Abstract
Diarrhea is the third leading cause of childhood mortality in India, and is responsible for 13% of all deaths/year in children under 5 years of age. Information on diarrheal diseases, its determinants and preventive and control strategies need to be reviewed for better planning and organization of health services. This study reviewed literature on diarrheal disease control among under-five children in India from literature published in PubMed, Google search engine and other databases on the internet. Data were described in terms of disease burden in India, determinants, management and intervention strategies, preventive strategies, and role of public health and scope for future action. This review calls for a comprehensive diarrheal disease control strategy, through improved case management, addressing social determinants of health and research in the field of cost-effective interventions to reduce the burden of diarrhea among children in India. With < almost one year left to reach the 2015 Millennium Development Goal on reducing child mortality, progress on control of diarrheal diseases must be accelerated.
Keywords: Diarrheal disease control, diarrheal diseases, India, under-five children
INTRODUCTION
India has made steady progress in reducing deaths in children younger than 5 years, with total deaths declining from 2.5 million in 2001 to 1.5 million in 2012.[1] This remarkable reduction was possible due to the inception and success of many universal programs like expanded program on immunization, program for the control of diarrheal diseases and acute respiratory infection. Even though the deaths among children under-5 years have declined, the proportional mortality accounted by diarrheal diseases still remains high. Diarrhea is the third most common cause of death in under-five children, responsible for 13% deaths in this age-group, killing an estimated 300,000 children in India each year.[2] Information on diarrheal diseases, its determinants in India and preventive and control strategies in light of recent developments need to be reviewed for better planning and organization of health services within the community.
MATERIALS AND METHODS
Identification of studies
We searched PubMed, Google search engine and other databases on the internet for articles on topics related to diarrheal diseases in India, published before 2012. We searched reference lists of all primary and review articles based on the key words “diarrheal diseases, India, problem burden, determinants, intervention strategies, and control program.” Eligibility criteria for studies included in review: Studies were included in the review if they reported the problem burden, determinants, and management strategies for diarrheal diseases in India.
Screening process
Initially, both authors reviewed the full citation list independently and then came to a consensus on 22 potentially relevant abstracts for retrieval. Next, both authors read all the abstracts and full papers that appeared potentially eligible to either, or both of them. Both authors then reached a consensus on ten papers from which to extract data.
Data extraction
Data regarding diarrheal diseases in India was collected, summarized and analyzed. Data concerning the study design, sample size, location, study population, and measures of effect were abstracted and tabulated independently by both authors. Information was described in terms of problem burden, determinants, management and intervention strategies, preventive strategies and role of public health and scope for future action for diarrheal disease control among under-five children in India.
RESULTS
Problem burden and determinants
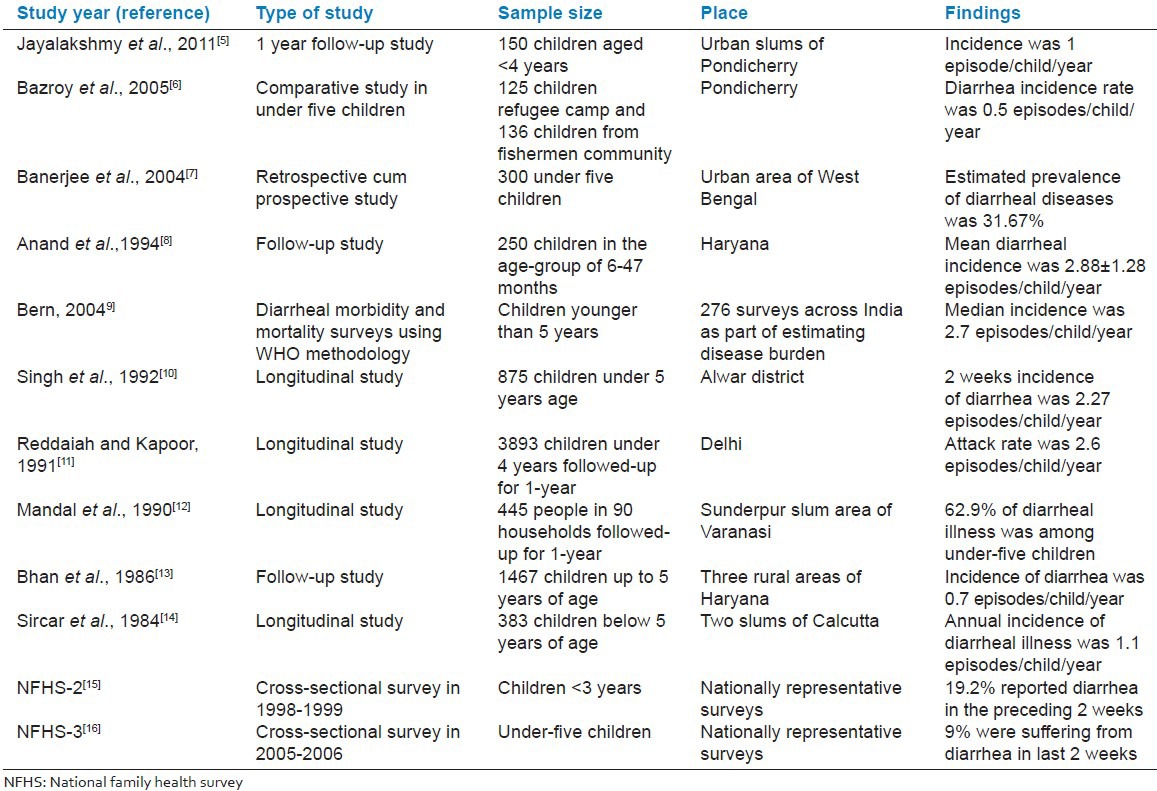
Globally, four billion episodes of diarrhea were estimated to occur each year, with > 90% occurring in developing countries. Diarrheal disease is an important public health problem among under-five children in developing countries. Total diarrheal deaths in India among children aged 0-6 years was estimated to be 158,209 and proportionate mortality due to diarrhea in this age-group was 9.1%. Average estimated incidence of diarrhea in children aged 0-6 years was 1.71 and 1.09 episodes/person/year in rural and urban areas.[3] According to National Family Health Survey-3 (NFHS-3) report, 9% of all under-five children were reported to be suffering from diarrhea in last 2 weeks.[4] Studies have shown that the incidence of acute diarrheal diseases was as low as 1 episode/child/year in some urban areas.[5] Table 1 shows the incidence of acute diarrheal disease in children as reported from studies done across India.
Table 1.
Burden of diarrheal diseases among children in India
Young age, low socioeconomic status, poor maternal literacy, presence of under-five sibling in the family, birth weight, inadequate breastfeeding, malnutrition, poor sanitation and hygiene practices of the mother are associated with a higher incidence of diarrheal diseases in young children.[17] Children belonging to poor socioeconomic status had a higher diarrheal incidence than the better socioeconomic group.[18] Educational status of the mother showed a positive correlation with the incidence of diarrheal diseases.[10] Studies have shown that families with more than one child had an attack rate for diarrheal diseases that was 22-70% higher than in houses with just one child < 5 year old.[11] Though the nutritional status of children is a well-known determinant of diarrhea, frequency of diarrhea was not significantly greater in those who were underweight or stunted compared with well-nourished children in a few studies.[5,8]
Incidence of diarrheal diseases was observed to be maximum during the summer months followed by rainy or winter months.[5,19] Poor sanitation and unhygienic conditions are important risk factors for diarrhea. Mode of water transportation, and poor handling of water at the household level, presence of wastewater in the street, refuse storage, collection and disposal, domestic water reservoir conditions, faeces disposal and presence of vectors predispose the under-five children to diarrhea.[20,21] Indiscriminate stool disposal by the mothers, lack of hand-washing before feeding their children and hand-washing without soap were associated with increased risk.[5,22]
Management strategies
Current guidelines for management of diarrhea by the Ministry of Health and Family Welfare, Government of India, recommend low osmolarity oral rehydration salt solution (ORS), zinc and continued feeding of energy dense feeds in addition to breastfeeding. Oral rehydration therapy (ORT) with ORS remains the cornerstone of appropriate case management of diarrheal dehydration and is considered the single most effective strategy to prevent diarrheal deaths in children.[23] Knowledge of ORS/ORT among mothers of under-five children in India is good (73%), but there is a big gap between knowledge and practice as reflected in poor ORS usage rates (43%).[4]
Zinc supplementation (10 mg of elemental zinc for 14 days for children aged 2-6 months and 20 mg/day for older children) has the potential to reduce morbidity and mortality by reducing the duration and severity of diarrheal episodes and lowering their incidence.[24] Though it is distributed under the National Rural Health Mission (NRHM), very low coverage of zinc prescription has been documented, due to lack of knowledge and awareness among the care providers. Compliance with the use of zinc for 14 days and scaling up of zinc use in communities need to be examined to evaluate its impact on diarrhea management.[25] Antimicrobials are recommended in diarrheal diseases only for gross blood in stools or Shigellapositive culture, cholera, associated systemic infection, or severe malnutrition. However, unwarranted antidiarrheal drugs and injections are prescribed frequently in the community as reported in NFHS-3 survey, where 16% and 30% children were treated with antibiotics and “unknown” drugs, respectively.[4]
Preventive strategies and role of public health
Measures for prevention of diarrheal diseases include the use of safe water, hand-washing, food safety, safe disposal of excreta, promoting exclusive breastfeeding and immunization against measles. Vitamin A supplementation does not reduce the incidence of diarrhea or diarrhea-related mortality in neonates and children < 6 months, but there is a benefit in children aged 6-59 months.[24]
Lack of toilets remains one of the leading causes of illness and death among children. According to United Nations Children's Fund report (UNICEF), 626 million people in India practice open defecation. Poor sanitation, lack of access to clean water, and inadequate personal hygiene are responsible for an estimated 88% of childhood diarrhea in India.[26] Though the sanitation coverage in India is 59%, there is a huge disparity in terms of use of toilets in the rural-urban areas (34% and 80%, respectively). However, there have been significant improvements in households using toilets in rural areas during the last 10 years. India has reached the Millenium Development Goal (MDG) 7 target on improved drinking water sources with 86% coverage, however, the piped water as a drinking water source has remained as 24%.[26]
Hand-washing before preparing food is a particularly important opportunity to prevent childhood diarrhea and it works best when it is part of a package of behavior change interventions. Washing hands after defecating or handling children's feces and before handling food entails an average of 32 hand washes a day and consumes 20 l of water.[27] Based on current evidence, washing hands with soap can reduce the risk of diarrheal diseases by 42-47%.[28] A survey conducted by UNICEF in 2005 on well-being of children and women had shown that only 47% of rural children in the age-group 5-14 wash hands after defecation.[26] Although the interventions promoting hand-washing and other hygiene measures clearly show a reduction in diarrheal risk in the short term, sustainability of hand-washing behavior in the communities and the benefits of upscaling interventions need to be studied, as India-specific data are scarce.[24] Hand-washing with soap before eating and after defecation, is being promoted among children in India through the school hygiene program and mass media campaign on “the hand-washing day.” Similarly World Toilet Day is an occasion to sensitise the community on the ill-effects of open air defecation and popularizing government programs.
Programs should aim to make all communities free of open defecation by focusing on social and behavior change and the use of affordable, appropriate technologies. Emphasis should be laid on the sustainable use of sanitation facilities rather than the construction of infrastructure, through involvement of a variety of stakeholders. As per the total sanitation campaign program in India, communities take a central role in planning and implementing improved sanitation with assistance from the Government. There is a need for prioritisation of certain interventional strategies with respect to environmental sanitation in India.[29] The possibility of faecal contamination is maximum in poor urban areas where insufficient water supply and sanitation coverage combine with overcrowded conditions. Therefore, particular attention should be devoted to extending services to slums and informal settlements.[26] Launching of the National Diarrheal Diseases Control Programme in 1978, has reduced child mortality from diarrhea by 50% between 1981 and 1990. In 1985-1986, the focus shifted to strengthening case management of diarrhea for children under age of 5 years and national ORT program was introduced. Subsequently, it became part of child survival and safe motherhood program in 1992 and reproductive and child health (RCH) programme in 1997. Integrated Management of Neonatal and Childhood Illnesses has been implemented under RCH phase II, in 223 of India's 640 districts, and more than 200,000 workers had been trained since 2003.[30] NRHM reaches out to underserved areas through health programs such as the Village Health and Nutrition Days. During these nutrition and health education sessions organized by the auxiliary nurse midwife and anganwadi workers, use of ORT is popularized among the community members.
Scope for future action
Overall, the steady decline in under-five mortality in a large country like India is laudable; however, acceleration through greater investment, focus, and innovation is needed in regions and districts that are doing less well.[1] Inclusion of Rotavirus vaccination of infants into national immunization programs has been recommended in areas where under-five mortality due to diarrheal diseases is > 10%.[31] The vaccine for rota virus has been launched in 62 countries and has been included the national immunization schedule in 11 countries. Though introduction of rotavirus vaccine into the national immunization program of India at an affordable price would be a cost-effective way to reduce morbidity and mortality, there is a need for sufficient and reliable efficacy and effectiveness data from the country.[32]
Apart from improved case management strategies, measures like environmental sanitation, health promotion and preventive practices like breastfeeding and use of clean drinking water are essential to reduce transmission of diarrheal diseases. Addressing other social determinants of health with respect to diarrheal diseases, poverty alleviation efforts in concert with programs to educate women and girls are necessary measures for improving overall children's health and reducing diarrheal mortality.
Continued investment in diarrheal disease research across the spectrum of basic, social and behavioral issues is essential. To refocus health research to target disease-burden reduction, the Child Health and Nutrition Research Initiative developed a systematic strategy to rank health research options. The research options receiving the highest priority score addressed health policy and systems research, cost-effectiveness of rotavirus vaccines and educational/behavior modification studies to improve the deliverability of zinc treatment in diarrhea. Such prioritization of research options has important implications for the assignment of available funds that are intended for the control of diarrheal disease.[33]
Millenium Development Goal 4 targets minimizing under-five mortality (by two thirds) to 39/1000 live births by 2015 and the average annual rate of decline at 3.1% in India was considered insufficient.[34] In the current circumstances, when several complementary interventions are packaged together and delivered through a range of health-care providers, the main bottlenecks are to ensure improved service delivery.[35] With < one year left to reach the 2015 MDG target on reducing child mortality, progress on control of diarrheal diseases must be accelerated.
CONCLUSION
Despite gains in controlling mortality relating to diarrheal disease, the burden of the disease remains unacceptably high. Reviewing current scenario presents an unprecedented opportunity to save many more children. Focus on comprehensive diarrheal disease control strategy through improved case management, addressing social determinants of health like environmental sanitation and clean drinking water, health promotion regarding preventive practices like breastfeeding and research in the field of cost-effective interventions is crucial to reduce the burden of diarrhea among children in India.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Bhan MK. Accelerated progress to reduce under-5 mortality in India. Lancet Glob Health. 2013;1:e172–3. doi: 10.1016/S2214-109X(13)70076-7. [DOI] [PubMed] [Google Scholar]
- 2.Million Death Study Collaborators. Bassani DG, Kumar R, Awasthi S, Morris SK, Paul VK, et al. Causes of neonatal and child mortality in India: A nationally representative mortality survey. Lancet. 2010;376:1853–60. doi: 10.1016/S0140-6736(10)61461-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.New Delhi, India: National Commission on Macroeconomics and Health, Ministry of Health and Family Welfare, Govt. of India; 2005. Report of the National Commission on Macroeconomics and Health. Estimation of burden of diarrheal diseases in India. In: NCMH Background Papers: Burden of Diseases in India; pp. 182–7. [Google Scholar]
- 4.I. Mumbai: IIPS; 2007. [Last accessed on 21 May 2014]. International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06: India. Available from: http://www.rchiips.org/NFHS/report.shtml . [Google Scholar]
- 5.Jayalakshmy R, Roy G, Premarajan KC. Incidence and risk factors of acute diarrheal disease among under-five children in urban slums in Pondicherry z— One year follow-up study. Indian J Matern Child Health. 2011;13:1–11. [Google Scholar]
- 6.Bazroy J, Panda P, Purty AJ, Philip B. Refugee children in India: A comparative study. Hong Kong J Paediatr. 2005;10:101–8. [Google Scholar]
- 7.Banerjee B, Hazra S, Bandyopadhyay D. Diarrhea management among under fives. Indian Pediatr. 2004;41:255–60. [PubMed] [Google Scholar]
- 8.Anand K, Sundaram KR, Lobo J, Kapoor SK. Are diarrheal incidence and malnutrition related in under five children? A longitudinal study in an area of poor sanitary conditions. Indian Pediatr. 1994;31:943–8. [PubMed] [Google Scholar]
- 9.Bern C. Diarrhoeal diseases. In: Christopher JL, Murray AD, Lopez CD, editors. Global Epidemiology of Infectious Diseases. Geneva: WHO; 2004. pp. 1–27. [Google Scholar]
- 10.Singh J, Gowriswari D, Chavan BR, Patiat RA, Debnath AC, Jain DC, et al. Diarrhoeal diseases amongst children under five. A study in rural Alwar. J Commun Dis. 1992;24:150–5. [PubMed] [Google Scholar]
- 11.Reddaiah VP, Kapoor SK. Epidemiology of diarrhea and its implications for providing services. Indian J Pediatr. 1991;58:205–8. doi: 10.1007/BF02751121. [DOI] [PubMed] [Google Scholar]
- 12.Mandal AK, Tiwari IC, Sanyal SC. A profile of diarrhoea in an urban slum area. Indian J Public Health. 1990;34:66–7. [PubMed] [Google Scholar]
- 13.Bhan MK, Arora NK, Ghai OP, Ramachandran K, Khoshoo V, Bhandari N. Major factors in diarrhoea related mortality among rural children. Indian J Med Res. 1986;83:9–12. [PubMed] [Google Scholar]
- 14.Sircar BK, Deb BC, Sengupta PG, Mondal S, De SP, Sen D, et al. A longitudinal study of diarrhoea among children in Calcutta communities. Indian J Med Res. 1984;80:546–50. [PubMed] [Google Scholar]
- 15.I. Mumbai: International Institute for Population Sciences; 2000. International Institute for Population Sciences (IIPS) and ORC Macro. National Family Health Survey (NFHS-2), 1998-99: India. [Google Scholar]
- 16.I. Mumbai: International Institute for Population Sciences; 2007. International Institute for Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-06: India. [Google Scholar]
- 17.Park K. Textbook of Preventive and Social Medicine. 19th ed. Jabalpur, India: Banarsidas Bhanot; 2007. Epidemiology of communicable disease; pp. 142–7. [Google Scholar]
- 18.Gupta P, Murali MV, Seth A. Epidemiology of diarrhea in urban slums. Indian Pediatr. 1998;35:147–51. [PubMed] [Google Scholar]
- 19.Gupta N, Jain SK, Ratnesh, Chawla U, Hossain S, Venkatesh S. An evaluation of diarrheal diseases and acute respiratory infections control programmes in a Delhi slum. Indian J Pediatr. 2007;74:471–6. doi: 10.1007/s12098-007-0080-4. [DOI] [PubMed] [Google Scholar]
- 20.Simiyu S. Water risk factors pre-disposing the under five children to diarrhoeal morbidity in Mandera district, Kenya. East Afr J Public Health. 2010;7:353–60. doi: 10.4314/eajph.v7i4.64761. [DOI] [PubMed] [Google Scholar]
- 21.Kumar SG, Subitha L. Diarrhoeal diseases in developing countries: A situational analysis. Kathmandu Univ Med J (KUMJ) 2012;10:83–8. doi: 10.3126/kumj.v10i2.7351. [DOI] [PubMed] [Google Scholar]
- 22.Ghosh S, Sengupta PG, Mondal SK, Banu MK, Gupta DN, Sircar BK. Risk behavioural practices of rural mothers as determinants of childhood diarrhoea. J Commun Dis. 1997;29:7–14. [PubMed] [Google Scholar]
- 23.Bhatnagar S, Lodha R, Choudhury P, Sachdev HP, Shah N, Narayan S, et al. IAP Guidelines 2006 on management of acute diarrhea. Indian Pediatr. 2007;44:380–9. [PubMed] [Google Scholar]
- 24.Shah D, Choudhury P, Gupta P, Mathew JL, Gera T, Gogia S, et al. Promoting appropriate management of diarrhea: A systematic review of literature for advocacy and action: UNICEF-PHFI series on newborn and child health, India. Indian Pediatr. 2012;49:627–49. doi: 10.1007/s13312-012-0134-1. [DOI] [PubMed] [Google Scholar]
- 25.Bajait C, Thawani V. Role of zinc in pediatric diarrhea. Indian J Pharmacol. 2011;43:232–5. doi: 10.4103/0253-7613.81495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The situation of children in India – A profile. [Last cited on 2013 Mar 11]. Available from: http://www.unicef.org/india/health.html .
- 27.Graeff JA, Elder JP, Booth EM. San Francisco, CA: Jossey Bass; 1993. Communication for Health and Behavior Change: A Developing Country Perspective. [Google Scholar]
- 28.Curtis V, Cairncross S. Effect of washing hands with soap on diarrhoea risk in the community: A systematic review. Lancet Infect Dis. 2003;3:275–81. doi: 10.1016/s1473-3099(03)00606-6. [DOI] [PubMed] [Google Scholar]
- 29.Kumar GS, Kar SS, Jain A. Health and environmental sanitation in India: Issues for prioritizing control strategies. Indian J Occup Environ Med. 2011;15:93–6. doi: 10.4103/0019-5278.93196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhandari N, Mazumder S, Taneja S, Sommerfelt H, Strand TA IMNCI Evaluation Study Group. Effect of implementation of Integrated Management of Neonatal and Childhood Illness (IMNCI) programme on neonatal and infant mortality: Cluster randomised controlled trial. BMJ. 2012;344:e1634. doi: 10.1136/bmj.e1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Verma R, Khanna P, Chawla S. Rotavirus vaccine can save millions of children's lives in developing countries. Hum Vaccin Immunother. 2012;8:272–4. doi: 10.4161/hv.18390. [DOI] [PubMed] [Google Scholar]
- 32.Lodha R, Shah D. Prevention of rotavirus diarrhea in India: Is vaccination the only strategy. Indian Pediatr. 2012;49:441–3. [PubMed] [Google Scholar]
- 33.Kosek M, Lanata CF, Black RE, Walker DG, Snyder JD, Salam MA, et al. Directing diarrhoeal disease research towards disease-burden reduction. J Health Popul Nutr. 2009;27:319–31. doi: 10.3329/jhpn.v27i3.3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.New York, USA: UNICEF; 2010. United Nations Children's Fund. Levels & nds in Child Mortality. Estimates Developed by the UN Inter-Agency Group for Child Mortality Estimation. [Google Scholar]
- 35.Kumar C, Singh PK, Rai RK. Under-five mortality in high focus states in India: A district level geospatial analysis. PLoS One. 2012;7:e37515. doi: 10.1371/journal.pone.0037515. [DOI] [PMC free article] [PubMed] [Google Scholar]


