchanged. The extent of stress this imposes on women, and its reflection on their mental health needs further investigation. The study finding that 30-day functioning was more impaired in women is an area for future research. Qatar's recently approved mental health strategy recognizes women's mental health as one of the national priorities.
The study findings showed that young 37.8% of Qatari population in the age group 35–49 years were affected with mental disorders. The prevalence of anxiety and depression, panic and any anxiety disorders were highest in the age group 65 and above, followed by 50–64 years. Our finding of a peak age for depression and anxiety disorders during midlife is in keeping with other epidemiological findings in the State of Qatar and other Western countries.[9,13,16,34,35,36,37,38,39] More recently a study reported[13] that the widely documented decrease in the prevalence of mental depression episode among the elderly is much more pronounced in developed than in developing countries. Although the prevalence of chronic physical conditions increased with age in both developed and developing countries, the association between depression and chronic conditions generally decreases with age. This is in line with findings of previous studies.[13,14,15,26,27]
Furthermore, there is great variation in the prevalence estimates of individual disorders, which could be due to the assumption that the WMH-CIDI does not adequately or consistently capture psychopathological syndromes in different cultures,[2,3,4,10,11] as the lowest prevalence rates were found in non-Western countries (Nigeria 12%, China 13.2% and Japan 18.1%),[21] with the exception of Israel with an overall prevalence rate of 17.6%[34,35] (but only including the assessment of mood and SUDs, and few anxiety disorders). Finally, the lifetime prevalence estimate of OCD in our study was high (10.98%, standard error [SE] =0.5), compared with the Brazilian study (6.7%, SE = 0.5).[21] Although the instrument used was the same, it was found to show little sensitivity in Brazil, and the skip patterns were modified to keep respondents in the section, answering more questions, with a greater probability of picking up otherwise false-negatives, or conversely, identifying more false-positives. Since the CIDI is based on the assessment of symptoms that compose diagnostic criteria for psychiatric disorders, it may have detected mild cases with no clinical relevance, contributing to the high prevalence rates.
High rates of somatization disorders in primary care clinics in our study might be explained by higher rates in the community, due, in particular, to the high proportion of immigrants expatriate workers in Qatar, since higher rates of somatization symptoms have been described in immigrant populations and minority ethnic groups than in native populations.[8,31,32] It is worthwhile noting that in two other Middle East populations, conversion disorder has also been reported to be high in primary care in Israel,[14,34,35] in general practice attendees across Europe[36,37,38,39] and in Qatar.[16,31,32]
The relationship between physical and mental illness is a complex one with close cause-effect factors. Diabetes, hypertension, and ischemic heart disease are among the most prevalent physical condition in this society, with a sedentary lifestyle and eating habits that contribute to the risk. Co-morbidity with mental illness raises concerns about the management options, quality of life and burden of disease for these disorders. Further studies are much needed as a matter of urgency.
The study findings highlight the urgent need for systematic development of community-based mental health services for the screening, early identification, and treatment of people with psychiatric disorders.
Limitations
No ongoing comprehensive electronic health registry exists to assess the morbidity burden at the national level. Therefore, we substituted and back translated a few words to be certain of the relevance of the questions. Some of the limitations of the instrument were: The rigidity of its rules; the inflexibility of the diagnostic algorithms; the need of some clinical judgment, with the consequent hampering of the administration by totally lay interviewers. The rigidity of the rules and the inflexibility of the diagnostic algorithms caused the detection of only the number of occurred symptoms and not their severity or hierarchical importance. The interview lasted an average of 75 min, which was difficult to maintain with many patients. Most of them were in the center because they were actually sick which affected their ability to continue the interview. Finally, the stigma of mental illness and particularly questions about suicide and substance abuse hindered the engagement of the responders, many of which preferred to abort the interview.
Conclusion
The study findings revealed that almost one-fifth of all adults who attended the PHCC setting presented with at least one type of mental disorders. Overall, the prevalence of the generalized anxiety disorders; social phobia, specific phobia, major depression, and personality disorders were the significantly higher in women than in men. The young Qatari population in the age groups 35–49 years and above 65 years old were the most affected with mental disorders. These results suggest that caution must be taken when using the CIDI as the sole diagnostic instrument in epidemiological research to estimate prevalence and incidence. The CIDI may be more useful for screening out potential candidates in clinical research and psychopharmacological trials. There is an urgent need to not only assess prevalence, but also risk factors, burden, treatment gaps and outcomes to obtain evidence for policy making.
Acknowledgments
This study was generously supported and funded by the Qatar Diabetes Association and Qatar National Research Fund Grant No. UREP 10-109-3-021. The authors would like to thank the Hamad Medical Corporation for their support and ethical approval (HMC RP no. 11187/11 and HMC RP no. 12061/12).
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–77. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 2.Cross-national comparisons of the prevalences and correlates of mental disorders. WHO International Consortium in Psychiatric Epidemiology. Bull World Health Organ. 2000;78:413–26. [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, et al. The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiol Psichiatr Soc. 2009;18:23–33. doi: 10.1017/s1121189x00001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC, Calabrese JR, Farley PA, Gruber MJ, Jewell MA, Katon W, et al. Composite International Diagnostic Interview screening scales for DSM-IV anxiety and mood disorders. Psychol Med. 2013;43:1625–37. doi: 10.1017/S0033291712002334. [DOI] [PubMed] [Google Scholar]
- 5.Mechanic D. Barriers to help-seeking, detection, and adequate treatment for anxiety and mood disorders: Implications for health care policy. J Clin Psychiatry. 2007;68(Suppl 2):20–6. [PubMed] [Google Scholar]
- 6.Bener A, Ghuloum S. Gender differences in the knowledge, attitude and practice towards mental health illness in a rapidly developing Arab society. Int J Soc Psychiatry. 2011;57:480–6. doi: 10.1177/0020764010374415. [DOI] [PubMed] [Google Scholar]
- 7.Ghuloum S, Bener A, Dafeeah EE, Zakareia AE, El-Amin A, El-Yazidi T. Prevalence of common mental disorders in general practice attendees: Using World Health Organization Composite International Diagnostic Interview (WHO-CIDI) in Qatar. Int J Clin Psychiatry Ment Health. 2014;2:38–46. [Google Scholar]
- 8.Bener A, Dafeeah EE, Chaturvedi SK, Bhugra D. Somatic symptoms in primary care and psychological comorbidities in Qatar: Neglected burden of disease. Int Rev Psychiatry. 2013;25:100–6. doi: 10.3109/09540261.2012.730993. [DOI] [PubMed] [Google Scholar]
- 9.Karam EG, Mneimneh ZN, Karam AN, Fayyad JA, Nasser SC, Chatterji S, et al. Prevalence and treatment of mental disorders in Lebanon: A national epidemiological survey. Lancet. 2006;367:1000–6. doi: 10.1016/S0140-6736(06)68427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, et al. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMHCIDI) Int J Methods Psychiatr Res. 2004;13:122–39. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wittchen HU. Generalized anxiety disorder: Prevalence, burden, and cost to society. Depress Anxiety. 2002;16:162–71. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]
- 13.Kessler RC, Birnbaum HG, Shahly V, Bromet E, Hwang I, McLaughlin KA, et al. Age differences in the prevalence and co-morbidity of DSM-IV major depressive episodes: Results from the WHO World Mental Health Survey Initiative. Depress Anxiety. 2010;27:351–64. doi: 10.1002/da.20634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Laufer N, Zilber N, Jecsmien P, Maoz B, Grupper D, Hermesh H, et al. Mental disorders in primary care in Israel: Prevalence and risk factors. Soc Psychiatry Psychiatr Epidemiol. 2013;48:1539–54. doi: 10.1007/s00127-012-0620-8. [DOI] [PubMed] [Google Scholar]
- 15.Gureje O, Lasebikan VO, Kola L, Makanjuola VA. Lifetime and 12-month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well-Being. Br J Psychiatry. 2006;188:465–71. doi: 10.1192/bjp.188.5.465. [DOI] [PubMed] [Google Scholar]
- 16.Bener A, Ghuloum S, Al-Mulla AA, Al-Marri S, Hashim MS, Elbagi IE. Prevalence of somatisation and psychologisation among patients visiting primary health care centres in the State of Qatar. Libyan J Med. 2010:5. doi: 10.3402/ljm.v5i0.5266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uutela A. Economic crisis and mental health. Curr Opin Psychiatry. 2010;23:127–30. doi: 10.1097/YCO.0b013e328336657d. [DOI] [PubMed] [Google Scholar]
- 18.Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, et al. Twelve-month prevalence of and risk factors for suicide attempts in the World Health Organization World Mental Health Surveys. J Clin Psychiatry. 2010;71:1617–28. doi: 10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. Int J Psychiatry Med. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- 20.Viana MC, Andrade LH. Lifetime Prevalence, age and gender distribution and age-of-onset of psychiatric disorders in the São Paulo Metropolitan Area, Brazil: Results from the São Paulo Megacity Mental Health Survey. Rev Bras Psiquiatr. 2012;34:249–60. doi: 10.1016/j.rbp.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 21.Bener A, Burgut FT, Ghuloum S, Sheikh J. A study of postpartum depression in a fast developing country: Prevalence and related factors. Int J Psychiatry Med. 2012;43:325–37. doi: 10.2190/PM.43.4.c. [DOI] [PubMed] [Google Scholar]
- 22.Bener A, Gerber LM, Sheikh J. Prevalence of psychiatric disorders and associated risk factors in women during their postpartum period: A major public health problem and global comparison. Int J Womens Health. 2012;4:191–200. doi: 10.2147/IJWH.S29380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liddell BJ, Chey T, Silove D, Phan TT, Giao NM, Steel Z. Patterns of risk for anxiety-depression amongst Vietnamese-immigrants: A comparison with source and host populations. BMC Psychiatry. 2013;13:329. doi: 10.1186/1471-244X-13-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mitchell PB, Johnston AK, Frankland A, Slade T, Green MJ, Roberts G, et al. Bipolar disorder in a national survey using the World Mental Health version of the composite international diagnostic interview: The impact of differing diagnostic algorithms. Acta Psychiatr Scand. 2013;127:381–93. doi: 10.1111/acps.12005. [DOI] [PubMed] [Google Scholar]
- 25.Quintana MI, Mari Jde J, Ribeiro WS, Jorge MR, Andreoli SB. Accuracy of the Composite International Diagnostic Interview (CIDI 2.1) for diagnosis of post-traumatic stress disorder according to DSM-IV criteria. Cad Saude Publica. 2012;28:1312–8. doi: 10.1590/s0102-311x2012000700009. [DOI] [PubMed] [Google Scholar]
- 26.Wittchen HU, Lachner G, Wunderlich U, Pfister H. Test-retest reliability of the computerized DSM-IV version of the Munich-Composite International Diagnostic Interview (M-CIDI) Soc Psychiatry Psychiatr Epidemiol. 1998;33:568–78. doi: 10.1007/s001270050095. [DOI] [PubMed] [Google Scholar]
- 27.Geneva: WHO; 1992. World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- 28.5th ed. Washington (DC): American Psychiatric Association; 1994. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. DSM-5. [Google Scholar]
- 29.Komiti AA, Jackson HJ, Judd FK, Cockram AM, Kyrios M, Yeatman R, et al. A comparison of the Composite International Diagnostic Interview (CIDI-Auto) with clinical assessment in diagnosing mood and anxiety disorders. Aust N Z J Psychiatry. 2001;35:224–30. doi: 10.1046/j.1440-1614.2001.00868.x. [DOI] [PubMed] [Google Scholar]
- 30.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, et al. Concordance of the composite international diagnostic interview version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. 2006;15:167–80. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bener A, Zirie MA, Kim EJ, Al Buz R, Zaza M, Al-Nufal M, et al. Measuring burden of diseases in a rapidly developing economy: State of Qatar. Glob J Health Sci. 2012;5:134–44. doi: 10.5539/gjhs.v5n2p134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bener A, Ghuloum S. Ethnic differences in the knowledge, attitude and beliefs towards mental illness in a traditional fast developing country. Psychiatr Danub. 2011;23:157–64. [PubMed] [Google Scholar]
- 33.Levinson D, Zilber N, Lerner Y, Grinshpoon A, Levav I. Prevalence of mood and anxiety disorders in the community: Results from the Israel National Health Survey. Isr J Psychiatry Relat Sci. 2007;44:94–103. [PubMed] [Google Scholar]
- 34.Cwikel J, Zilber N, Feinson M, Lerner Y. Prevalence and risk factors of threshold and sub-threshold psychiatric disorders in primary care. Soc Psychiatry Psychiatr Epidemiol. 2008;43:184–91. doi: 10.1007/s00127-007-0286-9. [DOI] [PubMed] [Google Scholar]
- 35.Weiller E, Besserbe JC, Maier W. Prevalence of anxiety symptoms in 5 European primary care settings. Br J Psychiatry. 1998;173:18–23. [PubMed] [Google Scholar]
- 36.Jacobi F, Wittchen HU, Holting C, Höfler M, Pfister H, Müller N, et al. Prevalence, co-morbidity and correlates of mental disorders in the general population: Results from the German Health Interview and Examination Survey (GHS) Psychol Med. 2004;34:597–611. doi: 10.1017/S0033291703001399. [DOI] [PubMed] [Google Scholar]
- 37.Lang AJ, Stein MB. Screening for anxiety in primary care: Why bother? Gen Hosp Psychiatry. 2002;24:365–6. doi: 10.1016/s0163-8343(02)00216-5. [DOI] [PubMed] [Google Scholar]
- 38.King M, Nazareth I, Levy G, Walker C, Morris R, Weich S, et al. Prevalence of common mental disorders in general practice attendees across Europe. Br J Psychiatry. 2008;192:362–7. doi: 10.1192/bjp.bp.107.039966. [DOI] [PubMed] [Google Scholar]
- 39.Ghuloum S, Bener A, Abou-Saleh MT. Prevalence of mental disorders in adult population attending primary health care setting in Qatari population. J Pak Med Assoc. 2011;61:216–21. [PubMed] [Google Scholar]


