Abstract
Background:
Monitoring blood utilization helps in effective management of blood stock to meet present and future demands in a hospital. Hence, we analyzed the age, gender and frequency distribution of each blood product used in different diseases conditions.
Materials and Methods:
We included all blood products utilized from January 2008 to December 2012 in our tertiary care hospital in South India. The primary and secondary discharge diagnoses (International Classification of Diseases [ICD-10]) were matched with clinical information provided in the request forms. The most relevant indication requiring blood transfusion was selected for each recipient and grouped into broad diagnostic categories according to the headings of ICD-10. The utilization of stored whole blood, packed red blood cells (RBCs), fresh frozen plasma (FFP) and platelets was stratified according to age, gender and diagnosis.
Results:
Our results indicated decline in usage of whole blood and an increase in use of FFP and platelets over the years. While packed RBCs were frequently used for treating injury and poisoning conditions, platelets and FFP were preferred for infectious and parasitic diseases. Various blood products were used less frequently in patients aged over 60 years and the overall usage of blood products was higher in males.
Conclusion:
The patterns of blood products utilization is in contrast to the Western nations, which may be due to difference in age structure among Indian population and higher prevalence of infectious diseases such as Dengue in our region. Nevertheless, this study highlights the importance of understanding the epidemiology of blood transfusion locally to improve usage of blood and blood products.
Keywords: Blood products, plasma, platelets, red blood cells, transfusion
INTRODUCTION
Blood obtained from voluntary non-remunerated blood donors is a scarce and precious resource, which must be effectively managed and stocked.[1] The patterns of blood transfusion have changed considerably in the recent years due to advances in blood banking techniques, increased frequency of complex surgical procedures, aging populations, initiatives aimed at improving health care standards and a decrease in donor availability because of stringent screening criteria.[1,2] Although several regional and national surveys on usage of blood components have been reported from the Western nations,[1,2,3,4,5,6,7,8] such studies from developing nations like India are lacking. Hence, this study was designed to evaluate the transfusion practices in our hospital over a period of 5 years and analyze the utilization pattern of each blood product based on age group, gender and disease conditions requiring transfusion.
MATERIALS AND METHODS
A retrospective study was planned in our 590-bed tertiary care teaching hospital in Puducherry, South India. Our hospital has most of the medical and surgical specialties. In the present study, all the requests for various blood products from January 2008 to December 2012 were evaluated retrospectively. We collected data for all patients who had been issued stored whole blood, packed red blood cells (RBCs), fresh frozen plasma (FFP), platelets and cryoprecipitate. We included all units cross matched and issued for use. All transfusions included in the study were allogenic. Platelets were prepared from whole blood donation (random donor platelets) during the study period. Some patients had multiple admissions and multiple transfusions for different indications. The clinical data and transfusion details were obtained from the request forms, blood bank records and computerized patient registration information. For each patient, the data included hospital number, age, gender, type and numbers of each blood component issued, date of issue of blood components, diagnosis requiring transfusion and any other relevant details.
The International Classification of Diseases (ICD-10) version was used for classification of the diagnoses requiring transfusion of blood products. We reviewed the primary diagnosis and secondary diagnoses available as ICD-10 codes in our medical record department (MRD). The ICD-10 codes assigned by our MRD for the particular period of care in which the transfusion occurred were matched with the clinical details and diagnosis obtained from the request forms. The most likely diagnosis requiring transfusion was selected. Some request forms lacked a specific diagnosis or the requesting physician had mentioned only a provisional diagnosis which did not tally with the ICD-10 codes for the primary or secondary discharge diagnoses. In such cases the most relevant diagnosis requiring transfusion was selected after a careful review of the clinical details recorded in case files. Though the primary ICD-10 code was chosen as the diagnosis requiring transfusion in majority of the cases, the secondary ICD-10 code proved to be the most appropriate indicator in some cases. The diagnoses were then grouped into broad categories according to the headings of ICD-10 for further analysis.
The data were entered in Microsoft Excel (Microsoft Corp., USA) and analyzed using IBM SPSS Statistics for Windows (version20. 0. Armonk, New York: IBM Corporation).
RESULTS
During the study period, 3876 stored whole blood units, 7137 packed RBC units, 5215 FFP units, 4455 platelet units and nine cryoprecipitate units were issued for use in patients admitted to our hospital. We excluded cryoprecipitate from further analysis since the total number of units was markedly less compared to other blood products. Variation in the usage of whole blood and its components over the 5-year study period is summarized in [Figure 1]. An overall progressive increase in requirement of blood products was evident. While a marked decline in the utilization of whole blood and a significant increase in consumption of FFP and platelets over the years was observed. The following change from 2008 to 2012 for whole blood (33.4-3.9%), RBCs (35.1-32.6%), FFP (20.3-32.3%) and platelets (11.1-31.2%) was observed respectively.
Figure 1.
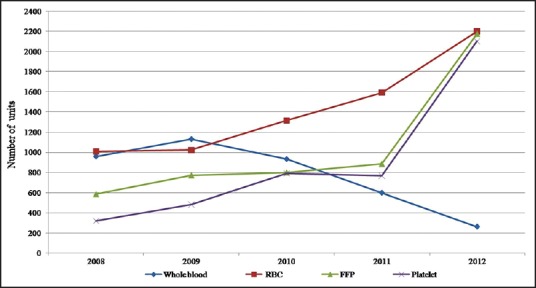
Trends in utilization of whole blood and components from 2008 to 2012
Distribution of blood products used in the diagnosis groups (ICD-10 headings) is represented in [Table 1]. RBCs were used frequently for injury and poisoning conditions (17.9%), circulatory disorders (15.3%), genitourinary diseases (14.1%), blood disorders (13.8%), digestive diseases (10.8%) and neoplasms (6.6%), respectively. Infectious and parasitic diseases (54.2%) were the most important indication for use of platelets transfusion followed by circulatory diseases (18.0%), injury and poisoning (7.3%), disorders of blood (4.1%) and neoplasms (3.8%). FFP was used commonly for infectious and parasitic diseases (31.4%), injury and poisoning (18.7%), disorders of the digestive system (17.6%), circulatory diseases (11.9%), disorders of pregnancy and childbirth (4.0%) and blood disorders (3.8%). Injury and poisoning (38.9%) and circulatory diseases (15.6%) were the most frequent indications for whole blood transfusion. However the utilization of whole blood is currently very minimal in our institute.
Table 1.
Distribution of blood product utilization (percentage of all units in each product) by diagnosis requiring transfusion during the years 2008-2012

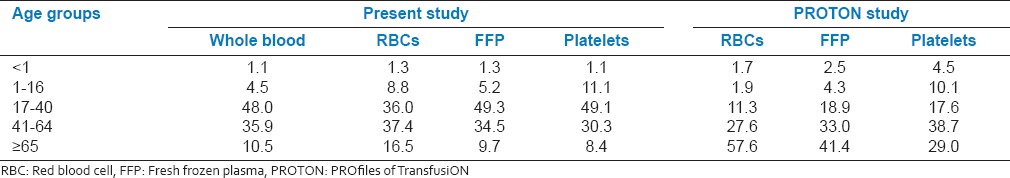
Patients aged 60 years or less had received 85.9% of all whole blood units, 79.1% of RBCs, 86.7% of FFP and 88.8% of platelets during the study period (tabulation not shown). The utilization of blood products in patients aged over 60 years was markedly less compared to the younger age groups. Table 2 compares our utilization by broad age groups with that of the PROTON (PROfiles of TransfusiON recipients) study from the Netherlands.[7]
Table 2.
Distribution of blood products (percentage of all units in each product) by broad age groups – A comparison between the current study and the PROTON study[7]
In our study, males had received 58.1% of whole blood units, 55.7% of RBCs, 67.1% of FFP and 61.1% of platelet units [Table 1]. Analysis by broad ICD-10 headings reveals a variation with respect to gender [Table 1]. Utilization of whole blood, RBCs and FFP for injury and poisoning was significantly higher in males. Similarly FFP utilization was more in males compared with females for the digestive diseases. Platelet and FFP usage for infectious and parasitic diseases were also significantly higher in males. The utilization of whole blood and components was higher in males in most of the categories evaluated in this study.
Figures 2 and 3 reveal a variation of whole blood and components with age and gender. Variation was minimal in pediatric age group. Requirement of RBCs was marginally higher in younger females between 17 and 40 years, mainly related to childbirth. However use of platelets and FFP was higher in younger males. Requirement of whole blood and components was higher in middle aged males between 41 and 64 years as well as in elderly men 65 years or more compared to females in the respective age groups.
Figure 2.
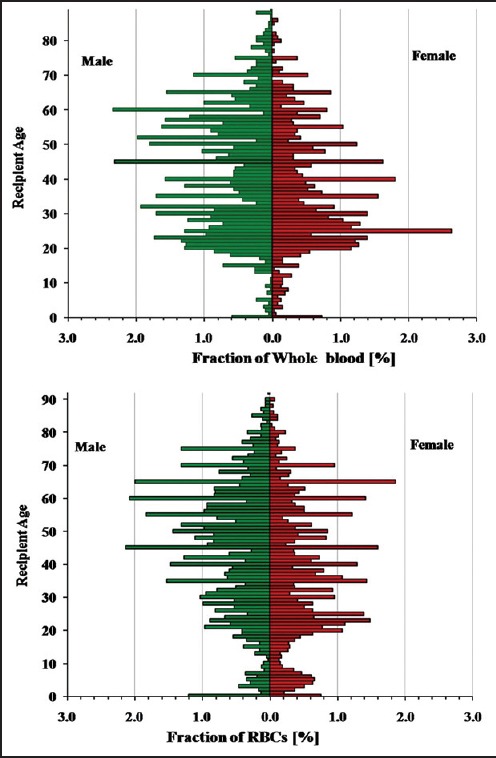
Age distribution of whole blood and red blood cells recipients
Figure 3.
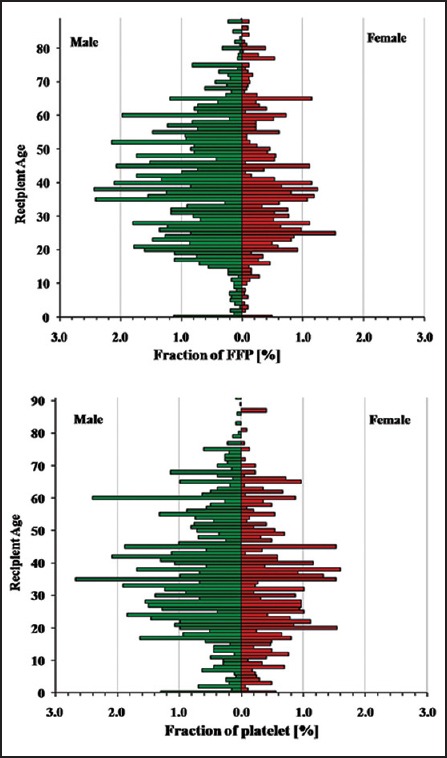
Age distribution of fresh frozen plasma and platelet recipients
DISCUSSION
The previous studies have used either the primary discharge diagnosis ICD code[7,9] or the diagnosis mentioned in preprinted data collection forms for allocation of the indication for transfusion.[4,5,6] The primary ICD code reflects the final discharge diagnosis and can be retrieved with ease in a retrospective study. The request form reflects the actual condition for which transfusion was given. In our pilot study, the clinical data in the request forms was compared with ICD-10 codes as well as details mentioned in case files. We observed that the most appropriate diagnosis requiring transfusion need not be based on the primary ICD-10 code always. Though the request form often reflects the indication of transfusion, the physicians may mention a provisional diagnosis at the time of transfusion or a diagnostic procedure like bone marrow aspiration or histopathological evaluation could subsequently alter the initial diagnosis. Hence instead of choosing the principal code in all the cases, we matched the primary and secondary ICD-10 codes with the clinical details provided in the request form to select the most appropriate condition requiring transfusion.
Western studies generally use computerized systems to match blood products usage with clinical data. This permits easy retrieval and management of enormous quantities of data. Blood banks in developing nations often lack such facilities and depend on paper-based resources, which may account for relative paucity of studies on patterns of blood utilization in developing nations.
We have compared our patterns of utilization of blood products with studies from other high, middle and low income countries, especially the PROTON study from the Netherlands[7] and two institutional studies from Sao Paulo, Brazil[9] and Uganda[10] to understand variations in utilization patterns across countries. The PROTON study has compiled information from 20 centers including general, academic and cancer hospitals.
Though most whole blood units are separated into components in the Western countries, low and middle income countries still continue to utilize whole blood.[10,11,12] Only about 35% blood units are separated into components in India.[11] Component separation is increasing (33.7% in 2006-07-50.5% in 2011-12) in states like Gujarat[13] and National AIDS control organization is supporting the installation of blood component separation units in various states to facilitate component separation and encourage appropriate clinical use of blood. The utilization of whole blood in our hospital is also declining [Figure 1] and accounts for less than 4% of all blood products used in 2012.
A major worry in Western countries is increase in utilization of various components with increasing age among transfusion recipients.[2,4,7,8,14] The dynamic demographic changes in the developed nations pose a tremendous challenge for blood services because ultimately it will become more difficult to recruit blood donors. Small increases in the number of elderly people will have large effects on demand[4] and a 30% increase in RBC transfusion is projected by year 2030.[8] The age structure of blood recipients in our study differs markedly in comparison to the West [Table 2]. The maximal utilization of all products in our study was in the age groups of 21-50 years. The age distribution of transfusion recipients in other developing nations also did not match the trends observed in the Western countries.[9,10,12]
Previous studies have also noted a variation in blood utilization with respect to gender.[7,9] The PROTON study revealed a higher RBC utilization in younger women due to childbirth.[7] Elderly men were transfused more blood products especially FFP due to higher probability of being hospitalized for circulatory diseases in the Netherlands.[7] Males received 62% of all components in the Brazilian study.[9]
The indications for transfusion also vary across countries. The diagnostic categories that used most blood products in the PROTON study were diseases of the circulatory system, neoplasms, injury and poisoning, diseases of the digestive system and disorders of blood.[7] Interestingly platelet and FFP utilization for infectious diseases in the PROTON study was significantly low compared with our study. The common indications in the Brazilian study include neoplasms, diseases of the digestive and circulatory systems and injury and poisoning. Platelets and plasma were used frequently for infectious diseases in the Brazilian study also (13% and 15%, respectively).[9] While malaria (33.1%), non-malarial infections (19.2%) and bleeding (29.6%) especially obstetric hemorrhage and gastrointestinal bleeding were common causes of transfusion in Uganda.[10]
Dengue was the most common infection utilizing about 80% of FFP and 90% of platelets issued for infectious and parasitic diseases in our study. Malaria accounted only for 1.5% of FFP and platelet usage. Dengue is becoming a major health problem in our region. Outbreak of epidemics is associated with a significant increase in requirement of blood components especially platelets. Dengue can also reduce the blood donor pool in endemic regions.[15] Hence clear and specific guidelines for usage of platelets and FFP in dengue are essential to prevent inappropriate usage of these precious blood products especially in areas with limited resources.[15]
The pattern of usage of blood products reflects the relative frequency of various diseases conditions. Infectious diseases are more prevalent in developing countries. Puducherry also happens to be a high accident prone region.[16] This explains the frequent usage of blood components for injuries in our study. Our center is not a specialized cancer care hospital and this could also be related with less utilization of blood components for neoplasms.
The pattern of blood utilization can also vary because of the age composition of the population. Africa, Latin America and South Asia have very young age structures with about half of the population under age 25. The proportion of population above age 65 is much greater in Europe in comparison to Africa and South Asia.[17,18] Figure 4 shows a comparison of age pyramids. Socio-economic factors in the developing world could also hinder elderly people especially women from accessing effective health care facilities. Recent studies on patterns of blood product utilization are lacking in India.
Figure 4.
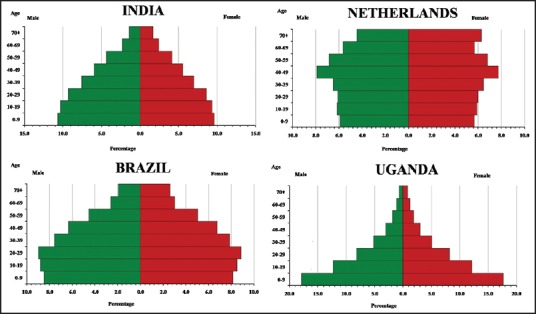
Population pyramids for India, Brazil, Netherlands and Uganda for the year 2010 based on data from “The 2012 Revision of the World Population Prospects,” Published by United Nations[18]
Our study has limitations because our data is derived from a single center and represents only a small proportion of the South Indian population. Well-designed national studies are essential to understand the variation in transfusion practices and formulate guidelines to improve transfusion practices in India. Nevertheless the current study highlights the importance of understanding the epidemiology of blood transfusion locally for planning optimal blood–saving strategies.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Zimmermann R, Büscher M, Linhardt C, Handtrack D, Zingsem J, Weisbach V, et al. A survey of blood component use in a German university hospital. Transfusion. 1997;37:1075–83. doi: 10.1046/j.1537-2995.1997.371098016449.x. [DOI] [PubMed] [Google Scholar]
- 2.Ali A, Auvinen MK, Rautonen J. The aging population poses a global challenge for blood services. Transfusion. 2010;50:584–8. doi: 10.1111/j.1537-2995.2009.02490.x. [DOI] [PubMed] [Google Scholar]
- 3.Titlestad K, Georgsen J, Jorgensen J, Kristensen T. Monitoring transfusion practices at two university hospitals. Vox Sang. 2001;80:40–7. doi: 10.1046/j.1423-0410.2001.00001.x. [DOI] [PubMed] [Google Scholar]
- 4.Wells AW, Mounter PJ, Chapman CE, Stainsby D, Wallis JP. Where does blood go? Prospective observational study of red cell transfusion in north England. BMJ. 2002;325:803. doi: 10.1136/bmj.325.7368.803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wallis JP, Wells AW, Chapman CE. Changing indications for red cell transfusion from 2000 to 2004 in the North of England. Transfus Med. 2006;16:411–7. doi: 10.1111/j.1365-3148.2006.00702.x. [DOI] [PubMed] [Google Scholar]
- 6.Tinegate H, Chattree S, Iqbal A, Plews D, Whitehead J, Wallis JP, et al. Ten-year pattern of red blood cell use in the North of England. Transfusion. 2013;53:483–9. doi: 10.1111/j.1537-2995.2012.03782.x. [DOI] [PubMed] [Google Scholar]
- 7.Borkent-Raven BA, Janssen MP, van der Poel CL, Schaasberg WP, Bonsel GJ, van Hout BA. The PROTON study: Profiles of blood product transfusion recipients in the Netherlands. Vox Sang. 2010;99:54–64. doi: 10.1111/j.1423-0410.2010.01312.x. [DOI] [PubMed] [Google Scholar]
- 8.Bosch MA, Contreras E, Madoz P, Ortiz P, Pereira A, Pujol MM, et al. The epidemiology of blood component transfusion in Catalonia, Northeastern Spain. Transfusion. 2011;51:105–16. doi: 10.1111/j.1537-2995.2010.02785.x. [DOI] [PubMed] [Google Scholar]
- 9.Goncalez TT, Sabino EC, Capuani L, Liu J, Wright DJ, Walsh JH, et al. Blood transfusion utilization and recipient survival at Hospital das Clinicas in São Paulo, Brazil. Transfusion. 2012;52:729–38. doi: 10.1111/j.1537-2995.2011.03387.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Natukunda B, Schonewille H, Smit Sibinga CT. Assessment of the clinical transfusion practice at a regional referral hospital in Uganda. Transfus Med. 2010;20:134–9. doi: 10.1111/j.1365-3148.2010.00992.x. [DOI] [PubMed] [Google Scholar]
- 11.Choudhury N. Blood transfusion in borderless South Asia. Asian J Transfus Sci. 2011;5:117–20. doi: 10.4103/0973-6247.83234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bugge HF, Karlsen NC, Oydna E, Rake MM, Wexels N, Bendabenda vJ, et al. A study of blood transfusion services at a district hospital in Malawi. Vox Sang. 2013;104:37–45. doi: 10.1111/j.1423-0410.2012.01628.x. [DOI] [PubMed] [Google Scholar]
- 13.Ramkishan A, Gupta VK, Koshia HG, Goswami KK, Shah KK, Shah RJ. Effective implementation of regulations and facilitation in improving blood transfusion services in Gujarat state. Asian J Transfus Sci. 2012;6:190–2. doi: 10.4103/0973-6247.98955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cobain TJ, Vamvakas EC, Wells A, Titlestad K. A survey of the demographics of blood use. Transfus Med. 2007;17:1–15. doi: 10.1111/j.1365-3148.2006.00709.x. [DOI] [PubMed] [Google Scholar]
- 15.Teo D, Ng LC, Lam S. Is dengue a threat to the blood supply? Transfus Med. 2009;19:66–77. doi: 10.1111/j.1365-3148.2009.00916.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Radjou AN, Balliga DK, Pal R, Mahajan P. Injury-related mortality audit in a regional trauma center at Puducherry, India. J Emerg Trauma Shock. 2012;5:42–8. doi: 10.4103/0974-2700.93111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bongaarts J. Human population growth and the demographic transition. Philos Trans R Soc Lond B Biol Sci. 2009;364:2985–90. doi: 10.1098/rstb.2009.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Population Prospects: The 2012 Revision, DVD Edition. United Nations, Department of Economic and Social Affairs, Population Division. [Last updated on 2013 Jun 13]. Available from: http://www.esa.un.org/unpd/wpp/Excel-Data/population.htm .


