Abstract
Since its introduction in 1984, laparoscopic ovarian drilling has evolved into a safe and effective surgical treatment for anovulatory, infertile women with polycystic ovary syndrome (PCOS), unresponsive to clomiphene citrate. It is as effective as gonadotropins in terms of pregnancy and live birth rates, but without the risks of ovarian hyperstimulation syndrome and multiple pregnancies. It improves ovarian responsiveness to successive ovulation induction agents. Its favorable reproductive and endocrinal effects are sustained long. Despite its advantages, its use in unselected cases of PCOS or for non-fertility indications is not prudent owing to the potential risks of iatrogenic adhesions and ovarian insufficiency.
Keywords: Clomiphene citrate resistance, laparoscopic ovarian drilling, polycystic ovary syndrome
INTRODUCTION
Polycystic ovary syndrome (PCOS), a common endocrine disorder affecting women in the reproductive age group, is a predominant cause of anovulatory infertility,[1] with a prevalence rate of 17-20% (Rotterdam diagnostic criteria).[2,3] Clomiphene citrate (CC), a selective estrogen receptor modulator, still remains the first line of treatment for ovulation induction (OI) in PCOS patients.[4,5,6,7,8] CC-resistance refers to the failure to ovulate with 150 mg of CC for at least 3 cycles, while CC-failure is defined as failure to conceive with CC despite successful regular ovulation for 6-9 cycles.[9] Since its inception in 1984, laparoscopic ovarian drilling (LOD) has evolved into a safe and effective surgical option for CC-resistant PCOS cases. It is as effective as gonadotropins in terms of clinical pregnancy rates and live birth rates with the obvious advantages of spontaneous mono-ovulation there by minimizing the need for intensive monitoring and eliminating the risks of ovarian hyperstimulation syndrome (OHSS) and multiple pregnancies.[4,9,10,11] However, there are concerns regarding the long-term effects on ovarian function, especially iatrogenic adhesions and decreased ovarian reserve (DOR), which may potentially jeopardize future fertility. Hence, this procedure should be employed rationally in selected CC-resistant cases for the sole purpose of correction of anovulatory infertility.
The aim of this review is to evaluate and summarize the current body of literature regarding the role of LOD in management of PCOS entailing its different pre, intra and postoperative aspects.
MATERIALS AND METHODS
A systematic search of Medline, PubMed, the Cochrane Library, the National Guideline Clearinghouse, and the Health Technology Assessment Database was performed from January 1, 1984 to December 31, 2013 using key words “PCOS,” “laparoscopic ovarian surgery,” “LOD,” “laparoscopic ovarian diathermy,” “laparoscopic ablative therapy” and “laparoscopic ovarian electrocautery.” Relevant evidence was identified and assessed for quality and suitability for inclusion in the following order — Systematic reviews, meta-analyses, guidelines, randomized controlled trials (RCTs), prospective cohort studies, observational studies, nonsystematic reviews, and case series.
Mechanism of action
The exact mechanism is yet to be elucidated. The most plausible one is the destruction of ovarian follicles and stroma resulting in a decrease in androgen and inhibin levels and a secondary rise in follicle-stimulating hormone (FSH) levels.[10,12,13,14] Production of inflammatory growth factors like insulin-like growth factor-1, in response to thermal injury, further potentiates the actions of FSH on folliculogenesis, while increased blood flow to the ovary provoked by surgery, facilitates increased delivery of gonadotropins.[12,14]
Indications
The main indication for LOD is CC-resistant PCOS - as a second-line therapy for anovulatory infertile PCOS cases; specifically, as an alternative to gonadotropins.[6,9,10,11,15] Royal College of Obstetricians and Gynecologists,[16] American College of Obstetricians and Gynecologists,[17] Society of Obstetricians and Gynecologists, Canada[8] and the recent PCOS consensus working group[4] — All recommend its use in highly selected cases, particularly in those with hypersecretion of luteinizing hormone (LH), normal body mass index, those needing laparoscopic assessment of the pelvis or who live too far away from the hospital for the intensive monitoring required during gonadotropin therapy. Despite its theoretical advantages, LOD is not superior to CC, neither as a first line therapy for OI[11,18] nor for CC-failure[19] or prior to in vitro fertilization (IVF).[11] A recent Cochrane systematic review of 9 RCTs and 16 trials concluded that there was no evidence of a significant difference in rates of clinical pregnancy (39.7 vs. 40.5%) or live birth (34 vs. 38%) in women with clomiphene-resistant PCOS undergoing LOD compared to other medical treatments.[20] This implies that LOD is a valid, but not the sole option for CC-resistant PCOS. The evidence for improvement in biochemical hyperandrogenism translating into comparable improvement in clinical hyperandrogenism is not clear; hence LOD should not be offered for non-fertility indications like amelioration of acne or hirsutism or for regularization of menstrual cycles.[21,22,23]
Surgical technique
Standardization of the surgical techniques is lacking. Reproductive outcomes are comparable with laser and diathermy.[24] Electrocautery, using an insulated unipolar needle electrode with a non-insulated distal end measuring 1-2 cm, is the most commonly used method, although few authors have reported similar ovulation and pregnancy rates with bipolar energy.[25,26] The number of punctures is empirically chosen depending on the ovarian size. In the original procedure, 3-8 diathermy punctures (each of 3 mm diameter and 2-4 mm depth) per ovary were applied, using power setting of 200-300 W for 2-4 s.[27] Most surgeons perform four punctures per ovary, each for 4 s at 40 W (rule of 4), delivering 640 J of energy per ovary (the lowest effective dose recommended).[28] Nevertheless, clinical response is dose-dependent, with higher ovulation and pregnancy rates observed by increasing dose of thermal energy up to 600 J/ovary, irrespective of ovarian volume.[29] Conversely, adjusting thermal dose based on ovarian volume (60 J/cc) has better reproductive outcomes with similar postoperative adhesion rates than fixed dose of 600 J/ovary.[30] Despite lack of convincing evidence and significant reduction in operative time, most gynecologists still perform bilateral over unilateral drilling.[20,31,32,33]
Different modifications of the classic needle electrode technique such as laparoscopic ovarian multi-needle intervention,[34] LOD using a monopolar hook electrode,[35] LOD using the harmonic scalpel[36,37] and office microlaparoscopic ovarian drilling are proposed.[38,39] Various transvaginal methods such as transvaginal hydrolaparoscopy (fertiloscopy)[40,41,42] and transvaginal sonography - guided ovarian interstitial laser treatment are also developed.[43,44] However, larger prospective studies are needed to validate the use, safety, efficacy and long-term effects of these alternate techniques.
Predictors of success
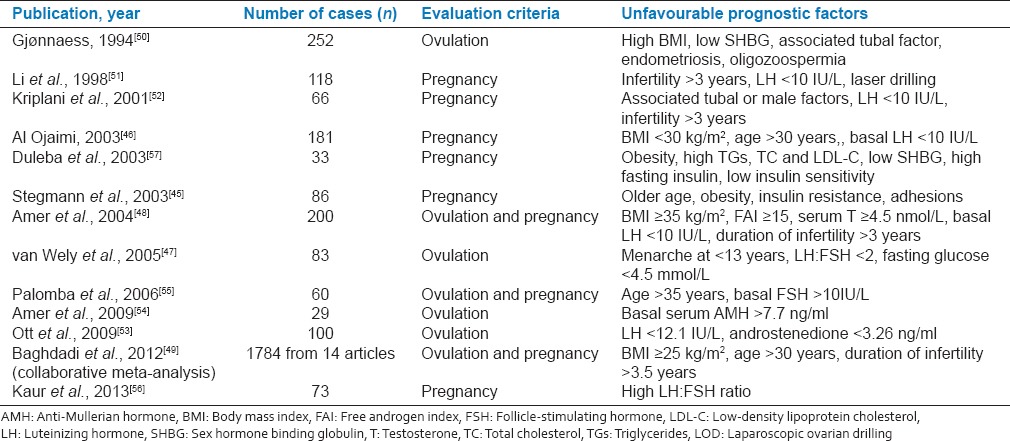
On an average, 20-30% of anovulatory PCOS women fail to respond to LOD; possibly due to inadequate destruction of ovarian stroma or inherent resistance of the ovaries. The rationality of increasing the number of punctures or thermal energy applied to improve response at the expense of increased risks of adhesions and premature ovarian failure (POF) is yet to be proved. Several prognostic factors are evaluated to predict successful outcomes,[45,46,47,48,49,50,51,52,53,54,55,56,57] knowledge of which may be useful in judicious patient selection thus avoiding unnecessary surgery [Table 1]. Some of these appear to play a consistent role like preoperative LH concentrations and duration of infertility. However, impact of other factors such as obesity, insulin resistance (IR), metabolic syndrome and hyperandrogenism on LOD outcomes is still disputable.
Table 1.
Predictors of success of LOD
Reproductive outcomes and endocrinal changes after laparoscopic ovarian drilling
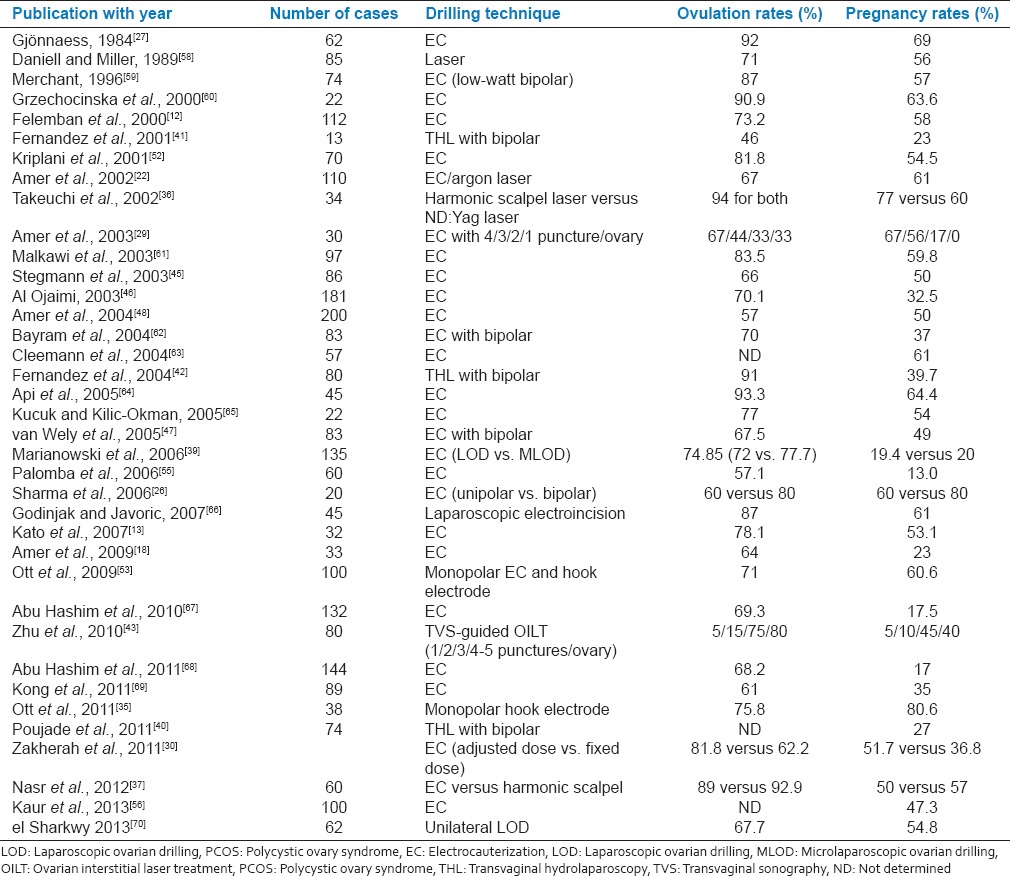
The clinical and endocrine response to LOD is governed by a dose-response relationship. Four punctures per ovary using a power setting of 30 W applied for 5 s/puncture (i.e., 600 J/ovary) are sufficient to produce optimal response (67% spontaneous ovulation and conception rates).[27] Reducing the thermal energy (<300 J/ovary) and/or number of punctures (2/ovary) reduces the chances of spontaneous ovulation and conception, while higher thermal doses (>1000 J/ovary) and/or number of punctures (≥7/ovary) causes extensive tissue destruction without additional improvement in outcomes. Table 2 depicts the spontaneous ovulation and pregnancy rates after various techniques of LOD, which have varied from 30-90% to 13-88% respectively, within 1-year of the procedure. LOD alone is usually effective in <50% of women.[4,62] In such cases, addition of CC and recombinant FSH (rFSH) may be considered after 3 and 6 months respectively. LOD also improves the sensitivity of the ovaries towards subsequent CC and FSH, especially in those who are less hyperandrogenic and less insulin-resistant.[46,50,71,72]
Table 2.
Reproductive outcomes after LOD in PCOS patients
The overall miscarriage rate varies from 0% to 36.5%.[14,55,56] Significant reduction of miscarriage rates after LOD were observed by Amer et al (reduced from 54% to 17%).[22] However, Cochrane systematic review did not find any significant differences in the abortion rates between LOD and other medical treatments (7.3% vs. 6.6%).[20]
The improved reproductive outcomes stem from an favorable intra-ovarian and systemic endocrinal milieu after LOD — Decreased plasma LH and in its pulsations, increased FSH, decreased LH:FSH ratio, a temporary fall in inhibin B, increased sex hormone binding globulin and a constant fall in androgens, free androgen index and Ferriman-Gallwey score.[10,27,36,58,65,66,73] Moreover, these beneficial reproductive and endocrinal effects are observed to chronically persist.[12,14,22,74,75,76,77]
Improvement in hormonal profiles does not translate into a comparable improvement in insulin sensitivity or reduction in risk of gestational diabetes mellitus (GDM).[10,14,61,78] Although patients with metabolic syndrome should not be precluded from LOD, adjuvant therapy with insulin sensitizers should be considered.[61] Few studies have demonstrated no impact on metabolic parameters.[79,80,81] Although, lower ovulation and pregnancy rates are reported in obese PCOS compared to lean counterparts,[48,49,50,57] one prospective study contradicts this.[46] Hence, obesity should not be considered as a contraindication, although anesthetic and surgical risks are increased in obese women.[46] However, impact of LOD in PCOS associated with obesity, IR or metabolic syndrome needs further research for clarification.
Complications
One of the main shortcomings of LOD is iatrogenic adhesions due to bleeding from the ovarian surface or premature contact between the ovary and the bowel after cauterization. Adhesion rates ranged from 0 to 100%,[12,33,34,37,62,82,83,84,85,86] involving higher risks with laser,[12,82,85] probably owing to lesser thermal penetration (2-4 mm) by the cone-shaped lesions of laser drilling compared with cylinder-shaped lesions (8 mm) of monopolar electrocoagulation. Most studies reported mild to moderate adhesions which do not seem to affect pregnancy rates after LOD. Adhesion prevention strategies like liberal peritoneal lavage,[87] application of adhesion barriers like intercede[85] and performance of adhesiolysis at early second-look laparoscopy,[82] are not effective in preventing de novo adhesions or in improving pregnancy rates.[20] Ovary should be raised before application of energy and saline washed after the procedure to decrease the temperature thereby reducing the risk of injury.[56]
Another potential risk is POF, especially if the ovarian blood supply is damaged inadvertently or if large number of punctures are made, leading to excessive destruction of ovarian follicular pool or production of anti-ovarian antibodies.[4] Only one isolated case of ovarian atrophy following high-energy drilling (eight coagulation points at 400 W for 5 s) is reported.[88] When applied correctly, it does not appear to compromise the ovarian reserve. A prospective comparative study found that the extent of ovarian tissue damage was limited, ranging from 0.4% after four to 1% after eight coagulation punctures, each of 40 W for 5 s.[89] In fact, changes in ovarian reserve markers can be interpreted as normalization of ovarian function rather than a reduction of ovarian reserve.[73,90] Coagulation should not be done within 8-10 mm of the ovarian hilum.[86,88] Unilateral drilling,[33,73] use of the harmonic scalpel,[37] use of bipolar energy or <5 perforations with monopolar energy[15] are associated with lesser risk of adhesions and DOR but with equivalent reproductive outcomes.
Alternative strategies in clomiphene citrate-resistant polycystic ovary syndrome and comparison of efficacy with laparoscopic ovarian drilling
A comparison of the efficacy between LOD and other drugs for OI in CC-resistant PCOS is demonstrated in Table 3. LOD is equally efficacious to rFSH in terms of ovulation, pregnancy and live birth rates.[34,91,92,100,101] Although cumulative conception rates at 6 months are lower with LOD than gonadotropin, they even-out after 12 months.[21] However, 2 RCTs found that the adjuvant therapy with CC or gonadotropins was required to achieve equivalent pregnancy and live birth rates in patients remaining anovulatory 8-12 weeks after LOD or those who subsequently became anovulatory.[62,93]
Table 3.
Comparison of efficacy between LOD and other medical treatments in CC-resistant PCOS
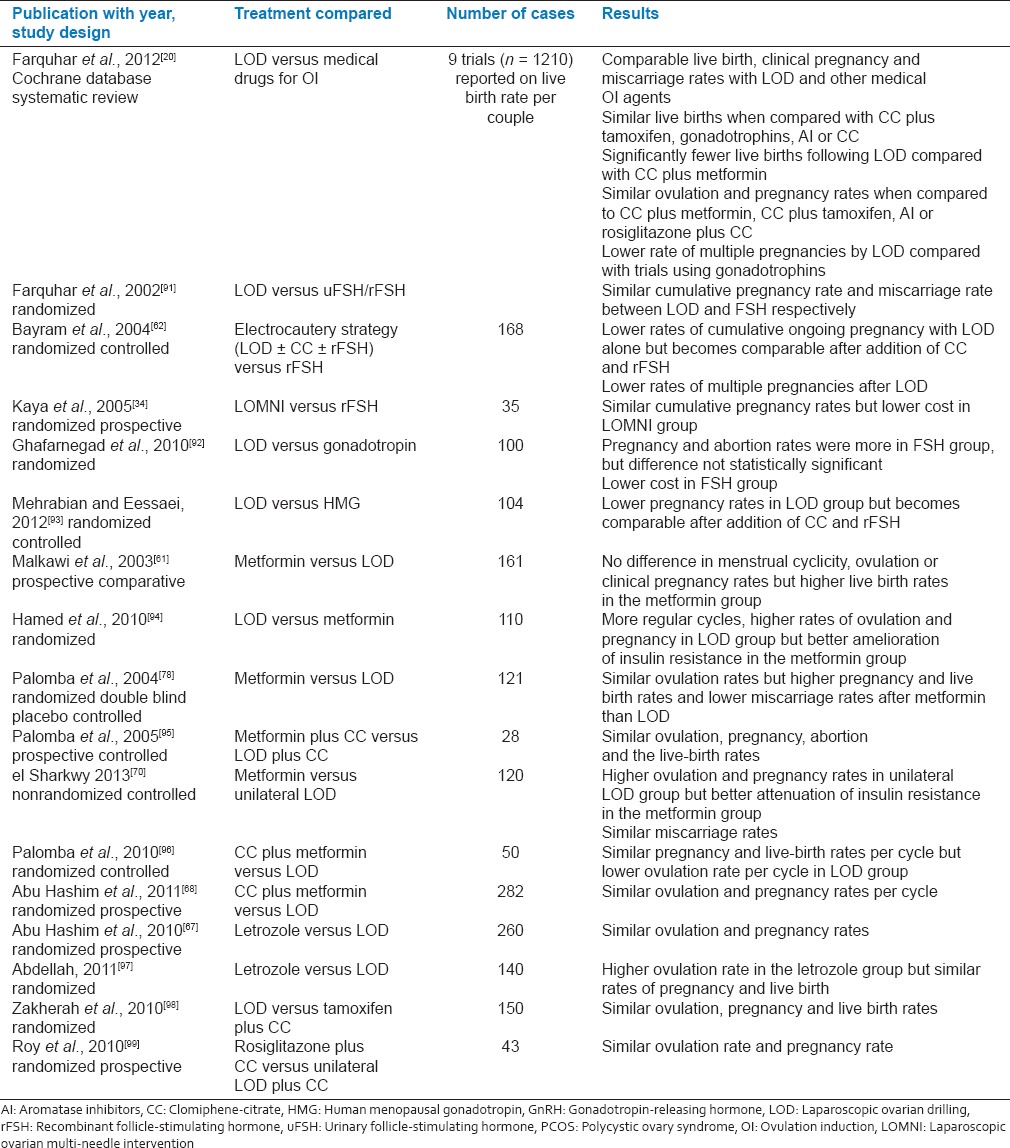
Trials comparing metformin with LOD in CC-resistant PCOS have shown variable results.[61,78,94] with some favoring LOD,[94] some favoring metformin[78] and others reporting equal efficacy.[61,95] Some studies have demonstrated higher ovulation and pregnancy rates with LOD but better attenuation of IR as well as lower GDM rates in those who conceived with metformin.[70,78,94] Even combined treatment with metformin, and CC is equally efficacious as LOD.[68,96] Since such combined treatment restores regular menstruation and ovulation in 70% women, this may be considered as a stepwise approach, before resorting to surgery or gonadotropin administration in CC-resistant PCOS cases.[102,103] Similarly, reproductive outcomes of other medical treatments such as letrozole,[67,97] CC plus tamoxifen[98] and CC plus rosiglitazone[99] are comparable with LOD.
Laparoscopic ovarian drilling in clomiphene citrate-failure and as first-line therapy in polycystic ovary syndrome
Role of LOD in CC-failure or as first-line therapy in PCOS remains largely undetermined. Only one RCT, comparing the efficacy of LOD versus continuation of CC up to six further cycles in 176 CC-failure PCOS patients, observed similar improvement in cycle length, pregnancy, miscarriage and live birth rates.[19] When compared to CC as first-line therapy in PCOS, one comparative study found higher ovulation (90.9% vs. 68%) and pregnancy (63.6% vs. 28%) rates in the LOD group[60] while an RCT found no difference at 12 months.[18] Interestingly, when offered to women after CC-resistance/failure, LOD achieved a pregnancy rate 2 times higher than that resulting from LOD as a first-line therapy (55% vs. 27%).[18] This possibly suggests that LOD may be more effective in CC-resistant PCOS women than in women without previous knowledge of their response to CC. Currently, LOD is not recommended for CC-failure PCOS or as first-line therapy due to lack of its superiority over CC.[11]
Pregnancy outcomes after laparoscopic ovarian drilling
Multiple pregnancy rate varies from 0% to 10%, but is significantly lower than gonadotropins, thus making LOD an attractive option for CC-resistant PCOS.[20] No difference in the incidence of OHSS and miscarriage rates is seen between LOD and other medical treatments.[20] LOD does not seem to improve risk of GDM, and higher incidence of GDM and pregnancy-induced hypertension have been reported after LOD.[52,69,78,104]
Cost-effectiveness
Laparoscopic ovarian drilling is more cost-effective than gonadotropins as single-treatment results in several mono-ovulatory cycles thus allowing multiple attempts at conception whereas one course of gonadotropin therapy yields a single ovulatory cycle with the inherent need for intensive monitoring.[20,34,92,100,105,106] The higher incidence of multiple pregnancies incurs extra costs in those who conceive with FSH.[20,100]
What next after laparoscopic ovarian drilling failure?
Laparoscopic ovarian drilling failure is defined as failure to ovulate within 6-8 weeks, recurrence of anovulatory status after an initial response or failure to conceive despite regular ovulation for 12 months.[9] Since LOD improves responsiveness of the polycystic ovaries to subsequent OI agents, reintroduction of drug treatments (first CC and then gonadotrophins) and possibly IVF can be considered in those do not spontaneously become pregnant within 6 months after LOD once ovulation has been re-established or after 3 months when ovulation has not been detected.[15]
Re-drilling — should it be done?
The effectiveness of a second LOD, that is re-drilling in women with PCOS was investigated in a retrospective study comprising of 20 women who had undergone LOD 1-6 years prior.[107] Overall, ovulation and pregnancy rates were 60% and 53%, respectively, with better outcomes in LOD-sensitive than LOD-resistant cases (83 and 67% vs. 25 and 29%, respectively). However, there are concerns of adhesions and DOR, precluding the feasibility of a RCT to address this issue. Until then, repeated application of LOD should not be encouraged.[4]
CONCLUSION
Laparoscopic ovarian drilling is currently recommended as a safe, efficacious and cost-effective alternative to gonadotropins for OI in infertile, anovulatory, CC-resistant PCOS women without the risks of OHSS or multiple gestation. Monopolar diathermy is the most widely used technique, although no technique is superior. Restoration of regular ovulation and menstruation as well as reduction in androgen and LH levels persist long-term. The evidence on the improvement of insulin sensitivity, lipid and lipoprotein disturbances, acne and hirsutism, are not clear; hence it should not be used for such non-fertility indications. Although iatrogenic adhesion formation and DOR are potential complications, they are of little clinical significance and can be minimized by limiting the number of punctures and energy applied. A detailed knowledge of the clinical and hormonal profile of the patients may be useful in a careful selection of cases likely to respond to LOD. Since LOD improves ovarian responsiveness to CC and gonadotropins, these may be considered after LOD failure instead of repeat LOD, before proceeding to the last resort that is, IVF. Despite its advantages, LOD is neither the first-line therapy in PCOS nor the treatment of choice in CC-resistant PCOS owing to the advent of a multitude of safe and efficacious oral alternatives and wider acceptance of relatively safe low-dose step-up regimen of gonadotropin therapy. Rather, it should be reserved to well-chosen anovulatory CC-resistant PCOS cases — Those with young age, raised LH levels, exaggerated response to gonadotropins, noncompliance or nonfeasibility with frequent, intensive monitoring or needing laparoscopic assessment of the pelvis. Importantly, reproductive specialists should remember that it is only an alternative, not the ultimate in management of PCOS.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Overbeek A, Lambalk CB. Phenotypic and pharmacogenetic aspects of ovulation induction in WHO II anovulatory women. Gynecol Endocrinol. 2009;25:222–34. doi: 10.1080/09513590802571118. [DOI] [PubMed] [Google Scholar]
- 2.March WA, Moore VM, Willson KJ, Phillips DI, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25:544–51. doi: 10.1093/humrep/dep399. [DOI] [PubMed] [Google Scholar]
- 3.Yildiz BO, Bozdag G, Yapici Z, Esinler I, Yarali H. Prevalence, phenotype and cardiometabolic risk of polycystic ovary syndrome under different diagnostic criteria. Hum Reprod. 2012;27:3067–73. doi: 10.1093/humrep/des232. [DOI] [PubMed] [Google Scholar]
- 4.Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome. Fertil Steril. 2008;89:505–22. doi: 10.1016/j.fertnstert.2007.09.041. [DOI] [PubMed] [Google Scholar]
- 5.Brown J, Farquhar C, Beck J, Boothroyd C, Hughes E. Clomiphene and anti-oestrogens for ovulation induction in PCOS. Cochrane Database Syst Rev. 2009;7:CD002249. doi: 10.1002/14651858.CD002249.pub4. [DOI] [PubMed] [Google Scholar]
- 6.Abu Hashim H. Clomiphene citrate alternatives for the initial management of polycystic ovary syndrome: An evidence-based approach. Arch Gynecol Obstet. 2012;285:1737–45. doi: 10.1007/s00404-012-2261-2. [DOI] [PubMed] [Google Scholar]
- 7.Bouchard P. Treatment of infertility in women with polycystic ovary syndrome. Ann Endocrinol (Paris) 2010;71:225–7. doi: 10.1016/j.ando.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 8.Vause TD, Cheung AP, Sierra S, Claman P, Graham J, Guillemin JA, et al. Ovulation induction in polycystic ovary syndrome: No 242, May 2010. Int J Gynaecol Obstet. 2010;111:95–100. doi: 10.1016/j.ijgo.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Amer SA. Laparoscopic ovarian surgery for polycystic ovarian syndrome. In: Dunlop W, Ledger WL, editors. Recent Advances in Obstetrics and Gynaecology. 24th ed. London: Royal Society of Medicine Press Ltd; 2009. pp. 227–43. [Google Scholar]
- 10.Flyckt RL, Goldberg JM. Laparoscopic ovarian drilling for clomiphene-resistant polycystic ovary syndrome. Semin Reprod Med. 2011;29:138–46. doi: 10.1055/s-0031-1272476. [DOI] [PubMed] [Google Scholar]
- 11.Abu Hashim H, Al-Inany H, De Vos M, Tournaye H. Three decades after Gjönnaess's laparoscopic ovarian drilling for treatment of PCOS; what do we know? An evidence-based approach. Arch Gynecol Obstet. 2013;288:409–22. doi: 10.1007/s00404-013-2808-x. [DOI] [PubMed] [Google Scholar]
- 12.Felemban A, Tan SL, Tulandi T. Laparoscopic treatment of polycystic ovaries with insulated needle cautery: A reappraisal. Fertil Steril. 2000;73:266–9. doi: 10.1016/s0015-0282(99)00534-8. [DOI] [PubMed] [Google Scholar]
- 13.Kato M, Kikuchi I, Shimaniki H, Kobori H, Aida T, Kitade M, et al. Efficacy of laparoscopic ovarian drilling for polycystic ovary syndrome resistant to clomiphene citrate. J Obstet Gynaecol Res. 2007;33:174–80. doi: 10.1111/j.1447-0756.2007.00504.x. [DOI] [PubMed] [Google Scholar]
- 14.Seow KM, Juan CC, Hwang JL, Ho LT. Laparoscopic surgery in polycystic ovary syndrome: Reproductive and metabolic effects. Semin Reprod Med. 2008;26:101–10. doi: 10.1055/s-2007-992930. [DOI] [PubMed] [Google Scholar]
- 15.Fernandez H, Morin-Surruca M, Torre A, Faivre E, Deffieux X, Gervaise A. Ovarian drilling for surgical treatment of polycystic ovarian syndrome: A comprehensive review. Reprod Biomed Online. 2011;22:556–68. doi: 10.1016/j.rbmo.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Obstetricians and Gynaecologists (RCOG). Longterm consequences of polycystic ovary syndrome. (Green-top Guideline; No. 33). London, (UK): Royal College of Obstetricians and Gynaecologists (RCOG) 2007:1–11. [Google Scholar]
- 17.ACOG Committee on Practice Bulletins — Gynecology. ACOG Practice Bulletin No 108: Polycystic ovary syndrome. Obstet Gynecol. 2009;114:936–49. doi: 10.1097/AOG.0b013e3181bd12cb. [DOI] [PubMed] [Google Scholar]
- 18.Amer SA, Li TC, Metwally M, Emarh M, Ledger WL. Randomized controlled trial comparing laparoscopic ovarian diathermy with clomiphene citrate as a first-line method of ovulation induction in women with polycystic ovary syndrome. Hum Reprod. 2009;24:219–25. doi: 10.1093/humrep/den325. [DOI] [PubMed] [Google Scholar]
- 19.Abu Hashim H, Foda O, Ghayaty E, Elawa A. Laparoscopic ovarian diathermy after clomiphene failure in polycystic ovary syndrome: Is it worthwhile? A randomized controlled trial. Arch Gynecol Obstet. 2011;284:1303–9. doi: 10.1007/s00404-011-1983-x. [DOI] [PubMed] [Google Scholar]
- 20.Farquhar C, Brown J, Marjoribanks J. Laparoscopic drilling by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2012;6:CD001122. doi: 10.1002/14651858.CD001122.pub4. [DOI] [PubMed] [Google Scholar]
- 21.Balen A. Surgical management of PCOS. Best Pract Res Clin Endocrinol Metab. 2006;20:271–80. doi: 10.1016/j.beem.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Amer SA, Gopalan V, Li TC, Ledger WL, Cooke ID. Long term follow-up of patients with polycystic ovarian syndrome after laparoscopic ovarian drilling: Clinical outcome. Hum Reprod. 2002;17:2035–42. doi: 10.1093/humrep/17.8.2035. [DOI] [PubMed] [Google Scholar]
- 23.Johnson NP, Wang K. Is ovarian surgery effective for androgenic symptoms of polycystic ovarian syndrome? J Obstet Gynaecol. 2003;23:599–606. doi: 10.1080/01443610310001604330. [DOI] [PubMed] [Google Scholar]
- 24.Farquhar C, Lilford RJ, Marjoribanks J, Vandekerckhove P. Laparoscopic ‘drilling’ by diathermy or laser for ovulation induction in anovulatory polycystic ovary syndrome. Cochrane Database Syst Rev. 2007;18:CD001122. doi: 10.1002/14651858.CD001122.pub3. [DOI] [PubMed] [Google Scholar]
- 25.Fernandez H, Faivre E, Gervaise A, Deffieux X. Laparoscopic ovarian drilling using a 5-French bipolar energy probe. Fertil Steril. 2010;94:740–1. doi: 10.1016/j.fertnstert.2009.03.048. [DOI] [PubMed] [Google Scholar]
- 26.Sharma M, Kriplani A, Agarwal N. Laparoscopic bipolar versus unipolar ovarian drilling in infertile women with resistant polycystic ovarian syndrome: A pilot study. J Gynecol Surg. 2006;22:105–11. [Google Scholar]
- 27.Gjönnaess H. Polycystic ovarian syndrome treated by ovarian electrocautery through the laparoscope. Fertil Steril. 1984;41:20–5. doi: 10.1016/s0015-0282(16)47534-5. [DOI] [PubMed] [Google Scholar]
- 28.Armar NA, McGarrigle HH, Honour J, Holownia P, Jacobs HS, Lachelin GC. Laparoscopic ovarian diathermy in the management of anovulatory infertility in women with polycystic ovaries: Endocrine changes and clinical outcome. Fertil Steril. 1990;53:45–9. doi: 10.1016/s0015-0282(16)53214-2. [DOI] [PubMed] [Google Scholar]
- 29.Amer SA, Li TC, Cooke ID. A prospective dose-finding study of the amount of thermal energy required for laparoscopic ovarian diathermy. Hum Reprod. 2003;18:1693–8. doi: 10.1093/humrep/deg307. [DOI] [PubMed] [Google Scholar]
- 30.Zakherah MS, Kamal MM, Hamed HO. Laparoscopic ovarian drilling in polycystic ovary syndrome: Efficacy of adjusted thermal dose based on ovarian volume. Fertil Steril. 2011;95:1115–8. doi: 10.1016/j.fertnstert.2010.10.037. [DOI] [PubMed] [Google Scholar]
- 31.Youssef H, Atallah MM. Unilateral ovarian drilling in polycystic ovarian syndrome: A prospective randomized study. Reprod Biomed Online. 2007;15:457–62. doi: 10.1016/s1472-6483(10)60373-2. [DOI] [PubMed] [Google Scholar]
- 32.Al-Mizyen E, Grudzinskas JG. Unilateral laparoscopic ovarian diathermy in infertile women with clomiphene citrate-resistant polycystic ovary syndrome. Fertil Steril. 2007;88:1678–80. doi: 10.1016/j.fertnstert.2007.01.060. [DOI] [PubMed] [Google Scholar]
- 33.Roy KK, Baruah J, Moda N, Kumar S. Evaluation of unilateral versus bilateral ovarian drilling in clomiphene citrate resistant cases of polycystic ovarian syndrome. Arch Gynecol Obstet. 2009;280:573–8. doi: 10.1007/s00404-009-0961-z. [DOI] [PubMed] [Google Scholar]
- 34.Kaya H, Sezik M, Ozkaya O. Evaluation of a new surgical approach for the treatment of clomiphene citrate-resistant infertility in polycystic ovary syndrome: Laparoscopic ovarian multi-needle intervention. J Minim Invasive Gynecol. 2005;12:355–8. doi: 10.1016/j.jmig.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 35.Ott J, Mayerhofer K, Aust S, Nouri K, Huber JC, Kurz C. A modified technique of laparoscopic ovarian drilling for polycystic ovary syndrome using the monopolar hook electrode. Acta Obstet Gynecol Scand. 2011;90:547–50. doi: 10.1111/j.1600-0412.2011.01103.x. [DOI] [PubMed] [Google Scholar]
- 36.Takeuchi S, Futamura N, Takubo S, Noda N, Minoura H, Toyoda N. Polycystic ovary syndrome treated with laparoscopic ovarian drilling with a harmonic scalpel. A prospective, randomized study. J Reprod Med. 2002;47:816–20. [PubMed] [Google Scholar]
- 37.Nasr AA, El-Naser A, El-Gaber AA, El-Sattar MA, Mgeed AA, Abolfotouh MM. A modified technique of laparoscopic ovarian drilling for polycystic ovary syndrome using harmonic scalpel. J Diabetes Metab. 2012;S6:008. [Google Scholar]
- 38.Salah TM. Office microlaproscopic ovarian drilling (OMLOD) versus conventional laproscopic ovarian drilling (LOD) for women with polycystic ovary syndrome. Arch Gynecol Obstet. 2013;287:361–7. doi: 10.1007/s00404-012-2526-9. [DOI] [PubMed] [Google Scholar]
- 39.Marianowski P, Kaminski P, Wielgos M, Szymusik I. The changes of hormonal serum levels and ovulation/pregnancy rates after ovarian electrocautery in microlaparoscopy and laparoscopy in patients with PCOS. Neuro Endocrinol Lett. 2006;27:214–8. [PubMed] [Google Scholar]
- 40.Poujade O, Gervaise A, Faivre E, Deffieux X, Fernandez H. Surgical management of infertility due to polycystic ovarian syndrome after failure of medical management. Eur J Obstet Gynecol Reprod Biol. 2011;158:242–7. doi: 10.1016/j.ejogrb.2011.05.007. [DOI] [PubMed] [Google Scholar]
- 41.Fernandez H, Alby JD, Gervaise A, de Tayrac R, Frydman R. Operative transvaginal hydrolaparoscopy for treatment of polycystic ovary syndrome: A new minimally invasive surgery. Fertil Steril. 2001;75:607–11. doi: 10.1016/s0015-0282(00)01746-5. [DOI] [PubMed] [Google Scholar]
- 42.Fernandez H, Watrelot A, Alby JD, Kadoch J, Gervaise A, deTayrac R, et al. Fertility after ovarian drilling by transvaginal fertiloscopy for treatment of polycystic ovary syndrome. J Am Assoc Gynecol Laparosc. 2004;11:374–8. doi: 10.1016/s1074-3804(05)60054-0. [DOI] [PubMed] [Google Scholar]
- 43.Zhu W, Fu Z, Chen X, Li X, Tang Z, Zhou Y, et al. Transvaginal ultrasound-guided ovarian interstitial laser treatment in anovulatory women with polycystic ovary syndrome: A randomized clinical trial on the effect of laser dose used on the outcome. Fertil Steril. 2010;94:268–75. doi: 10.1016/j.fertnstert.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 44.Ferraretti AP, Gianaroli L, Magli MC, Iammarrone E, Feliciani E, Fortini D. Transvaginal ovarian drilling: A new surgical treatment for improving the clinical outcome of assisted reproductive technologies in patients with polycystic ovary syndrome. Fertil Steril. 2001;76:812–6. doi: 10.1016/s0015-0282(01)02001-5. [DOI] [PubMed] [Google Scholar]
- 45.Stegmann BJ, Craig HR, Bay RC, Coonrod DV, Brady MJ, Garbaciak JA., Jr Characteristics predictive of response to ovarian diathermy in women with polycystic ovarian syndrome. Am J Obstet Gynecol. 2003;188:1171–3. doi: 10.1067/mob.2003.289. [DOI] [PubMed] [Google Scholar]
- 46.Al Ojaimi EH. Laparoscopic ovarian drilling for polycystic ovarian syndrome in clomiphene citrate- resistant women with anovulatory infertility. Bahrain Med Bull. 2003;2:1–14. [Google Scholar]
- 47.van Wely M, Bayram N, van der Veen F, Bossuyt PM. Predictors for treatment failure after laparoscopic electrocautery of the ovaries in women with clomiphene citrate resistant polycystic ovary syndrome. Hum Reprod. 2005;20:900–5. doi: 10.1093/humrep/deh712. [DOI] [PubMed] [Google Scholar]
- 48.Amer SA, Li TC, Ledger WL. Ovulation induction using laparoscopic ovarian drilling in women with polycystic ovarian syndrome: Predictors of success. Hum Reprod. 2004;19:1719–24. doi: 10.1093/humrep/deh343. [DOI] [PubMed] [Google Scholar]
- 49.Baghdadi LR, Abu Hashim H, Amer SA, Palomba S, Falbo A, Al-Ojaimi E, et al. Impact of obesity on reproductive outcomes after ovarian ablative therapy in PCOS: A collaborative meta-analysis. Reprod Biomed Online. 2012;25:227–41. doi: 10.1016/j.rbmo.2012.05.010. [DOI] [PubMed] [Google Scholar]
- 50.Gjønnaess H. Ovarian electrocautery in the treatment of women with polycystic ovary syndrome (PCOS). Factors affecting the results. Acta Obstet Gynecol Scand. 1994;73:407–12. doi: 10.3109/00016349409006253. [DOI] [PubMed] [Google Scholar]
- 51.Li TC, Saravelos H, Chow MS, Chisabingo R, Cooke ID. Factors affecting the outcome of laparoscopic ovarian drilling for polycystic ovarian syndrome in women with anovulatory infertility. Br J Obstet Gynaecol. 1998;105:338–44. doi: 10.1111/j.1471-0528.1998.tb10097.x. [DOI] [PubMed] [Google Scholar]
- 52.Kriplani A, Manchanda R, Agarwal N, Nayar B. Laparoscopic ovarian drilling in clomiphene citrate-resistant women with polycystic ovary syndrome. J Am Assoc Gynecol Laparosc. 2001;8:511–8. doi: 10.1016/s1074-3804(05)60613-5. [DOI] [PubMed] [Google Scholar]
- 53.Ott J, Wirth S, Nouri K, Kurz C, Mayerhofer K, Huber JC, et al. Luteinizing hormone and androstendione are independent predictors of ovulation after laparoscopic ovarian drilling: A retrospective cohort study. Reprod Biol Endocrinol. 2009;7:153. doi: 10.1186/1477-7827-7-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Amer SA, Li TC, Ledger WL. The value of measuring anti-Mullerian hormone in women with anovulatory polycystic ovary syndrome undergoing laparoscopic ovarian diathermy. Hum Reprod. 2009;24:2760–6. doi: 10.1093/humrep/dep271. [DOI] [PubMed] [Google Scholar]
- 55.Palomba S, Falbo A, Orio F, Jr, Russo T, Sbano F, D’Alessandro P, et al. Efficacy of laparoscopic ovarian diathermy in clomiphene citrate-resistant women with polycystic ovary syndrome: Relationships with chronological and ovarian age. Gynecol Endocrinol. 2006;22:329–35. doi: 10.1080/09513590600645700. [DOI] [PubMed] [Google Scholar]
- 56.Kaur M, Pranesh G, Mittal M, Gahlan A, Deepika K, Sashikala T, et al. Outcome of laparoscopic ovarian drilling in patients of clomiphene resistant polycystic ovary syndrome in a tertiary care center. Int J Infertil Fetal Med. 2013;4:39–44. [Google Scholar]
- 57.Duleba AJ, Banaszewska B, Spaczynski RZ, Pawelczyk L. Success of laparoscopic ovarian wedge resection is related to obesity, lipid profile, and insulin levels. Fertil Steril. 2003;79:1008–14. doi: 10.1016/s0015-0282(02)04848-3. [DOI] [PubMed] [Google Scholar]
- 58.Daniell JF, Miller W. Polycystic ovaries treated by laparoscopic laser vaporization. Fertil Steril. 1989;51:232–6. doi: 10.1016/s0015-0282(16)60482-x. [DOI] [PubMed] [Google Scholar]
- 59.Merchant RN. Treatment of polycystic ovary disease with laparoscopic low-watt bipolar electrocoagulation of the ovaries. J Am Assoc Gynecol Laparosc. 1996;3:503–8. doi: 10.1016/s1074-3804(05)80158-6. [DOI] [PubMed] [Google Scholar]
- 60.Grzechocinska B, Fracki S, Marianowski L. Results of clomiphene citrate ovarian stimulation vs laparoscopic electrocoagulation of the ovaries in infertile women with PCOS. Ginekol Pol. 2000;71:979–83. [PubMed] [Google Scholar]
- 61.Malkawi HY, Qublan HS, Hamaideh AH. Medical vs. Surgical treatment for clomiphene citrate-resistant women with polycystic ovary syndrome. J Obstet Gynaecol. 2003;23:289–93. doi: 10.1080/01443610310000100123. [DOI] [PubMed] [Google Scholar]
- 62.Bayram N, van Wely M, Kaaijk EM, Bossuyt PM, van der Veen F. Using an electrocautery strategy or recombinant follicle stimulating hormone to induce ovulation in polycystic ovary syndrome: Randomised controlled trial. BMJ. 2004;328:192. doi: 10.1136/bmj.328.7433.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cleemann L, Lauszus FF, Trolle B. Laparoscopic ovarian drilling as first line of treatment in infertile women with polycystic ovary syndrome. Gynecol Endocrinol. 2004;18:138–43. doi: 10.1080/09513590410001667869. [DOI] [PubMed] [Google Scholar]
- 64.Api M, Görgen H, Cetin A. Laparoscopic ovarian drilling in polycystic ovary syndrome. Eur J Obstet Gynecol Reprod Biol. 2005;119:76–81. doi: 10.1016/j.ejogrb.2004.07.023. [DOI] [PubMed] [Google Scholar]
- 65.Kucuk M, Kilic-Okman T. Hormone profiles and clinical outcome after laparoscopic ovarian drilling in women with polycystic ovary syndrome. Med Sci Monit. 2005;11:CR29–34. [PubMed] [Google Scholar]
- 66.Godinjak Z, Javoric R. Clinical outcome and hormone profiles before and after laparoscopic electroincision of the ovaries in women with polycystic ovary syndrome. Bosn J Basic Med Sci. 2007;7:171–5. doi: 10.17305/bjbms.2007.3076. [DOI] [PubMed] [Google Scholar]
- 67.Abu Hashim H, Mashaly AM, Badawy A. Letrozole versus laparoscopic ovarian diathermy for ovulation induction in clomiphene-resistant women with polycystic ovary syndrome: A randomized controlled trial. Arch Gynecol Obstet. 2010;282:567–71. doi: 10.1007/s00404-010-1566-2. [DOI] [PubMed] [Google Scholar]
- 68.Abu Hashim H, El Lakany N, Sherief L. Combined metformin and clomiphene citrate versus laparoscopic ovarian diathermy for ovulation induction in clomiphene-resistant women with polycystic ovary syndrome: A randomized controlled trial. J Obstet Gynaecol Res. 2011;37:169–77. doi: 10.1111/j.1447-0756.2010.01383.x. [DOI] [PubMed] [Google Scholar]
- 69.Kong GW, Cheung LP, Lok IH. Effects of laparoscopic ovarian drilling in treating infertile anovulatory polycystic ovarian syndrome patients with and without metabolic syndrome. Hong Kong Med J. 2011;17:5–10. [PubMed] [Google Scholar]
- 70.el Sharkwy IA. Metformin versus laparoscopic unilateral ovarian drilling in clomiphene resistant women with polycystic ovary syndrome. Middle East Fertil Soc J. 2013;18:202–7. [Google Scholar]
- 71.Soliman EM, Attia AM, Elebrashi AN, Younis AS, Salit ME. Laparoscopic ovarian electrocautery improves ovarian response to gonadotropins in clomiphene citrate resistant patients with polycystic ovary syndrome. Middle East Fertil Soc J. 2000;5:120–5. [Google Scholar]
- 72.Abu Hashim H, El-Shafei M, Badawy A, Wafa A, Zaglol H. Does laparoscopic ovarian diathermy change clomiphene-resistant PCOS into clomiphene-sensitive? Arch Gynecol Obstet. 2011;284:503–7. doi: 10.1007/s00404-011-1931-9. [DOI] [PubMed] [Google Scholar]
- 73.Kandil M, Selim M. Hormonal and sonographic assessment of ovarian reserve before and after laparoscopic ovarian drilling in polycystic ovary syndrome. BJOG. 2005;112:1427–30. doi: 10.1111/j.1471-0528.2005.00684.x. [DOI] [PubMed] [Google Scholar]
- 74.Amer SA, Banu Z, Li TC, Cooke ID. Long-term follow-up of patients with polycystic ovary syndrome after laparoscopic ovarian drilling: Endocrine and ultrasonographic outcomes. Hum Reprod. 2002;17:2851–7. doi: 10.1093/humrep/17.11.2851. [DOI] [PubMed] [Google Scholar]
- 75.Gjønnaess H. Late endocrine effects of ovarian electrocautery in women with polycystic ovary syndrome. Fertil Steril. 1998;69:697–701. doi: 10.1016/s0015-0282(98)00006-5. [DOI] [PubMed] [Google Scholar]
- 76.Mohiuddin S, Bessellink D, Farquhar C. Long-term follow up of women with laparoscopic ovarian diathermy for women with clomiphene-resistant polycystic ovarian syndrome. Aust N Z J Obstet Gynaecol. 2007;47:508–11. doi: 10.1111/j.1479-828X.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 77.Nahuis MJ, Kose N, Bayram N, van Dessel HJ, Braat DD, Hamilton CJ, et al. Long-term outcomes in women with polycystic ovary syndrome initially randomized to receive laparoscopic electrocautery of the ovaries or ovulation induction with gonadotrophins. Hum Reprod. 2011;26:1899–904. doi: 10.1093/humrep/der141. [DOI] [PubMed] [Google Scholar]
- 78.Palomba S, Orio F, Jr, Nardo LG, Falbo A, Russo T, Corea D, et al. Metformin administration versus laparoscopic ovarian diathermy in clomiphene citrate-resistant women with polycystic ovary syndrome: A prospective parallel randomized double-blind placebo-controlled trial. J Clin Endocrinol Metab. 2004;89:4801–9. doi: 10.1210/jc.2004-0689. [DOI] [PubMed] [Google Scholar]
- 79.Tulandi T, Saleh A, Morris D, Jacobs HS, Payne NN, Tan SL. Effects of laparoscopic ovarian drilling on serum vascular endothelial growth factor and on insulin responses to the oral glucose tolerance test in women with polycystic ovary syndrome. Fertil Steril. 2000;74:585–8. doi: 10.1016/s0015-0282(00)00684-1. [DOI] [PubMed] [Google Scholar]
- 80.Lemieux S, Lewis GF, Ben-Chetrit A, Steiner G, Greenblatt EM. Correction of hyperandrogenemia by laparoscopic ovarian cautery in women with polycystic ovarian syndrome is not accompanied by improved insulin sensitivity or lipid-lipoprotein levels. J Clin Endocrinol Metab. 1999;84:4278–82. doi: 10.1210/jcem.84.11.6140. [DOI] [PubMed] [Google Scholar]
- 81.Tiitinen A, Tenhunen A, Seppälä M. Ovarian electrocauterization causes LH-regulated but not insulin-regulated endocrine changes. Clin Endocrinol (Oxf) 1993;39:181–4. doi: 10.1111/j.1365-2265.1993.tb01771.x. [DOI] [PubMed] [Google Scholar]
- 82.Gürgan T, Urman B, Aksu T, Yarali H, Develioglu O, Kisnisci HA. The effect of short-interval laparoscopic lysis of adhesions on pregnancy rates following Nd-YAG laser photocoagulation of polycystic ovaries. Obstet Gynecol. 1992;80:45–7. [PubMed] [Google Scholar]
- 83.Naether OG, Fischer R. Adhesion formation after laparoscopic electrocoagulation of the ovarian surface in polycystic ovary patients. Fertil Steril. 1993;60:95–8. doi: 10.1016/s0015-0282(16)56043-9. [DOI] [PubMed] [Google Scholar]
- 84.Greenblatt EM, Casper RF. Adhesion formation after laparoscopic ovarian cautery for polycystic ovarian syndrome: l0 ack of correlation with pregnancy rate. Fertil Steril. 1993;60:766–70. [PubMed] [Google Scholar]
- 85.Saravelos H, Li TC. Post-operative adhesions after laparoscopic electrosurgical treatment for polycystic ovarian syndrome with the application of Interceed to one ovary: A prospective randomized controlled study. Hum Reprod. 1996;11:992–7. doi: 10.1093/oxfordjournals.humrep.a019337. [DOI] [PubMed] [Google Scholar]
- 86.Mercorio F, Mercorio A, Di Spiezio Sardo A, Barba GV, Pellicano M, Nappi C. Evaluation of ovarian adhesion formation after laparoscopic ovarian drilling by second-look minilaparoscopy. Fertil Steril. 2008;89:1229–33. doi: 10.1016/j.fertnstert.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 87.Naether OG. Significant reduction of adnexal adhesons following laparoscopic electrocautery of the ovarian surface (LEOS) by lavage and artificial ascites. Gynaecol Endosc. 1995;4:17–19. [Google Scholar]
- 88.Dabirashrafi H. Complications of laparoscopic ovarian cauterization. Fertil Steril. 1989;52:878–9. [PubMed] [Google Scholar]
- 89.El-Sheikhah A, Aboulghar M, Read R, El-Hendawi E. The extent of ovarian damage produced by ovarian cauterisation in the human. J Obstet Gynaecol. 2004;24:664–6. doi: 10.1080/01443610400007992. [DOI] [PubMed] [Google Scholar]
- 90.Api M. Is ovarian reserve diminished after laparoscopic ovarian drilling? Gynecol Endocrinol. 2009;25:159–65. doi: 10.1080/09513590802585605. [DOI] [PubMed] [Google Scholar]
- 91.Farquhar CM, Williamson K, Gudex G, Johnson NP, Garland J, Sadler L. A randomized controlled trial of laparoscopic ovarian diathermy versus gonadotropin therapy for women with clomiphene citrate-resistant polycystic ovary syndrome. Fertil Steril. 2002;78:404–11. doi: 10.1016/s0015-0282(02)03225-9. [DOI] [PubMed] [Google Scholar]
- 92.Ghafarnegad M, Arjmand N, Khazaeipour Z. Pregnancy rate of gonadotrophin therapy and laparoscopic ovarian electrocautery in polycystic ovary syndrome resistant to clomiphene citrate: A comparative study. Tehran Univ Med J. 2010;67:712–7. [Google Scholar]
- 93.Mehrabian F, Eessaei F. The laparoscopic ovarian electrocautery versus gonadotropin therapy in infertile women with clomiphene citrate-resistant polycystic ovary syndrome; a randomized controlled trial. J Pak Med Assoc. 2012;62:S42–4. [PubMed] [Google Scholar]
- 94.Hamed HO, Hasan AF, Ahmed OG, Ahmed MA. Metformin versus laparoscopic ovarian drilling in clomiphene- and insulin-resistant women with polycystic ovary syndrome. Int J Gynaecol Obstet. 2010;108:143–7. doi: 10.1016/j.ijgo.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 95.Palomba S, Orio F, Jr, Falbo A, Russo T, Caterina G, Manguso F, et al. Metformin administration and laparoscopic ovarian drilling improve ovarian response to clomiphene citrate (CC) in oligo-anovulatory CC-resistant women with polycystic ovary syndrome. Clin Endocrinol (Oxf) 2005;63:631–5. doi: 10.1111/j.1365-2265.2005.02392.x. [DOI] [PubMed] [Google Scholar]
- 96.Palomba S, Falbo A, Battista L, Russo T, Venturella R, Tolino A, et al. Laparoscopic ovarian diathermy vs clomiphene citrate plus metformin as second-line strategy for infertile anovulatory patients with polycystic ovary syndrome: A randomized controlled trial. Am J Obstet Gynecol. 2010;202(577):e1–8. doi: 10.1016/j.ajog.2009.11.042. [DOI] [PubMed] [Google Scholar]
- 97.Abdellah MS. Reproductive outcome after letrozole versus laparoscopic ovarian drilling for clomiphene-resistant polycystic ovary syndrome. Int J Gynaecol Obstet. 2011;113:218–21. doi: 10.1016/j.ijgo.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 98.Zakherah MS, Nasr A, El Saman AM, Shaaban OM, Shahin AY. Clomiphene citrate plus tamoxifen versus laparoscopic ovarian drilling in women with clomiphene-resistant polycystic ovary syndrome. Int J Gynaecol Obstet. 2010;108:240–3. doi: 10.1016/j.ijgo.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 99.Roy KK, Baruah J, Sharma A, Sharma JB, Kumar S, Kachava G, et al. A prospective randomized trial comparing the clinical and endocrinological outcome with rosiglitazone versus laparoscopic ovarian drilling in patients with polycystic ovarian disease resistant to ovulation induction with clomiphene citrate. Arch Gynecol Obstet. 2010;281:939–44. doi: 10.1007/s00404-009-1305-8. [DOI] [PubMed] [Google Scholar]
- 100.van Wely M, Bayram N, van der Veen F, Bossuyt PM. An economic comparison of a laparoscopic electrocautery strategy and ovulation induction with recombinant FSH in women with clomiphene citrate-resistant polycystic ovary syndrome. Hum Reprod. 2004;19:1741–5. doi: 10.1093/humrep/deh319. [DOI] [PubMed] [Google Scholar]
- 101.Malkawi HY, Qublan HS. Laparoscopic ovarian drilling in the treatment of polycystic ovary syndrome: How many punctures per ovary are needed to improve the reproductive outcome? J Obstet Gynaecol Res. 2005;31:115–9. doi: 10.1111/j.1447-0756.2005.00255.x. [DOI] [PubMed] [Google Scholar]
- 102.Saleh AM, Khalil HS. Review of nonsurgical and surgical treatment and the role of insulin-sensitizing agents in the management of infertile women with polycystic ovary syndrome. Acta Obstet Gynecol Scand. 2004;83:614–21. doi: 10.1111/j.0001-6349.2004.00481.x. [DOI] [PubMed] [Google Scholar]
- 103.Palomba S, Falbo A, Zullo F. Management strategies for ovulation induction in women with polycystic ovary syndrome and known clomifene citrate resistance. Curr Opin Obstet Gynecol. 2009;21:465–73. doi: 10.1097/GCO.0b013e328332d188. [DOI] [PubMed] [Google Scholar]
- 104.Al-Ojaimi EH. Pregnancy outcomes after laparoscopic ovarian drilling in women with polycystic ovarian syndrome. Saudi Med J. 2006;27:519–25. [PubMed] [Google Scholar]
- 105.Farquhar CM, Williamson K, Brown PM, Garland J. An economic evaluation of laparoscopic ovarian diathermy versus gonadotrophin therapy for women with clomiphene citrate resistant polycystic ovary syndrome. Hum Reprod. 2004;19:1110–5. doi: 10.1093/humrep/deh219. [DOI] [PubMed] [Google Scholar]
- 106.Nahuis MJ, Oude Lohuis E, Kose N, Bayram N, Hompes P, Oosterhuis GJ, et al. Long-term follow-up of laparoscopic electrocautery of the ovaries versus ovulation induction with recombinant FSH in clomiphene citrate-resistant women with polycystic ovary syndrome: A n economic evaluation. Hum Reprod. 2012;27:3577–82. doi: 10.1093/humrep/des336. [DOI] [PubMed] [Google Scholar]
- 107.Amer SA, Li TC, Cooke ID. Repeated laparoscopic ovarian diathermy is effective in women with anovulatory infertility due to polycystic ovary syndrome. Fertil Steril. 2003;79:1211–5. doi: 10.1016/s0015-0282(02)04960-9. [DOI] [PubMed] [Google Scholar]


