Abstract
Background
The introduction of buprenorphine as office-based treatment for opioid dependence was designed to expand treatment capacity, but virtually there are no data about use of this medication in rural areas.
Methods
The survey of the first cohort of physicians in rural Washington State who obtained buprenorphine waivers (2002-2010) to determine the volume of treated patients, physician appraisal of the efficacy of this treatment, and perceived barriers to treatment was conducted. Twenty-four (73 percent) of the 33 rural buprenorphine-certified physicians practicing in the state were interviewed in 2010.
Results
Twenty physicians (83 percent) were actively prescribing buprenorphine/naloxone for treatment of addiction. Those currently prescribing averaged 23 active patients and had treated 125 patients since certification. All respondents reported that buprenorphine was efficacious in the treatment of addiction and 95 percent recommended that other rural colleagues adopt buprenorphine treatment. The following four major barriers were cited: 1) lack of adequate financial support from Medicaid, the largest source of third-party coverage for these patients; 2) unavailability of local mental health and behavioral addiction treatment services; 3) difficulty in finding consultants to assist in managing complex patients; and 4) shortages of other rural physicians providing this service.
Conclusions
Buprenorphine is viewed as a highly effective treatment of opioid addiction by early adopters in rural Washington State, but relatively few rural physicians currently provide this service. Inadequate insurance coverage, a shortage of effective links with consultants and colleagues, and the lack of mental health services are persistent barriers to the use of this modality in rural Washington State.
Keywords: buprenorphine, opioid dependence, rural physicians
INTRODUCTION
Opioid misuse, abuse, and dependence have become major clinical and public health problems in the United States.1 Although heroin remains a major drug of abuse, the growing number of people addicted to prescription opioids now eclipses the number of people addicted to heroin.2 This pervasive trend is reflected in the rapid increase in the number of unintended lethal overdoses in the United States, most of which can be attributed at least in part to prescription opioids.1
The most effective treatment for opioid addiction is opioid replacement therapy,3 and methadone has been the principal agent for this approach. In the United States, the use of methadone for addiction is highly regulated and restricted to opioid treatment programs that are certified by both the state and federal governments. In Washington State, there are 11 such programs, all of which are in urban areas. As a result, rural patients seeking treatment in a methadone maintenance program must travel almost daily to an urban site, which is often infeasible or prohibitively expensive in terms of travel time and cost.
Recognizing that access to opioid replacement therapy is severely limited, the US government passed the Drug Addiction Treatment Act in 2000 (DATA 2000), which made it possible for trained physicians to prescribe buprenorphine in their normal clinical practices.4 Extensive well-designed studies demonstrate that buprenorphine–usually combined with naloxone to reduce the potential for diversion of the medication–is very effective in treating opioid dependence in the office-based setting.5-7* Physicians are required to receive a waiver from the Substance Abuse and Mental Health Services Administration (SAMSHA) to use this schedule III medication for addiction treatment, and a number of organizations with the assistance of the National Administration on Drug Abuse and SAMSHA have created and disseminated training programs that allow physicians to receive the waiver. The number of physicians prescribing buprenorphine for addiction increased from 2,518 in 2004 to 9,069 in 20088 and has continued to increase since then, although there are still significant access barriers for large segments of the addicted population.
One of the most critical gaps is in the rural United States.9 Methadone is an alternative medication for the treatment of opioid addiction, but access to methadone clinics, addiction specialists, or counselors is extremely limited outside of major cities. Relatively, a few physicians in rural areas have received the federal waiver that allows them to prescribe buprenorphine for addiction; to acquire a waiver, physicians require to take a certified 8-hour course, the content of which is specified by SAMSHA. Very little is known about the experiences of rural physicians with this mode of treatment, how well it has been integrated into their practices, and which barriers prevent rural physicians from using this evidence-based approach.
As we attempt to increase the appropriate use of buprenorphine for the treatment of opioid addiction in rural areas, it would be very helpful to be guided by the experiences of those physicians who have practical experience in these settings. This study attempts to fill this gap in our knowledge by exploring the major issues and characteristics of buprenorphine prescription for opioid addiction through telephone interviews with 24 of the 33 currently practicing physicians in rural Washington who chose to be “early adopters” of this clinical practice.
METHODS
Physician sample
We purchased a list from the National Technical Information Service (www.ntis.gov). This list is provided by the Drug Enforcement Administration DEA of the Department of Justice of all Washington physicians who have received a waiver to prescribe buprenorphine for addiction as of January 2010, which included the last-known practice address and phone number for each physician. Our sample included both those physicians who agreed to have their names listed on the buprenorphine physician locater site maintained by SAMSHA10 and those who were not listed on the physician locator site.
For the purposes of this study, rural was defined as the 22 Washington Counties that were designated as “nonmetropolitan” by the US Office of Management and Budget. These designations are derived from the 2003 Urban Influence Codes created by the US Department of Agriculture.11
Data collection and measures
We developed a semistructured telephone survey to elicit information about the experience and opinions of this sample of physicians regarding their use of buprenorphine to treat patients with opioid addiction. The survey was pilot tested with urban primary care physicians with buprenorphine prescribing experience not in the study sample. The interviews were conducted by the senior author (R. A. R.) and a second-year medical student (T. L. Q.). Interviews were not audio taped, but responses were written at the time of the interview, including capture of verbatim responses to open-ended questions. Physicians were contacted via phone.
We obtained both structured descriptive data about the physicians themselves and the characteristics of their buprenorphine practices, as well as responses to semistructured questions about their motivations for adding this clinical service to their repertoire. We asked about their experiences–both positive and negative–in treating patients addicted to opioids with buprenorphine and what they perceived as barriers to buprenorphine treatment. Institutional review board approval of the study and the survey instrument was obtained from the University of Washington Human Subjects Division.
Analysis
We report descriptive statistics for practice characteristics of general physician. To present the variability in buprenorphine prescribing practices, we divided physician respondents into three groups based on the volume of patients they were currently treating with buprenorphine. For qualitative analyses of physician attitudes and opinions about rural buprenorphine practice, verbatim comments were transcribed and grouped by two authors (T. L. Q. and R. A. R.) into distinct response categories. The process was iterative and differences were resolved by consensus. We report only those comments that reflect the sentiments of three or more physicians.
RESULTS
Survey response
Thirty-eight physicians had obtained the SAMHSA waiver and were listed as practicing in a rural county in Washington State. We recorded the last-known practice address and phone number for each of these physicians. Five physicians were eliminated because they were no longer practicing medicine in Washington State. Of the remaining 33 physicians, we successfully interviewed 24 (73 percent); nine refused to participate because they were unwilling to devote the time required to answer the telephone survey.
Characteristics of physicians who have received a waiver to prescribe buprenorphine for addiction
The characteristics of the respondents are summarized in Table 1. Of the 24 interviewed physicians, 83 percent were board certified in family practice, whereas 17 percent described themselves as specialists: two psychiatrists, one physiatrist, and one family physician certified in addiction medicine. Two-thirds of our sample worked in group practice and one-third were solo practitioners. Most of the physicians worked in entities that receive state or federal support (62 percent), with the other 38 percent in private practices. Two-thirds obtained their waiver after taking an in-person course, with the remainder qualifying through online course. After certification, 75 percent elected to be published on the Buprenorphine Physician and Treatment Program Locator public list maintained by the Center for Substance Abuse Training (CSAT).10
Table 1.
Characteristics of rural physician respondents certified to prescribe buprenorphine in Washington State, 2010
| Characteristics | N = 24 (100) |
|---|---|
| Specialty | |
| Family practice | 20 (83) |
| Psychiatrist | 2 (8) |
| Physiatrist | 1 (4) |
| Addiction medicine | 1 (4) |
| Practice setting | |
| Solo practice | 8 (33) |
| Group | 16 (67) |
| Practice ownership | |
| Private practice | 9 (38) |
| Hospital based | 4 (17) |
| Community health center | 3 (13) |
| Indian health center | 3 (13) |
| Rural health clinic | 2 (8) |
| State facility | 2 (8) |
| Student health | 1 (4) |
| Training used to obtain waiver | |
| In-person course | 16 (67) |
| Online course | 8 (33) |
| Current buprenorphine practice status | |
| Currently prescribing or planning to prescribe | 20 (83) |
| Discontinued prescribing with no plans to restart | 3 (13) |
| Never prescribed and has no plans to start | 1 (4) |
| Year of certification | |
| 2002 | 2 (8) |
| 2003 | 1 (4) |
| 2004 | 0 (0) |
| 2005 | 7 (30) |
| 2006 | 2 (8) |
| 2007 | 3 (12) |
| 2008 | 7 (30) |
| 2009 | 2 (8) |
| CSAT physician locator list status | |
| Chose to be published on public list | 18 (75) |
| Not published on public list | 6 (25) |
Values in parentheses are given in percent.
Of the 24 respondents, 20 (83 percent) were currently actively prescribing buprenorphine or had received a waiver and planned to prescribe buprenorphine in the future. One respondent had obtained the waiver but after training was not interested in prescribing the medication. One physician stopped prescribing buprenorphine because of uncertainty about the efficacy of the medication and two had stopped because of administrative issues specific to their current practice situation.
Patient volume, type of practice, and characteristics of physician
The characteristics of physicians according to the volume of currently treated buprenorphine patients are given in Table 2. The most active third were currently treating a mean of 51.6 patients, representing physicians who have requested to treat more than the first-year limit of 30 patients per physician. The middle group was currently treating a mean of 14.2 patients, a number that the respondents told us could be comfortably accommodated within their current primary care practice. The lowest third were much less active, with an average of two patients currently receiving buprenorphine in their practices.
Table 2.
Mean number of patients currently in treatment by low, medium, and high volume buprenorphine prescribers, and characteristics of respondent associated with differing practice volume (N = 20)
| Low-volume prescribers | Medium-volume prescribers | High-volume prescribers | Total | |
|---|---|---|---|---|
| Physicians | 7 | 6 | 7 | 20 |
| Current number of patients | ||||
| Mean | 2 | 14.2 | 51.6 | 23 |
| Median | 3 | 11.5 | 43 | 11.5 |
| Range | 0-5 | 5-25 | 30-89 | 0-89 |
| Family practice (percent) | 7 (100) | 5 (83) | 6 (86) | 18 (90) |
| Specialty (percent) | 0 (0) | 1 (17) | 1 (14) | 2 (10) |
| On CSAT, percent | 57 | 83 | 86 | 66.6 |
| In group practice, percent | 71 | 50 | 71 | 65 |
| Receive referrals, percent | 43 | 67 | 71 | 60 |
| With consultant, percent | 71 | 67 | 86 | 75 |
| Mean years of certification | 4.3 | 2.8 | 4.6 | 4 |
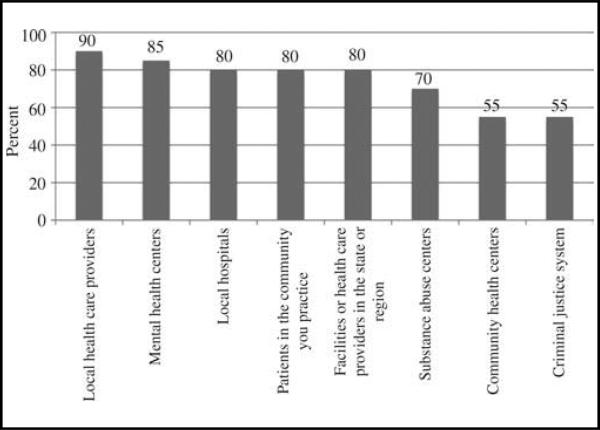
Figure 1 illustrates differences in the extent to which our respondents informed other healthcare organizations in their communities that they were available to treat patients addicted to opioids with buprenorphine. In most cases, the fact that the respondents offered this clinical service was widely disseminated.
Figure 1.
Community groups informed of respondent's buprenorphine practice, in percent (n = 20).
Resources
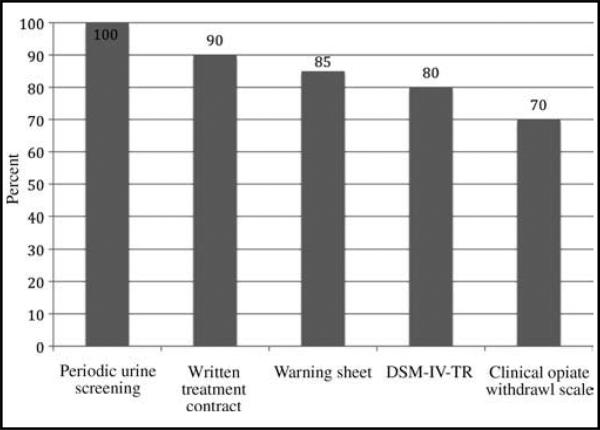
Physicians used a variety of standard tools (Figure 2) in prescribing buprenorphine. Most of the physicians used the major tools that were key elements of the required training for receiving the buprenorphine waiver. All of them used periodic urine screening, and almost all of them used written treatment contracts and distributed warning sheets explaining risks and precautions to their patients.
Figure 2.
Percent of physicians using various tools when prescribing buprenorphine (n = 20). Abbreviation: DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision).
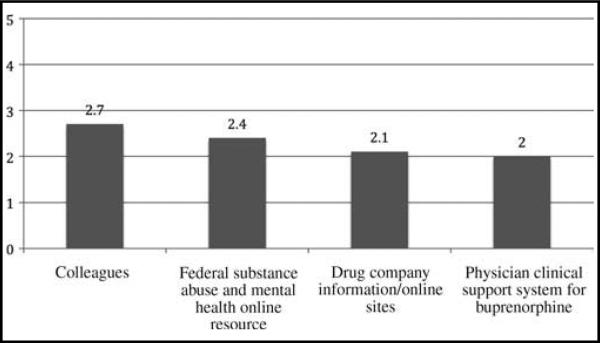
In addition to the clinical and diagnostic tools displayed earlier, our respondents turned to a number of individuals and organizations that were potential sources of support to providers prescribing buprenorphine for addiction, as seen in Figure 3. The most frequently used source was other physician colleagues, followed by SAMSHA's online resources and similar resources made available by the medication's manufacturer. The least frequently used resource of these four options was the physician clinical support system, a network of expert physicians established by SAMSHA.
Figure 3.
Sources of informational support for physicians treating opiate addiction with buprenorphine; 5, used frequently and 0, do not use (n = 20).
Motivations for obtaining buprenorphine waiver and initiating treatment of opioid addiction
There were remarkable similarities in the reasons these rural physicians obtained buprenorphine waivers and began to initiate therapy in their respective communities. Most of our respondents cited the following two specific motivations:
- Newborns addicted to opioids:What really affected me were the babies who were born addicted.A few patients were heroin addicts, but what really affected me was babies born addicted.I was active in OB and had patients who were addicted to opioids, and who were delivering babies that went into withdrawal.
- Opioid addiction was epidemic, disruptive, and lethal in respondents’ communities, and buprenorphine seemed like the best tool to address it in the rural context:From day 1 in rural practice I knew it was needed. The quantities of narcotics are astronomic ... As a new provider, I got hit up.I had a lot of ... pain patients on high doses of narcotics that weren’t effective. I wanted an easy, quick, effective and safe approach to deal with this.... I was working with an Indian tribe. They wanted me to start a methadone program. This wasn’t really an option, so I was very interested in <buprenorphine> certification.
There were 3 people in <my community> who died from opioid overdose. Two of them were the grandchildren of a patient in our clinic who was being treated for cancer. A former patient went to Seattle and died from an overdose of methadone.
Physician acceptance and evaluation of the efficacy of buprenorphine
One hundred percent of the current prescribers reported that they were generally satisfied with the effectiveness of buprenorphine for the treatment of opioid addiction, and 95 percent would recommend the use of buprenorphine to their rural colleagues. A few of the more cogent positive physician responses are quoted verbatim below; virtually all our respondents made comments that were a variant of these quoted.
... it is the best thing (for addiction). No relapses. Patients tell you how great it is and how amazed they are.
It basically works very effectively. I think it is the answer to not having the restrictions of a methadone program and to allow people to get on with their lives.
It's not perfect, but it works well. For some patients it is a miracle. People who have been on opiates for years have been able to get clean. 80-85% of (my) patients have stayed clean.
This restores lives–sometimes literally. I had a patient recovering from endocarditis from heroin use who was basically given a death sentence. For her, the Bup was life saving. I see that over and over again. Plus, these patients are some of my best patients. They always pay their bills, and it is worth it to them.
In addition to their own personal experiences, all but one respondent recommended that other rural colleagues consider using buprenorphine for management of addiction. One physician, while positive about the efficacy of buprenorphine, would only recommend its use to other physicians who were properly trained and devoted to treating addiction.
It's a great extra tool. Opioid dependence is a big deal, and it's just nice to have an extra tool in your belt. Also a great help to the community.
It's another tool in the large toolbox I think family physicians need to have. This problem is so prevalent, and we don’t know about it because secrecy is part of it. The reward is an incredible difference this can make in people.
... it works, and it saves people's lives. There aren’t many things as a family doc you can do to change or save peoples lives.
It should be a part of every physician's formulary without question.
Barriers
Respondents cited the following four major barriers to the use of buprenorphine in rural settings: inadequate fiscal support from Medicaid; a lack of mental health and behavioral addiction treatment resources; a lack of adequate consultant support; and an insufficient number of rural buprenorphine providers.
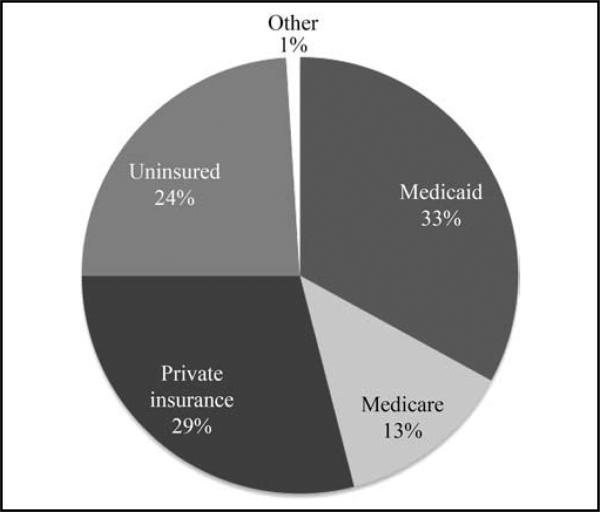
For the respondents in our study, Medicaid is the largest third-party payer for patients on buprenorphine/naloxone (Figure 4). Although patients with Medicare or private insurance in general had coverage of both the physician visits and buprenorphine prescriptions,12 most patients were either uninsured or on Medicaid. At the time of this survey, Medicaid funding for buprenorphine treatment was restricted to patients who were currently enrolled in a state-certified addiction treatment program, and the duration of treatment was limited to 6 months, with a single 6-month extension permitted. Physicians often had difficulty in getting patients who were covered by Medicaid approved for reimbursement for the medication, and even in cases where buprenorphine was covered, it was relatively rare for Medicaid to extend the coverage beyond 6 months and never beyond 12 months.
(We need) changes in the Medicaid approach to Suboxone.
The state needs to gain insight and education on the topic.
Medicaid is the major barrier. Very hard to find outpatient care for this group. Can't sustain them on the appropriate therapy because of Medicaid's policies.
Figure 4.
Third-party payers for patients treated with buprenorphine by study respondents (n = 20).
The other most frequently mentioned barrier was the lack of available mental health and behavioral addiction treatment resources. Although state and federally funded community mental health centers were available in or near many of the rural communities, these organizations receive most of their substance abuse patients through referrals from the criminal justice system. Several respondents noted that local mental health agencies were generally unwilling or reluctant to provide counseling to patients receiving buprenorphine for long-term treatment of addiction. They described these agencies as chronically under funded; they reported that the chemical dependency counselors in these settings primarily used a 12-step abstinence-based approach to the treatment of addiction and were neither familiar nor supportive of medication-assisted treatment.
I need help. I’m walking a very fine line when dealing with drug counseling. I don’t do drug counseling.
I would love a social worker who could coordinate care. Also a psychiatric nurse practitioner.
I wish Chemical Dependency Practitioners could be like physical therapists – you could just refer to them.
I don't consistently hear back from local mental health centers. Often have to contact them many times.
Physicians also referred to lack of access to consultants and an insufficient number of rural buprenorphine providers.
(We need) a better support system and a way to know more people (prescribing buprenorphine) in order to share experiences.
Having someone with experience to work with and share experience with is the best.
To start out, I would have liked to be able to talk to a physician and share resources.
Need more physicians using it.
More local providers would be the best resource for me and I could be a resource to them.
DISCUSSION
Slow diffusion of buprenorphine into rural America
Office-based physicians have adopted the use of buprenorphine as addiction treatment unevenly; previous studies have shown numerous barriers at the patient and physician level.13-15 Our study demonstrates that diffusion of office-based treatment of opioid addiction into rural areas of Washington State has been particularly slow. Only 38 rural physicians were listed as having received a buprenorphine waiver as of 2010, and only 33 of these were actually practicing in the state in 2010. Given the fact that there are 22 rural counties in the state and more than 2,000 rural physicians,16,17 fewer than 2 percent of rural Washington physicians are allowed to use buprenorphine.
Experience of the first cohort of rural Washington State physicians to use buprenorphine for the treatment of opioid addiction
The early adopters of buprenorphine treatment for addiction in rural Washington State were overwhelmingly positive about the efficacy of the treatment in their office-based practices. Of the interviewed 24 physicians–73 percent of those who had received the buprenorphine waiver and were still in practice–20 were still committed to using buprenorphine in their practices. Of the four physicians who were no longer using buprenorphine, only one had discontinued using buprenorphine because of dissatisfaction with the efficacy of the medication.
The comments of the physician respondents reflected not only acceptance but also enthusiasm about the impact of this treatment on their addicted patients. Although some of their responses may have been somewhat unrealistic (eg, “no relapses”), virtually every respondent reported that using buprenorphine was extremely rewarding from a professional standpoint because their patients were able to “get their lives back.” Despite the barriers that rural physicians confronted in prescribing buprenorphine, they virtually all recommended that their rural colleagues add this clinical modality to their repertoire.
Ninety percent of the rural physicians whom we studied were family physicians, demonstrating the extent to which this is a treatment that is likely to be offered predominantly in rural areas by office-based primary care physicians. The volume of treated patients varied widely from physician to physician. For most physicians, the treatment of opioid addiction was a small component of their practice, but one-third of our sample were currently treating more than 30 patients, the volume threshold that requires physicians to notify the DEA that they have been prescribing buprenorphine for over 1 year and that they intend to exceed the original limit of 30 patients under treatment.
It is clear from the surveys that physicians were extensively using the methods and tools covered in the required waiver course whether they received the training at a course or obtained their waiver through online instruction. Twenty percent of the respondents did not allow their names to be published on the CSAT. Some of these physicians restrict their use of buprenorphine to established patients or to those in their communities, whereas others are willing to receive referrals from other physicians. Anecdotally, most of the physicians on the CSAT locator list told us that they received inquiries from patients living in distant urban areas and in some cases from other states.
Barriers to the treatment of opioid addiction in rural areas with buprenorphine
Despite the evidence that rural physicians are extremely satisfied with buprenorphine as an office-based treatment for opioid addiction, they also reported that substantial barriers exist in the use of this modality. Financial barriers are ubiquitous. Suboxone, the buprenorphine formulation that is generally used, is costly. Most of the rural patients treated by our respondents are either uninsured or on Medicaid, and the absence of adequate insurance coverage has a major effect on the ability of the medically indigent to obtain treatment.18
The second most important barrier is the shortage of chemical dependency and mental health programs in rural areas. Rural chemical dependency programs in Washington State provide services in large part for patients referred for mandatory treatment by the courts, and they have little capacity for patients who are voluntarily seeking counseling as an adjunct to opioid replacement therapy. The situation is further complicated by the fact that most chemical dependency programs use variants of the 12-step abstinence-based recovery model and thus are reluctant or unwilling to accept patients who continue to use opioids, even if they are part of an established addiction treatment program. The physicians in our survey have been relatively creative in the ways they have responded to this obstacle, including in one case requiring their buprenorphine patients to start and attend their own Narcotics Anonymous group, but the lack of mental health resources was the most cited obstacle in our survey.
The other major barriers reflect the fact that there are very few rural physicians who provide addiction treatment, and thus our respondents had difficulty in finding colleagues with whom to share the experience or consultants with whom they could confer about complex cases. Resources such as the physician clinical support system supported by SAMSHA were either unknown or under used. The most common sources of consultant support were the instructors whom these physicians had met at the buprenorphine waiver courses they attended.
Study limitations
This study has the following limitations:
This study covers rural areas in only one state, and thus it is difficult to know the extent to which it can be generalized to the rest of the country. Other national studies suggest that similar problems exist in other parts of the country,9 and it is likely that these results are not unique. Washington State is a rapidly growing western state that is predominantly urban, but which also has a large rural population, not unlike many of the states in the country.
The number of respondents is relatively small. Our survey includes data from only 24 subjects of which only 20 were actively involved in the use of buprenorphine to treat opiate addiction. It should be noted that the surveyed 24 physicians represent 73 percent of all the providers with waivers who were practicing in the state at the time of the study, a very high physician response rate for a lengthy phone survey.
The data are derived from physician reports; we did not review charts or interview patients. However, the physicians participated voluntarily, and the interviewers are unaffiliated with any pharmaceutical company and did not have any preconceived expectations about the results.
What does the future hold?
This study builds on a substantial body of evidence that supports the efficacy and acceptability of buprenorphine for office-based treatment of opioid addiction. It extends our knowledge by demonstrating that rural primary care physicians can provide this therapy in the context of both publicly supported and private practices in isolated parts of the state, with only minimal support from mental health agencies or other specialists. It also reflects the extremely favorable experience of those early adopters who initiated this therapy within a decade of the passage of the law legalizing the use of buprenorphine for this indication.
At the same time, this study shows that diffusion of this treatment modality into rural areas has been very slow. Only 33 certificated physicians were in rural practice 10 years after the passage of DATA 2000; a net addition of only four rural physicians per year in Washington falls far short of current and future needs. Further studies are needed to specifically examine how to overcome the barriers that prevent rural physicians from using buprenorphine to treat addiction. Virtually, there is neither information in the literature that addresses the sustainability of addiction treatment in rural primary care settings nor studies that demonstrate successful models of integrating behavioral counseling with primary care provision in these remote locations.
To obtain maximum benefit from this very promising therapeutic approach, we will need to 1) develop programs to train substantially more rural primary care physicians in the use of buprenorphine; 2) provide support and consultation to physicians providing this service; 3) develop ways to complement pharmacological therapy with appropriate mental health services for patients; and 4) improve insurance coverage of outpatient addiction treatment with buprenorphine.
ACKNOWLEDGMENT
This research was supported by a grant from the Life Sciences Discovery Fund to the Program of Excellence in Rural Mental Health and Substance Abuse Treatment.
Footnotes
Hereafter, buprenorphine in the text refers to the combination of buprenorphine/naloxone medication.
Contributor Information
Tyler L. Quest, Department of Family Medicine, University of Washington School of Medicine, Seattle, Washington..
Joseph O. Merrill, Department of Medicine, Division of General Internal Medicine, University of Washington School of Medicine, Seattle, Washington..
John Roll, Program of Excellence in the Addictions, Washington State University School of Nursing, Spokane, Washington..
Andrew J. Saxon, Department of Psychiatry and Behavioral Sciences, Center of Excellence in Substance Abuse Treatment and Education, VA Puget Sound Health Care System, University of Washington School of Medicine, Seattle, Washington..
Roger A. Rosenblatt, Department of Family Medicine, University of Washington School of Medicine, Seattle, Washington..
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Overdose deaths involving prescription opioids among Medicaid enrollees–Washington, 2004-2007. Morb Mortal Wkly Rep. 2009;58:1171–1175. [PubMed] [Google Scholar]
- 2.Okie S. A flood of opioids, a rising tide of deaths. N Engl J Med. 2010;363:1981–1985. doi: 10.1056/NEJMp1011512. [DOI] [PubMed] [Google Scholar]
- 3.Fiellin DA. Buprenorphine: Effective treatment of opioid addic tion starts in the office. Am Fam Physician. 2006;73:1513–1514. [PubMed] [Google Scholar]
- 4.Jaffe JH, O'Keeffe C. From morphine clinics to buprenor phine: Regulating opioid agonist treatment of addiction in the United States. Drug Alcohol Depend. 2003;70:S3–S11. doi: 10.1016/s0376-8716(03)00055-3. [DOI] [PubMed] [Google Scholar]
- 5.Johnson RE, Jaffe JH, Fudala PJ. A controlled trial of buprenorphine treatment for opioid dependence. JAMA. 1992;267:2750–2755. [PubMed] [Google Scholar]
- 6.Fiellin DA, O'Connor PG. Clinical practice. Office-based treat ment of opioid-dependent patients. N Engl J Med. 2002;347:817–823. doi: 10.1056/NEJMcp013579. [DOI] [PubMed] [Google Scholar]
- 7.Fudala PJ, Bridge TP, Herbert S, et al. Office-based treatment of opiate addiction with a sublingual-tablet formulation of buprenorphine and naloxone. N Engl J Med. 2003;349:949–958. doi: 10.1056/NEJMoa022164. [DOI] [PubMed] [Google Scholar]
- 8.Arfken CL, Johanson CE, di Menza S, et al. Expanding treat ment capacity for opioid dependence with office-based treat ment with buprenorphine: National surveys of physicians. J Subst Abuse Treat. 2010;39:96–104. doi: 10.1016/j.jsat.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Lenardson J, Race M, Gale JA. Availability, Characteristics, and Role of Detoxification Services in Rural Areas [working paper #41] University of Southern Maine, Maine Rural Health Research Center; Portland, ME: 2009. [Google Scholar]
- 10. [March 21, 2011];Substance Abuse & Mental Health Services Administration: Buprenorphine Physician and Treatment Program Locator. 2010 Available at http://buprenorphine.samhsa.gov/bwns_locator/.
- 11.Hailu A, VanEenwyk J. Guidelines for Using Rural-Urban Classification Systems for Public Health Assessment. Washington State Department of Health; Olympia, WA: 2009. [March 1, 2010]. Available at http://www.doh.wa.gov/data/guidelines/RuralUrban1.htm. [Google Scholar]
- 12.Kennedy J, Dipzinski A, Roll J, et al. Medicare prescription drug plan coverage of pharmacotherapies for opioid and alco hol dependence in WA. Drug Alcohol Depend. 2011;114(2-3):201–206. doi: 10.1016/j.drugalcdep.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 13.Knudsen HK, Abraham AJ, Johnson JA, et al. Buprenorphine adoption in the National Drug Abuse Treatment Clinical Trials Network. J Subst Abuse Treat. 2009;37:307–312. doi: 10.1016/j.jsat.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meier BR, Patkar AA. Buprenorphine treatment: Factors and first-hand experiences for providers to consider. J Addict Dis. 2007;26:3–14. doi: 10.1300/J069v26n01_02. [DOI] [PubMed] [Google Scholar]
- 15.Thomas CP, Reif S, Haq S, et al. Use of buprenorphine for addiction treatment: perspectives of addiction specialists and general psychiatrists. Psychiatr Serv. 2008;59:909–916. doi: 10.1176/ps.2008.59.8.909. [DOI] [PubMed] [Google Scholar]
- 16.Fordyce MA, Chen FM, Doescher MP. Physician Supply and Distribution in Rural Areas of the United States. WWAMI Rural Health Research Center, University of Washington; Seattle, WA: 2007. p. 2005. [Google Scholar]
- 17.Yen W. Washington State Health Services Research Project. Washington State Office of Financial Management; Olympia, WA: 2010. Washington State's Practicing Physician Workforce– Capacity and Characteristics. Research Brief No. 058. [Google Scholar]
- 18.Ducharme LJ, Abraham AJ. State policy influence on the early diffusion of buprenorphine in community treatment pro grams. Subst Abuse Treat Prev Policy. 2008;3:17. doi: 10.1186/1747-597X-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]