Abstract
Background:
C-reactive protein (CRP) is an acute phase reactant synthesized in the liver. CRP immunoreactivity is a feature of inflammatory hepatocellular adenomas with a higher risk of malignant transformation. A high serum CRP level denotes poor prognosis in hepatocellular carcinoma (HCC) patients. This study was conducted to determine whether CRP is produced in HCC and to assess the clinicopathologic significance of CRP expression in cancer cells.
Methods:
CRP immunoreactivity was examined in treatment-naïve HCCs (n=224) using tissue microarrays and was correlated with clinicopathologic parameters. The expression of CRP mRNA and protein was also assessed in 12 HCC cases by quantitative real-time polymerase chain reaction and immunoblotting. Hep3B and SNU-449 HCC cell lines were used for the analysis of CRP mRNA regulation by interleukin 6 (IL-6).
Results:
CRP was expressed in 133 of 224 HCCs (59.4%) with a variable degree of immunoreactivity (grade 1 in 25.9%; grade 2 in 20.1%; grade 3 in 13.4%). There was an inverse relationship between grade 3 CRP immunoreactivity and cancer-specific survival (p=.0047), while no associations were found with other parameters, including recurrence-free survival. The CRP mRNA expression level was significantly higher in CRP immunopositive cases than in immunonegative cases (p<.05). CRP mRNA expression was increased in Hep3B cells, but was not detected in SNU-449 cells even after IL-6 treatment.
Conclusions:
We report the expression of CRP in HCC for the first time. CRP expression was associated with poor cancer-specific survival in patients with resectable HCC.
Keywords: Carcinoma, hepatocellular; C-reactive protein; Immunohistochemistry; Prognosis
Acute phase reactants are a group of hepatic proteins that are synthesized and released into the circulation in response to certain stresses such as infection and physical injury [1]. C-reactive protein (CRP) is a well-known, major acute phase reactant that was originally found in the sera of patients infected with Streptococcus pneumoniae [2,3]. CRP mRNA transcription is primarily induced by pro-inflammatory cytokines interleukin (IL)-6 and IL- 1 [4-6]. The blood concentration of CRP is increased in inflammatory conditions of both infectious and non-infectious etiologies such as urinary tract infection and hyperlipidemic acute pancreatitis [7,8]. A growing body of evidence indicates a solid pathobiological relationship between chronic inflammation and carcinogenesis [9]. Innate immune components such as Toll-like receptors and NOD-like receptors play a role in the regulation of inflammation and development of cancer [10-12]. Serum CRP level has been shown to be a prognostic marker in various human cancers [13,14]. Likewise, high serum CRP level is a poor prognostic factor in hepatocellular carcinoma (HCC) in relation to early recurrence [15,16].
As hepatocytes are the primary origin of CRP synthesis, it is highly likely that neoplastic hepatocytes retain a functional capacity to synthesize CRP under the influence of pro-inflammatory stimuli. Not surprisingly, CRP expression has been rather extensively studied in hepatocellular adenomas [17,18], and CRP immunoreactivity is a critical parameter for molecular phenotyping and defining of the inflammatory subtype of hepatocel lular adenoma, which has a higher risk of malignant transformation [19-21]. Of note, based on the results of immunohistochemistry using a panel of antibodies and fluorescence in situ hybridization for gains of chromosomes 1, 8, and MYC in HCC arising in adenoma, Kakar et al.[22] recently proposed that a certain subset of hepatocellular adenomas may represent a well-differentiated version of HCCs. However, CRP expression in HCCs has not yet been studied. We postulated that the evaluation of CRP expression in HCC may provide valuable information regarding the unique biology of HCCs. This study was conducted to determine whether CRP is produced by HCC cells and to assess its clinicopathologic significance.
MATERIALS AND METHODS
Patients and tissue samples
A total of 224 cases of treatment-naïve HCCs (n=224) were retrieved from the files of the Department of Pathology, Asan Medical Center, Seoul, Korea. All cases were surgically resectable (R0). Early recurrence was defined as a recurrence of the tumor within 2 years after surgery. All patients provided written informed consent, and this study was approved by the Institutional Review Board of Asan Medical Center, Seoul, Korea.
Tissue microarray and immunohistochemistry
Tissue microarrays were prepared using representative formalin-fixed, paraffin-embedded blocks of HCC cases. Two 2-mmthick tissue cores were obtained from the donor blocks and transferred onto the recipient blocks after reviewing hematoxylin and eosin–stained slides. Four-micrometer-thick tissue microarray sections were immunostained using a rabbit polyclonal antiCRP antibody (1:1,000, AbCam, Cambridge, UK). The sections were transferred onto silanized slides, and heat-induced epitope retrieval was performed by treating the slides with Cell Conditioning 1 buffer for 32 minutes in a BenchMark XT automatic immunostainer (Ventana Medical Systems, Tucson, AZ, USA). The signals were detected using the OptiView DAB IHC Detection Kit (Ventana Medical Systems). The immunoreactivity was evaluated by a pathologist (C.J.K.) blinded to clinical information, using a 4-tier grading system: negative, grade 0; positive in less than 10% of tumor cells, grade 1; positive in less than 50% of tumor cells, grade 2; diffusely positive, grade 3.
Cell culture
Human HCC cell lines, Hep3B and SNU-449, were used for the analysis of CRP mRNA regulation by IL-6. Hep3B cells were cultured in Dulbecco’s modified Eagle medium (Life Technologies, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (FBS) and 1% penicillin/streptomycin. SNU-449 cells were cultured in RPMI 1640 medium (GE Healthcare Life Sciences, Pittsburgh, PA, USA) supplemented with 10% FBS and 1% penicillin/streptomycin. For IL-6 treatment, 5×105 cells were seeded into 100-mm dishes and were treated with 50 ng/mL of IL-6 (Cell Sciences, Canton, MA, USA) on the following day for 6 hours.
Quantitative real-time polymerase chain reaction
Total RNA was isolated from liver tissues (n=12) and cultured Hep3B and SNU-449 cells using Trizol and the miRNeasy Mini Kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. The extracted RNA (1 µg) was reversetranscribed using the Reverse Transcription System (Promega, Madison, WI, USA). Quantitative real-time polymerase chain reaction (qRT-PCR) analyses of CRP mRNA expression were performed using a TaqMan Gene Expression Assay (Hs00357041_ m1, Applied Biosystems, Carlsbad, CA, USA) and an ABI PRISM 7000 Sequence Detection System (Applied Biosystems). The human RPLPO (Large Ribosomal Protein) was used as an endogenous control for normalization.
Immunoblotting
Immunoblotting was done in 12 cases. Liver tissues were pulverized in liquid nitrogen, and total protein lysates were obtained using RIPA lysis buffer. Thirty micrograms of protein were electrophoresed in 12% sodium dodecyl sulfate–polyacrylamide gel and transferred onto polyvinylidene fluoride membranes (GE Healthcare Life Sciences). The membranes were blocked with 5% bovine serum albumin in Tris-buffered saline with 0.1% Tween 20 (TBS-T) and incubated at 4˚C overnight with mouse monoclonal primary antibodies against CRP (1:1,000, AbCam, Cambridge, MA, USA) and vinculin (1:1,000; SigmaAldrich, St. Louis, MO, USA), respectively. The blots were subsequently incubated at room temperature with horseradish peroxidase–conjugated secondary antibody for 1 hour (Cell Signaling Technology, Danvers, MA, USA). The signals were detected using a SuperSignal West Dura Chemiluminescent Substrate (Thermo Scientific, Waltham, MA, USA).
Statistical analyses
The analyses of continuous variables and proportions were done using Pearson’s chi-square test and Fisher exact test. The survival analysis was done using the Kaplan-Meier method. Independent variables and groups were compared using the MannWhitney U test. SPSS ver. 18.0 software (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
RESULTS
CRP expression in HCC
The demographics of the study population are summarized in Table 1. CRP immunoreactivity was observed as diffuse cytoplasmic immunostaining. Overall, 59.4% (133/224) of HCC cases were immunopositive for CRP, with grades 1, 2, and 3 immunoreactivity in 25.9% (58/224), 20.1% (45/224), and 13.4% (30/224) of the cases, respectively (Fig. 1). When we analyzed the relationship between multiple clinicopathologic parameters and CRP immunoreactivity, we found a significant difference in cancer-specific survival between CRP-negative or non-diffuse immunopositive cases (grades 0, 1, and 2) and grade 3 immunopositive cases (Fig. 2A). Grade 3 CRP immunopositive cases showed significantly shorter survival compared to CRP-negative or non-diffuse immunopositive cases (median of 50.7 months and range of 6-58 months vs. median of 58.5 months and range of 5–88 years; p=.0047). However, no significant correlation was found between the degree of CRP immunoreactivity and other clinicopathologic parameters including recurrence-free survival (Fig. 2B).
Table 1.
Clinical parameters and their relationship with CRP immunoreactivity
| Clinical parameter | CRP grade 0, 1, 2 | CRP grade 3 | p-value |
|---|---|---|---|
| Gender | .019 | ||
| Male | 150 (67.0) | 20 (8.9) | |
| Female | 44 (19.6) | 10 (4.5) | |
| Age (yr) | .054 | ||
| < 60 | 123 (54.9) | 22 (9.8) | |
| ≥ 60 | 71 (31.7) | 8 (3.6) | |
| Tumor size (cm) | .110 | ||
| < 5 | 138 (61.6) | 19 (8.5) | |
| ≥ 5 | 56 (25.0) | 11 (4.9) | |
| Serum AFP (ng/mL) | .125 | ||
| < 400 | 141 (62.9) | 24 (10.7) | |
| ≥ 400 | 53 (23.6) | 6 (2.7) | |
| BCLC stage | < .001 | ||
| A | 185 (82.6) | 26 (11.6) | |
| B | 9 (4.0) | 4 (1.8) | |
| Etiology | .096 | ||
| HBV | 139 (62.1) | 23 (10.3) | |
| HCV | 20 (8.9) | 1 (0.4) | |
| NBNC | 35 (15.6) | 6 (2.7) | |
| Fibrosis stage (Batts-Ludwig) | .454 | ||
| Stage 1, 2 | 39 (17.4) | 7 (3.1) | |
| Stage 3, 4 | 155 (69.2) | 23 (10.3) | |
| Microvascular invasion | .983 | ||
| Not identified | 136 (60.7) | 21 (9.4) | |
| Present | 58 (25.9) | 9 (4.0) | |
| Tumor number | < .001 | ||
| <3 | 185 (82.6) | 26 (11.6) | |
| ≥3 | 9 (4.0) | 4 (1.8) | |
| Edmondson-Steiner grade (worst) | .814 | ||
| Grade 1, 2 | 67 (29.9) | 10 (4.5) | |
| Grade 3, 4 | 127 (56.7) | 20 (8.9) | |
| Edmondson-Steiner grade (most) | .241 | ||
| Grade 1, 2 | 128 (57.1) | 18 (8.0) | |
| Grade 3, 4 | 66 (29.5) | 12 (5.4) | |
| Capsular invasion | .492 | ||
| Absent | 156 (69.6) | 25 (11.2) | |
| Present | 38 (17.0) | 5 (2.2) | |
| Early recurrence | .098 | ||
| Absent | 114 (50.9) | 15 (6.7) | |
| Occurs | 80 (35.7) | 15 (6.7) |
Values are presented as number (%).
CRP, C-reactive protein; AFP, alpha-fetoprotein; BCLC, Barcelona Clinic Liver Cancer; HBV, hepatitis B virus; HCB, hepatitis C virus; NBNC, non-B, non-C hepatocellular carcinoma.
Fig. 1.
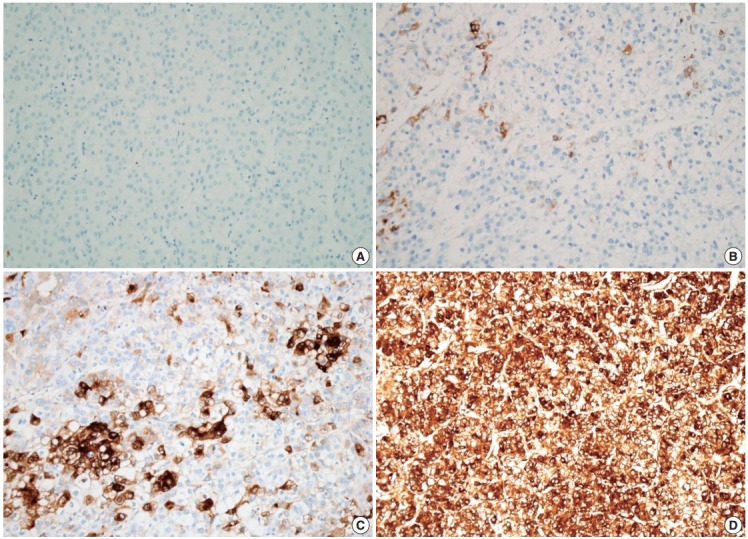
Cytoplasmic C-reactive protein (CRP) immunoreactivity in hepatocellular carcinoma cases. Immunoreactivity is analyzed using a 4-tier grading system: grade 0 (A), grade 1 (B), grade 2 (C), and grade 3 (D).
Fig. 2.
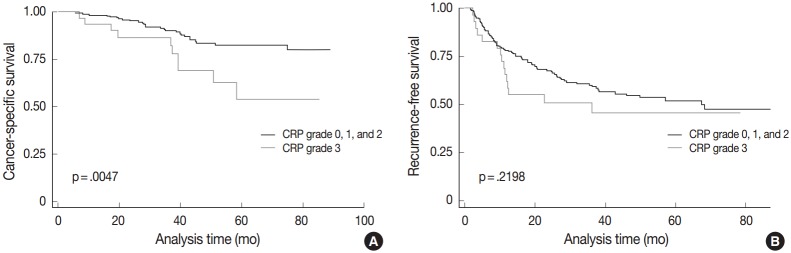
Clinical significance of C-reactive protein (CRP) immunoreactivity. (A) There is a significant difference in cancer-specific survival between patients with CRP grade 3 hepatocellular carcinomas (HCCs) and those with CRP grade 0, 1, and 2 HCCs. (B) There is no difference in recurrence-free survival between the two groups.
CRP mRNA expression in HCC
We further analyzed CRP protein and mRNA expression in HCCs (n=12) to see whether CRP expression is regulated at the transcriptional level. Immunoblotting for CRP confirmed variable expression of CRP in HCC cases (Fig. 3A). CRP signals were readily detected in six cases, but not in the remaining six cases. qRT-PCR analysis demonstrated a higher CRP mRNA expression in CRP immunopositive cases than in immunonegative cases (p=.046; ΔCt median of 3.62, range of 2.8–5.98 vs ΔCt median of 8.56, range of 1.07–15) (Fig. 3B).
Fig. 3.
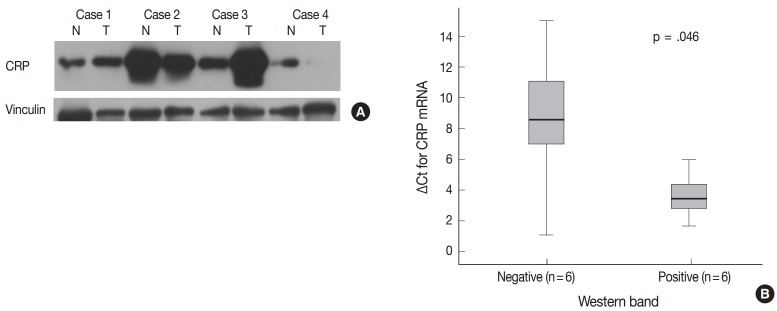
Correlation between C-reactive protein (CRP) mRNA and protein expression in hepatocellular carcinomas (HCCs). (A) Immunoblotting for CRP protein shows variable expression in HCCs (N, non-neoplastic liver; T, HCC). CRP protein expression is not found in the tumor of case 4, while CRP bands are readily detectable in both non-neoplastic and HCC samples of cases 1, 2, and 3. (B) Quantitative real-time polymerase chain reaction results are shown in box plots of ΔCt for CRP mRNA expression (Ct_CRP–Ct_RPLPO).
After confirming the relationship between CRP protein and mRNA expression, we tested if CRP mRNA transcription was dependent on pro-inflammatory mediators. The treatment of Hep3B and SNU-449 cells with IL-6 at the concentration of 50 ng/mL for 6 hours induced a 17.5-fold increase in CRP mRNA expression in Hep3B cells, but CRP mRNA expression was not detected in SNU-449 cells even after IL-6 treatment (Fig. 4).
Fig. 4.
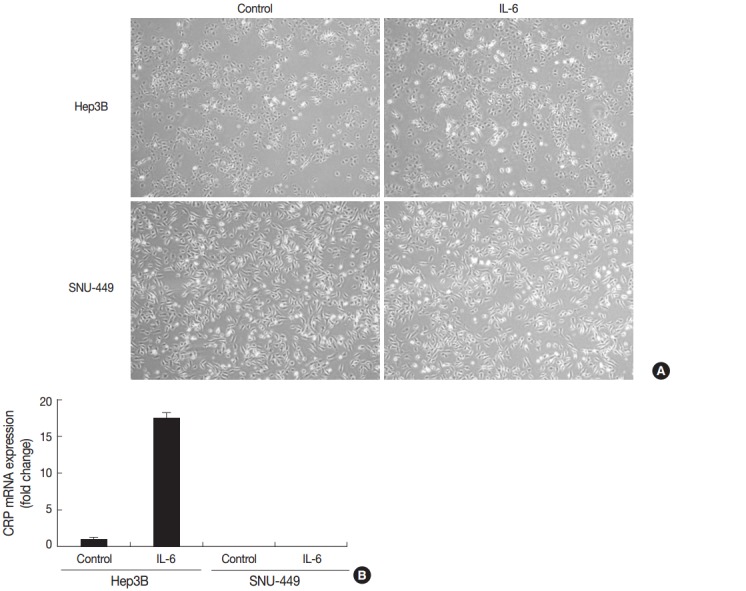
Induction of C-reactive protein (CRP) mRNA in Hep3B and SNU-449 hepatocellular carcinoma cell lines after interleukin 6 (IL-6) treatment. (A) There are no significant changes in cellular morphology in either cell line after IL-6 treatment. (B) There is a 17.5-fold increase in CRP mRNA expression in IL-6–treated Hep3B cells (50 ng/mL for 6 hours), while CRP mRNA expression is not detected in SNU-449 cells. The yaxis represents fold-changes in CRP mRNA expression following IL-6 treatment.
DISCUSSION
The primary findings of this study are (1) CRP expression is relatively common in HCCs, with variable immunoreactivity in nearly 60% of the cases tested, (2) there is an inverse relationship between diffuse and strong CRP immunoreactivity and cancer-specific patient survival (p=.0047), (3) CRP-positive cases in immunoblotting showed significantly higher CRP mRNA expression, suggesting that increased CRP production is a consequence of transcriptional activation of CRP, and (4) CRP mRNA transcription is induced by IL-6 in Hep3B cells, but not in SNU- 449 cells, suggesting that CRP expression marks distinct molecular phenotypes among HCCs.
Hepatocellular carcinogenesis represents a classic model of viral etiology associated with chronic inflammation [23]. The elevation of inflammatory biomarkers such as CRP, IL-6, C-peptide, and adiponectin is associated with a higher risk of HCC [24]. Several investigations have addressed the clinical significance of serum CRP. Serum CRP has been consistently shown to be a key component of inflammation-based prognostication of HCC. Mori et al.[25] proposed that a preoperative scoring system based on the preoperative serum concentration of CRP and alpha-fetoprotein has a prognostic value in patients with HCC after hepatectomy. Although the contribution of CRP produced by tumor cells to the elevation of serum CRP cannot be directly assessed, it is very probable that CRP of tumor origin is released into the systemic circulation. Although we expected certain differences in clinicopathologic characteristics between CRP immunopositive and immunonegative HCCs, a clear difference was found only in the cancer-specific survival of strong CRP immunopositive cases.
One of the major potential drives for CRP overexpression is IL-6, and a role of IL-6 in hepatocellular carcinogenesis has been strongly suggested. When compared to healthy controls, cirrhotic patients and HCC patients had serum IL-6 concentrations that were 4-fold and 25-fold higher, respectively [26]. IL-6 signaling mediated via IL-6 receptors activates STAT3, mitogen-activated protein kinase, and phosphatidylinositol 3-kinase pathways. IL-6–mediated STAT3 activation is known to be a biological link between chronic inflammation and carcinogenesis [27], and IL-6 confers anti-apoptotic effects to cells. Blocking STAT3 activation using STAT3 siRNA or small molecular STAT3 inhibitor LLL 12 has been shown to abrogate the anti-apoptotic effects of IL-6 against doxorubicin-induced apoptosis in SNU- 449 HCC cells, which express a higher level of endogenous IL-6 compared to Hep3B cells [28]. We thought that CRP would be induced in both Hep3B and SNU-449 cells by IL-6 treatment. However, CRP mRNA expression after IL-6 treatment was significantly different between SNU-449 cells and Hep3B cells. Therefore, the observations in HCC tissue samples and the cell lines in vitro indicate that the degree of CRP expression involves several mechanisms, which need further elucidation.
A major drawback of this study is that serum CRP or IL-6 levels could not be determined due to a lack of blood samples. Future analyses of the relationship between the CRP-positive HCC phenotype and systemic inflammatory profile will provide a more comprehensive understanding of the biology of HCC. We also could not determine the underlying biochemical mechanisms involved in the differential IL-6-induced responses between Hep3B and SNU-449 cells in terms of induction of CRP mRNA expression. Considering the complexities of IL-6 signaling and CRP transcription, more in vitro studies are necessary.
In summary, we report the expression of CRP in HCC for the first time, and provide evidence to support the significance of CRP in HCC based on the clear difference in cancer-specific survival between CRP-positive and -negative cases. Overall findings strongly suggest that CRP is a marker for future molecular phenotyping of HCC.
Acknowledgments
This work was supported by a grant (14-521) from the Asan Institute for Life Sciences, Seoul, Korea.
Footnotes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Lazzarotto C, Ronsoni MF, Fayad L, et al. Acute phase proteins for the diagnosis of bacterial infection and prediction of mortality in acute complications of cirrhosis. Ann Hepatol. 2013;12:599–607. [PubMed] [Google Scholar]
- 2.Kushner I, Feldmann G. Control of the acute phase response: demonstration of C-reactive protein synthesis and secretion by hepatocytes during acute inflammation in the rabbit. J Exp Med. 1978;148:466–77. doi: 10.1084/jem.148.2.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Volanakis JE, Kaplan MH. Specificity of C-reactive protein for choline phosphate residues of pneumococcal C-polysaccharide. Proc Soc Exp Biol Med. 1971;136:612–4. doi: 10.3181/00379727-136-35323. [DOI] [PubMed] [Google Scholar]
- 4.Castell JV, Gómez-Lechón MJ, David M, et al. Interleukin-6 is the major regulator of acute phase protein synthesis in adult human hepatocytes. FEBS Lett. 1989;242:237–9. doi: 10.1016/0014-5793(89)80476-4. [DOI] [PubMed] [Google Scholar]
- 5.Castell JV, Gómez-Lechón MJ, David M, Fabra R, Trullenque R, Heinrich PC. Acute-phase response of human hepatocytes: regulation of acute-phase protein synthesis by interleukin-6. Hepatology. 1990;12:1179–86. doi: 10.1002/hep.1840120517. [DOI] [PubMed] [Google Scholar]
- 6.Yoshizaki K. Pathogenic role of IL-6 combined with TNF-alpha or IL-1 in the induction of acute phase proteins SAA and CRP in chronic inflammatory diseases. Adv Exp Med Biol. 2011;691:141–50. doi: 10.1007/978-1-4419-6612-4_15. [DOI] [PubMed] [Google Scholar]
- 7.de Man P, Jodal U, Svanborg C. Dependence among host response parameters used to diagnose urinary tract infection. J Infect Dis. 1991;163:331–5. doi: 10.1093/infdis/163.2.331. [DOI] [PubMed] [Google Scholar]
- 8.Yin G, Hu G, Cang X, et al. C-reactive protein: rethinking its role in evaluating the severity of hyperlipidemic acute pancreatitis. Pancreas. 2014;43:1323–8. doi: 10.1097/MPA.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 9.Lee CH, Chang JS, Syu SH, et al. IL-1beta promotes malignant transformation and tumor aggressiveness in oral cancer. J Cell Physiol. 2015;230:875–84. doi: 10.1002/jcp.24816. [DOI] [PubMed] [Google Scholar]
- 10.Sipos F, Fűri I, Constantinovits M, Tulassay Z, Műzes G. Contribution of TLR signaling to the pathogenesis of colitis-associated cancer in inflammatory bowel disease. World J Gastroenterol. 2014;20:12713–21. doi: 10.3748/wjg.v20.i36.12713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saxena M, Yeretssian G. NOD-like receptors: master regulators of inflammation and cancer. Front Immunol. 2014;5:327. doi: 10.3389/fimmu.2014.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Castaño-Rodríguez N, Kaakoush NO, Mitchell HM. Pattern-recognition receptors and gastric cancer. Front Immunol. 2014;5:336. doi: 10.3389/fimmu.2014.00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Szkandera J, Stotz M, Absenger G, et al. Validation of C-reactive protein levels as a prognostic indicator for survival in a large cohort of pancreatic cancer patients. Br J Cancer. 2014;110:183–8. doi: 10.1038/bjc.2013.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yi JH, Wang D, Li ZY, Hu J, Niu XF, Liu XL. C-reactive protein as a prognostic factor for human osteosarcoma: a meta-analysis and literature review. PLoS One. 2014;9:e94632. doi: 10.1371/journal.pone.0094632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zheng Z, Zhou L, Gao S, Yang Z, Yao J, Zheng S. Prognostic role of C-reactive protein in hepatocellular carcinoma: a systematic review and meta-analysis. Int J Med Sci. 2013;10:653–64. doi: 10.7150/ijms.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nishikawa H, Arimoto A, Wakasa T, Kita R, Kimura T, Osaki Y. Pretreatment C-reactive protein as a prognostic factor for recurrence after surgical resection of hepatocellular carcinoma. Anticancer Res. 2013;33:1181–8. [PubMed] [Google Scholar]
- 17.Bioulac-Sage P, Rebouissou S, Thomas C, et al. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology. 2007;46:740–8. doi: 10.1002/hep.21743. [DOI] [PubMed] [Google Scholar]
- 18.Han J, van den Heuvel MC, Kusano H, de Jong KP, Gouw AS. How normal is the liver in which the inflammatory type hepatocellular adenoma develops? Int J Hepatol. 2012;2012:805621. doi: 10.1155/2012/805621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bioulac-Sage P, Laumonier H, Cubel G, Rossi JZ, Balabaud C. Hepatic resection for inflammatory hepatocellular adenomas: pathological identification of micronodules expressing inflammatory proteins. Liver Int. 2010;30:149–54. doi: 10.1111/j.1478-3231.2009.02098.x. [DOI] [PubMed] [Google Scholar]
- 20.Fonseca S, Hoton D, Dardenne S, et al. Histological and immunohistochemical revision of hepatocellular adenomas: a learning experience. Int J Hepatol. 2013;2013:398308. doi: 10.1155/2013/398308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sempoux C, Chang C, Gouw A, et al. Benign hepatocellular nodules: what have we learned using the patho-molecular classification. Clin Res Hepatol Gastroenterol. 2013;37:322–7. doi: 10.1016/j.clinre.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 22.Kakar S, Grenert JP, Paradis V, Pote N, Jakate S, Ferrell LD. Hepatocellular carcinoma arising in adenoma: similar immunohistochemical and cytogenetic features in adenoma and hepatocellular carcinoma portions of the tumor. Mod Pathol. 2014;27:1499–509. doi: 10.1038/modpathol.2014.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tarocchi M, Polvani S, Marroncini G, Galli A. Molecular mechanism of hepatitis B virus-induced hepatocarcinogenesis. World J Gastroenterol. 2014;20:11630–40. doi: 10.3748/wjg.v20.i33.11630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aleksandrova K, Boeing H, Nöthlings U, et al. Inflammatory and metabolic biomarkers and risk of liver and biliary tract cancer. Hepatology. 2014;60:858–71. doi: 10.1002/hep.27016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mori S, Kita J, Kato M, Shimoda M, Kubota K. Usefulness of a new inflammation-based scoring system for prognostication of patients with hepatocellular carcinoma after hepatectomy. Am J Surg. 2015;209:187–93. doi: 10.1016/j.amjsurg.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 26.Porta C, De Amici M, Quaglini S, et al. Circulating interleukin-6 as a tumor marker for hepatocellular carcinoma. Ann Oncol. 2008;19:353–8. doi: 10.1093/annonc/mdm448. [DOI] [PubMed] [Google Scholar]
- 27.Hodge DR, Hurt EM, Farrar WL. The role of IL-6 and STAT3 in inflammation and cancer. Eur J Cancer. 2005;41:2502–12. doi: 10.1016/j.ejca.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 28.Liu Y, Li PK, Li C, Lin J. Inhibition of STAT3 signaling blocks the anti-apoptotic activity of IL-6 in human liver cancer cells. J Biol Chem. 2010;285:27429–39. doi: 10.1074/jbc.M110.142752. [DOI] [PMC free article] [PubMed] [Google Scholar]


