Abstract
Objective: The purpose of this study was to conduct a pilot randomized trial of dialectical behavior therapy (DBT) versus psychosocial treatment as usual (TAU) for adolescents diagnosed with bipolar disorder (BP).
Methods: We recruited participants 12–18 years of age with a primary BP diagnosis (I, II, or operationalized not otherwise specified [NOS] criteria) from a pediatric specialty clinic. Eligible patients were assigned using a 2:1 randomization structure to either DBT (n=14) or psychosocial TAU (n=6). All patients received medication management from a study-affiliated psychiatrist. DBT included 36 sessions (18 individual, 18 family skills training) over 1 year. TAU was an eclectic psychotherapy approach consisting of psychoeducational, supportive, and cognitive behavioral techniques. An independent evaluator, blind to treatment condition, assessed outcomes including affective symptoms, suicidal ideation and behavior, nonsuicidal self-injurious behavior, and emotional dysregulation, quarterly over 1 year.
Results: Adolescents receiving DBT attended significantly more therapy sessions over 1 year than did adolescents receiving TAU, possibly reflecting greater engagement and retention; both treatments were rated as highly acceptable by adolescents and parents. As compared with adolescents receiving TAU, adolescents receiving DBT demonstrated significantly less severe depressive symptoms over follow-up, and were nearly three times more likely to demonstrate improvement in suicidal ideation. Models indicate a large effect size, for more weeks being euthymic, over follow-up among adolescents receiving DBT. Although there were no between-group differences in manic symptoms or emotional dysregulation with treatment, adolescents receiving DBT, but not those receiving TAU, evidenced improvement from pre- to posttreatment in both manic symptoms and emotional dysregulation.
Conclusions: DBT may offer promise as an adjunct to pharmacotherapy in the treatment of depressive symptoms and suicidal ideation for adolescents with BP. The DBT focus on commitment to treatment may be important for the treatment of early-onset BP. Larger controlled trials are needed to establish the efficacy of this approach, examine impact on suicidal behavior, and demonstrate cost effectiveness.
Introduction
Bipolar disorder (BP) in youth is a severe and recurrent illness characterized by prominent and impairing depressive symptoms, poor psychosocial functioning, and substance use (Birmaher and Axelson 2006; Birmaher et al. 2006; Goldstein et al. 2008; Birmaher et al. 2009; Goldstein et al. 2009). Given the hallmark symptoms of abnormal mood, some assert that the core feature of pediatric BP is emotional dysregulation (Leibenluft et al. 2003; Dickstein and Leibenluft 2006). Nonsuicidal self-injury, a behavior commonly linked to emotional dysregulation, is also documented in youth with BP (Esposito et al. 2010). Of particular clinical concern is the associated risk for suicide: Of all psychiatric diagnoses, BP imparts the greatest risk for completed suicide in youth (Brent et al. 1993). Up to 50% of youth with BP attempt suicide (Strober et al. 1995; Bhangoo et al. 2003; Lewinsohn et al. 2003; Goldstein et al. 2005, 2012), and 75% report suicidal thoughts (Lewinsohn et al. 2003; Goldstein et al. 2005).
Guidelines for the treatment of BP in youth identify both pharmacotherapy and psychotherapy as important components of optimal treatment (McClellan et al. 2007). In clinical practice, mood-stabilizing medications serve as the foundation for the treatment of pediatric BP. However, the majority of adolescents with BP experience illness recurrences even with adequate pharmacotherapy (Kowatch et al. 2005), possibly attributable to poor medication adherence in this population (DelBello et al. 2007). Furthermore, recent data also indicate low rates of sustained psychosocial treatment use among youth with BP (Geller et al. 2010; Evans-Lacko et al. 2011). Given that BP substantially disrupts the vast developmental tasks of adolescence (Kowatch et al. 2005) and is associated with poor outcomes into adulthood (Geller et al. 2008), adjunctive psychotherapy for adolescents with BP may have the potential to minimize the long-term debilitating effects of the illness.
Controlled trials support the efficacy of multiple psychotherapy approaches for the treatment of BP in adults (Schottle et al. 2011). However, far less is known about effective psychotherapy for adolescents with BP. In the only controlled trial published to date of a psychosocial intervention for adolescents with BP, Miklowitz and colleagues (2008) compared Family-Focused Therapy for Adolescents (FFT-A; n=53), a 21-session psychoeducational approach, with three sessions of psychoeducation. FFT-A was associated with faster recovery from depression, less time in depressive episodes, and lower depression severity scores over 2 years. Hlastala and Frank (2006) modified Interpersonal and Social Rhythm Therapy (IPSRT) (Frank 2005), a treatment focused on regularizing circadian and social rhythms with demonstrated efficacy in adults, for adolescents with BP. In a small open trial (n=12), they documented improvement in manic and depressive severity from pre- to posttreatment (Hlastala et al. 2010). For school-age children with both unipolar and bipolar mood disorders, Fristad and colleagues demonstrated the efficacy of a multifamily psychoeducational program (MF-PEP) in improving mood symptoms (Fristad et al. 2009), while Pavuluri and colleagues developed a cognitive behavioral intervention for children with mood spectrum disorders (Child and Family-Focused Cognitive-Behavioral Therapy [CFF-CBT]) (Pavuluri et al. 2004; West et al. 2009).
Although these studies are promising, none of these treatments explicitly target suicidality in this high-risk population. Furthermore, youth with BP are commonly systematically excluded from treatment trials targeting adolescent suicidality (King et al. 2006; Stanley et al. 2009). There is, therefore, a void in the treatment armamentarium regarding effective psychotherapeutic approaches for adolescents with BP, and particularly those targeting suicidality.
Dialectical behavior therapy (DBT) (Linehan, 1993) is an evidence-based psychotherapy originally developed for adults with borderline personality disorder. DBT appears to be a face-valid approach for the treatment of adolescents with BP, given the substantial overlap in treatment targets; central DBT treatment foci include emotional dysregulation and its related behaviors, including suicidality and nonsuicidal self-injury. As compared with community treatment, DBT is associated with greater reductions in suicidal behaviors and higher rates of treatment adherence for suicidal adults with borderline personality disorder (Linehan et al. 1994, 2006). A recent pilot study examined a psychoeducational DBT group format for adults with BP, demonstrating significant decreases in depressive symptoms, emergency room visits, and inpatient stays among participants (Van Dijk et al. 2013). Miller and colleagues (2006) incorporated developmentally appropriate modifications to the DBT model for the treatment of suicidal adolescents. Results from several quasi-experimental and pre/post studies support decreases in depressive symptoms and suicidal ideation among teens receiving DBT (for a review, see Klein and Miller 2010).
Our group previously published findings describing an open treatment development study of DBT for adolescents with BP (Goldstein et al. 2007) based on Miller et al.'s DBT with Suicidal Adolescents (2006). Adaptations for adolescents with BP include the addition of a psychoeducation module on pediatric BP, tailoring skills for bipolar mood states, and delivering skills training with family units (Goldstein et al. 2007). Data from this initial open trial (n=10; Goldstein et al. 2007) support the acceptability and feasibility of the treatment model for this population, and demonstrate significant improvement from pre- to posttreatment in suicidal ideation, depressive symptoms, and emotional dysregulation. A second open trial (n=10) enabled us to develop and implement therapist training procedures and incorporate the DBT consultation team. Data from the second open trial similarly indicate significant decreases in suicidal ideation, depressive severity, and emotional dysregulation, and increases in time spent well over 1 year of treatment (Goldstein et al. 2010, 2011).
Based on these promising preliminary findings, we sought to expand our prior work by conducting a small randomized controlled trial of DBT versus psychosocial treatment as usual (TAU; i.e., eclectic psychotherapy primarily consisting of psychoeducational, supportive, and cognitive techniques) as an adjunct to pharmacotherapy at a pediatric bipolar specialty clinic. We aimed to determine the feasibility of conducting a randomized trial in this population and building experience with the DBT model in the context of a clinical trial. We expected greater improvements in targeted domains including depressive symptoms, suicidal ideation and behavior, nonsuicidal self-injurious behavior, and emotional dysregulation among adolescents with BP receiving DBT as compared with those receiving psychosocial TAU.
Methods
Participants
We recruited participants from the Child and Adolescent Bipolar Services (CABS) specialty clinic at Western Psychiatric Institute and Clinic at the University of Pittsburgh Medical Center. Members of the CABS treatment team (psychiatrist, psychiatric nurse and/or therapist) approached potentially eligible participants regarding their interest in participating in the study.
Inclusion criteria
Eligible adolescents met the following criteria: 1) age between 12 years 0 months and 18 years 11 months; 2) an American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) diagnosis of bipolar I, bipolar II, or bipolar not otherwise specified (NOS; see Diagnostic evaluation section) via semistructured interview (American Psychiatric Association 1994); 3) an acute manic, mixed, or depressive episode within 3 months of study entry; 4) willingness to engage in pharmacotherapy with a study-affiliated child psychiatrist; 5) at least one parent or guardian willing to participate in family skills training sessions; 6) no evidence of mental retardation or autism spectrum disorder; and 7) not being engaged in other outpatient psychotherapy.
Procedures
The study was approved by the Institutional Review Board at the University of Pittsburgh. Study staff explained all procedures to interested adolescents and parents. Parents provided written informed consent and adolescents provided assent prior to the initiation of any study procedures.
Diagnostic evaluation
Experienced research staff with master's degrees in a mental health field were trained on site to conduct all diagnostic evaluations. Evaluators assessed for current and past Axis I disorders at intake via direct interview with the parent and adolescent. Non-mood psychiatric disorders were assessed using the Schedule for Affective Disorders and Schizophrenia for School-Aged Children Present and Lifetime Version (K-SADS-PL) (Kaufman et al. 1997), mood symptoms were assessed by the mood disorder sections of the K-SADS-P (Present Episode, 4th revision) (Chambers et al. 1985), plus additional items from the K-SADS Mania Rating Scale (K-SADS-MRS) (Axelson et al. 2003) to provide more detailed data on affective symptoms. A study-affiliated child psychiatrist conducted a clinical interview with the adolescent and parent, and then conferred with the evaluator on the adolescent's final diagnoses. All participants met criteria for DSM-IV BP. We applied operationalized criteria to diagnose BP NOS (Axelson et al. 2006; Birmaher et al. 2006). Inter-rater reliability for presence/absence of Axis I disorders on the KSADS-PL was good (κ≥0.80). The clinical evaluator and attending psychiatrist rated the adolescent's global functioning during the worst lifetime episode as well as over the past 2 weeks using the Children's Global Assessment Scale (Shaffer et al. 1983).
Randomization
Upon confirmation of study eligibility, participants were randomly assigned to study condition by the project manager. Given that this was a feasibility study, we utilized a 2:1 (DBT:standard of care psychotherapy [SOC]) randomization structure in order to gain greater experience delivering the DBT intervention. Participants were informed of their assigned group following completion of the baseline evaluation.
Pharmacotherapy
All study participants received pharmacotherapy with a study-affiliated child psychiatrist. Pharmacotherapy consisted of an initial assessment followed by weekly to biweekly visits for the 1st month of treatment. Assuming adequate treatment response, visits were scheduled monthly thereafter. When patients were actively symptomatic, appointments were scheduled more frequently. Study psychiatrists were not blind to treatment condition, in order to maximize collaboration between treatment providers. Study psychiatrists managed participants' medications according to flexible but standardized best-practice algorithms based on treatment guidelines established by the American Academy of Child and Adolescent Psychiatry for the management of pediatric BP (Kowatch et al. 2005). Study psychiatrists attended weekly treatment team meetings to discuss issues related to management of participants' psychotropic medications.
DBT
Standard DBT, as originally described by Linehan (1993) includes four components: Weekly skills training delivered in a multipatient group format, weekly individual DBT therapy, telephone skills coaching to promote skills generalization, and weekly consultation team for DBT therapists. Patients completed diary cards daily on which they tracked treatment targets and skills use. A treatment hierarchy guided prioritization of session content for both individual and skills training sessions. The manualized intervention we developed for adolescents with BP was based on Miller et al's (2003, 2006) DBT for suicidal adolescents. We developed illness-specific modifications to the treatment for adolescents with BP and their families in the context of our prior treatment development study (Goldstein et al. 2007). In brief, the intervention was delivered in 36 sessions over the course of 12 months. During the acute treatment period (months 1–6), sessions were conducted weekly, and tapered in frequency during the continuation phase (months 7–12). All sessions were 1 hour in duration, and alternated between the two modalities: Individual DBT therapy and family skills training sessions. DBT therapists adhered to the standard DBT treatment hierarchy in individual therapy sessions, and utilized diary cards adapted for this population (Goldstein et al. 2007). Skills training sessions were conducted with the individual family unit. Study therapists provided telephone skills coaching for all study participants per standard DBT protocol.
DBT therapist training and supervision
DBT therapists included master's level staff clinicians and a doctoral-level psychologist with at least 2 years of clinical experience with individuals with psychiatric disturbance (mean years of experience=3.3±5.3). DBT therapist training consisted of a 2 day didactic that began with an overview of pediatric BP. We then introduced the DBT model, with detailed discussion of each component of DBT treatment (individual therapy, skills training, skills coaching, consultation team). Adaptations for adolescents with BP were highlighted, including the addition of the psychoeducation module and the tailored diary cards. All study therapists read the Miller et al. “DBT with Suicidal Adolescents” text (Miller et al. 2006), as well as the study treatment manual prior to treating any study participants. Study therapists videotaped all individual and family skills training sessions. The first author and an intensively trained senior clinical supervisor (M.R.) conducted weekly individual supervision with study therapists; study supervisors reviewed videotaped sessions. Clinical supervisors completed either the Individual or Family Skills Training version of the DBT Therapy Supervisor Rating Scales as appropriate to the session being rated (Fruzzetti 2005 a,b) for 20% of study skills training and individual DBT sessions. The Rating Scale served to help structure the individual supervision.
DBT consultation team
The consultation team met weekly for 90 minutes throughout the course of the study. The first 60 minutes of the consultation team meeting adhered to the standard consultation team format (Linehan 1993; Miller et al. 2006); the last 30 minutes was reserved for didactics related to DBT, pediatric BP, and the assessment and treatment of suicidality, as a means of enhancing therapists' knowledge and skills.
SOC psychotherapy
Participants randomized to CABS SOC received psychotherapy with a study-affiliated CABS therapist. CABS therapists included master's level clinicians with experience treating youth with BP. CABS SOC therapists did not have any training in DBT. On average, SOC therapists had significantly more years of experience treating youth with BP and their families than did DBT therapists (mean years of experience for SOC therapists=10.5±0.7; for DBT therapists=3.3±5.3; t=3.2, p=0.02).
The CABS SOC psychotherapy approach is eclectic. Individual and family therapy sessions are scheduled as clinically indicated. CABS SOC therapists draw from supportive, psychoeducational, and family systems models. CABS SOC therapists attended a weekly treatment team meeting during which they discussed their therapy cases. Although little is known about the specific types of psychotherapy received by youth with BP in the community (Geller et al. 2010), our clinical experience indicates that eclectic and supportive approaches are common. Therefore, CABS SOC is likely similar to services that youth with BP may obtain in the community, but may be more rigorous, given CABS therapists' level of experience and supervision received in the context of the specialty clinic. We did not systematically evaluate the content of CABS SOC sessions in this pilot study.
Outcome measures
Participants and their parents completed assessments quarterly throughout the 1 year study (i.e., at 3, 6, 9, and 12 months) with an independent master's level evaluator blind to treatment group. Outcomes included mood symptoms, suicidal ideation and behavior, nonsuicidal self-injurious behavior, and emotional dysregulation.
Mood symptoms
The study evaluator administered the semistructured KSADS Depression Rating Scale (DRS) and MRS at each follow-up assessment to adolescents and parents separately. Summary ratings incorporated all available information, and reflected the worst week in the month preceding the evaluation. Inter-rater reliability between the first author and the study evaluator for K-SADS mood items was good (DRS intraclass correlation coefficient [ICC]=0.84; MRS ICC=0.96). Additionally, we monitored the course of affective symptoms over follow-up using the Adolescent Longitudinal Follow-Up Evaluation (ALIFE) semistructured interview (Keller et al. 1987). The ALIFE methodology calls for the evaluator to gather weekly information over the period being rated (i.e., the preceding 12 weeks). For follow-up assessments, the evaluator first orients the adolescent and parent to any symptoms that were present during the prior rating period, and then methodically probes for “change points” in symptoms since that time. Evaluators use major events in time to help adolescents and parents with recall (e.g., birthdays, holidays). Once the evaluator has ascertained that a period(s) of depression and/or mania/hypomania symptoms was present, each week is then assigned a Psychiatric Status Rating (PSR) on a 1–6 symptom severity scale based on DSM-IV criteria for depression, hypomania, and mania, as follows: 1=no symptoms, 2–4=subthreshold symptoms, 5–6=full threshold DSM-IV criteria). This methodology has been shown to have excellent reliability and validity for examining the course of illness in adults (Keller et al. 1987; Warshaw et al. 1994, 2001) and youth (Lewinsohn et al. 2000; Birmaher et al. 2009) with anxiety and affective disorders. For the present analyses, we operationalized ALIFE PSR data as follows: Depression-free weeks were those for which ALIFE depression PSR≤2; hypo/mania-free weeks were those for which ALIFE hypomania and mania PSR≤2; and weeks being euthymic were those for which both ALIFE depression and hypo/mania PSR≤2. Inter-rater reliability (ICC) between the first author and the study evaluator for ALIFE PSR ratings of depressive episodes and manic/hypomanic episodes were ≥0.80.
Suicidal ideation
Adolescents completed the self-report Suicidal Ideation Questionnaire-Junior (SIQ-Jr) (Reynolds 1987), a measure of the severity of suicidal thoughts. The scale asks youth to indicate the frequency of 15 items on a seven point scale from “almost every day” to “never.”
Suicidal and nonsuicidal self-injurious behavior
We utilized the Longitudinal Interval Follow-Up Evaluation (LIFE) Self-Injurious/Suicidal Behavior Scale (Goldstein et al. 2012) to assess suicidal and nonsuicidal self-injurious behavior. Clinicians recorded all self-injurious behaviors that occurred during the follow-up period, regardless of intent. Ratings of intent to die and medical threat were assigned for each behavior using the K-SADS-P Depression Scale ratings for these items (Chambers et al. 1985) on a 1 (none) to 6 (extreme, careful planning and every expectation of death) scale, and lethality on a 1 (no danger) to 7 (death) scale. In keeping with our prior work (Goldstein et al. 2005,2012), any behavior that included definite intent (intent score of 3, definite but ambivalent, or greater) and/or mild lethality (medical threat score of 3, mild, or greater) was considered a suicide attempt. Behaviors devoid of intent and/or lethality were classified as nonsuicidal self-injurious behaviors.
Emotional dysregulation
Parents and adolescents completed the Children's Affective Lability Scale (CALS) (Gerson et al. 1996), a 20 item measure of behavior reflective of emotional dysregulation.
Treatment satisfaction
Adolescents and parents completed a 12 item Treatment Satisfaction Questionnaire upon completing the year-long treatment study.
Data analysis
We first conducted t, χ2, Wilcoxon two sample Z approximations, and Fisher exact tests as appropriate to examine for baseline group differences in demographic and clinical variables. Given that the DBT group exhibited higher severity scores at intake on several outcome domains (see Study sample section), statistical models accounted for these baseline differences. Specifically, we first constructed linear mixed models to examine the treatment effect on each outcome variable, controlling for baseline score. Models were first examined including the interaction between group and time. Interaction terms that were evidenced to improve model fit were maintained in the model. Effect size estimates for models examining between-group effects were determined using Cohen's d (where d≥0.2 is considered a small effect size, d≥0.5 is a medium effect size, and d≥0.8 is a large effect size) (Cohen 1977). We also constructed mixed models to examine for the within-group effect of time on the outcome variable. Effect size estimates for models examining within-group effects were determined using partial η2 (where partial η2≥0.01 is considered a small effect size, partial η2≥0.06 is a medium effect size, and partial η2≥0.14 is large effect size) (Richardson 2011). For models examining weekly ALIFE PSR data, we utilized negative binomial models to account for overdispersion of count data; models accounted for total weeks of follow-up. Effect size estimates for negative binomial models were determined using rate ratios. All analyses were conducted using the intent-to-treat sample; p values are based on two tailed tests with α=0.05.
Results
Study sample
Adolescents randomly assigned to receive DBT (n=14) and TAU (n=6) did not differ on baseline demographic characteristics including age, sex, socioeconomic status (Hollingshead 1975), or race (Table 1). Overall, the sample included relatively ill youth who had early illness onset, psychiatric hospitalizations, and poor functioning. The groups evidenced similar clinical characteristics including BP subtypes, rates of comorbid psychiatric disorders, and number of medications prescribed at intake. However, on average, adolescents randomized to DBT had more severe ratings of manic symptoms on the MRS and parent-rated emotional dysregulation on the CALS at baseline, as well as fewer mean weeks depression-free in the 3 months preceding study intake. There was also a nonsignificant statistical trend whereby adolescents randomized to receive DBT had more past suicide attempts.
Table 1.
Demographics and Baseline Clinical Characteristics
| DBT (n=14) | TAU (n=6) | Stat | p value | |
|---|---|---|---|---|
| Age | 15.82 (2.1) | 16.83 (1.4) | Z=0.83 | 0.4 |
| Sex (female) | 11 (79%) | 4 (67%) | Fisher's exact | 0.6 |
| Race | ||||
| Caucasian | 13 (93%) | 3 (50%) | Fisher's exact | 0.06 |
| African American | 1 (7%) | 1 (17%) | ||
| Multiracial | 0 | 2 (33%) | ||
| SESa | 33.36 (15.7) | 41.17 (18.5) | Z=0.91 | 0.4 |
| Bipolar type | ||||
| BPI | 3 (21%) | 0 | Fisher's exact | 0.7 |
| BPII | 5 (36%) | 3 (50%) | ||
| BPNOS | 6 (43%) | 3 (50%) | ||
| Age at illness onset | 13.03 (3.6) | 11.40 (3.8) | Z=1.08 | 0.3 |
| Comorbid conditionsb | ||||
| ADHD | 4 (29%) | 2 (33%) | Fisher's exact | ∼1 |
| GAD | 4 (29%) | 1 (17%) | ∼1 | |
| Social phobia | 1 (7%) | 0 (0%) | ∼1 | |
| Panic disorder | 1 (7%) | 0 (0%) | ∼1 | |
| PTSD | 1 (7%) | 0 (0%) | ∼1 | |
| Other anxiety | 2 (14%) | 1 (17%) | ∼1 | |
| Substance abuse | 0 (0%) | 1 (17%) | 0.3 | |
| ODD | 0 (0%) | 2 (33%) | 0.08 | |
| Number of psychotropic medications prescribed | 1.93 (1.2) | 1.67 (1.5) | Z=0.56 | 0.6 |
| CALS-Cc | 40.17 (19.1) | 31.00 (18.0) | Z=1.03 | 0.3 |
| CALS-Pd | 41.79 (15.8) | 21.00 (14.3) | Z=2.02 | 0.04 |
| K-SADS DRSe | 25.71 (7.1) | 19.17 (9.6) | Z=1.53 | 0.1 |
| K-SADS MRSf | 27.14 (8.5) | 14.50 (6.7) | Z=2.73 | 0.006 |
| ALIFE PSR weeks euthymicg | 0.93 (1.6) | 3.17 (4.3) | Z=0.98 | 0.3 |
| ALIFE PSR weeks depression-free | 1.36 (2.1) | 5.33 (4.3) | Z=2.16 | 0.03 |
| ALIFE PSR weeks hypo/mania-free | 5.79 (4.3) | 8.00 (4.6) | Z=1.22 | 0.2 |
| SIQ-Jrh | 19.17 (21.0) | 15.50 (29.7) | Z=0.80 | 0.4 |
| C-GASi | ||||
| most severe past | 42.64 (5.4) | 45.17 (2.9) | Z=1.03 | 0.3 |
| past 2 weeks | 50.07 (5.4) | 51.83 (2.5) | Z=0.89 | 0.4 |
| Nonsuicidal self-injurious behaviorj | 5 (36%) | 1 (17%) | Fisher's exact | 0.6 |
| Number of past hospitalizations | 1.64 (3.0; Range 0–11) | 0.33 (0.5; Range=0–1) | Z=0.96 | 0.3 |
| Number of past suicide attempts | 1.00 (1.8; Range 0–5) | 0 | Z=1.79 | 0.07 |
Socioeconomic status, Hollingshead-Redlich Criteria (1965).
Diagnosed via Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children, Present and Lifetime version (KSADS-PL) semistructured interview.
Children's Affective Lability Scale, Child Self-Report (CALS-C).
Children's Affective Lability Scale, Parent-Report.
K-SADS Depression Rating Scale.
K-SADS Mania Rating Scale.
Adolescent Longitudinal Follow-Up Evaluation Psychiatric Status Ratings (3 months preceding study intake).
Suicidal Ideation Questionnaire, Jr version.
Children's Global Assessment Scale.
over the past 3 months, assessed via the LIFE Self-Injurious/Suicidal Behavior Scale.
ADHD=Attention Deficit Hyperactivity Disorder; GAD=Generalized Anxiety Disorder; PTSD=Post-Traumatic Stress Disorder; ODD=Oppositional Defiant Disorder.
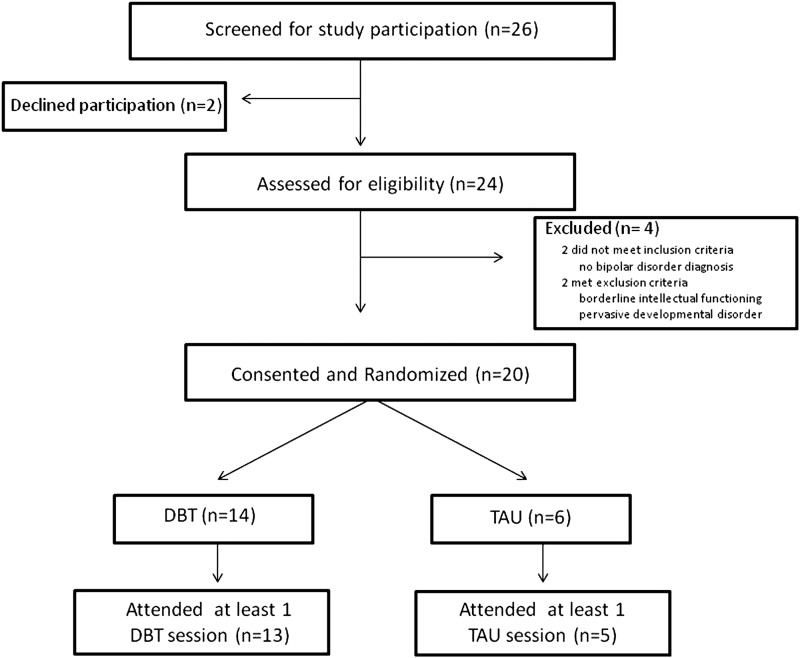
Feasibility
As can be seen in Figure 1, to yield the study sample of 20 adolescents, we screened 26 interested families. The two families who declined participation prior to determining eligibility cited concerns regarding ability to attend weekly sessions. Of the 24 adolescents assessed for eligibility, 2 failed to meet study inclusion criteria (no primary BP diagnosis), and 2 met study exclusion criteria (1 pervasive developmental disorder, 1 borderline intellectual functioning). Of the 20 subjects who were randomized, 2 withdrew prior to attending any study therapy sessions (1 DBT required a higher level of care; 1 TAU refused further participation).
FIG. 1.
Study Consort Diagram.
On average, adolescents randomized to receive DBT attended 12.9±8.2 DBT skill sessions and 17.4±10.4 DBT individual sessions over an average of 39 weeks, for a mean total number of 30.3±17.7 DBT therapy sessions over the year-long study period. Adolescents randomized to receive TAU attended, on average, 8.6±8.5 total therapy sessions over the year-long study. Subjects in the DBT condition attended significantly more total therapy sessions than TAU subjects (t=3.5, p<0.01).
Patient satisfaction
Adolescents and their parents reported high levels of satisfaction with DBT (scale=1 [very dissatisfied] to 7 [very satisfied]; mean adolescent rating=6.6±0.8; mean parent rating=6.4±0.5), as well as with the adolescent's progress at posttreatment (mean adolescent rating=6.3±1.0; mean parent rating=6.0±0.6). Mean satisfaction with TAU (adolescent=4.5±3.5; parent=5.0±0) and satisfaction with the adolescent's progress in TAU (adolescent=6.3±1.0; parent=5.5±0.7) were not different from those reported in DBT (for all, p>0.1).
On average, adolescents and parents rated the length of treatment in both DBT and TAU as appropriate (scale=1 [much too short] to 7 [much too long]; adolescent DBT=3.4±0.8, adolescent TAU=3.0+1.4; parent DBT=3.7±0.8, parent TAU=4.0±0.0). Both adolescents and parents felt that the frequency of visits in both treatments was appropriate (adolescent DBT=4.0±0, adolescent TAU=4.0+1.4; parent DBT=4.0±0, parent TAU=4.0±0.0).
Treatment response
Mood symptoms
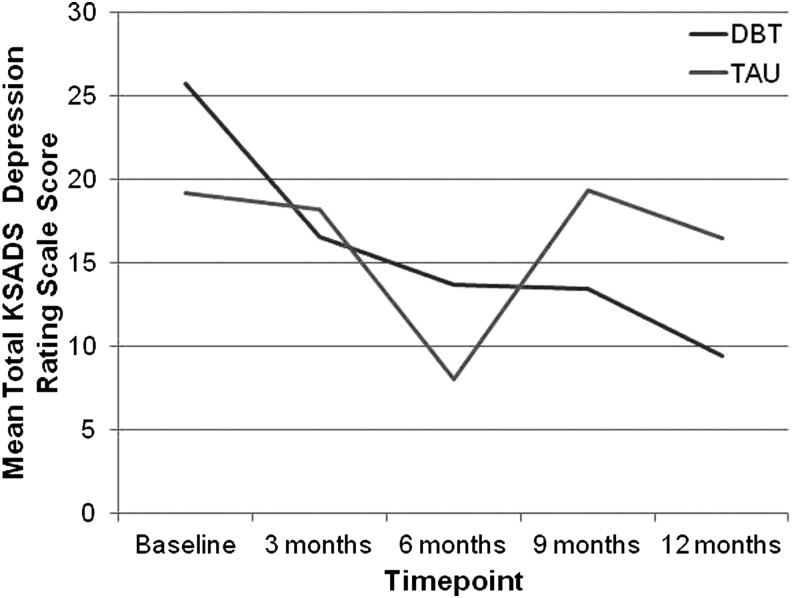
As compared with adolescents receiving TAU, adolescents receiving DBT evidenced less severe depressive symptoms on the DRS over follow-up (F=4.02, p=0.05; d=0.98). Within-group mixed models indicated a significant effect of time on DRS score among adolescents receiving DBT (F=8.99, p<0.0001; partial η2=0.47) but not TAU (F=0.52, p=0.72; partial η2=0.12; Fig. 2).
FIG. 2.
Improvement in depressive symptom severity over one year among adolescents receiving Dialectical Behavior Therapy (DBT) versus psychosocial treatment as usual (TAU)
The between-group mixed model does not support a significant difference between groups in severity of manic symptoms on the MRS over follow-up (F=0.19, p=0.67; d=0.21). Within-group mixed models indicate a significant effect of time on MRS score among adolescents receiving DBT (F=7.10, p=0.0003; partial η2=0.39) but not TAU (F=0.25, p=0.90; partial η2=0.11).
There was not a significant difference between groups in mean rate of weeks depression-free (x2=0.81, p>0.10; rate ratio=1.6) or hypo/mania-free (x2=0.96, p>0.10; rate ratio=1.4) on the ALIFE PSR over follow-up. However, the estimated mean rate of depression-free weeks over follow-up was 1.6 times greater, and the estimated mean rate of hypo/mania-free weeks was 1.4 times greater among adolescents receiving DBT than among adolescents receiving TAU, corresponding with a moderate effect size. Similarly, there was not a significant difference between groups in mean rate of euthymic weeks over follow-up (x2=1.89, p>0.10; rate ratio=2.2). However, the model indicates that the estimated mean rate of euthymic weeks is 2.2 times greater for adolescents receiving DBT rather than TAU, corresponding with a large effect size.
Suicidal ideation
The SIQ data were non-normally distributed, whereby five subjects (two TAU, three DBT) denied suicidal ideation (i.e., SIQ total score=0) at study intake. At 12 month follow-up, 83% of the DBT group and 50% of the TAU group showed a decrease in SIQ score (reflecting improvement in suicidal ideation), 17% of the DBT group and 0% of the TAU group showed no change in SIQ score, and 0% of the DBT group and 50% of the TAU group showed an increase in SIQ score (i.e., worsening of suicidal ideation). Using ordered logistic regression, there was a statistical trend for adolescents receiving DBT to be more likely to demonstrate improvement in suicidal ideation on the SIQ (F=3.39, p=0.07; OR=2.9).
Nonsuicidal self-injurious behavior
At study intake, five subjects in the DBT group and one subject in the TAU group reported engaging in nonsuicidal self-injurious behavior during the 3 months preceding study entry (see Table 1). At 12 month follow-up, no DBT subjects had engaged in nonsuicidal self-injury in the preceding 3 months, whereas 1 TAU subject had engaged in nonsuicidal self-injury during that period. The small numbers of behaviors preclude statistical analysis.
Suicide attempts
At study intake, the DBT group displayed a significantly greater lifetime history of suicidal behavior than the TAU group (see Table 1); at intake, none of the TAU group had a history of suicidal behavior. Over follow-up, there were no suicide attempts in the TAU group, and two attempts by two different subjects in the DBT group (3 month follow-up and 9 month follow-up). The small numbers of behaviors preclude statistical analysis.
Emotional dysregulation
The DBT and TAU groups did not differ in terms of improvement on the CALSC (F=0.01, p>0.1; d=0.07) or CALSP (F=0.02, p>0.1; d=0.06) with treatment. However, within-group mixed effects models indicated that both CALSC (F=4.22, p=0.008; partial η2=0.32) and CALSP (F=3.71, p=0.01; partial η2=0.26) scores significantly decreased over time among adolescents receiving DBT, whereas this was not the case for adolescents receiving TAU (CALSC [F=1.1, p=0.44; partial η2=0.46]; CALSP [F=2.62, p=0.19; partial η2=0.74]).
Discussion
Results from this small randomized trial of DBT for adolescents with BP provide further preliminary support for the DBT treatment model in the psychosocial treatment of this population. Findings suggest that randomization to psychosocial treatment in the context of a specialty clinic is acceptable to adolescents with BP and their families. Outcome data indicate that compared with psychosocial TAU, DBT is associated with greater rates of treatment adherence, and less severe depressive symptoms; although not statistically significant, models estimate large effect sizes for adolescents receiving DBT to spend over twice as many weeks being euthymic over follow-up than adolescents receiving TAU, and to be nearly three times more likely to demonstrate improvement in suicidal ideation. Adolescents receiving DBT also exhibited significant improvement in manic symptoms and emotional dysregulation over time.
Before we discuss the specific findings, it is important to highlight the limitations of this feasibility study. Primarily, the small sample size and purposely unequal randomization structure (2 DBT:1 TAU) yielded limited statistical power to detect significant changes between groups in outcome domains over time. Such analyses necessitate future conducting of controlled studies with larger samples. Additionally, randomization did not result in an even distribution of certain clinical characteristics between groups, such that adolescents randomly assigned to receive DBT were, on average, significantly more symptomatic at study intake (i.e., more severe mania, emotion dysregulation, and lifetime suicidal behavior) than adolescents assigned to TAU. It is, therefore, possible that improvement among adolescents receiving DBT may be attributable to regression to the mean. Medium to large effect sizes for improvement in depression, mania, and suicidal ideation with DBT suggest meaningful changes that should be further explored. Stratified randomization should be considered in future studies to evenly distribute key clinical variables. Additionally, adolescents and parents were not blind to treatment assignment. Therefore, treatment expectancy may have differentially impacted outcomes between groups. Such effects may have been minimized by outcome ratings from the independent study evaluator, who was blind to treatment group.
Our primary goal was to demonstrate feasibility of conducting a small randomized trial of psychosocial intervention in this population. Our recruitment efforts indicate that the majority of families approached about participation were interested, and accepted randomization to psychosocial intervention. This experience bodes well for future studies aiming to establish the efficacy of psychosocial interventions for these difficult-to-treat populations.
Despite findings that adolescents randomly assigned to DBT attended significantly more therapy sessions during the year-long study than did adolescents assigned to TAU (mean DBT sessions=30; mean TAU sessions=9), adolescents and parents from both groups rated the frequency of visits and length of treatment program as appropriate. Given that adolescents in DBT were, on average, more symptomatic than adolescents in TAU at study intake, a more intensive treatment schedule may have been deemed more acceptable to these youth and families. Baseline illness severity may, therefore, be examined as an important predictor of engagement in DBT. It is also possible that socialization regarding expectations of session frequency shapes satisfaction with any psychosocial intervention. Alternatively, in a less prescribed treatment model such as TAU, family preference may directly inform session frequency, thereby impacting satisfaction. It is tempting to conclude that because youth randomized to TAU were less symptomatic at study intake, TAU therapists determined that less frequent sessions were clinically indicated. However, the frequency of sessions attended by adolescents in TAU did not increase over time as clinical acuity increased. The frequency of TAU sessions decreased over the course of the 1 year study. It therefore seems that the DBT treatment model was more successful at engaging adolescents and their families in treatment and promoting therapy adherence. Both commitment to treatment and treatment-interfering behaviors are expressly targeted in DBT (Linehan 1993; Miller et al. 2010). Prior studies indicate lower rates of treatment dropout among adults (Linehan et al. 2006) and adolescents (Rathus and Miller 2002) receiving outpatient DBT than with among those receiving community outpatient treatment. Given recent data indicating low rates of sustained psychosocial treatment use among youth with BP (Geller et al. 2010; Evans-Lacko et al. 2011), the potential of DBT to engage and retain adolescents with BP and their families appears promising.
Recent naturalistic data indicate that youth with BP spend 60% of their time symptomatic over longitudinal follow-up, with a greater predominance of depressive than manic symptoms (Birmaher et al. 2009). In the current study, the estimated average rate of euthymic weeks over follow-up among adolescents receiving DBT was over twice that of those receiving TAU. Furthermore, adolescents receiving DBT evidenced less severe depressive symptoms over follow-up, and displayed significant improvement in manic symptoms with treatment, whereas adolescents receiving TAU did not. Fristad et al. similarly documented improvement in mood symptom severity on a composite scale of depression and mania among school-age mood-disordered youth with a 12 week MF-PEP (Fristad et al. 2009). Among adolescents with BP, Miklowitz and colleagues demonstrated improvement in depression, but not mania, symptoms with FFT-A (Miklowitz et al. 2008). Hlastala and colleagues documented improvement in both depression and mania symptoms among adolescents with BP in an open trial of IPSRT (Hlastala et al. 2010).
Annual healthcare service use and expenditures for adolescents with BP exceed those for adolescents with all other mood and non-mood psychiatric disorders (Peele et al. 2004), primarily driven by high use of inpatient and emergency services for suicidal behavior (Peele et al. 2004; Rizzo et al. 2007; Stensland et al. 2010). As such, outpatient treatment for youth with BP that effectively targets suicidality may not only enhance quality of life, but also result in significant healthcare cost savings. Adolescents receiving DBT showed a nearly threefold reduction in clinically significant suicidal ideation, which in our small sample was a statistical trend. Statistical power was limited to examine differential rates of suicidal behavior over follow-up in our study with treatment. An adequately powered trial will be able to determine whether DBT is associated with reduction in suicidal behavior, as has been demonstrated among adults with borderline personality disorder (Linehan et al. 2006). Furthermore, given the relative intensity of comprehensive outpatient DBT, administrators cite fiscal concerns as a barrier to implementation (Herschell et al. 2009). Demonstrating that the expense is justified by superior and sustained long-term patient outcomes and associated with lifelong reductions in costly service utilization will be important for ultimate dissemination (Hlatky et al. 2006).
Some argue that emotional dysregulation represents the core feature of early-onset BP (Dickstein and Leibenluft 2006), rendering this a potentially beneficial treatment focus for this population. Not surprisingly, deficits in emotion regulation are also linked to adolescent suicidality (Esposito et al. 2003; Tamas et al. 2007) and nonsuicidal self-injury (Nock and Prinstein 2005). However, few intervention studies explicitly target, and subsequently assess, changes in emotion regulation and nonsuicidal self-injurious behavior with treatment among youth with BP. We did not find significant differences in emotional dysregulation between adolescents receiving DBT and those receiving TAU. However, adolescents receiving DBT did exhibit significant improvement from pre- to posttreatment in emotional dsyregulation per self- and parent-report, whereas adolescents receiving TAU did not. With respect to nonsuicidal self-injurious behavior, of the five adolescents receiving DBT who exhibited nonsuicidal self-injurious behavior in the 3 months preceding study intake, all denied nonsuicidal self-injurious behavior at posttreatment. Given the centrality of emotional dysregulation to pediatric BP and its association with suicidal behavior, nonsuicidal self-injury, and functioning, multimethod assessment of emotional dysregulation may be considered.
Conclusions
Our experience conducting this feasibility study indicates that randomization to psychosocial intervention is acceptable to adolescents with BP and their families. Both DBT and TAU psychotherapy were viewed positively by participants. Data suggest DBT is associated with greater treatment engagement and less severe depressive symptoms over follow-up than psychosocial TAU.
Clinical Significance
Clinicians treating adolescents with BP, and particularly those who exhibit low commitment to treatment, suicidality, nonsuicidal self-injury, or emotional dysregulation, may consider DBT as a promising adjunct to pharmacotherapy.
Acknowledgments
The authors thank study therapists Anne Conway, Maria Garcia, Nina Hotkowski, Emily Kane, Tiffany Painter, Barbara Pane, and Gloria Pollard, and the faculty and staff of the CABS clinic.
Disclosures
Dr. Goldstein has received research support from Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), The Fine Foundation, National Institute on Drug Abuse (NIDA), NIMH, The Pittsburgh Foundation, and The Ryan Licht Sang Foundation, and royalties from Guilford Press. Dr. Axelson has received research support from NIMH. Dr. Brent currently employed by the University of Pittsburgh, School of Medicine and the University of Pittsburgh Medical Center, Western Psychiatric Institute and Clinic; has received research support from NIMH; receives royalties from Guilford Press; has or will receive royalties from the electronic self-rated version of the Columbia Suicide Severity Rating Scale (C-SSRS) from eResearchTechnology (ERT), Inc.; and serves as an UpToDate psychiatry editor. Dr. Birmaher has received research support from The Fine Foundation and NIMH, and receives royalties from Lippincott Williams & Wilkins and Random House, Inc. The remaining authors have no disclosures to report.
References
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- Axelson DA, Birmaher B, Brent D, Wassick S, Hoover C, Bridge J, Ryan N: A preliminary study of the Kiddie Schedule for Affective Disorders and Schizophrenia for School-age Children Mania Rating Scale for children and adolescents. J Child Adolesc Psychopharmacol 13:463–470, 2003 [DOI] [PubMed] [Google Scholar]
- Axelson DA, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan ND, Leonard H, Junt J, Iyengar S, Bridge J, Keller M: Phenomenology of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry 63:1139–1148, 2006 [DOI] [PubMed] [Google Scholar]
- Bhangoo RK, Dell ML, Towbin KE, Myers F, Lowe C, Pine D, Leibenluft E: Clinical correlates of episodicity in juvenile mania. J Child Adolesc Psychopharmacol 13:507–514, 2003 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D: Course and outcome of bipolar spectrum disorder in children and adolescents: A review of the existing literature. Dev Psychopathol 18:1023–1035, 2006 [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Strober M, Gill MK, Valeri S, Chiappetta L, Ryan ND, Leonard H, Hunt J, Iyengar S, Keller M: Clinical course of children and adolescents with bipolar spectrum disorders. Arch Gen Psychiatry 63:175–183, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson DA, Goldstein BI, Strober M, Gill MK, Hunt J, Houck M, Ha W, Iyengar S, Kim E, Yen S, Hower H, Smythers C, Goldstein T, Ryan N, Keller M: Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: The Course and Outcome of Bipolar Youth (COBY) study. Am J Psychiatry 166:795–804, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Roth C, Schweers J, Balach L, Baugher M: Psychiatric risk factors for adolescent suicide: A case-control study. J Am Acad Child Psychiatry 32:521–529, 1993 [DOI] [PubMed] [Google Scholar]
- Chambers WJ, Puig–Antich J, Hirsch M, Paez P, Tabrizi N, Johnson R: The schedule for affective disorders and schizophrenia for school age children. Arch Gen Psychiatry 42:696–702, 1985 [DOI] [PubMed] [Google Scholar]
- Cohen J: Statistical Power Analysis for the Behavioral Sciences, Vol. 1 New York: Academic Press, Inc.; 1977 [Google Scholar]
- DelBello MP, Hanseman D, Adler C, Fleck D, Strakowski S: Twelve month outcome of adolescents with bipolar disorder following first-hospitalization for a manic or mixed episode. Am J Psychiatry 164:582–590, 2007 [DOI] [PubMed] [Google Scholar]
- Dickstein DP, Leibenluft E: Emotion regulation in children and adolescents: Boundaries between normalcy and bipolar disorder. Dev Psychopathol 18:1105–1131, 2006 [DOI] [PubMed] [Google Scholar]
- Esposito C, Goldstein TR, Birmaher B, Goldstein B, Hunt J, Ryan N, Axelson D, Strober M, Gill M, Hanley A, Keller M: Clinical and psychosocial correlates of non-suicidal self-injury within a sample of children and adolescents with bipolar disorder. J Affect Disord 125:89–97, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito C, Spirito A, Boergers J, Donaldson D: Affective, behavioral, and cognitive functioning in adolescents with multiple suicide attempts. Suicide Life Threat Behav 33:389–399, 2003 [DOI] [PubMed] [Google Scholar]
- Evans–Lacko S, dosReis S, Kastelic E, Riley A: Mental health service use before and after diagnosis of early-onset bipolar disorder. J Behav Health Serv Res 38:398–413, 2011 [DOI] [PubMed] [Google Scholar]
- Frank E: Treating Bipolar Disorder: A Clinician's Guide to Interpersonal and Social Rhythm Therapy. New York: Guilford Press, 2005 [Google Scholar]
- Fristad MA, Verducci J, Walters K, Young M: Impact of multifamily psychoeducational psychotherapy in treating children aged 8 to 12 years with mood disorders. Arch Gen Psychiatry 66:1013–1021, 2009 [DOI] [PubMed] [Google Scholar]
- Fruzzetti AE: DBT individual therapy supervisor rating scale: Unpublished scale, University of Nevada, Reno, 2005a [Google Scholar]
- Fruzzetti AE: DBT skills training supervisor rating scale: Unpublished scale, University of Nevada, Reno, 2005b [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B: Child bipolar I disorder: Prospective continuity with adult bipolar I disorder; characteristics of second and third episodes; predictors of 8-year outcome. Arch Gen Psychiatry 65:1125–1133, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B: Pharmacological and non-drug treatment of child bipolar I disorder during prospective eight-year follow-up. Bipolar Disord 12:164–171, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerson AC, Gerring JP, Freund L, Joshi P: The children's affective lability scale: A psychometric evaluation of reliability. Psychiatry Res 65:189–197, 1996 [DOI] [PubMed] [Google Scholar]
- Goldstein BI, Strober MA, Birmaher B, Axelson D, Esposito–Smythers C, Goldstein T, Leonard H, Hunt J, Gill M, Iyengar S, Grim C, Yang M, Ryan N, Keller M: Substance use disorders among adolescents with bipolar spectrum disorders. Bipolar Disord 10:469–478, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Axelson DA, Birmaher B, Brent DA: Dialectical behavior therapy for adolescents with bipolar disorder: A one-year open trial. J Am Acad Child Adolesc Psychiatry 46:820–830, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Birmaher B, Axelson DA, Goldstein BI, Gill MK, Smythers C, Ryan ND, Strober M, Hunt J, Keller M: Psychosocial functioning among bipolar youth. J Affect Disord 114:174–183, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Birmaher B, Axelson D, Ryan N, Keller M, Strober M, Gill M, Bridge J, Valeri S, Chiappetta L, Leonard H, Hunt J, Brent DA: History of suicide attempts in pediatric bipolar disorder: Factors associated with increased risk. Bipolar Disord 7:525–535, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Fersch RK, Rivera M, Axelson DA, Goldstein BI, Birmaher B, Brent DA: Dialectical Behavior Therapy for adolescents with bipolar disorder. Paper presented at the annual meeting of the Association of Behavioral and Cognitive Therapies, San Francisco, CA, November, 2010 [Google Scholar]
- Goldstein TR, Fersch–Podrat RK, Rivera M, Axelson DA, Goldstein BI, Birmaher B, Brent DA: Dialectical Behavior Therapy for adolescents with bipolar disorder: Preliminary findings on suicide-related outcomes, paper presented at the annual meeting of the Association for Behavioral and Cognitive Therapies, Toronto, Canada, November, 2011 [Google Scholar]
- Goldstein TR, Ha W, Axelson DA, Goldstein BI, Liao F, Gill MK, Ryan ND, Yen S, Hunt J, Hower H, Keller M, Strober M, Birmaher B: Predictors of prospectively observed suicide attempts among youth with bipolar disorder. Arch Gen Psychiatry 69:1113–1122, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herschell AD, Kogan JN, Celedonia K, Gavin J, Stein B: Understanding community mental health administrators' perspectives on Dialectical Behavior Therapy implementation. Psychiatr Serv 60:989–992, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlastala S, Kotler J, McClellan J, McCauley E: Interpersonal and social rhythm therapy for adolescents with bipolar disorder: Treatment development and results from an open trial. Depress Anxiety 27:457–464, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hlastala SA, Frank E: Adapting interpersonal and social rhythm therapy to the developmental needs of adolescents with bipolar disorder. Dev Psychopathol 18:1267–1288, 2006 [DOI] [PubMed] [Google Scholar]
- Hlatky MA, Oewens DK, Sanders GD: Cost-effectiveness as an outcome in randomized clinical trials. Clin Trials 3:543–551, 2006 [DOI] [PubMed] [Google Scholar]
- Hollingshead A: Four-factor Index of Social Status. New Haven: Yale University; 1975 [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N: Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988, 1997 [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald–Scott P, Andreasen NC: The Longitudinal Interval Follow-Up Evaluation: A comprehensive method for outcome in prospective longitudinal studies. Arch Gen Psychiatry 44:540–548, 1987 [DOI] [PubMed] [Google Scholar]
- King CA, Kramer A, Preuss L, Kerr DC, Weisse L: Youth-nominated support team for suicidal adolescents: A randomized controlled trial. J Consult Clin Psychol 74:199–206, 2006 [DOI] [PubMed] [Google Scholar]
- Klein DA, Miller AL: Dialectical behavior therapy for suicidal adolescents with borderline personality disorder. Child Adolesc Psychiatr Clin N Am 20:205–216, 2010 [DOI] [PubMed] [Google Scholar]
- Kowatch R, Fristad MA, Birmaher B, Wagner KD, Findling R, Hellander M: Treatment guidelines for children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 44:213–235, 2005 [DOI] [PubMed] [Google Scholar]
- Leibenluft E, Charney DS, Pine D: Researching the pathophysiology of pediatric bipolar disorder. Biol Psychiatry 53:1009–1020, 2003 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib IH: Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. Am J Psychiatry 157:1584–1591, 2000 [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Seeley JR, Klein DN: Bipolar disorder in adolescents: Epidemiology and suicidal behavior. In: Bipolar Disorder in Childhood and Early Adolescence, edited by Geller B, DelBello M.P. New York: Guilford Press, 7–24, 2003 [Google Scholar]
- Linehan M, Comtois KA, Murray A, Brown MZ, Gallop R, Heard H, Korslund K, Tutek D, Reynolds S, Lindenboim N: Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry 63:757–766, 2006 [DOI] [PubMed] [Google Scholar]
- Linehan MM: Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press, 1993 [Google Scholar]
- Linehan MM, Tutek DA, Heard HL, Armstrong H: Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. Am J Psychiatry 151:1771–1776, 1994 [DOI] [PubMed] [Google Scholar]
- McClellan J, Kowatch R, Findling RL, Workgroup on Quality Improvement: Practice parameter for the assessment and treatment of children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 46:107–125, 2007 [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, Birmaher B, George EL, Taylor DO, Schneck CD, Beresford CA, Dickinson LM, Craighead WE, Brent DA: Family-focused treatment for adolescents with bipolar disorder: Results of a two-year randomized trial. Arch Gen Psychiatry 65:1053–1061, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller AL, Rathus JH, Landsman M, Linehan MM: Dialectical Behavior Therapy: Multi-Family Skills Training Group. Unpublished manual, 2003
- Miller AL, Rathus JH, Linehan MM: Dialectical Behavior Therapy with Suicidal Adolescents. New York: Guilford Press, 2006 [Google Scholar]
- Miller AL, Smith HL, Klein DA, German M: Engaging suicidal youth in outpatient treatment: theoretical and empirical underpinnings. Arch Suicide Res 14:111–119, 2010 [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ: Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol 114:140–146, 2005 [DOI] [PubMed] [Google Scholar]
- Pavuluri MN, Graczyk P, Henry D, Carbray JA, Heidenreich J, Miklowitz DJ: Child- and family- focused cognitive behavioral therapy for pediatric bipolar disorder: Development and preliminary results. J Am Acad Child Adolesc Psychiatry 43:528–537, 2004 [DOI] [PubMed] [Google Scholar]
- Peele PB, Axelson DA, Xu Y, Malley ER: Use of medical and behavioral health services by adolescents with bipolar disorder. Psychiatr Serv 55:1392–1396, 2004 [DOI] [PubMed] [Google Scholar]
- Rathus JH, Miller AL: Dialectical behavior therapy adapted for suicidal adolescents. Suicide Life Threat Behav 32:146–157, 2002 [DOI] [PubMed] [Google Scholar]
- Reynolds WM: Suicidal ideation Questionnaire-Junior. Odessa, FL: Psychological Assessment Resources Inc., 1987 [Google Scholar]
- Richardson J: Eta squared and partial eta squared as measures of effect size in educational research. Educ Res Rev 6:135–147, 2011 [Google Scholar]
- Rizzo CJ, Esposito–Smythers C, Swenson L, Birmaher B, Ryan ND, Strober M, Chiappetta L, Valeri S, Hunt J, Axelson D, Leonard H, Keller M: Factors associated with mental health service utilization among bipolar youth. Bipolar Disord 9:839–850, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schottle D, Huber C, Bock T, Meyer T: Psychotherapy for bipolar disorder: A review of the most recent studies. Curr Opin Psychiatry 24:549–555, 2011 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H: A Children's Global Assessment Scale (C-GAS). Arch Gen Psychiatry 40:1228–1231, 1983 [DOI] [PubMed] [Google Scholar]
- Stanley B, Brown G, Brent D, Wells K, Poling K, Kennard B, Wagner A, Curry J, Cwik M, Goldstein T, Klomek–Brunstein A, Barnett S, Daniel S: Cognitive Behavior Therapy for Suicide Prevention (CBT-SP): Treatment model, feasibility and acceptability. J Am Acad Child Adolesc Psychiatry 48:1005–1013, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stensland M, Ascher–Svanum H, Ball D: Costs associated with attempted suicide among individuals with bipolar disorder. J Ment Health Policy Econ 13:87–92, 2010 [PubMed] [Google Scholar]
- Strober M, Schmidt–Lackner S, Freeman R, Bower S, Lampert C, DeAntonio M: Recovery and relapse in adolescents with bipolar affective illness: A five-year naturalistic, prospective follow-up. J Am Acad Child Adolesc Psychiatry 34:724–731, 1995 [DOI] [PubMed] [Google Scholar]
- Tamas Z, Kovacs M, Gentzler AL, Tepper P, Gagaros J, Kiss E, Kapornai K, Vetro A: The relations of temperament and emotion self-regulation with suicidal behaviors in a clinical sample of depressed children in Hungary. J Abnorm Psychol 35:640–652, 2007 [DOI] [PubMed] [Google Scholar]
- Van Dijk S, Jefferey J, Katz M: A randomized, controlled, pilot study of dialectical behavior therapy skills in a psychoeducational group for individuals with bipolar disorder. J Affect Disord 145:386–393, 2013 [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL: Reliability and validity of the longitudinal interval follow-up evaluation for assessing the outcome of anxiety disorders. J Psychiatr Res 28:531–545, 1994 [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB: Maintaining reliability in a long-term psychiatric study: an ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. J Psychiatr Res 35:297–305, 2001 [DOI] [PubMed] [Google Scholar]
- West AE, Jacobs R, Westerholm R, Lee A, Carbray J, Heidenreich J, Pavuluri M: Child and family-focused cognitive behavioral therapy for pediatric bipolar disorder: Pilot study of group treatment format. J Am Acad Child Adolesc Psychiatry 18:239–246, 2009 [PMC free article] [PubMed] [Google Scholar]