Abstract
Cervical pregnancy is a rare type of ectopic pregnancy and it represents <1% of all ectopic pregnancies. Early diagnosis and medical management with systemic or local administration of methotrexate is the treatment of choice. If the pregnancy is disturbed, it may lead to massive hemorrhage, which may require hysterectomy to save the patient. We report three cases of cervical pregnancy managed successfully with different approaches of management. Our first case, 28 years old G3P2L2 with previous two lower segment cesarean sections, presented with bleeding per vaginum following 6 weeks of amenorrhea. Clinical examination followed by transvaginal ultrasound confirmed the diagnosis of cervical pregnancy. Total abdominal hysterectomy was done in view of intractable bleeding to save the patient. The second case, a 26-year-old second gravida with previous normal vaginal delivery presented with pain abdomen and single episode of spotting per vaginum following 7 weeks of amenorrhea. Transvaginal ultrasound revealed empty endometrial cavity, closed internal os with gestational sac containing live fetus of 7 weeks gestational age in cervical canal and she was treated with intra-amniotic potassium chloride followed by systemic methotrexate. Follow up with serum beta human chorionic gonadotropin level revealed successful outcome. Our third case, a 27-year-old primigravida with history of infertility treatment admitted with complaints of bleeding per vaginum for 1 day following 8 weeks amenorrhea. She was diagnosed as cervical pregnancy by clinical examination, confirmed by transvaginal ultrasonography and subsequently managed by dilation and curettage with intracervical Foleys’ ballon tamponade.
Keywords: Cervical pregnancy, ectopic pregnancy, hysterectomy
INTRODUCTION
Cervical ectopic pregnancy is the implantation of blastocyst in the intracervical canal. The incidence of cervical pregnancy is 1:1,000-95,000.[1] Cervical pregnancy are high risk cases as they may present with an unexpected life-threatening hemorrhage secondary to the erosion of cervical blood vessels, which may require hysterectomy to save the patient. Early diagnosis and nonsurgical management with local and systemic methotrexate helps in decreasing maternal mortality and morbidity.
CASE REPORTS
Case 1
A 28-year-old G3P2L2 with previous two lower segment cesarean sections, presented to our casualty with complaint of painless bleeding per vaginum of 1 day duration following 6 weeks of amenorrhea. Her urine pregnancy test was detected positive 2 days ago following which she had taken some medication for induction of abortion. General examination revealed severe pallor with tachycardia and blood pressure of 90/60 mmHg. No abnormality was detected in system examination. Local examination revealed active bleeding from external cervical os. On gentle per vaginum examination, there was ballooning of cervix with a patulous external os. Transvaginal scan revealed empty uterine cavity with endometrial thickness 8 mm, closed internal os with product of conception in the cervical canal. Both the ovaries and tubes were normal and there was no free fluid in pouch of Douglas. Serum beta human chorionic gonadotropin (hCG) level was 84,543 mIU/ml at that point of time. Provisional diagnosis of cervical pregnancy was made. She was resuscitated with intravenous fluid and blood transfusion. The condition of the patient gradually deteriorated due to intractable bleeding. Emergency laparotomy followed by total abdominal hysterectomy was done in order to save the patient. Hysterectomy specimen shows hemorrhagic necrosed product of conception adherent in the intracervical canal [Figure 1]. Postoperative period was uneventful. Histopathology report confirmed the diagnosis.
Figure 1.
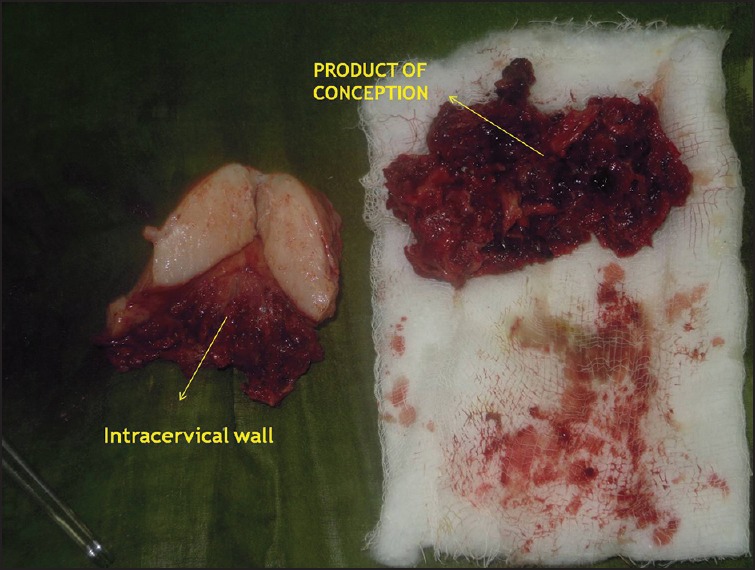
Cut section of uterus showing product of conception adherent to cervical wall
Case 2
Our second case is about a 26-year-old second gravida having previous normal vaginal delivery presented with pain abdomen and one episode of spotting per vaginum following 7 weeks of amenorrhea. General and systemic examination revealed no abnormality. On per vaginum examination, uterus size could not be elicited; there was ballooning of the cervix and partially open external os. Transvaginal ultrasonography revealed empty uterine cavity with endometrial thickness 7 mm, closed internal os and a gestational sac containing live fetus with 7 weeks gestational age [Figure 2]. Color Doppler showed peritrophoblastic blood flow [Figure 3]. Both the ovaries and tubes were normal. On further evaluation, complete blood counts were within normal limits. Serum beta hCG was 74, 014 mIU/ml. After counseling the patient about the risk-benefit ratio, she was planned for conservative management. Ultrasound guided intra-amniotic potassium chloride was administered following which absent cardiac activity was observed in the fetus. Methotrexate was given intramuscularly in a dose of 1.0 mg/kg body weight on day 1, 3, 5, and 7 interspaced with 0.1 mg/kg of leucoverin. She was followed-up with serum beta hCG weekly and the level became normal within 5 weeks. Follow-up scan revealed complete resolution.
Figure 2.
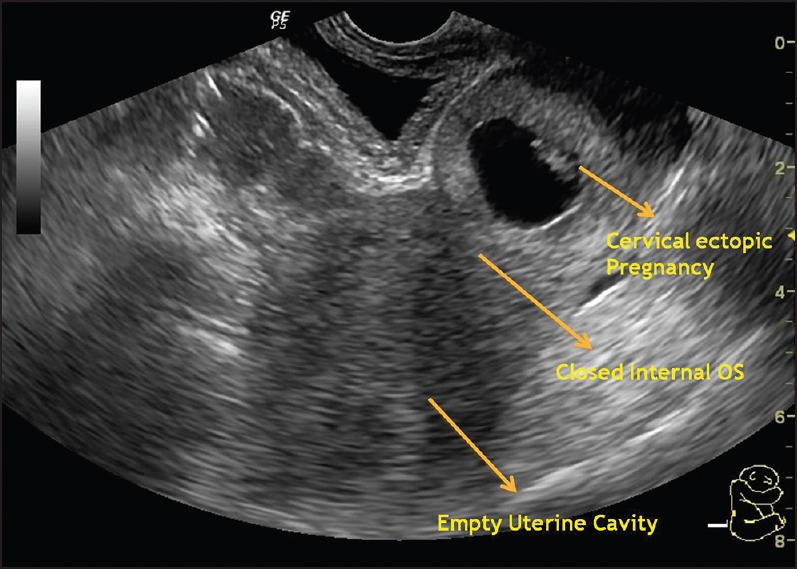
“Hour glass” appearance of uterus, closed internal os and gestational sac containing live embryo in intracervical canal
Figure 3.
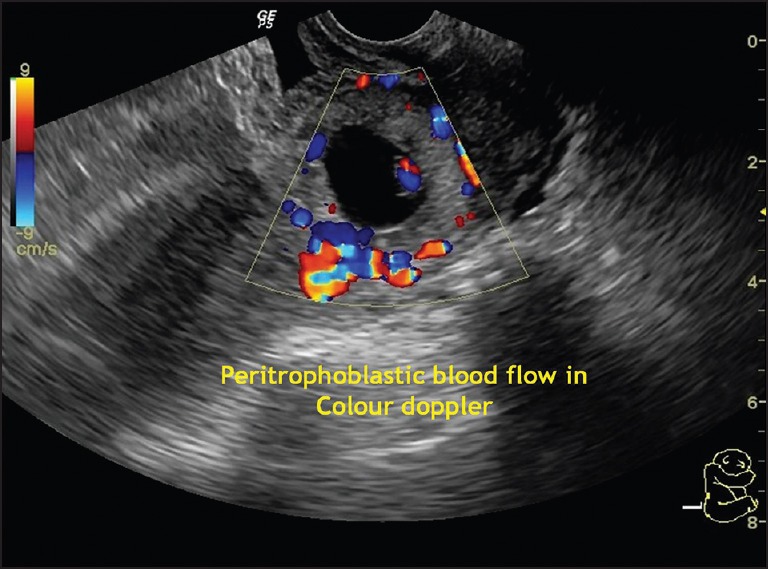
Color doppler showing peritrophoblastic blood flow
Case 3
A 27-year-old primigravida referred from local hospital as a case of missed abortion and presented with mild bleeding per vaginum of 1 day duration following 8 weeks amenorrhea. She was married since 6 years and there was history of treatment for primary infertility. She had an outside ultrasonography report showing single irregular gestational sac in the uterine cavity with no fetal pole. Cervix and bilateral adnexa were reported normal and she was diagnosed as missed abortion. Clinical examination revealed ballooning of cervix with partially open external os. Blood investigation reports were within the normal limits. Serum beta hCG level was 1047 mIU/ml at that point of time. Transvaginal ultrasound scan revealed empty uterine cavity with endometrial thickness 13 mm, closed internal os and a heterogenous space occupying lesion of size 4 cm × 4 cm [Figure 4]. Provisional diagnosis of cervical pregnancy was made. In ward, the patient suddenly started bleeding profusely. After counseling, informed consent was taken for dilation and curettage and for exploratory laparotomy and hysterectomy if required. Under local anesthesia, gentle cervical curettage was done followed by insertion of a no. 18 Foleys’ catheter with 40 ml saline inflated in the cervical canal to control bleeding by tamponade effect. Hemostasis was achieved finally but she required 3 units of blood and 1 unit of fresh frozen plasma transfusion. Foleys’ catheter was removed after 24 h. Postoperative period was uneventful. Single dose of 50 mg methotrexate was given intramuscularly. Histopathology report confirmed presence of chorionic villi and decidual tissue with cervical stroma and glands. Patient was discharged on the 3rd day and advised for weekly follow-up with serum Beta hCG report. Beta hCG level was 168 mIU/ml and 4 mIU/ml at 2 weeks and 2 months after the procedure. The patient resumed her normal periods after 2 months.
Figure 4.
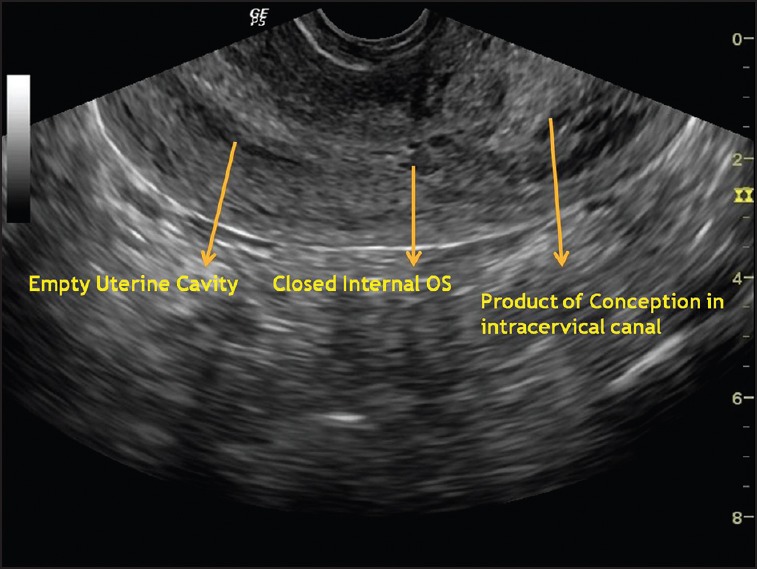
Empty uterine cavity, closed internal os with product of conception in the intracervical canal
DISCUSSION
Common risk factors for cervical pregnancy are prior dilatation and curettage, prior caesarean section and in vitro fertilization.[2] In our first case, the patient had history of two previous caesarean sections and in the third case history of infertility treatment with assisted reproductive technique. The most common symptom is vaginal bleeding following a period of amenorrhea which is often painless and at times massive bleeding can occur which may even require hysterectomy to save the patient as observed in our first case. In 1911, Rubin[3] proposed three anatomical and histological criteria for the diagnosis of cervical pregnancy, which can be established in a hysterectomy specimen. Paalman and McElin[4] in 1959 proposed five more clinically practical criteria which includes:
Uterine bleeding without cramping pain following a period of amenorrhea
A soft, enlarged cervix equal to or larger than the fundus
Products of conception entirely confined within and firmly attached to the endocervix
A closed internal cervical os and
A partially opened external cervical os. Most of the criteria were seen fulfilled in our cases.
Differential diagnosis include an aborting intrauterine pregnancy residing in cervix which can be differentiated by detecting ‘Sliding sign’ on transvaginal ultrasound as reported by Jurkovic et al. in 1996.[5] When gentle pressure was applied on the cevix with the probe, the gestational sac of an abortus slides against the endocervical canal unlike an implanted cervical pregnancy. Furthermore, peritrophoblastic blood flow can be demonstrated on color Doppler ultrasonography in case of cervical pregnancy.[6]
Before 1980, cervical pregnancy was diagnosed when dilation and curettage for presumed incomplete abortion resulted in unexpected hemorrhage.[7] However, now it can be easily diagnosed by a first trimester ultrasound examination. Introduction of methotrexate with or without intra-amniotic potassium chloride represents a major advance in terminating cervical ectopic pregnancy especially when fetal heart is present.[8] Among the various routes for methotrexate administration, intramuscular route is usually preferred. The patient should be hemodynamically stable and must comply with posttreatment monitoring.[9] In case of cervical pregnancy usually the multidose methotrexate regimen, i.e., 1.0 mg/kg body weight on days 1, 3, 5 and 7 interspaced by leucoverin 0.1 mg/kg body weight is preferred which was followed in the management of our second case. Posttreatment decline in weekly serum beta hCG level shows the successful therapeutic intervention, as observed in our second case.
In recent times, in vitro fertilization and other assisted reproductive technique have been reported to be associated with increased risk of cervical pregnancy and the etiology is attributed to the rapid transport of fertilized ovum in to the endocervical canal because of an unreceptive endometrium. According to one review, the incidence of cervical pregnancy is 0.1% among in vitro fertilization pregnancies.[9] Arrest of bleeding can be achieved by tamponade of the uterine cervix with a Foleys’ catheter or vaginal packing, ligation of descending branches of the uterine arteries, bilateral hypogastric artery ligation or uterine artery embolization[2] where conservation of uterus is required for future fertility, as demonstrated in our third case.
CONCLUSION
Although cervical pregnancy are rare, increased number of cases being reported because of risk factors like high cesarean section rate and increased use of assisted reproductive technique for management of infertility. The success of conservative treatment depends on the timely and prompt diagnosis by early ultrasound, which can reduce the chances of severe life threatening hemorrhage necessitating hysterectomy or blood transfusion.
ACKNOWLEDGMENTS
We would like to thank the Department of OBGYN, SCB Medical College, Cuttack for their valuable support and co-operation of patients and their families admitted to the hospital.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Celik C, Bala A, Acar A, Gezginç K, Akyürek C. Methotrexate for cervical pregnancy. A case report. J Reprod Med. 2003;48:130–2. [PubMed] [Google Scholar]
- 2.Sharma A, Ojha R, Mondal S, Chattopadhyay S, Sengupta P. Cervical intramural pregnancy: Report of a rare case. Niger Med J. 2013;54:271–3. doi: 10.4103/0300-1652.119670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubin IC. Cervical pregnancy. Surg Gynecol Obstet. 1911;13:625. [Google Scholar]
- 4.Paalman RJ, McElin TW. Cervical pregnancy; review of the literature and presentation of cases. Am J Obstet Gynecol. 1959;77:1261–70. [PubMed] [Google Scholar]
- 5.Jurkovic D, Hacket E, Campbell S. Diagnosis and treatment of early cervical pregnancy: A review and a report of two cases treated conservatively. Ultrasound Obstet Gynecol. 1996;8:373–80. doi: 10.1046/j.1469-0705.1997.08060373.x. [DOI] [PubMed] [Google Scholar]
- 6.Kirk E, Condous G, Haider Z, Syed A, Ojha K, Bourne T. The conservative management of cervical ectopic pregnancies. Ultrasound Obstet Gynecol. 2006;27:430–7. doi: 10.1002/uog.2693. [DOI] [PubMed] [Google Scholar]
- 7.Leeman LM, Wendland CL. Cervical ectopic pregnancy. Diagnosis with endovaginal ultrasound examination and successful treatment with methotrexate. Arch Fam Med. 2000;9:72–7. doi: 10.1001/archfami.9.1.72. [DOI] [PubMed] [Google Scholar]
- 8.Polak G, Stachowicz N, Morawska D, Kotarski J. Treatment of cervical pregnancy with systemic methotrexate and KCI solution injection into the gestational sac – Case report and review of literature. Ginekol Pol. 2011;82:386–9. [PubMed] [Google Scholar]
- 9.Surampudi K. A case of cervical ectopic pregnancy: Successful therapy with methotrexate. J Obstet Gynaecol India. 2012;62(Suppl 1):1–3. doi: 10.1007/s13224-013-0351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


