Abstract
Objective: Suicide among adolescents is a major public health problem. Decision-making deficits may play an important role in vulnerability to suicidal behavior, but few studies have examined decision-making performance in youth at risk for suicide. In this study, we seek to extend recent findings that adolescent suicide attempters process risk evaluations differently than adolescents who have not attempted suicide.
Methods: We assessed decision-making in 14 adolescent suicide attempters and 14 non-attempter comparison subjects, ages 15–19, using the Cambridge Gambling Task (CGT). Each participant was also administered a diagnostic interview (Mini-International Neuropsychiatric Interview [MINI]), structured suicide severity measures, and a brief intelligence quotient (IQ) measure.
Results: After controlling for gender and IQ differences, suicide attempters displayed an elevated risk-taking propensity on the CGT relative to comparison subjects, such that they were more willing to take a large risk with their bank of points, a decision-making style that proves disadvantageous over time. No group differences in the latency or accuracy of decision-making were observed.
Conclusions: Adolescents with a history of suicide attempt display increased risk-taking and greater difficulty predicting probable outcomes on the CGT. Such deficits have been associated with dysfunction in the orbitofrontal prefrontal cortex, which supports other studies implicating impaired decision-making among individuals with a history of suicide attempt.
Introduction
Suicidal behavior is a serious and growing public health problem, particularly among adolescents. In a nationally representative study, Nock and colleagues (2013) estimated that 12.1% of United States adolescents experience suicidal ideation, 4.0% develop a plan to engage in suicidal behavior, and 4.1% attempt suicide. More than half of those with a plan attempt suicide within the 1st year of onset. Furthermore, suicidal behaviors increase substantially during adolescence (Cash and Bridge 2009), a period of significant social, emotional, and neurocognitive change.
An examination of decision making in the context of risk calculation is critical to understanding adolescent suicidal behavior. Prior studies using adult samples have linked suicidal behavior to specific neurocognitive factors including executive dysfunction and decision-making deficits (Jollant et al. 2005; Dour et al. 2011; Chamberlain et al. 2013; Keilp et al. 2013) in the context of relatively unimpaired global brain functioning (Marzuk et al. 2005). Behavioral and neuroimaging data have increasingly implicated prefrontal cortex (PFC) deficits, and associated reward-sensitive pathways in the expression of suicidal behavior among at-risk individuals (Mann 2003; Oquendo et al. 2003; Monkul et al. 2007; Jollant et al. 2010; Dombrovski et al. 2013). Relative to adults, adolescents are vulnerable to decision-making deficits because of an underdeveloped ability to judge long-term risk (Blakemore and Robins 2012). Moreover, compared with adolescents who have not attempted suicide, adolescents with a history of suicide attempt predict adverse outcomes less accurately, and negative consequences appear to influence decision making to a lesser degree (Bridge et al. 2012).
Few studies have examined associations between risk-sensitive decision making and suicidal behavior among adolescents. The current study investigates adolescent decision making in the context of systematic variation of risk conditions, and aims to extend previous findings (Bridge et al. 2012), suggesting that adolescents with a history of recent suicide attempt display decision-making impairments in comparison with never-suicidal youth. However, unlike the previous study by Bridge and colleagues (2012), we employed the Cambridge Gambling Task (CGT) from the Cambridge Automated Battery of Neuropsychological Function (CANTAB). A primary difference between the Iowa Gambling Task (IGT), used by Bridge et al. (2012), and the CGT, is that the CGT explicitly presents probability conditions (visually) under conditions of uncertainty and reward. It does not rely on the multitrial learning for which the IGT is well known. The CGT involves fewer cognitive demands for working memory, reinforcement learning, and reversal learning than the IGT (Fellows and Farah 2005), making alternative explanations for risky betting less plausible, should group differences be determined.
Methods
Subjects
The sample consisted of youth, 15–19 years of age, 14 who had attempted suicide and 14 psychiatric controls matched on age, sex, and race, who had never engaged in suicidal behavior. Suicide attempt was defined as self-injurious behavior with stated or inferred intent to die, within 1 year of the recruitment date. All participants from this study had participated in a larger study of suicidal behavior (see Bridge et al. 2012 for eligibility and recruitment criteria). Participants had at least one legal guardian available for a caregiver interview. The study was approved by the institutional review board (IRB) of The Research Institute at Nationwide Children's Hospital. Informed consent and assent were obtained from all participants and their parents or guardians.
Assessment
Demographic information was elicited from subjects using a general information sheet. Lifetime family history of suicidal behavior (suicide, suicide attempts) among first degree relatives was obtained using the Family History Screen (Weissman et al. 2000). Lifetime history of suicide attempts was assessed using the Columbia University Suicide History Form (Posner et al. 2011), which was administered to both subjects and parents as a semistructured interview. We inquired about number of suicide attempts, methods, medical lethality, and triggering events. When a history of suicide attempt was reported, the Pierce Suicide Intent Scale (Pierce 1977) was administered to assess relevant behavioral and circumstantial aspects surrounding the suicide attempt, including plans, preparation, and lethality. Psychiatric diagnoses were obtained using the Mini-International Neuropsychiatric Interview (MINI) (Sheehan et al. 2010), a brief, structured diagnostic interview. Psychotropic medication use within the month prior to the interview was assessed by the Services Assessment for Children and Adolescents (Stiffman et al. 2000). Each participant was administered the Kaufman Brief Intelligence Test, 2nd edition (Kaufman and Kaufman 2004), which served as a brief general intellectual assessment.
To assess risk-sensitive decision making, participants were administered the CGT from the CANTAB (Cambridge Cognition 2006) using a touch-screen computer. The CGT is a sensitive tool for assessing orbitofrontal functioning, and has been used to detect reliable differences between adults who had attempted suicide and those who had not, on indices of risk-sensitive decision making (Clark et al. 2011; Chamberlain et al. 2013).
The CGT is a gambling and decision-making task in which subjects are presented with an array of 10 colored boxes, either red or blue, and are required to decide whether a yellow token is hidden inside a red or blue box. Choices are associated with explicit risks of winning or losing dependent upon the ratio of red to blue boxes (e.g., 7 red, 3 blue=70% chance of winning one's bet when placed on red). Subjects then place a bet on their decision. The amount of the bet is then added to (if correct) or subtracted from (if incorrect) the subject's total point score. Bets are either offered in ascending order, beginning with a small bet until the subject chooses a bet, or in descending order, beginning with a large bet.
The primary dependent variables from the CGT task included for this study were rational choices (%), decision latency (ms), and overall proportion bet (%). “Rational choices” represents the proportion of trials in which the majority color was chosen. Decision latency represents the response time to make a decision (red/blue). Overall proportion bet is the average amount of points that the participant chooses to bet on each trial across explicit risk conditions presented in a pseudorandom order. Because high CGT betting patterns increase potential losses, the overall proportion bet variable is hypothesized to reflect a participant's risk-sensitive decision making, and may differentiate attempters from psychiatric controls.
Statistical analyses
Demographic, clinical, and neurocognitive characteristics were compared between attempters and comparison subjects by using independent t tests and Fisher's exact test (FET) as appropriate (see Table 1). The CGT decision latency and betting dependent variables were compared between groups in an unadjusted univariate model, followed by a 2 x 2 ANOVA adjusting for gender and intelligence quotient (IQ), given differences on dependent variables detected in preliminary analyses (e.g., males riskier than females; decision-making accuracy associated with IQ; see Table 1). A Mann–Whitney U test was used to test for group differences in CGT Rational Choices scores because the Shapiro–Wilk normality test indicated significant deviation from a normal distribution, and common data transformations did not normalize this variable. Separate van Elteren tests, a type of stratified Wilcoxon–Mann–Whitney test for comparing two groups accounting for strata, were used to determine whether gender or IQ (based on median split=96) influenced the overall findings for the Rational Choices scores. Because the two groups were matched one-to-one, we also examined CGT outcome variables using paired t tests for decision latency and betting dependent variables and the Wilcoxon signed rank test for Rational Choices scores.
Table 1.
Comparison of Adolescent Suicide Attempters and Nonattempter Comparison Subjects
| Suicide attempters (n=14) | Comparison subjects (n=14) | Statistic | p value | |
|---|---|---|---|---|
| Sample characteristics | ||||
| Agea | 16.9 (1.1) | 16.9 (1.1) | t=0.00 | p=1.00 |
| IQa | 102.1 (17.3) | 95.7 (13.1) | t=1.10 | p=0.28 |
| Sex | ||||
| Male | 36% | 36% | χ2=0.00 | p=1.00 |
| Female | 64% | 64% | ||
| Race | ||||
| White, non-Hispanic | 79% | 79% | χ2=0.00 | p=1.00 |
| Black, non-Hispanic | 21% | 21% | ||
| Mental health diagnosisb | 57% | 57% | χ2=0.00 | p=1.00 |
| Mood disorder | 14% | 7% | χ2=0.37 | p=0.54 |
| Anxiety disorder | 21% | 29% | χ2=0.19 | p=0.66 |
| Externalizing disorder | 36% | 29% | χ2=0.16 | p=0.69 |
| Substance use disorder | 14% | 7% | χ2=0.37 | p=0.54 |
| Psychotropic medicationc | 71% | 46% | χ2=1.78 | p=0.20 |
| CGT outcomes | ||||
| Rational Choices (%)d | 0.87 (0.16) | 0.92 (0.11) | MWU=73.50 | p=0.27 |
| Decision Latency (ms)e | 1941.9 (448.2) | 1839.2 (533.4) | t26=0.96 | p=0.35 |
| Overall Proportion Bet (%)e | 0.57 (0.11) | 0.52 (0.09) | t26=2.15 | p=0.04 |
Means (standard deviations) reported.
Mental health diagnosis refers to current diagnosis derived from the Mini-International Neuropsychiatric Interview (MINI) at the time of the research visit.
Information about psychotropic medications including antidepressant, mood stabilizer, anxiolytic, stimulant, sleep-specific, and antipsychotic medications was obtained using the Service Assessment for Children and Adolescents (SACA).
Findings of no group differences on Rational Choices scores remained in separate van Elteren tests that controlled for intelligence quotient (IQ) and gender.
p values are adjusted for IQ and gender.
CGT, Cambridge Gambling Task; MWU, Mann–Whitney U.
Matched results were very similar to unmatched results and, therefore, results shown are unmatched, as these are easier to display. For overall proportion bet, a repeated measures analysis of covariance (ANCOVA) was conducted accounting for variable ratio presentations caused by a main effects for box ratio condition. We analyzed the overall proportion bet as the dependent measure, the fixed factors of box ratio (within- subjects: 9:1, 8:2, 7:3, 6:4), group (between-subjects), gender, and IQ as covariates. Separate analyses were run for ascending and descending conditions of the CGT, but results did not differ; therefore, only combined results are presented. The Greenhouse–Geisser correction was used when the assumption of sphericity was violated; the test statistic for these estimates is denoted by ɛ. All tests were two tailed and p<0.05 was considered significant. Statistical analyses were conducted with SPSS, version 21.0 (IBM SPSS Statistics, Somers, NY)
Results
There were no demographic or clinical differences between the suicide attempters and comparison subjects in terms of age, gender, race, intellectual functioning, rates of psychotropic medication use, or mental health diagnosis (see Table 1). Initial unadjusted models indicate no statistically significant group differences across dependent variables. Because of associations between gender and IQ on preliminary analyses as well as a priori assumptions, an adjusted model (2×2 ANOVA) accounting for these covariates was conducted. There was a significant main group effect such that attempters wagered more than nonattempters (see Table 1). Males wagered significantly more than females, but there was no significant group by gender interaction. Adjusted models indicate no significant differences between attempters and nonattempters in rational choices or decision latency.
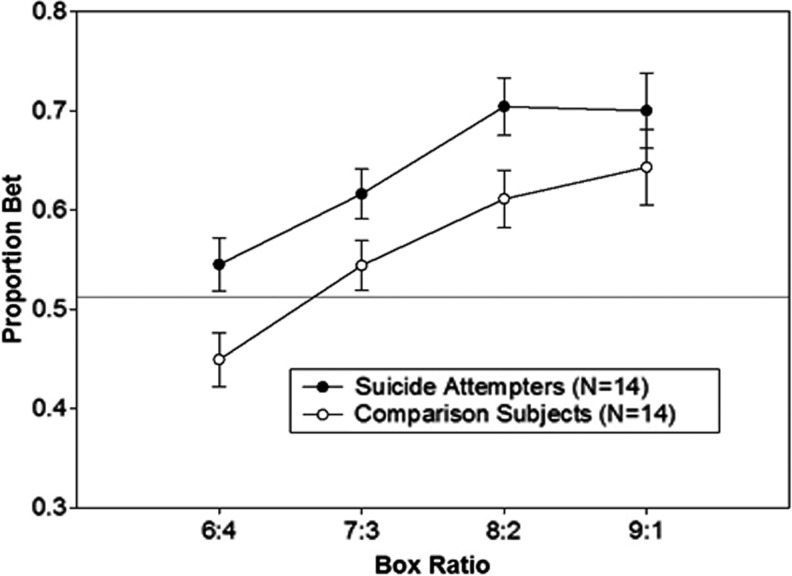
The repeated measures ANCOVA on overall proportion bet performed to account for box ratio differences revealed a significant effect of group (F1,24=5.41, p=0.029, η2=0.18) and a significant effect of ratio (F1.88, 45.12=5.45, ɛ=0.63, p=0.009, η2=0.19). This finding indicates that attempters bet significantly higher amounts than comparison subjects across box ratio conditions, although both groups were more likely to select the majority box color at higher ratios (Fig. 1). There was a main effect of gender (F1,24=11.25, p=0.003, η2=0.32), such that boys placed higher bets than girls across ratio. The box ratio by IQ interaction was significant (F1.88, 45.12=8.89, ɛ=0.63, p=0.001, η2=0.27), because subjects with higher IQs bet less at the more uncertain, lower ratios than at higher ratios. The box ratio by group and box ratio by gender interaction terms were not significant (p>0.25).
FIG. 1.
Overall proportion of points bet as a function of box ratio in adolescent suicide attempters and comparison subjects, controlling for participant gender and intelligence quotient (IQ).
Discussion
Participants with a history of suicide attempt displayed an overall tendency to bet more on an explicit gambling task despite an equivalent capacity to make rational choices. Findings are consistent with a recent study implicating impaired decision making in favor of short-term gain among adolescents with a history of suicide attempt assessed by the IGT (Bridge et al. 2012). The CGT paradigm from the CANTAB, however, reduces the potential confounding demands for working memory, reinforcement, and reversal learning that the IGT requires, thereby simplifying risk calculations for participants. Whereas the IGT measures decision making under uncertainty and risk, the CGT eliminates much of the uncertainty element by providing an explicit ratio for participants to choose (Clark et al. 2011). Our study provides preliminary support for the theory that adolescents with a history of suicide attempt display a riskier betting style than adolescents with no history of attempt, perhaps representing a failure to account for the possibility of low-incidence negative consequences. Although their decisions are not significantly less likely to be accurate, attempters do not appear to protect themselves against highly aversive outcomes, unlike nonattempters.
Our findings are partially consistent with recent results from a nonclinical, young adult sample, which found decision-making accuracy and risk-taking differences among suicide attempters and comparison subjects (Chamberlain et al. 2013). Results suggest that participants with a history of suicide attempt were not different from nonattempters in their ability to identify appropriate choices during the gambling task. However, suicide attempters were more likely to take a large risk with their bank of points, which proves disadvantageous over time. This particular deficit in risk-sensitive decision making appears to reflect a minimization of negative outcomes in the face of uncertainty, and has been associated with deficits in the orbitofrontal prefrontal cortex (Fellows and Farah 2005; Jollant et al. 2010). In previous adult studies, suicide attempts were associated with a style of decision processing that discounted past consequences in favor of immediate loss or gain (Jollant et al. 2005; Dombrovski, et al. 2010, 2013). The authors concluded that suicide attempters were vulnerable to a specific type of executive dysfunction, such that learning from past events was more challenging for attempters than for nonattempters.
Our findings add to a growing literature suggesting that attempted suicide is associated with an increased risk-taking propensity that may place individuals at risk beyond psychopathology alone (see Richard-Devantoy et al. 2013). Findings suggest that adolescent suicide attempters process risk evaluations differently than adolescents who have not attempted suicide. Data suggest potential cognitive vulnerability stemming from orbitofrontal prefrontal cortex-related deficits of uncertain etiology. Although findings are consistent with those in the adult literature demonstrating a link between impaired decision-making and attempted suicide, associations between risk-taking propensity and attempted suicide in adolescence has received limited attention to date.
Findings are promising but stem from a relatively small, homogeneous clinic-referred sample and warrant replication. Although decision-making deficits among suicide attempters were detected, this preliminary study was underpowered to detect differences with small to moderate effect sizes. The ability to examine potential interactions between history of suicide attempt and variables of interest such as age, gender, intellectual functioning, substance use, and comorbid diagnoses was also limited. The data presented are cross-sectional and it remains unclear whether risk-sensitive decision-making deficits predispose an individual to a suicide attempt, or whether living with a mood disorder and its associated biological changes contributes to distinct patterns of risk evaluation. In future studies, longitudinal designs will be necessary to test the direction of effects and obtain a clearer understanding of how neurocognitive markers of suicidal behavior change throughout adolescence. It would also be highly relevant to distinguish state-dependent from trait-specific aspects of risk taking. Overall, this study provides preliminary evidence that a history of suicide attempt in adolescence is linked with impaired decision making in ways that are consistent with adult and young adult samples.
Clinical Significance
There are few studies that look at risk-sensitive decision-making among adolescent suicide attempters. Data from our study suggest that adolescents with a history of suicide attempt showed riskier betting styles and greater difficulty predicting probable outcomes on the CGT than did nonattempting psychiatric controls. Such behavioral deficits have been associated with orbitofrontal dysfunction.
Acknowledgments
The authors gratefully acknowledge the youth and parents who participated in this study, and the staff of Community Behavioral Health Services at Nationwide Children's Hospital for their assistance with subject recruitment.
Disclosures
No competing financial interests exist.
References
- Blakemore SJ, Robbins TW: Decision-making in the adolescent brain. Nat Neurosci 15:1184–1191, 2012 [DOI] [PubMed] [Google Scholar]
- Bridge JA, McBee–Strayer SM, Cannon EA, Sheftall AH, Reynolds B, Campo JV, Pajer KA, Barbe RP, Brent DA: Impaired decision making in adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry 51:394–403, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cambridge Cognition: CANTABeclipse Version 3. Test Administration Guide. Cambridge: Cambridge Cognition Ltd.; 2006 [Google Scholar]
- Cash SC, Bridge JA: Epidemiology of youth suicide and suicidal behavior. Curr Opin Pediatr 21:613–619, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Odlaug BL, Schreiber LR, Grant JE: Clinical and neurocognitive markers of suicidality in young adults. J Psychiatr Res 47:586–591, 2013 [DOI] [PubMed] [Google Scholar]
- Clark L, Dombrovski AY, Siegle GJ, Butters MA, Shollenberger CL, Sahakian BJ, Szanto K: Impairment in risk-sensitive decision-making in older suicide attempters with depression. Psychol Aging 26:321–330, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Clark L, Siegle GJ, Butters MA, Ichikawa N, Sahakian BJ, Szanto K: Reward/punishment reversal learning in older suicide attempters. Am J Psychiatry 167:699–707, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dombrovski AY, Szanto K, Clark L, Reynolds CF, Siegle GJ: Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatr 70:1020–1103, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dour HJ, Cha CB, Nock MK: Evidence for an emotion-cognition interaction in the statistical prediction of suicide attempts. Behav Res Ther 49:294–298, 2011 [DOI] [PubMed] [Google Scholar]
- Fellows LK, Farah MJ: Different underlying impairments in decision-making following ventromedial and dorsolateral frontal lobe damage in humans. Cereb Cortex 15:58–63, 2005 [DOI] [PubMed] [Google Scholar]
- Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, Castelnau D, Malafosse A, Courtet P: Impaired decision making in suicide attempters. Amer J Psychiatry 162:304–310, 2005 [DOI] [PubMed] [Google Scholar]
- Jollant F, Lawrence NS, Olie E, O'Daly O, Malafosse A, Courtet P, Phillips ML: Decreased activation of lateral orbitofrontal cortex during risky choices under uncertainty is associated with disadvantageous decision-making and suicidal behavior. Neuroimage 51:1275–1281, 2010 [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL: Kaufman Brief Intelligence Test. 2nd ed. Minneapolis: Pearson; 2004 [Google Scholar]
- Keilp JG, Gorlyn M, Russell M, Oquendo MA, Burke AK, Harkavy–Friedman J, Mann JJ: Neuropsychological function and suicidal behavior: Attention control, memory and executive dysfunction in suicide attempt. J Psychol Med 43:539–551, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann JJ: Neurobiology of suicidal behaviour. Nat Rev Neurosci 4:819–828, 2003 [DOI] [PubMed] [Google Scholar]
- Marzuk PM, Hartwell N, Leon AC, Portera L: Executive functioning in depressed patients with suicidal ideation. Acta Psychiatr Scand 112: 294–301, 2005 [DOI] [PubMed] [Google Scholar]
- Monkul ES, Hatch JP, Nicoletti MA, Spence S, Brambilla P, Lacerda AL, Sassi RB, Mallinger AG, Keshavan MS, Soares JC: Fronto-limbic brain structures in suicidal and non-suicidal female patients with major depressive disorder. Mol Psychiatry 12:360–366, 2007 [DOI] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, Kessler RC: Prevalence, correlates and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication – Adolescent Supplement (NCS-A). JAMA Psychiatry 70:300–310, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Placidi GP, Malone KM, Campbell C, Keilp J, Brodsky B, Kegeles LS, Cooper TB, Parsey RV, van Heertum RL, Mann JJ: Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry 60:14–22, 2003 [DOI] [PubMed] [Google Scholar]
- Pierce DW: Suicidal intent in self-injury. Br J Psychiatry 130:377–385, 1977 [DOI] [PubMed] [Google Scholar]
- Posner K, Brown G, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ: The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 168:1266–1277, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard–Devantoy S, Berlim MT, Jollant F: A meta-analysis of neuropsychological markers of vulnerability to suicidal behavior in mood disorders. Psychol Med 1–11, 2013 [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, Milo KM, Stock SL, Wilkinson B: Reliability and Validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J Clin Psychiatry 71:313–326, 2010 [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Horwitz SM, Hoagwood K, Compton W, Cottler L, Bean DL, Narrow WE, Weisz JR: The Service Assessment for Children and Adolescents (SACA): Adult and child reports. J Am Acad Child Adolesc Psychiatry 39:1032–1039, 2000 [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M: Brief screening for family psychiatric history: The Fail History Screen. Arch Gen Psychiatry 57:675–682, 2000 [DOI] [PubMed] [Google Scholar]