Abstract
Caries or trauma induced non-vital immature permanent tooth with blunderbuss, thin root which are very common among childrens are corrected using regenerative endodontic (revascularization) procedures. In the presented case, a 16-year-old boy reported with chief complaint of pain in maxillary left central incisor (Tooth #21). Tooth #21 showed grade III mobility, draining labial sinus, and short blunderbuss root with diffuse periapical radiolucency. Patient was explained the treatment plan and written informed consent was taken. Platelet rich fibrin (PRF) was prepared according to standard protocol. Autologous PRF was carried to the apical portion of the root canal after inducing revascularization. Access opening was double sealed with MTA and resin modified glass ionomer cement (RMGI). Baseline, 12 month and 18 month follow-up intraoral radiographs were taken. Clinically case was asymptomatic with complete resolution of intraoral sinus. Periapical healing, apical closure, root lengthening and dentinal wall thickening were uneventful. Thus PRF supplementation hastens the predictability and rate of revascularization in non-vital immature permanent teeth.
Keywords: Open apex, PRF, revascularization
INTRODUCTION
Caries or trauma induced loss of pulp vitality in an immature permanent tooth results in blunderbuss, short root with thin radicular walls. Such cases can be managed by revascularization that lengthens as well as strengthens the thin root walls. In revascularization various biomaterials such ascollagen, platelet rich plasma (PRP) can be used as a scaffold in addition to blood clot.[1] Use of second generation platelet concentrate {platelet rich fibrin (PRF)} as an additional scaffold is a step ahead in the field of revascularization. This case report higlights the use of PRF as an additional scaffold in therevascularization to enhance therapeutic outcome.
CASE REPORT
A 16-year-old healthy boy reported with the chief complaint of pain in upper front teeth. Clinical examination revealed grade III mobility (Millers index of mobility) in maxillary left central incisor (Tooth #21) associated with draining labial sinus. Radiographic examination revealed blunderbuss root apex with very thin radicular dentinal walls and diffuse periapical radiolucency [Figure 1a]. The patient was explained about the risks, complications, and possible outcomes of PRF supplemented revascularization and written informed consent was taken. Under rubber dam isolation, root canal treatment was initiated. After thorough chemo-mechanical preparation, inter-appointment medication of triple antibiotic paste (TAP) was given. Tooth #21 was stabilized using rigid splinting. Patient was recalled after 3 weeks when sinus resolved completely.
Figure 1.
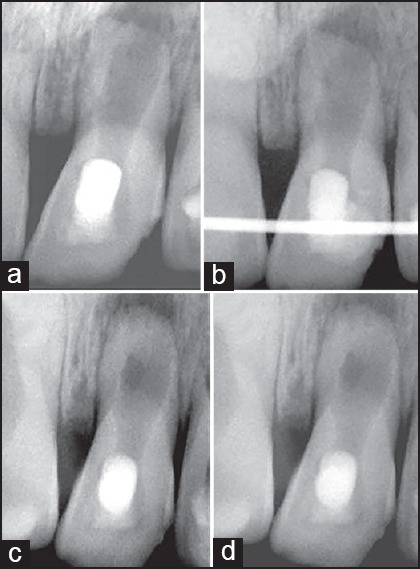
(a) Tooth #21 exhibited blunderbuss root apex with very thin radicular dentinal walls and diffuse periapical radiolucency. (b) It was stabilised using rigid splinting and PRF aided revascularization was carried out. (c), (d). 12 month and 18 month follow up radiographs revealed excellent periapical healing, apical closure, root lengthening and dentinal wall thickening.
PRF was prepared by centrifugating patients own blood at 3000 rpm for 12 min. Revascularization was carried out according to standard protocol.[2] Autologus PRF was introduced into the pulp chamber with the help of sterile cotton pliers and carried to the apical portion witha size # 40 finger plugger (Sybronendo, CA, USA). Access opening was sealed with MTA and Resin Modified Glass Ionomer Cement (Photac-Fill, 3MESPE, Minnesota). Intraoral radiographs were taken at baseline, 12 and 18 month post procedure [Figure 1b–d]. At 18 month follow up, case was asymptomatic with complete resolution of intraoral sinus. Tooth mobility was reduced. Interestingly, periapical healing, apical closure, root lengthening and dentinal wall thickening was optimal radiographically [Figure 1d].
DISCUSSION
Immature non-vital permanent teeth with thin fragile radicular walls are difficult to manage with the conventional root canal procedure. In such cases, revascularization is a viable treatment option. The success of revascularization depends upon methodical disinfection, use of a suitable scaffold and a good coronal seal. In the presented case, a double seal of RMGI and MTA was used. MTA placed directly over the PRF clot had two-fold benefits; moisture from PRF helped in the setting of MTA and MTA provided signalling molecules for the growth of the stem cells.[3]
In the revascularization, scaffold is essential to support the in-growth of new tissue from the periapical area and to provide an environment for cell growth and differentiation. Platelet rich fibrin, an autologous leukocyte and platelet rich fibrin biomaterial, is aninnovative advancement in the field of regenerative medicine. Use of PRF as a scaffold in revascularization has several advantages. It can be easily prepared, avoids the biochemical handling of blood andrequires only single centrifugation cycle. It forms an organized fibrin network where the platelets and leukocytes are concentrated leading to sustained release of various growth factors like platelet-derived growth factor-AB, transforming growth factor-1, and vascular endothelial growth factors over a prolonged period of time.[4] These growth factors can stimulate scaffold remodelling, proliferation of undifferentiated mesenchymal stem cells like dental pulp stem cells (DPSC) and promote angiogenesis.[5] Moreover, the natural fibrin of PRF also protects the growth factors from proteolysis. PRF clot traps all important circulating immune cells and different cytokinesthat act against infection.[4]
Thus supplementation of revascularization with PRF improves its regenerative outcome. However, randomized long term prospective clinical studies are needed to establish PRF supplements in revascularization as a routine protocol.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Jadhav G, Shah N, Logani A. Revascularization with and without Platelet-rich Plasma in Nonvital, Immature, Anterior Teeth: A Pilot Clinical Study. J Endod. 2012;38:1581–7. doi: 10.1016/j.joen.2012.09.010. [DOI] [PubMed] [Google Scholar]
- 2.Jadhav GR, Shah N, Logani N. Platelet-Rich plasma supplemented revascularization of an immature tooth associated with a periapical lesion in a 40-year-old man. Case Rep Dent 2014. 2014 doi: 10.1155/2014/479584. 479584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torabinejad M, Parirokh M. Mineral trioxide aggregate: A comprehensive literature review--part II: Leakage and biocompatibility investigations. J Endod. 2010;36:190–202. doi: 10.1016/j.joen.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part IV: Clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e56–60. doi: 10.1016/j.tripleo.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 5.Wirthlin MR. The current status of new attachment therapy. J Periodontol. 1981;52:529–44. doi: 10.1902/jop.1981.52.9.529. [DOI] [PubMed] [Google Scholar]


