Abstract
Background
The purpose of this two-phase project was to conduct formative evaluation and test the preliminary efficacy of a newly developed web-based, tailored behavioral preparation program (WebTIPS) for children undergoing outpatient surgery and their parents
Methods
Phase I enrolled 13 children aged 2–7 years undergoing outpatient elective surgery and their parents for formative evaluation of WebTIPS. Parent participation focus groups which are common in qualitative research and are a method of asking research participants about their perceptions and attitudes regarding a product or concept. In phase II, children age 2–7 years in two medical centers were randomly assigned to receive the WebTIPS program (n = 38) compared to children receiving standard of care (n = 44). The primary outcome of phase II was child and parent preoperative anxiety.
Results
In phase I, parents reported WebTIPS to be both helpful (p < 0.001) and easy to use (p < 0.001). In phase II, children in the WebTIPS group (36.2 ± 14.1) were less anxious than children in the standard of care group (46.0 ± 19.0) at entrance to the operating room (p = 0.02; Cohen’s d = 0.59) and introduction of the anesthesia mask (43.5 ± 21.7 vs. 57.0 ± 21.2, respectively, p = 0.01; Cohen’s d = 0.63). Parents in the WebTIPS group (32.1 ± 7.4) also experienced less anxiety compared to parents in the control group (36.8 ± 7.1) in the preoperative holding area (p = 0.004; Cohen’s d = 0.65).
Conclusions
WebTIPS was well received by parents and children and led to reductions in preoperative anxiety.
Introduction
Preoperative preparation for children and families appears to have become a lower priority in the face of health care cost-containment efforts. The majority of pediatric hospitals offered behavioral preparation for children undergoing surgery in the 1990s1 and research has shown that the more extensive the preparation, the greater impact in reducing preoperative anxiety.2 Currently, however, very few hospitals and ambulatory surgery centers offer extensive behavioral preparation of children, and those who do mostly prepare children on the day of surgery. This approach of preparing children on the day of surgery does not allow children the necessary time to learn coping strategies and develop self-efficacy to adequately manage preoperative anxiety. Moreover, in a busy perioperative setting, it is simply not possible to adequately prepare each child-parent dyad on the day of surgery because of the limited time providers have to interact with children in the preoperative area.3
Accordingly, as part of a National Institute of Child Health and Human Development-funded project, our group developed a tailored web-based preparation program (WebTIPS) for children and parents undergoing outpatient surgery. This tailored program includes a fully animated children’s website comprised of education, skills training, and interactive games to prepare children for what to expect before, during, and after surgery and to teach coping strategies to manage perioperative anxiety and pain. WebTIPS also includes a parent website that uses a variety of modalities to provide parents with information, skills training, anxiety management, and modeling techniques to prepare parents for the day of surgery. The reader is directed to the first article in this series for a detailed description of the development and content of WebTIPS.4
Once developed, our group conducted a two-phase evaluation of this novel intervention and the purpose of this article is to present the results of this evaluation process. Phase one consisted of formative evaluation (usability and feasibility) with parents of children who had previously undergone surgery and parents of children who were scheduled for an upcoming outpatient surgery. Phase two consisted of a small-scale randomized controlled trial (RCT) to examine the efficacy of WebTIPS in reducing anxiety in a sample of parents and children before outpatient surgery. It was hypothesized that WebTIPS would result in significantly less preoperative anxiety in both children and parents compared to children receiving standard of care perioperative management, as measured by the modified Yale Preoperative Anxiety Scale (mYPAS) and State-Trait Anxiety Inventory, respectively.
Methods
IRB approval was obtained from Children’s Hospital of Orange County and Yale-New Haven Children’s Hospital. All parents provided written consent and children provided assent when appropriate.
WebTIPS is an empirically based, tailored, innovative, web-based preoperative preparation program for children undergoing surgery and their parents. WebTIPS was designed for children ages 2–7 years and includes a fully animated children’s website as well as a multimedia parent website. The children’s website is tailored based upon children’s trait anxiety and type of surgery and includes information provision, modeling, and coping skills. The parent website is tailored based upon parent baseline anxiety, coping style, pain management attitudes, and preferences for sedative premedication and parental presence at anesthesia induction (PPIA) and includes information provision and coping skills training. Both websites are divided into 4 sections covering the perioperative period: Home (preoperative), preoperative holding area & anesthesia induction & surgery, postanesthesia care unit (PACU), and home (postoperative). WebTIPS is also structured to allow for tailoring based upon hospital and health care provider preferences and standard of care (e.g., use of sedative premedication, parental presence in the operating room [OR], etc.). WebTIPS was designed to complement (rather than replace) standard of care for surgical preparation. The reader is referred to Part 1 of this series in this issue of Anesthesia & Analgesia for a detailed description of WebTIPS.4
Phase I: Formative Evaluation
A focus group is common in qualitative research and is a method of asking research participants about their perceptions and attitudes regarding a product or concept. Focus groups are useful to generate qualitative data because participants can stimulate discussion among one another in addition to the interview questions that are asked.
Children aged 2–7 years undergoing outpatient elective surgery and their parents were enrolled in this phase of the study (n=13). Seven parent-child dyads were enrolled after having recently undergone surgery (postoperative group) and 6 parent-child dyads were enrolled 5–10 days before undergoing surgery (preoperative group). Exclusion criteria included developmental delays, premature birth (less than 32 weeks), and ASA status III or higher. Parents were given instructions to access WebTIPS at home and the content/usability measure after completion of the intervention. All parents participated in an individual interview and a focus group with two interviewers and 2–3 other parents, which were audio recorded. Parents rated the usability and likeability of each WebTIPS module on a 5-point Likert-type scale (0–4), with higher scores indicating more positive responses (very helpful or very useful). Participants were also asked open-ended questions regarding the content and ease of navigation. As part of the feasibility/usability testing, parents also participated in a one-on-one interview with the researchers to ask additional questions and complete quantitative usability/likeability measures about WebTIPS.
Data Analysis
The sample size for formative evaluation was determined by theoretical saturation, which is determined by review of data collected such that new information is no longer being generated.5 All audio recordings were transcribed and the text files were uploaded into Dedoose, a web-based mixed methods analysis program. Data were analyzed in two ways: 1) content analysis of the audio recordings using Dedoose to identify narrative themes, and 2) statistical analysis of quantitative data from the content/usability measure. Using content analysis, we identified analytical categories, as evidenced by salient verbatim quotes from the transcripts. Dedoose was useful for organizing these categories with the salient quotes (or raw data) to support the categories. After performing content analysis of the data two times, indexed categories were refined and reduced, and frequencies of responses within each category were calculated. Quantitative data from content/usability measure were coded and analyzed using SPSS. Nonparametric One-Sample Wilcoxon Signed Rank Tests were performed to test whether parent ratings were different from the midpoint of the scale. Median values and interquartile ranges are reported.
Phase II: Preliminary RCT
Participants included 82 English-speaking parent-child dyads scheduled to undergo outpatient surgery and general anesthesia at Children’s Hospital of Orange County or Yale-New Haven Children’s Hospital between August 2011 and August 2012. Inclusion criteria included: children ASA classification I and II (children in good health) between the ages of 2–7 years, born at least 32 weeks gestational age, and without any developmental delays or cognitive impairment. Children were excluded from participation if they were ASA status III or higher, were receiving services for developmental delay or cognitive impairment that would preclude participating in WebTIPS and may impact surgical recovery, and were non-English speaking given that WebTIPS is currently available only in English. Children with previous experience with surgery and/or anesthesia were not excluded from participation.
Measures
Child Temperament: Emotionality Activity Sociability Temperament Survey (EAS-TS):6
This tool assesses temperament of the child through parental report and the reader is referred to previous articles detailing its psychometric properties.6–8
Parent-Coping: Miller Behavioral Style Scale:9
The Miller Behavioral Style Scale assesses parental coping style and identifies individuals as information seekers (monitors) or information avoiders, and distracters (blunters). This measure has excellent reliability and validity.9
Modified Yale Preoperative Anxiety Scale:10
This is a well validated observational measure of children’s preoperative anxiety that is widely used in experimental protocols.10,11 To obtain interrater and intrarater reliability for the current study, three research associates were trained using a standardized protocol developed within the University of California Irvine Center for Stress & Health. In the first phase of training, raters learn the mYPAS manual, which describes the purpose, administration, and scoring of the measure. In the second phase, raters in training and previously trained raters score videos as a group and discuss their scoring decisions. In the final phase, raters in training score videos alone and have their scores compared to previously trained raters’ scores. Any discrepancies between scores are discussed. This procedure is continued until raters in training achieve intra and inter-reliability scores (Kappa) of at least 0.80.
Parent Anxiety: State-Trait Anxiety Inventory:12,13
This is a widely used self-report assessment instrument for adults that measures trait and state anxiety and the reader is referred to previous publications detailing its psychometric properties.13
Pediatric Anesthesia Emergence Delirium:14
This is a validated 5-item measure of emergence delirium that assesses specific behavioral components that are distinct from pain.14 Each of the 5 items is rated on a 0 to 4 scale and summed to provide a continuous score from 0 to 20. Higher scores are associated with increased emergence delirium.
Other Outcome Data
Intraoperative and PACU data were abstracted from medical records, including analgesics administered, length of surgery, length of PACU stay, and nurse-rated pain severity (0–10 numeric rating scale).
Study Procedures
In order to assure external validity of this study we chose not to standardize any of the clinical management of the participants. That is, all participants of this study were managed based on the standard of care of the particular institution and the particular health care provider.
Preoperative Period
Interested participants provided informed consent and were assigned to either the WebTIPS or standard of care group based on a computer-generated random number sequence. Allocation concealment was obtained using the computer-generation protocol. Although it was not possible to mask participants or health care providers to group assignment, the research associates (RAs) responsible for data collection were masked. Specifically, RAs who did not recruit patients were responsible for all participant phone calls during the recruitment process. In addition, in order to maintain masking on the day of surgery, the recruiting RAs were given a blank envelope to be given to the health care provider that either contained the patient-specific Web-TIPS information or a blank “control” slip of paper. Providers were advised to use their usual clinical care that may include preoperative midazolam, child life preparation, PPIA and any other intervention they routinely use.
WebTIPS Group
Before surgery, families were provided instructions via email on how to access WebTIPS from home. The email included a direct link to the website as well as log in information. Parents were supplied with a unique password to enable them access to the WebTIPS website as many times as desired starting 7 days before surgery and until 7 days after surgery. A research email account was established to allow parents to e-mail the researchers with any questions or problems. When possible, anesthesiologists were also provided with output of child and parent data on the day of surgery. The output of the clinician component included the child’s favorite interests and activities (to be used for distraction) and summary information regarding anxiety and coping style of the parent, parent preference for PPIA and sedative premedication. Children in the WebTIPS group received standard of care along with the WebTIPS intervention.
Standard of Care Group
Participants in the standard of care group were provided the usual care in the institution.
Day of Surgery
In the preoperative holding both groups of children and parents were handled based on the standard of care of each of the two institutions that were part of this study. During the intraoperative and postoperative periods, the anesthetic and medical management was conducted as the standard of care and was not controlled for the study groups. A trained research associate assessed child anxiety (m-YPAS) at 3 time points: separation to the OR, entrance to the OR, and introduction of the anesthesia mask to the child. Parents provided self-report ratings of anxiety in the preoperative holding area and upon separation to go to the OR. The RAs obtained data in the PACU including emergence delirium, analgesic consumption, pain ratings, and length of stay.
Statistical Analysis
Power analysis was conducted based upon expected differences in mean anxiety scores (mYPAS) at induction of anesthesia to determine necessary sample size. Anticipating an effect size of 0.5–0.6 based upon our previous work,15 it was determined that a minimum of 35 children was necessary per group with power set at .80 and an alpha of .05 to detect group differences in children’s anxiety at anesthesia induction. Descriptive analyses, including frequencies, means, and medians, were calculated to explore baseline and demographic variables of the study sample as a whole and for the two study groups separately. Independent samples t-tests, Kruskal-Wallis nonparametric ANOVA, and chi-square analyses were conducted to examine group differences in baseline and demographic variables. Independent samples t-tests and repeated measures ANOVA were used to examine group differences in preoperative anxiety and the effects of group assignment on children’s anxiety over time. Cohen’s d was calculated as a measure of effect size. It is generally accepted that a “small” effect size is 0.20, a “medium” effect size is 0.50, and a “large” effect size is 0.80.16 Data presented as mean ± standard deviation satisfied the Kolmogorov-Smirnov (K-S) test with Lilliefors correction (p > 0.07) unless otherwise noted in table legends. Skewed data are presented as median and interquartile range (75% - 25%).
Results
Phase I: Formative Evaluation
Parents who participated in formative evaluation were primarily mothers (92.3%) and non-Hispanic Caucasian (76.9%). Parents reported a mean 32.0 ± 5.0 years of age and 13.8 ± 2.3 years of education. The children of parent participants were primarily (84.6%) undergoing ear-nose-throat procedures (tonsillectomy and adenoidectomy were the most frequent surgery).
Content Analysis
Parents analysis
After analysis of all transcripts we identified several dominant responses among focus group participants (Distraction to Reduce Children’s Preoperative Anxiety; Relaxation Techniques for Parent Anxiety; Waking up in the PACU; Exposure to the Anesthesia Mask: Recovery from Surgery: Ease of use). In cases where a consistent negative response was identified to a particular item on WebTIPS, revisions were made to the website.
Child Analysis
Eleven parents reported their child used the child website, with nine parents (81.8%) indicating their children were engaged and two parents (18.20%) reporting their children were not engaged, both of whom acknowledged their children were younger than the intended age range.
Usability Analysis
Median ratings for the helpfulness measure were significantly greater than the midpoint (“moderately helpful”) of the scale for each of the modules: home before surgery (3.50 [1.0], p = 0.029), waiting area and induction (4.00 [1.0], p = 0.002), PACU (3.50 [1.0], p = 0.004), and home after surgery (4.00 [1.0], p = 0.030). Mean ratings of ease of use for all modules of WebTIPS were significantly greater than the midpoint (“neither easy nor difficult”) of the scale for each of the modules: home before surgery (4.00 [0], p = 0.001), waiting area and induction (4.00 [0.75], p = 0.002), PACU recovery (4.00 [0], p = 0.001), and home after surgery (4.00 [0], p = 0.006).
Phase II: Randomized Controlled Trial
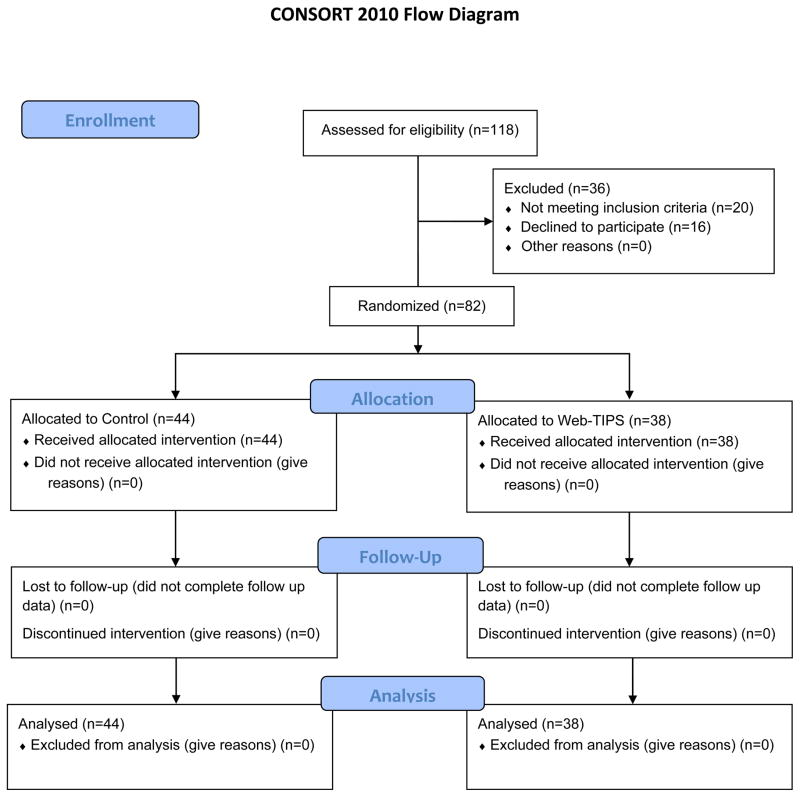
Participants were recruited and data collected from August 2011 through August 2012, at which point the proposed sample size had been recruited (Figure 1). There were no differences in demographic or baseline data between children and parents across the study sites with the exception of race/ethnicity, with a larger percentage of Hispanic/Latino children in California (40%) compared to Connecticut (17%), p = 0.01). Across sites, 71% of children received sedative premedication and 22% of participants received PPIA; these practices did not differ between the experimental groups (Table 1). In terms of intervention adherence, the majority of families in the WebTIPS group accessed all modules of the preparation program. Each website (parent and child) has 4 modules. All 38 parents accessed modules 1 and 2 of the parent website. One parent did not access modules 3 and 4, and one parent did not access module 4. In terms of the child website, all families accessed modules 1–3, whereas 7 families did not access module 4.
Figure 1.
Consort Flow Diagram illustrating progress through the phases of the randomized trial, including enrollment, intervention allocation, follow-up, and data analysis. WebTIPS = Web-based Tailored Intervention for Preparation of parents and children undergoing Surgery
Table 1.
Baseline and Demographic Characteristics
| Group
| |||
|---|---|---|---|
| Baseline Variable | WebTIPS n = 38 |
Standard Care n = 44 |
p |
| Child Age (Mean ± SD) | 4.3 ± 1.8 | 4.4 ± 1.7 | 0.73a |
| Child Gender (n, [%male]) | 24 (50%) | 22 (58%) | 0.76b╪ |
| Race/Ethnicity (%) | 0.97b | ||
| Caucasian | 42.1 | 43.2 | |
| Hispanic/Latino | 34.2 | 34.1 | |
| Asian | 7.9 | 6.8 | |
| African American | 2.6 | 2.3 | |
| Multiracial | 13.2 | 11.4 | |
| Other/missing | 0 | 2.3 | |
| Procedure (%) | 0.14b | ||
| ENT | 54 | 59 | |
| General | 5 | 23 | |
| Urology | 22 | 7 | |
| Ophthalmology | 14 | 7 | |
| Plastics | 3 | 2 | |
| Orthopedic | 3 | 2 | |
| Child Temperament (EAS-TS) (Mean ± SD) | |||
| Emotionality | 2.6 ± 0.96 | 2.8 ± 1.0 | 0.29a |
| Shyness | 2.4 ± 0.80 | 2.4 ± 0.84 | 0.93a |
| Activity | 4.1 ± 0.76 | 4.3 ± 0.57 | 0.24a╪ |
| Sociability | 3.6 ± 0.47 | 3.6 ± 0.57 | 0.99a╪ |
| Family Income | 0.54b | ||
| Category $ (%) | |||
| < 10,000 | 13.2 | 9.1 | |
| 11–20,000 | 10.5 | 13.6 | |
| 21–30,000 | 5.3 | 9.1 | |
| 31–50,000 | 7.9 | 15.9 | |
| 51–80,000 | 7.9 | 4.5 | |
| 81–100,000 | 23.7 | 2.3 | |
| >100,000 | 23.7 | 40.9 | |
| Did not report | 7.9 | 4.5 | |
| Parent Age (Mean yrs. ± SD) | 34.7 ± 8.0 | 33.1 ± 6.8 | 0.34a |
| Parent Education (Mean yrs. ± SD) | 15.1 ± 3.3 | 15.6 ± 3.3 | 0.48a |
| Parent Coping (Mean ±SD) | |||
| Blunter | 3.3 ± 2.2 | 3.4 ± 2.5 | 0.83a |
| Monitor | 8.4 ± 3.2 | 7.5 ± 3.1 | 0.18a |
Note. ENT = ear, nose, throat; EAS-TS = Emotionality, Activity, Sociability Temperament Survey; webTIPS = Web-based Tailored Intervention for Preparation of parents and children undergoing Surgery
Indicates Independent samples t-test was used to analyze group differences.
Indicates chi-square analysis was used to analyze group differences.
Due to non-normality of data, child age and EAS activity and sociability were also analyzed using median comparison with equivalent results for age (p = 0.77), activity (p = 0.51), and sociability (p = 0.50).
Intraoperative Period
All intraoperative analgesics were converted to morphine equivalents and independent samples t-tests revealed no significant differences between the WebTIPS and control groups (p = 0.85). Intraoperative analgesic data are presented in Table 2.
Table 2.
Intraoperative Analgesics and Length of Surgery
| WebTIPS Mean ± SD |
Control Mean ± SD |
p-value | |
|---|---|---|---|
| Morphine (mg/kg) | 0.09 ± 0.01 | 0.17 ± 0.36 | 0.741 |
| Meperidine (mg/kg) | 0.76 ± 0.30 | 0.74 ± 0.32 | 0.825 |
| Fentanyl (mcg/kg) | 1.40 ± 0.47 | 1.48 ± 0.89 | 0.856 |
| Acetaminophen (mg/kg) | 26.62 ± 2.26 | 29.34 ± 5.10 | 0.204 |
| Length of surgery (mins) | 35 ± 22 | 33 ± 18 | 0.708 |
webTIPS = Web-based Tailored Intervention for Preparation of parents and children undergoing Surgery
Independent samples t-tests were used to analyze group differences.
Due to unequal variances, a Mann-Whitney U test was also used to examine group differences.
No significant differences were found for morphine (p = 0.239), meperidine (p = 0.750), fentanyl (p = 0.947), or length of surgery (p = 0.936). Significant differences were found for acetaminophen (p = 0.027).
Primary Outcome - Preoperative Anxiety
Independent samples t-tests revealed that children in the WebTIPS group experienced significantly lower anxiety at entrance to the OR (t(72) = 2.5, p = 0.02) and at introduction of anesthesia mask (t(72) = 2.7, p = 0.01) as compared to children in the standard care (Table 3). There were no significant site differences in children’s anxiety scores at entrance to the OR (p = 0.66) or mask introduction (p = 0.90).
Table 3.
Primary Outcomes – Child and Parent Preoperative Anxiety
| WebTIPS Mean ± SD |
Control Mean ± SD |
p-value | 95% CI of Mean Difference | Cohen’s d | |
|---|---|---|---|---|---|
| Child mYPAS | (n = 33) | (n = 41) | |||
| Separation to OR | 36.4 ± 12.7 | 40.7 ± 16.6 | 0.23 | −2.7 to 11.2 | 0.29 |
| Entrance to OR | 36.2 ± 14.1 | 46.0 ± 19.0 | 0.02 | 1.9 to 17.7 | 0.59 |
| Introduction of Mask | 43.5 ± 21.7 | 57.0 ± 21.2 | 0.01 | 3.5 to 23.5 | 0.63 |
| Parent STAI | (n = 38) | (n = 42) | |||
| Preoperative Holding | 32.7 ± 7.9 | 36.8 ± 7.1 | 0.004 | 0.7 to 7.4 | 0.65 |
| Separation to OR | 43.8 ± 13.4 | 47.2 ± 12.8 | 0.26 | −2.5 to 9.2 | 0.25 |
Note. mYPAS = modified Yale Preoperative Anxiety Scale; OR = Operating Room; STAI = State-Trait Anxiety Inventory. CI = Confidence Interval; webTIPS = Web-based Tailored Intervention for Preparation of parents and children undergoing Surgery mYPAS data are missing from 8 participants due to inability to access OR; STAI data are missing from 3 parents due to lack of time to complete measure.
Independent samples t-tests were used to analyze group differences.
Due to non-normality of data, child mYPAS data were also analyzed using median comparison with equivalent results for separation to OR (p = 0.47), entrance to OR (p = 0.01), and introduction of mask (p = 0.03).
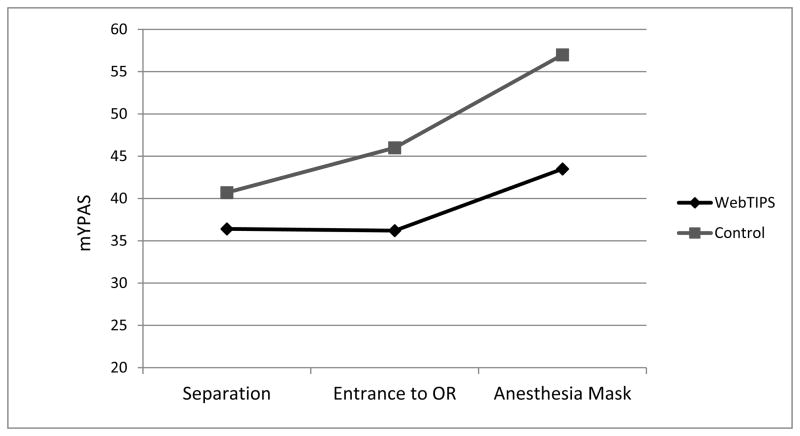
A repeated measures ANOVA revealed a significant effect of time (F(2, 72) = 11.9, p < 0.001) suggesting anxiety increased significantly across the preoperative period. There may also have been an interaction of time and group (F(1, 72) = 3.8, p = 0.05), indicating that for the WebTIPS group, anxiety stayed relatively stable from separation to entrance to the OR, increasing only at introduction to the anesthesia mask. Conversely children in the standard care group experienced a significant increase in anxiety at each of the 3 time points (Figure 2).
Figure 2.
Illustration of the significant interaction of time and experimental group on children’s anxiety across the preoperative period. mYPAS = mYPAS = modified Yale Preoperative Anxiety Scale; OR = operating room; WebTIPS = Web-based Tailored Intervention for Preparation of parents and children undergoing Surgery
Preoperative Anxiety - Parents
Independent samples t-tests revealed that although no differences emerged with State-Trait Anxiety Inventory scores at separation to the OR (p = 0.26), parents in the WebTIPS group experienced significantly lower anxiety in the preoperative holding area (t(78) = 2.43, p = 0.02) compared to parents in the standard care group (Table 3). There were no site differences in parent’s anxiety scores in the holding area (p = 0.80) or at separation to the OR (p = 0.30).
A repeated measures ANOVA revealed a significant effect of time (F(1, 77) = 50.6, p < 0.001) suggesting parental anxiety increased significantly across the preoperative period. There was no significant interaction of time and group (p = 0.71), suggesting that the increase in anxiety between the experimental groups was similar, despite parents in the WebTIPS groups experiencing significantly less anxiety in the preoperative holding area.
PACU Period
Children in the WebTIPS group may have experienced significantly lower emergence delirium compared to children in the control group on the Pediatric Anesthesia Emergence Delirium test, [t(75) = 2.01, p = 0.04, Cohen’s d = 0.45, 95% CI = 0.06 to 2.71] (Table 4). No differences were observed in nurse-rated pain severity (0–10 numeric rating scale) or analgesics administered in the PACU between groups (Table 4).
Table 4.
Postanesthesia Care Unit Recovery Variables
| PACU Variable | WebTIPS | Control | p-value |
|---|---|---|---|
| PAED (Mean ± SD) | 12.3 ± 2.9 | 13.6 ± 2.9 | 0.04a |
| Nurse-rated pain (Median, IQR) | 0 (0.67) | 0.38 (1.76) | 0.30c |
| Analgesics (Median mg/kg, mcg/kg, IQR) | |||
| Morphine (mg/kg) | 0.11 (0) | 0.05 (0.01) | 0.22c |
| Meperidine (mg/kg) | 0.48 (0.23) | 0.31(0.20) | 0.36c |
| Fentanyl (mcg/kg) | 1.84 (0) | 0.84 (0.83) | 0.37c |
| Hydrocodone (mg/kg) | 0.10 (0) | 0.10 (0) | 0.74c |
| Acetaminophen (mg/kg) | 12.09 (0) | 6.58 (0) | 0.42c |
| Time to discharge in minutes (Median, IQR) | 71 (68) | 88 (54) | 0.26c |
Note. PAED = Pediatric Anesthesia Emergence Delirium Scale; IQR = interquartile range; webTIPS = Web-based Tailored Intervention for Preparation of parents and children undergoing Surgery; PACU = postanesthesia care unit
Study was not powered to detect group differences in postoperative recovery variables.
Indicates independent samples t-test was used to analyze group differences.
Indicates Kruskal-Wallis nonparametric ANOVA was used to analyze group differences.
Discussion
Under the conditions of this small-scale preliminary trial, we demonstrated that a web-based tailored preoperative preparation program is an effective intervention for reducing children’s and parents’ anxiety before surgery and may be effective for reducing emergence delirium after surgery. Also, although results did not reach statistical significance, PACU stay for children in the WebTIPS group was shorter by 17 minutes compared to the control group, which is clinically significant given the median PACU stay for both groups was just over 60 minutes. It is important to note that there were no differences in either baseline or outcome data between hospitals in this multisite study.
WebTIPS is unique in a number of ways. First, it is a tailored intervention and includes not only surgical characteristics of the child in the tailoring matrix, but personality and baseline characteristics of both parents and children. Tailored interventions are more refined and complex than targeted interventions and can be customized to an individual’s situation and needs.17–22 More specifically, computer tailoring is a relatively new technique that has gained popularity in health care during the last decade.19,20,22–24 Computer tailoring has been shown to efficiently convey information in a number of health areas.18,20,25 Second, there is a move in health care to incorporate health information technology to increase access to patients, increase patient engagement in health care, and improve health care provider-patient communication and decision-making in order to minimize the gap between evidence and practice.26–28 There is empirical evidence that the use of computer-based decision support, for example, can positively impact management of pain29 and can lead to significant improvements in clinical care, including use of appropriate treatment.29–32 Moreover, data from the Pew Internet and American Life Project revealed a dramatic increase in internet usage over the past two decades and indicated that as of 2014, more than 87% of American adults and 95% of teens use the internet.33 Given the limited time health care providers are able to spend with patients on the day of surgery,3 which is when the majority of preoperative preparation is offered, means of widespread access to patients before surgery is needed and web-based interventions fill this gap. Third, WebTIPS is grounded in empirical evidence and is directed at outcomes that are measurable and clinically significant to children, parents, and health care providers.
This preliminary efficacy study of WebTIPS suggests that it is a well-accepted, feasible intervention to implement and demonstrate positive impacts on patient-reported and clinical variables of interest in the perioperative setting. It will also be important to examine postoperative data, namely postoperative pain and analgesic administration in the home setting. In addition, behavioral recovery after surgery is an important domain given that preoperative anxiety and emergence delirium have direct associations with postoperative behavioral recovery.34 Accordingly, postoperative pain, analgesic administration at home, and behavioral recovery will be assessed in a future large-scale effectiveness RCT across multiple institutions. In addition, a cost-benefit analysis is needed. Given that WebTIPS is currently capable of being modified to be hospital- or surgery center-specific (e.g., insert hospital logo, modify content to be consistent with hospital practice), does not require any additional hospital visits to be administered, and can be accessed independent of health care provider administration, we expect WebTIPS to prove more cost effective than current means of behavioral preparation. That said, because WebTIPS is associated with software-related costs an official cost-benefit analysis is needed. Finally, increasing the interactivity of the program, such as by allowing users to ask real-time questions, may be an important avenue to consider for future web-based preparation programs.
Several methodological issues related to this article have to be addressed. First, we decided a priori to conduct this trial in two institutions in order to test WebTIPS over a variety of surgical procedures and practices of parental presence and sedative premedication. Indeed, we have demonstrated that WebTIPS is effective in the context of the conditions of the trial. Although this allowed a high level of external validity, it does raise the possibility of confounding effects of various anesthetic drugs on variables such as emergence delirium. Nonetheless, because patients were randomized, it is likely that any such possible confounding effects were eliminated. The next steps in this program of research are to implement a large-scale trial of WebTIPS in order to examine a wider range of behavioral and clinical outcomes, including PACU recovery time, postoperative pain management at home, and family and health care provider satisfaction.
In addition, although a strength of WebTIPS is that it includes preparation in management of pain after surgery, the present study was not powered to examine the impact of the intervention on postoperative pain and analgesic administration as outcomes. Moreover, a larger trial would allow for examination of the effects of adherence to the intervention on perioperative outcomes as well as determination of the effective components of WebTIPS. Finally, it is not known to what extent families may have sought out additional, external sources of preparation information via the internet and what impact this might have had on the outcomes.
In conclusion, WebTIPS was shown to result in improved immediate behavioral outcomes, including decreased preoperative anxiety in parents and children and decreased emergence delirium in children undergoing surgery. WebTIPS was well received overall by families and has widespread applicability and access, particularly given the increasing rates of Internet usage among adults and children. WebTIPS has the potential to transform the delivery of behavioral interventions for children and families undergoing surgery, will likely reduce hospital costs, and can reach a broad health care provider and patient base. WebTIPS capitalizes upon use of the web, which is a medium that the majority of families in the United States engage with regularly. In addition, this novel program uses a variety of multimedia components (e.g., animation, motion graphics, video, audio), which resulted in an engaging program from which families could easily learn preparation skills needed for preoperative anxiety and postoperative pain management in real time and repeatedly, which we believe contributed to the success of WebTIPS. Our goal is that WebTIPS become standard of care in hospitals across the country.
Acknowledgments
Funding: This work was funded by National Institutes of Health 5R01HD056104-02 (PI: Zeev N. Kain, MD)
Footnotes
The authors declare no conflicts of interest.
DISCLOSURES:
Name: Michelle A. Fortier, PhD
Contribution: This author helped design and conduct the study, analyzed the data, and helped prepare the manuscript.
Attestation: Michelle Fortier approved the final manuscript and attests to the integrity of the original data and the analysis reported in this manuscript.
Name: Elizabeth Bunzli, BS
Contribution: This author helped collect and analyze the data.
Attestation: Elizabeth Bunzli approved the final manuscript.
Name: Jessica Walthall, BS
Contribution: This author helped collect and analyze the data.
Attestation: Jessica Walthall approved the final manuscript.
Name: Ellen Olshansky, PhD
Contribution: This author helped with data analysis and manuscript preparation.
Attestation: Ellen Olshansky approved the final manuscript.
Name: Haleh Saadat, MD
Contribution: This author helped design and conduct the study.
Attestation: Haleh Saadat approved the final manuscript.
Name: Ricci Santistevan, CCLS
Contribution: This author helped design and conduct the study and assisted with manuscript preparation.
Attestation: Ricci Santistevan approved the final manuscript.
Name: Linda Mayes, MD
Contribution: This author helped design and conduct the study and assisted with manuscript preparation.
Attestation: Linda Mayes approved the final manuscript.
Name: Zeev N. Kain, MD, MBA
Contribution: This author helped design and conduct the study, analyzed the data, and helped prepare the manuscript.
Attestation: Zeev Kain approved the final manuscript and attests to the integrity of the original data and the analysis reported in this manuscript. Zeev Kain is the archival author.
This manuscript was handled by: James A. DiNardo, MD
Reprints will not be available from the authors.
Contributor Information
Michelle A. Fortier, Department of Anesthesiology and Perioperative Care, University of California, Irvine School of Medicine, Irvine, California; UCI Center on Stress & Health, Irvine, California.
Elizabeth Bunzli, Department of Anesthesiology and Perioperative Care, University of California, Irvine, Irvine, California.
Jessica Walthall, Department of Anesthesiology, Yale School of Medicine, New Haven, Connecticut.
Ellen Olshansky, School of Nursing Science, University of California, Irvine, Irvine, California.
Haleh Saadat, Department of Anesthesiology, Yale School of Medicine, New Haven, Connecticut.
Ricci Santistevan, Child Life Department, CHOC Children’s Hospital, Orange, California.
Linda Mayes, Child Study Center, Yale University, New Haven, Connecticut.
Zeev N. Kain, Department of Anesthesiology & Perioperative Care, University of California, Irvine School of Medicine, Irvine, California; Director, UCI Center on Stress & Health, Irvine, California.
References
- 1.O’Byrne K, Peterson L, Saldana L. Survey of pediatric hospitals’ preparation programs: Evidence of the impact of health psychology research. Health Psychol. 1997;16:147–54. doi: 10.1037//0278-6133.16.2.147. [DOI] [PubMed] [Google Scholar]
- 2.Kain ZN, Caramico LA, Mayes LC, Genevro JL, Bornstein MH, Hofstadter MB. Preoperative preparation programs in children: a comparative examination. Anesth Analg. 1998;87:1249–55. doi: 10.1097/00000539-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Kain ZN, MacLaren JE, Hammell C, Novoa C, Fortier MA, Huszti H, Mayes L. Healthcare provider-child-parent communication in the preoperative surgical setting. Pediatric Anesthesia. 2009;19:376–84. doi: 10.1111/j.1460-9592.2008.02921.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kain ZN, Fortier MA, Chorney JM, Mayes L. Web-based Tailored Intervention for Preparation of Parents and Children for Outpatient Surgery (WebTIPS): Development. Anesth Analg. 2015 doi: 10.1213/ANE.0000000000000610. IN THIS ISSUE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Strauss AL, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- 6.Buss AH, Plomin R. Theory and Measurement of EAS Temperament: Early Developing Personality Traits. Hillsdale: L. Erlbaum Associates, New Jersey; 1984. [Google Scholar]
- 7.Gibbs MV, Reeves D, Cunningham CC. The application of temperament questionnaires to a british sample: Issues of reliability and validity. J Child Psychol Psychiatr. 1987;28:61–77. doi: 10.1111/j.1469-7610.1987.tb00652.x. [DOI] [PubMed] [Google Scholar]
- 8.Plomin R, Dunn J. The study of temperament: Changes, continuities, and challenges. Hillsdale, NJ: Erlbaum; 1986. [Google Scholar]
- 9.Miller S. Monitoring and blunting: Validation of a questionnaire to assess styles of information seeking under threat. J Pers Soc Psychol. 1987;52:345–53. doi: 10.1037//0022-3514.52.2.345. [DOI] [PubMed] [Google Scholar]
- 10.Kain ZN, Mayes LC, Cicchetti DV, Bagnall AL, Finley JD, Hofstadter MB. The Yale Preoperative Anxiety Scale: how does it compare with a “gold standard”? Anesth Analg. 1997;85:783–8. doi: 10.1097/00000539-199710000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Kain Z, Mayes LC, Cicchetti DV, Caramico LA, Spieker M, Nygren MM, Rimar S. Measurement tool for preoperative anxiety in young children: The Yale Preoperative Anxiety Scale. Child Neuropsychology. 1995;1:203–10. [Google Scholar]
- 12.Spielberger C, Gorsuch R, Lushene R. State-trait anxiety inventory manual. Palo Alto, CA: Consulting Psychologist Press; 1970. [Google Scholar]
- 13.Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI: Form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. pp. 4–26. [Google Scholar]
- 14.Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004;100:1138–45. doi: 10.1097/00000542-200405000-00015. [DOI] [PubMed] [Google Scholar]
- 15.Kain ZN, Caldwell-Andrews AA, Mayes LC, Weinberg ME, Wang SM, MacLaren JE, Blount RL. Family-centered preparation for surgery improves perioperative outcomes in children: a randomized controlled trial. Anesthesiology. 2007;106:65–74. doi: 10.1097/00000542-200701000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, New Jersey: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 17.De Vries H, Brug J. Computer-tailored interventions motivating people to adopt health promoting behaviours: introduction to a new approach. Patient Educ Couns. 1999;36:99–105. doi: 10.1016/s0738-3991(98)00127-x. [DOI] [PubMed] [Google Scholar]
- 18.Dijkstra A, De Vries H. The development of computer-generated tailored interventions. Patient Educ Couns. 1999;36:193–203. doi: 10.1016/s0738-3991(98)00135-9. [DOI] [PubMed] [Google Scholar]
- 19.Brug J, Campbell M, van Assema P. The application and impact of computer-generated personalized nutrition education: a review of the literature. Patient Educ Couns. 1999;36:145–56. doi: 10.1016/s0738-3991(98)00131-1. [DOI] [PubMed] [Google Scholar]
- 20.Brug J, Steenhuis IHM, Van Assema P, De Vries H. The impact of a computer-tailored nutrition intervention. Prev Med. 1996;25:236–42. doi: 10.1006/pmed.1996.0052. [DOI] [PubMed] [Google Scholar]
- 21.Lauver DR, Ward SE, Heidrich SM, Keller ML, Bowers BJ, Brennan PF, Kirchhoff KT, Wells TJ. Patient-centered interventions. Research in Nursing & Health. 2002;25:246–55. doi: 10.1002/nur.10044. [DOI] [PubMed] [Google Scholar]
- 22.Kreuter MW, Wray RJ. Tailored and targeted health communication: strategies for enhancing information relevance. Am J Health Behav. 2003;27:s227–3. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- 23.Kreuter MW, Skinner CS. Tailoring: what’s in a name? Health Educ Res. 2000:1–4. doi: 10.1093/her/15.1.1. [DOI] [PubMed] [Google Scholar]
- 24.Oenema A, Brug J, Lechner L. Web-based tailored nutrition education: results of a randomized controlled trial. Health Education Research. 2001;16:647–60. doi: 10.1093/her/16.6.647. [DOI] [PubMed] [Google Scholar]
- 25.Rakowski W, Clark MA, Ehrich B. Smoking and cancer screening for women ages 42–75: associations in the 1990–1994 National Health Interview Surveys. Prev Med. 1999;29:487–95. doi: 10.1006/pmed.1999.0578. [DOI] [PubMed] [Google Scholar]
- 26.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, Spurr C, Khorasani R, Tanasijevic M, Middleton B. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10:523–30. doi: 10.1197/jamia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the Frequency of Errors in Medicine Using Information Technology. J Am Med Inform Assoc. 2001;8:299–308. doi: 10.1136/jamia.2001.0080299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blumenthal D, Glaser JP. Information Technology Comes to Medicine. N Engl J Med. 2007;356:2527–34. doi: 10.1056/NEJMhpr066212. [DOI] [PubMed] [Google Scholar]
- 29.Knab JH, Wallace MS, Wagner RL, Tsoukatos J, Weinger MB. The Use of a Computer-Based Decision Support System Facilitates Primary Care Physicians’ Management of Chronic Pain. Anesth Analg. 2001;93:712–20. doi: 10.1097/00000539-200109000-00035. [DOI] [PubMed] [Google Scholar]
- 30.Evans RS, Pestotnik SL, Classen DC, Clemmer TP, Weaver LK, Orme JF, Lloyd JF, Burke JP. A Computer-Assisted Management Program for Antibiotics and Other Antiinfective Agents. N Engl J Med. 1998;338:232–8. doi: 10.1056/NEJM199801223380406. [DOI] [PubMed] [Google Scholar]
- 31.Hunt DL, Haynes RB, Hanna SE, Smith K. Effects of Computer-Based Clinical Decision Support Systems on Physician Performance and Patient Outcomes: A Systematic Review. JAMA. 1998;280:1339–46. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 32.Pestotnik SL, Classen DC, Evans RS, Burke JP. Implementing Antibiotic Practice Guidelines through Computer-Assisted Decision Support: Clinical and Financial Outcomes. Ann Intern Med. 1996;124:884–90. doi: 10.7326/0003-4819-124-10-199605150-00004. [DOI] [PubMed] [Google Scholar]
- 33.Pew Internet & American Life Project. [Accessed April 30, 2014];Internet User Demogrphics. 2014 Available at: http://www.pewinternet.org/data-trend/internet-use/latest-stats/
- 34.Kain ZN, Caldwell-Andrews AA, Maranets I, McClain B, Gaal D, Mayes LC, Feng R, Zhang H. Preoperative anxiety and emergence delirium and postoperative maladaptive behaviors. Anesth Analg. 2004;99:1648–54. doi: 10.1213/01.ANE.0000136471.36680.97. [DOI] [PubMed] [Google Scholar]