Abstract
Objective: The purpose of this study was to conduct a treatment development study to examine the feasibility, acceptability, and preliminary efficacy of treating depressed, suicidal adolescents and their depressed parent concurrently in a cognitive behavioral therapy (CBT) protocol (Parent-Adolescent-CBT [PA-CBT]).
Methods: A randomized, controlled, repeated measures design was used to test the hypothesis that PA-CBT would lead to greater reductions in suicidality and depression compared with Adolescent Only CBT (AO-CBT). Participants included 24 adolescent and parent dyads in which the adolescent met American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) criteria for current major depressive episode (MDE) and the parent met DSM-IV criteria for current or past MDE.
Results: The concurrent protocol was found to be feasible to implement with most depressed adolescents and parents. Adolescent ratings of program satisfaction were somewhat lower in PA-CBT, suggesting that some teens view treatment negatively when they are required to participate with a parent. The concurrent treatment protocol was more effective in reducing depressed mood in the parent–adolescent dyad at the end of maintenance treatment (24 weeks) than treating an adolescent alone for depression; the largest effect was on parental depressed mood. This difference between dyads was no longer significant, however, at the 48 week follow-up. Adolescent and parent suicidal ideation improved equally in both groups during active and maintenance treatment, and remained low at follow-up in both groups.
Conclusions: The PA-CBT protocol is feasible to conduct and acceptable to most but not all adolescents. The strongest effect was on parental depressed mood. A larger study that has sufficient power to test efficacy and moderators of treatment outcome is necessary to better understand which adolescents would benefit most from concurrent treatment with a parent.
Introduction
Both depression and suicidality are highly familial. The risk of developing depression among children of depressed parents is between two and four times greater than for children whose parents are not depressed (Goodman 2007; Hammen 2009). Offspring of parents who attempt suicide are six times more likely to attempt suicide than the offspring of non-attempters (Brent et al. 2002). Genetic risk factors have been found for depressive disorders (Caspi et al. 2003, 2010; Bosker et al. 2011), suicidality (Brent and Mann 2005), and co-occurring suicidality and depression (Mann et al. 2000; Klempan et al. 2009; Schosser et al. 2012). Other studies have pointed to contextual factors as having an equal influence on adolescent offspring, including parental maladaptive cognitions, parental psychopathology, poor parenting, and family conflict (Goodman and Gotlib 1999).
Links between parent and child suicidality represent a complex interaction of psychosocial risk factors. Although family conflict is often described as one of the most salient predictors of adolescent suicidality (Wilkinson et al. 2011; Brent et al. 2013), the processes underlying this link are less clear. Deficits in family communication and problem solving may also play a role, as parents and teens fail to consider alternative responses to life stressors and are unable to adequately communicate with each other (Wagner 1997). Some adolescents may express suicidality as a means to decrease conflict in their home, by shifting attention away from the conflict to themselves, or as a means of escape from school and other problems. Alternatively, parents may inadvertently reinforce suicidal behavior (Wagner et al. 2003), by acquiescing to demands when adolescents use suicide threats to control their environment or to terminate aversive family relationship patterns. For example, a parent of an adolescent with a suicide attempt history might be reluctant to enforce a consequence out of fear that limit setting may cause another suicide attempt. A parent's own emotional distress may also contribute to adolescents' suicidality. For example, a parent with a history of depression and suicidality may respond to conflicts by modeling suicidal statements or actually attempting suicide. Parental factors may also interfere with basic aspects of adolescent treatment, including session attendance and monitoring of medication compliance.
Despite the strong association between parent and teen depression and suicidality, most treatment protocols for adolescent depressed mood and suicidality include minimal parental involvement. One review (Sander and McCarty 2005) found that parents were not included in two thirds of treatment studies for adolescent depression, and the effects of parental depressed mood on parenting style and parent–child interactions have rarely been treatment targets for depressed adolescents. However, maternal depressive symptoms are strong predictors of poor treatment response for depressed and suicidal teens (Brent et al. 1998) as well as anxious children and adolescents (Southam-Gerow et al. 2001). Some treatment studies of adult depression have found a relationship between improvement in child and adolescent symptomatology and improvement in parental depression (Gunlicks and Weissman 2008). For example, Weissman and colleagues (2006) studied the children (7–17 years old) of parents treated for depression in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study, and found that remission of maternal depression after 3 months of psychotropic medication treatment resulted in a corresponding decrease in their children's rate of diagnosis and symptomatology. Compas et al. (2011) compared a family group cognitive-behavioral (FGCB) preventive intervention with a written information comparison condition for families with a depressed parent. They found that FGCB condition showed a trend toward greater reductions in parental depressive symptoms, and was associated with lower rates of major depressive episodes in youth (ages 9–15) over the course of 2 years.
Although it is common clinical practice to refer parents to individual treatment for their own depression, follow-up on whether these services have been obtained is typically limited. An integrated protocol for depressed adolescents with a depressed parent would ensure that parents actually do receive therapy. In addition, using the same theoretical approach to psychotherapy with both parents and adolescents has the potential to enhance treatment outcomes by creating a synergy between parent and child. For example, if both family members are taught problem solving in cognitive behavioral therapy (CBT), then parents can reinforce their teens' use of this skill in stressful circumstances. In addition, coordinating services for the parent and teen eliminates the potential for conflicting treatment recommendations, and may improve session attendance because of mutual convenience of scheduling.
The present study examined the feasibility, acceptability, and preliminary efficacy of a concurrent parent-adolescent CBT protocol (PA-CBT) in a stage I clinical trial. A randomized, controlled, repeated measures design was used to test the hypothesis that PA-CBT would lead to greater reductions in adolescent suicidality and depression compared with Adolescent Only CBT (AO-CBT).
Method
Participants
Participants included 24 adolescent and parent dyads who lived together in the Northeast and spoke English. Adolescent participants were eligible if they: 1) were 11–17 years old, 2) met American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM-IV) criteria for current major depressive episode (MDE) (American Psychiatric Association 1994), 3) had a Clinical Depression Severity Rating Scale (CDRS) (Poznanski 1984) t score ≥65, and 4) had experienced current or past suicidality (as reported on the Beck Depression Inventory II (BDI-II) (Beck et al. 1996) or The Kiddie Schedule for Affective Disorders and Schizophrenia- Present Version (K-SADS-P) (Kaufman et al. 1997). Parent eligibility included: either 1) DSM-IV criteria for current or past MDE, and 2) a minimum BDI score of 15 for parents with a current MDE and a minimum BDI score of 10 for parents with a past MDE. Adolescents and parents were excluded for bipolar disorder, substance use disorder, developmental/cognitive delays, or psychosis.
Measures
Past week suicidality was measured with the Beck Suicide Scale (BSS) (Beck et al. 1979) for adolescents and parents. Scores on item 20, which assesses number of prior attempts, were combined with K-SADS and The Structured Clinical Interview for DSM-IV – Patient Version (SCID-I/P) questions about suicide to arrive at a consensus score for suicide attempts. The BDI-II (Beck et al. 1996) was used to assess adolescent and parent symptoms of depression. Internal consistency for this sample on the BSS and BDI were excellent (α=0.90 for both adolescent measures; α=0.93 and 0.95 for parents, respectively). The CDRS was administered to adolescent participants as a measure of clinician-rated depression (α=0.77). The K-SADS was administered separately to parents and adolescents with diagnoses determined by consensus with a third clinician. SCID-I/P (First et al. 1995) was used to diagnose past and current MDE in parents. A second clinician rated 20% of all CDRS, K-SADS, and SCID-I/P interviews to establish reliability. Inter-rater reliability for the CDRS, K-SADS, and SCID-I/P ranged from 0.69 to 0.94.
Several constructs known to be strongly related to suicidality were used to characterize the sample. The Hopelessness Scale for Children (HSC) (Kazdin et al. 1983) was administered to adolescents and the Beck Hopelessness Scale (BHS) (Beck et al. 1974) was administered to parents. Internal consistency was high in both adolescents (α=0.90) and parents (α=0.91). The McLean Screening Instrument for Borderline Personality Disorder (MSI-BPD) (Zanarini et al. 2003) was used at baseline in both adolescent and parent participants; clinical cutoff scores ≥8 out of 10 items were used to classify participants as BPD positive. The Childhood Trauma Questionnaire (CTQ) (Bernstein et al. 1994) was used at baseline to assess history of trauma (α=0.92).
The Client Satisfaction Questionnaire (CSQ) (Larsen et al. 1979), an eight item measure of treatment acceptability rated on a five point Likert Scale, was administered to parent and adolescent participants in PA-CBT at mid-treatment and end of treatment to assess acceptability of treatment. The Working Alliance Inventory (WAI) (Horvath and Greenberg 1989), an 11 item measure on a seven point Likert scale, was rated by adolescents and parents in PA-CBT with respect to their alliance with their therapists.
Procedure
This study was approved by the hospital and university Human Subjects Protection Committees. Participants were referred to the study by local pediatricians, therapists, and psychiatrists, and by social workers arranging dispositions for psychiatrically hospitalized adolescents. All participants provided written informed consent and/or assent if <18 years of age. In order to maximize our experience implementing this new protocol in this treatment development grant, families were randomized on a 2:1 basis with twice as many families receiving the experimental treatment (n=16) as the comparison condition (n=8). Twenty of the 24 dyads completed all research evaluations at baseline, midtreatment (6 weeks), end of treatment (12 weeks), and 48 week follow-up.
Treatment conditions
The adolescent component of the CBT protocol was nearly identical in the two conditions. Both the concurrent PA-CBT and AO-CBT treatments were divided into an acute phase (weekly for 12 weeks) and a maintenance phase (biweekly for 12 weeks).
AO-CBT
In AO-CBT treatment, adolescents were assigned their own therapist and treatment included primarily individual sessions. Parents in the AO-CBT condition participated in end-of-session check-ins regarding the adolescent's progress, for most sessions. Parents in the AO-CBT condition were always involved in sessions where safety concerns were discussed. Adolescent CBT was based on protocols used in prior clinical trials with depressed adolescents (March et al. 2004; Vitiello et al. 2006; Brent et al. 2008; Kennard et al. 2009; Lewis et al. 2010; Esposito-Smythers et al. 2011).
In the AO-CBT and PA-CBT protocols for the adolescent, teens developed safety plans and were taught core skills, including problem solving, cognitive restructuring, affect regulation, and behavioral activation, to address depressed mood and suicidality. Based on the adolescent's individual needs, these skills were then repeated or additional modules (e.g., Chain Analysis of Problem Behaviors, Distress Tolerance) were administered. In addition, conjoint parent– adolescent sessions addressed family problem solving and family communication. A relapse prevention session was conducted at the end of treatment. Adolescents were assigned a personalized “homework” assignment at the end of each session to facilitate practice of a particular CBT skill.
PA-CBT
In PA-CBT treatment, parents and teens were each assigned their own therapist and therapy included individual sessions for parents and adolescents as well as conjoint family sessions. The adolescent sessions in PA-CBT were essentially the same as those in AO-CBT. Parent sessions comprised the same skills as adolescent sessions, using essentially the same format to allow for better communication between parents and adolescents about skills.
In the PA-CBT condition, all individual sessions concluded with a conjoint meeting between parent and teen. The check-in included an exchange of positive comments between the parent and teen to enhance positive communication (Asarnow, personal communication) and a review of the skills learned. The parent and adolescent were assigned a personalized “homework” assignment at the end the session to facilitate practice of a particular CBT skill.
Medication management
Parents and adolescents in the PA-CBT treatment met with the study psychiatrist for medication management. The Texas Children's Medication Algorithm for depression was used to guide psychopharmacology choices for adolescents (Emslie et al. 2004), whereas The Texas Medication Algoritm Project (TMAP) manual was used to guide antidepressant choice for parents (Suehs et al. 2008). Clinical experience guided antidepressant choice for those adolescents and parents who had already had complex antidepressant regimens prior to enrollment. Psychiatry appointments occurred weekly while medications were being modified and during change to dosages, and every other week or monthly when medications were stable.
In order to most closely mimic standard care, parents in the AO-CBT treatment condition were allowed to see their own therapists and take medication. Adolescents in the AO-CBT treatment condition were allowed to take medications for mood problems, but did not meet with the study psychiatrist for medication management.
Training and fidelity
Therapists (n=8) included Masters and Ph.D. level clinicians who saw patients in both treatment conditions. They were trained through didactic instruction, tape reviews, and role plays. All sessions were videotaped. All videos for the first two cases seen by each therapist, and a random selection of 20% of subsequent videos, were reviewed to rate fidelity and provide detailed feedback and supervision. The Cognitive Therapy Rating Scale (CTRS) (Young 1980) was used to assess competency, and checklists of session content were used to assess adherence. Scores ≥44 on the CTRS and adherence to at least 80% of items on session adherence checklists were deemed acceptable.
In both conditions, weekly group supervision was used to discuss skills implementation and review ratings from video reviews. Individual supervision was also provided when emergent situations arose. If therapist drift was evident through any method of supervision, obstacles to adherence were processed, solutions generated, and role plays conducted to enhance training.
Data analyses
Baseline group comparisons and treatment acceptability ratings are reported as between group effect sizes using Cohen's d, with size estimates recommended by Cohen (1988): small, 0.2; medium, 0.5; and large, 0.8. Given the small sample size and the exploratory nature of this study, results were considered worthy of comment if a medium or stronger effect size was found.
Tests of treatment and maintenance effects were simultaneously estimated using maximum likelihood with robust standard errors (MLR) estimation procedures (MPlus Version 7.11) (Muthén and Muthén 1998–2011). MLR estimation procedures were selected, as the estimates of standard errors are robust to distributional concerns such as nonnormality as well as small samples (Muthen and Shedden 1999; McLachlan and Peel 2000). Consistent with recommendations for treatment of missing data in clinical trials (Little et al. 2012), participants with incomplete data were retained through the use of Bayesian estimation procedures with multiple imputation of 100 data sets, which were subsequently used for maximum likelihood estimation with parameter estimates averaged across imputed data sets. Using this intent to treat framework, treatment effects were evaluated using latent growth models (LGM), and treatment maintenance was assessed using a test of regression. Intercept was indicated at baseline and time was parameterized by number of months postbaseline. To account for the non-independence of parent–adolescent dyads, as well as to match group level randomization procedures, treatment effects were first evaluated using mixed LGM with the CLUSTER option applied to account for dyad membership. Treatment and maintenance effects were then modeled separately for parents and adolescents.
Results
Treatment acceptability
Adolescents in AO-CBT (mean=26.83, SD=4.62) scored higher on the CSQ than did PA-CBT adolescents (mean=22.77, SD=6.81) at midtreatment (t[17]=1.32, p=0.21, Cohen's d=0.70), and end of treatment (mean=25.29, SD=4.61 and mean=21.43, SD=8.72, respectively), (t[19]=1.09, p=0.29, Cohen's d=0.55. Three PA-CBT adolescents rated the program and their two different therapists with the lowest possible scores. There were no differences between conditions in parent ratings of program satisfaction at midtreatment (AO-CBT, mean=27.33, SD=3.01; PA-CBT, mean=26.84, SD=5.05, t[17]=0.22, p=0.83, Cohen's d=0.12) and end of treatment (AO-CBT, mean=28.14, SD=4.06; PA-CBT, mean=28.71, SD=4.73, t[19]=.27, p=0.29, Cohen's d=0.13). AO-CBT adolescents (mean=67.29, SD=15.04) reported greater alliance with their therapist than PA-CBT adolescents (mean=54.64, SD=23.81) based on WAI scores at the end of treatment (t[19]=1.28, p=0.22, Cohen's d=0.64). PA-CBT parents (mean=73.85, SD=11.25) reported significantly greater alliance with their own therapists than adolescents in the same dyad (mean=55.92, SD=24.27) at the end of treatment (t[12]=3.10, p<0.01, Cohen's d=0.95). PA-CBT parents (mean=13.63, SD=6.80) attended more sessions than did adolescents (mean=11.38, SD=5.98) in the same dyad (t[15]=2.64, p<0.05, Cohen's d=0.35).
Baseline functioning across conditions
For the sample as a whole, the baseline correlation between parents and adolescents was small but not statistically significant on the BDI (r=0.27, p=0.20) and even lower on the BSS (r=0.08, p=0.71).
With the exception of adolescent scores on the CTQ, PA-CBT adolescents reported higher baseline scores on all clinical measures than did AO-CBT adolescents. Large effect sizes for between-group differences were found for adolescents on the BDI, CDRS, HSC, and MSI- BPD scores as well as for parents on the BHS (See Table 1). Medium effect sizes were found on the remaining measures for adolescents (BSS) and parents (BDI, BHS, MSI-BPD). Five adolescents met screening criteria for BPD, all of whom were randomized to PA-CBT. Additionally, 50% of PA-CBT adolescents reported a history of suicide attempt, whereas none of the AO-CBT adolescents reported a previous attempt. There were no differences between conditions in the percentage of adolescents and parents on medication or the number of medications prescribed at baseline or follow-up.
Table 1.
Baseline Scores by Treatment Condition
| Measure | PA-CBT (n=16) | AO-CBT (n=8) | χ-value |
|---|---|---|---|
| Adolescent gender | 87.5% female | 75% female | 0.60 |
| Parent gender | 93.8% female | 100% female | 0.52 |
| Adolescent history of attempt | 50% | 0% | — |
| Parent history of attempt | 37.5% | 37.5% | 0.0 |
| Parent current MDE | 87.5% | 75% | 0.60 |
| Adolescent medication at baseline | 68.8% | 50% | 0.80 |
| Parent medication at baseline | 75.0% | 87.5% | 0.51 |
| Adolescent medication end of treatment | 66.7% | 57.1% | 1.47 |
| Parent medication end of treatment | 78.6% | 85.7% | 0.15 |
| Adolescent medication follow-up | 71.4% | 66.7% | 0.05 |
| Parent medication follow-up | 64.3% | 66.7% | 0.01 |
| Measure | PA-CBT (n=16) | AO-CBT (n=8) | t value | Effect size |
|---|---|---|---|---|
| Adolescent age | 14.69 (1.78) | 14.00 (1.69) | 0.91 | 0.40 |
| Parent age | 44.94 (7.48) | 42.25 (8.68) | 0.79 | 0.33 |
| Adolescent BDI | 29.32 (11.76) | 19.13 (5.94) | 2.82** | 1.09 |
| Parent BDI | 28.81 (14.78) | 19.00 (10.04) | 1.86 | 0.78 |
| Adolescent current BSS | 9.81 (7.85) | 5.75 (6.09) | 1.28 | 0.58 |
| Parent current BSS | 4.63 (6.96) | 1.00 (1.85) | 1.95† | 0.71 |
| Adolescent HSC | 9.25 (4.92) | 4.63 (2.77) | 2.45* | 1.16 |
| Parent BHS | 9.69 (5.47) | 5.38 (4.81) | 1.89† | 0.84 |
| Adolescent CDRS | 62.13 (12.78) | 52.38 (10.50) | 1.86† | 0.83 |
| Adolescent MSI-BPD | 6.38 (2.13) | 4.50 (1.41) | 2.25* | 1.04 |
| Parent MSI-BPD | 5.44 (1.86) | 4.00 (2.62) | 1.56 | 0.63 |
| CTQ | 44.50 (14.92) | 42.25 (8.88) | 0.39 | 0.18 |
| Number of sessions adolescents attended | 11.38 (5.98) | 11.88 (6.66) | 0.19 | 0.08 |
| Adolescent number of medications baseline | 1.0 (.82) | 0.88 (.99) | 0.33 | 0.14 |
| Parent number of medications baseline | 1.25 (1.0) | 1.25 (.89) | 0 | 0 |
| Adolescent number of medications end of treatment | 1.13 (1.06) | 1.14 (1.07) | 0.02 | 0.01 |
| Parent number of medications end of treatment | 1.21 (.89) | 1.0 (.58) | 0.57 | 0.28 |
| Adolescent number of medications follow-up | 1.0 (.78) | 1.0 (.89) | 0 | 0 |
| Parent number of medications follow-up | 1.36 (1.34) | 0.60 (.55) | 1.21 | 0.75 |
The measure of effect size used was Cohen's d. Size estimates recommended by Cohen (1988) are: small, 0.2; medium, 0.5; and large, 0.8. End of treatment medication data include (n=22) adolescents and (n=21) parents; follow-up medication include (n=20) adolescents and (n=20) parents.
p<0.05, **p=0.01, †p<0.10.
AO-CBT, adolescent only cognitive behavioral therapy condition; PA- CBT, parent and adolescent concurrent cognitive behavioral therapy condition; MDE, major depressive episode; BDI, Beck Depression Inventory; BSS, Beck Suicide Scale; HSC, Hopelessness Scale for Children; BHS, Beck Hopelessness Scale; CDRS, Children's Depression Rating Scale; MSI-BPD, McLean Screening Instrument for Borderline Personality Disorder; CTQ, Childhood Trauma Questionnaire.
These baseline differences were also confirmed by the growth mixture models, which account for nonindependence of parent–adolescent dyads. As demonstrated by Table 2 intercepts, PA-CBT dyads had significantly higher baseline BDI scores (z score=−2.33, p<0.01), and baseline BSS scores, (z score=2.11, p<0.05) than AO-CBT dyads.
Table 2.
Latent Growth Models of Treatment and Maintenance Effects
| Treatment effect | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Intercept | Slope | Treatment maintenance | |||||||
| Outcome | estimate | SE | Z score | estimate | SE | Z score | Estimate | SE | Z score |
| Dyads (n=48) | |||||||||
| BDI | 9.99 | 3.04 | 3.29** | −0.44 | 0.19 | −2.25* | 2.73 | 4.15 | 0.66 |
| BSS | 4.07 | 1.58 | 2.57* | −0.09 | 0.06 | −1.47 | 1.60 | 0.98 | 1.62 |
| Parent (n=24) | |||||||||
| BDI | 9.83 | 4.85 | 2.03* | −0.73 | 0.24 | −3.07** | 2.62 | 5.71 | 0.46 |
| BSS | 2.07 | 1.81 | 1.14 | −0.5 | 0.05 | −1.08 | 0.97 | 1.03 | 0.94 |
| Adol (n=24) | |||||||||
| BDI | 10.16 | 3.48 | 2.92** | −0.14 | 0.19 | −0.74 | 1.76 | 3.92 | 0.45 |
| BSS | 1.66 | 1.74 | 1.52 | 0.02 | 0.06 | 0.32 | 2.05 | 1.70 | 1.20 |
All composite models test baseline (intercept) and treatment (slope) effects using latent linear growth models, with treatment regressed on intercept and slope processes as well as the 48 month maintenance outcome. Dyad analyses involve multilevel latent growth models of both parent and adolescent outcomes with dyadic membership indicated as the cluster variable.
p<0.05, **p<0.01.
BDI, Beck Depression Inventory; BSS, Beck Suicide Scale.
Response to treatment
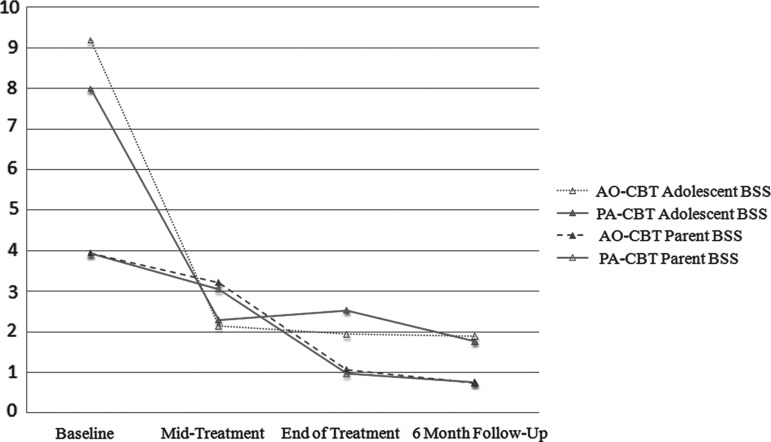
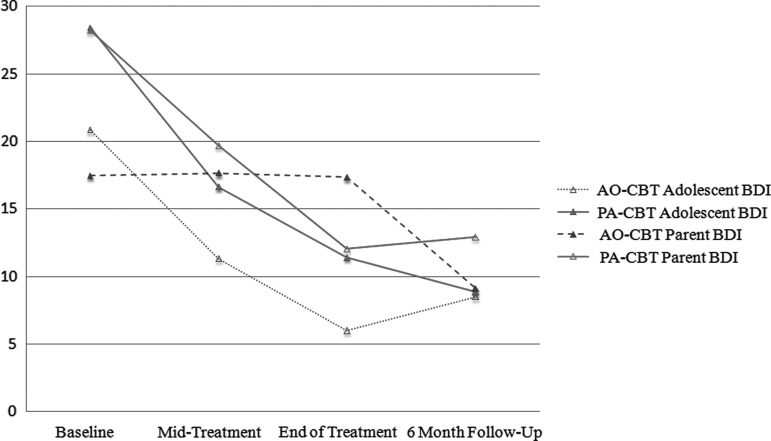
Unconditional mixture models of parent and adolescent responses were tested in order to examine change in symptoms over time, irrespective of treatment group assignment. Statistics for all the analyses are presented in Table 2. Only statistically significant results are repeated here. Parent–adolescent BSS scores decreased significantly over the course of treatment (z score=−3.17, p<0.01, d=0.91) (See Fig. 1.). BDI scores of parent–adolescent dyads also decreased significantly over the course of the 24 week treatment period (z score=−5.65, p<0.01, d=1.63) (See Fig. 2.).
FIG. 1.
Adolescent and parent outcomes on the Beck Suicide Scale (BSS) by treatment condition at baseline, mid-treatment, end of treatment, and 6 month posttreatment follow-up. BSS scores significantly decreased over the course of treatment, but there were no differences between treatment conditions. AO-CBT, adolescent only cognitive behavioral therapy condition; PA-CBT, parent and adolescent concurrent cognitive behavioral therapy condition.
FIG. 2.
Adolescent and parent outcomes on the Beck Depression Inventory (BDI) by treatment condition at baseline, midtreatment, end of treatment, and 6 month posttreatment follow-up. PA-CBT dyads had significantly greater reductions in BDI total scores over time than did AO-CBT participants. AO-CBT, adolescent only cognitive behavioral therapy condition; PA-CBT, parent and adolescent concurrent cognitive behavioral therapy condition.
As shown in Table 2 and illustrated in Figure 1, mixture models examining BDI scores in parent–adolescent dyads indicated that PA-CBT participants evidenced greater reductions in BDI total scores over time relative to AO-CBT participants (z score=− 2.33, p<0.05, d=0.67). Treatment effects were then examined separately in parents and adolescents, with PA-CBT parents observed to report significantly greater reductions in depressed mood over time than AO-CBT participants (z score=−3.07, p<0.01, d=1.25). Analyses did not support any significant effects of treatment condition on BSS (See Table 2, Fig. 1). During treatment, one adolescent and one parent attempted suicide; both participants were enrolled in PA-CBT (but from different dyads) and had a history of prior attempts. In addition, three PA-CBT adolescents were psychiatrically hospitalized during the treatment phase, one for emotional distress after revealing sexual abuse had occurred in the family, one for suicidal ideation and cutting, and one for being unable to contract for safety. Two of these adolescents had been previously hospitalized on two occasions and the third had been hospitalized on one occasion.
Maintenance of intervention effects
As shown in Table 2, after adjusting for prior scores on the BDI and BSS, there were no significant between-group differences on these measures over the 24 week follow-up period. Two adolescents reported a suicide attempt during the 6 month posttreatment follow-up period, one of whom had been enrolled in PA-CBT and one who had been enrolled in AO-CBT. Both had a history of prior hospitalizations.
Discussion
This study examined the acceptability, feasibility, and preliminary treatment efficacy of a concurrent parent and adolescent CBT protocol. Overall, adolescents and parents in both PA-CBT and AO-CBT demonstrated clinically significant improvements. The concurrent protocol was found to be feasible to implement with most depressed adolescents and parents. Program satisfaction was lower in PA-CBT, at least in part because three PA-CBT adolescents rated the program and their therapists (two therapists in total) with the lowest possible scores. All three adolescents remitted – two at the end of treatment and one during follow-up – but they refused to participate in sessions with their parents. Two adolescents were described by their therapists as oppositional and in need of family sessions to address parent–adolescent conflict. The third adolescent reported abuse in the family midway through treatment and was psychiatrically hospitalized.
With respect to treatment outcomes, adolescents in both conditions demonstrated significant improvement in suicidal ideation from baseline to end of treatment, and the level remained low throughout follow-up. The low rates of suicidal ideation in parents limit any interpretation of findings: 75% of AO-CBT parents and 50% of PA-CBT parents denied any suicidal ideation at baseline. The correlation between adolescent and parent suicidal ideation at baseline was very low. Treatment-emergent suicide attempts, defined as first lifetime suicide attempt, did not occur in either adolescents or parents in AO-CBT or PA-CBT during the 6 months that participants received treatment. Repeat attempts did occur in the PA-CBT condition for two adolescents who had previous suicide attempt-related hospitalizations prior to entering treatment. Therefore, it is possible that these adolescents were at high risk regardless of type of treatment received because a previous suicide attempt is the best predictor of future attempts (Shaffer and Pfeffer 2001; Asarnow et al. 2008). It is also possible that PA-CBT was iatrogenic for some teens. Although these teens are exposed to their depressed parent's difficulties regulating affect within the family environment, some teens may have responded negatively to the specific emphasis on parent mood in addition to teen mood in the PA-CBT protocol. By clinician report, this seemed especially true in situations that involved a shared traumatic experience for the parent and teen. Alternatively, parents in PA-CBT had higher levels of psychopathology overall than those in AO-CBT, including the parents of the three adolescents who refused to participate in sessions with their parent; therefore, these adolescents may have been trying to protect themselves from even greater exposure to parental dysfunction.
With respect to adolescent depressed mood, our primary analyses included outcomes reported by adolescents as well as parents while accounting for their shared dyadic participation in treatment. Improvement was strongest in the PA-CBT dyad, as hypothesized. The added utility of treating a depressed parent in the same protocol as their adolescent was most evident with respect to improving parental depression. Parents in the PA-CBT protocol demonstrated a steady, linear decease in depressed mood across the 24 week treatment, whereas parents in AO-CBT did not demonstrate an improvement in depressed mood during the 24 weeks of treatment. Parents in PA-CBT rated their alliance with their therapist as higher than did their adolescents, and they attended more sessions on average than the adolescent, suggesting that they found therapy useful. Parents in PA-CBT also participated in structured medication management sessions, which might also have contributed to their improvement in mood compared with the AO-CBT parents, who were not prescribed medication in a systematic fashion.
The outcome data from this study must be considered within the context of its limitations, including the small sample size, which reduces both the power to detect differences between groups as well as the stability of findings. In addition, more families were enrolled in the experimental condition, in order to increase clinical experience using the concurrent treatment protocol. Although there were higher numbers of attempts and hospitalizations in PA-CBT, there were twice as many patients treated in this condition compared with AO-CBT. Also, randomization was unsuccessful in this small sample, as adolescents in the experimental condition had significantly higher levels of preexisting suicidality and psychopathology. Therefore, the fact that adolescents in PA-CBT did as well as those in AO-CBT might be interpreted as evidence for the superiority of the concurrent intervention for most adolescents. Nonetheless, some adolescents may still prefer to receive treatment on their own and not concurrently in the same clinic as a parent. The small correlation between parent and adolescent depressed mood at baseline also reinforces the fact that mood states are multidetermined and that successful treatment of one person in a parent–adolescent dyad will not always result in improvement in the other person. Clinical inspection of weekly mood assessments collected during therapy clearly indicated that mood ratings co-occurred between parent and adolescent in some, but not all, cases.
The same therapists treated adolescents in both conditions, which helps control for therapist effects but creates a higher standard than is seen in most treatment studies. Patients stayed in treatment for more sessions than typically found in other CBT trials for adolescent depression (March et al. 2004; Vitiello et al. 2006; Brent et al. 2008; Kennard et al. 2009; Lewis et al. 2010), and both conditions responded very well to the treatments overall. Also, many AO-CBT parents were receiving therapy, and seven out of eight parents were taking medication for their mood. We allowed the parents to receive outside treatment, because it approximated standard care. Treatment of parents, even when not systematically controlled, is valuable even if not integrated with treatment of the adolescent.
Conclusions
This study established feasibility of recruitment, randomization, and retention for a CBT protocol that concurrently treats a depressed adolescent with a depressed parent. The pilot concurrent treatment protocol appeared more effective than treating an adolescent alone in reducing parent and adolescent depressed mood during the 24 weeks of active treatment, with its largest effect on parental depressed mood. The treatment outcomes for adolescent suicidality were comparable in both groups. A larger study that has sufficient power to test efficacy would be necessary to understand the potential utility of a concurrent protocol. A larger study is also necessary to delineate the moderators of treatment outcome for adolescent only versus concurrent adolescent–parent treatment, such as trauma history and chronicity/severity of parental depression/suicidality.
Clinical Significance
Comparable results with the concurrent treatment protocol were achieved despite the greater baseline psychopathology in the adolescents in the experimental condition relative to the comparison condition, indicating the potential added value of the concurrent protocol. The concurrent protocol did result in a faster improvement in parental depression than did standard care. Therefore, in cases in which parental depression is considered to be a major impediment to improvement in an adolescent's depressed mood, concurrent treatment may be the more efficacious approach to treating adolescent. The large majority of parents in the comparison condition received treatment on their own. Consequently, a concurrent treatment protocol is not necessarily more expensive than standard care. That is, insurers were already paying for parents to receive psychiatric treatment in standard care, so integrated treatment would not likely have added much additional cost.
Acknowledgments
The authors thank Drs. Joan Asarnow, David Brent, and Graham Emslie for consulting with the research team on the development of the integrated treatment protocol.
Disclosures
No competing financial interests exist.
References
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- Asarnow JR, Baraff LJ, Berk M, Grob C, Devich-Navarro M, Suddath R, Piacentini J, Tang L: Pediatric emergency department suicidal patients: Two-site evaluation of suicide ideators, single attempters, and repeat attempters. J Am Acad Child Adolesc Psychiatry 47:958–966, 2008 [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G: Manual for the Beck Depression Inventory-II. San Antonio: Psychological Corporation, 1996 [Google Scholar]
- Beck AT, Kovacs M, Weissman A: Assessment of suicidal intention: The Scale for Suicide Ideation. J Consult Clin Psychol 47:343–352, 1979 [DOI] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, Trexler L: The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol 42:861–865, 1974 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K, Sapareto E, Ruggiero J: Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 151:1132–1136, 1994 [DOI] [PubMed] [Google Scholar]
- Bosker FJ, Hartman CA, Nolte IM, Prins BP, Terpstra P, Posthuma D, van Veen T, Willemsen G, DeRijk RH, de Geus EJ, Hoogendijk WJ, Sullivan PF, Penninx BW, Boomsma DI, Snieder H, Nolen WA: Poor replication of candidate genes for major depressive disorder using genome-wide association data. Mol Psychiatry 16:516–532, 2011 [DOI] [PubMed] [Google Scholar]
- Brent D, Emslie G, Clarke G, Wagner KD, Asarnow JR, Keller M, Vitiello B, Ritz L, Iyengar S, Ahebe K, Birmaher B, Ryan N, Kennard B, Hughes C, DeBar L, McCracken J, Strober M, Suddath R, Spirito A, Leonard H, Melhem N, Porta G, Onorato M, Zelazny J: Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: The TORDIA randomized controlled trial. JAMA 299:901–913, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D, Gaynor S, Weersing V: Cognitive-behavioral approaches to the treatment of depression and anxiety, In: Child and Adolescent Psychiatry. Oxford: Blackwell, 921–937, 2002 [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D: Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. J Am Acad Child Adolesc Psychiatry 37:906–914, 1998 [DOI] [PubMed] [Google Scholar]
- Brent DA, Mann JJ: Family genetic studies, suicide, and suicidal behavior. Am J Med Genet C Semin Med Genet 133C:13–24, 2005 [DOI] [PubMed] [Google Scholar]
- Brent DA, McMakin DL, Kennard BD, Goldstein TR, Mayes TL, Douaihy AB: Protecting adolescents from self-harm: A critical review of intervention studies. J Am Acad Child Adolesc Psychiatry 52:1260–1271, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Hariri AR, Holmes A, Uher R, Moffitt TE: Genetic sensitivity to the environment: The case of the serotonin transporter gene and its implications for studying complex diseases and traits. Am J Psychiatry 167:509–527, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R: Influence of life stress on depression: Moderation by a polymorphism in the 5-HTT gene. Science 301:386–389, 2003 [DOI] [PubMed] [Google Scholar]
- Cohen J: Statistical power analysis for the behavioral sciencies. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988 [Google Scholar]
- Compas BE, Forehand R, Thigpen JC, Keller G, Hardcastle EJ, Cole DA, Potts J, Watson KH, Rakow A, Colletti C, Reeslund K, Fear J, Garai E, McKee L, Merchant MJ, Roberts L: Family group cognitive-behavioral preventive intervention for families of depressed parents: 18- and 24-month outcomes. J Consult Clin Psychol 79:488–499, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emslie GJ, Hughes CW, Crismon ML, Lopez M, Pliszka S, Toprac MG, Boemer C, Texas Children's Medication Algorithm P: A feasibility study of the childhood depression medication algorithm: The Texas Children's Medication Algorithm Project (CMAP). J Am Acad Child Adolesc Psychiatry 43:519–527, 2004 [DOI] [PubMed] [Google Scholar]
- Esposito–Smythers C, Spirito A, Kahler CW, Hunt J, Monti P: Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized clinical trial. J Consult Clinic Psychol 79:728–739, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Spitzer R, Williams J, Gibbons M: Structured clinical interview for DSM-IV-Patient version. New York, Biometrics Research Department, New York State Psychiatric Institute, 1995 [Google Scholar]
- Goodman SH: Depression in mothers. Annu Rev Clin Psychol 3: 107–135, 2007 [DOI] [PubMed] [Google Scholar]
- Goodman SH, Gotlib IH: Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychol Rev 106:458, 1999 [DOI] [PubMed] [Google Scholar]
- Gunlicks ML, Weissman MM: Change in child psychopathology with improvement in parental depression: A systematic review. J Am Acad Child Adolesc Psychiatry 47:379–389, 2008 [DOI] [PubMed] [Google Scholar]
- Hammen CL: Children of depressed parents. In: Gotlib IH, Hammen C. (Eds), Handbook of Depression (2nd Ed.) New York: Guilford Press, 2009. pp. 275–297 [Google Scholar]
- Horvath AO, Greenberg LS: Development and validation of the Working Alliance Inventory. J Counsel Psychol 36: 223, 1989 [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U: Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988, 1997 [DOI] [PubMed] [Google Scholar]
- Kazdin AE, French NH, Unis AS, Esveldt–Dawson K, Sherick RB: Hopelessness, depression, and suicidal intent among psychiatrically disturbed inpatient children. J Consult Clin Psychol 51:504–510, 1983 [DOI] [PubMed] [Google Scholar]
- Kennard BD, Silva SG, Tonev S, Rohde P, Hughes JL, Vitiello B, Kratochvil CJ, Curry JF, Emslie GJ, Reinecke M, March J: Remission and recovery in the Treatment for Adolescents With Depression Study (TADS): Acute and long-term outcomes. J Am Acad Child Adolesc Psychiatry 48:186–195, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klempan TA, Sequeira A, Canetti L, Lalovic A, Ernst C, Ffrench–Mullen J, Turecki G: Altered expression of genes involved in ATP biosynthesis and GABAergic neurotransmission in the ventral prefrontal cortex of suicides with and without major depression. Mol Psychiatry 14:175–189, 2009 [DOI] [PubMed] [Google Scholar]
- Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD: Assessment of client/patient satisfaction: Development of a general scale. Eval Program Plann 2:197–207, 1979 [DOI] [PubMed] [Google Scholar]
- Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW, Silva SG, March JS: Impact of childhood trauma on treatment outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry 49:132–140, 2010 [DOI] [PubMed] [Google Scholar]
- Little RJ, D'Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, Frangakis C, Hogan JW, Molenberghs G, Murphy SA, Neaton JD, Rotnitzky A, Scharfstein D, Shih WJ, Siegel JP, Stern H: The prevention and treatment of missing data in clinical trials. N Engl J Med 367:1355–1360, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann JJ, Huang YY, Underwood MD, Kassir SA, Oppenheim S, Kelly TM, Dwork AJ, Arango V: A serotonin transporter gene promoter polymorphism (5-HTTLPR) and prefrontal cortical binding in major depression and suicide. Arch Gen Psychiatry 57:729–738, 2000 [DOI] [PubMed] [Google Scholar]
- March J, Silva S, Petrycki S, Curry J, Wells K, Fairbank J, Burns B, Domino M, McNulty S, Vitiello B, Severe J, Treatment for Adolescents With Depression Study: Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. JAMA 292:807–820, 2004 [DOI] [PubMed] [Google Scholar]
- McLachlan G, Peel D: Finite mixture models. New York: Wiley and Sons; 2000 [Google Scholar]
- Muthen B, Shedden K: Finite mixture modeling with mixture outcomes using the EM algorithm. Biometrics 55:463–469, 1999 [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B: Mplus user's guide. Los Angeles: Muthén & Muthén; 1998–2011 [Google Scholar]
- Poznanski EO, Freeman LN, Mokros HB: Children's Depression Rating Scale – Revised. Psychopharm Bull 21:927–989, 1984 [Google Scholar]
- Sander JB, McCarty CA: Youth depression in the family context: Familial risk factors and models of treatment. Clin Child Fam Psychol Rev 8:203–219, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schosser A, Calati R, Serretti A, Massat I, Kocabas NA, Papageorgiou K, Linotte S, Mendlewicz J, Souery D, Zohar J, Juven–Wetzler A, Montgomery S, Kasper S: The impact of COMT gene polymorphisms on suicidality in treatment resistant major depressive disorder—a European multicenter study. Eur Neuropsychopharmacol 22:259–266, 2012 [DOI] [PubMed] [Google Scholar]
- Shaffer D, Pfeffer C: Summary of the practice parameters for the assessment and treatment of children and adolescents with suicidal behavior. J Am AcadChild Adolesc Psychiatry 40:24–51, 2001 [DOI] [PubMed] [Google Scholar]
- Suehs B, Argo T, Bendele S, Crismon M, Trivedi M, Kurian B: Texas Medication Algorithm Project procedural manual: Major depressive disorder algorithms. Austin, TX: Texas Department of State Health Services; 2008 [Google Scholar]
- Southam–Gerow M, Kendall P, Weersing R:. Examining outcome variability: correlates of treatment response in a child and adolescent anxiety clinic. J Clin Child Adolesc Psychol 30:422–436, 2001 [DOI] [PubMed] [Google Scholar]
- Vitiello B, Rohde P, Silva S, Wells K, Casat C, Waslick B, Simons A, Reinecke M, Weller E, Kratochvil C, Walkup J, Pathak S, Robins M, March J: Functioning and quality of life in the Treatment for Adolescents With Depression Study (TADS). J Am Acad Child Adolesc Psychiatry 45:1419–1426, 2006 [DOI] [PubMed] [Google Scholar]
- Wagner BM: Family risk factors for child and adolescent suicidal behavior. Psychol Bull 121:246–298, 1997 [DOI] [PubMed] [Google Scholar]
- Wagner BM, Silverman MAC, Martin CE: Family factors in youth suicidal behaviors. Am Behav Scientist 46:1171–1191, 2003 [Google Scholar]
- Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, Hughes CW, Garber J, Malloy E, King CA, Cerda G, Sood AB, Alpert JE, Trivedi MH, Rush AJ, Team STD-C: Remissions in maternal depression and child psychopathology: A STAR*D-child report. JAMA 295:1389–1398, 2006 [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Kelvin R, Roberts C, Dubicka B, Goodyer I: Clinical and psychosocial predictors of suicide attempts and nonsuicidal self-injury in the Adolescent Depression Antidepressants and Psychotherapy Trial (ADAPT). Am J Psychiatry 168:495–501, 2011 [DOI] [PubMed] [Google Scholar]
- Young J, Beck AT: Cognitive Therapy Scale Rating Manual. Philadelphia: University of Pennsylvania; 1980 [Google Scholar]
- Zanarini MC, Vujanovic AA, Parachini EA, Boulanger JL, Frankenburg FR, Hennen J: A screening measure for BPD: The McLean screening instrument for borderline personality disorder (MSI-BPD). J Pers Disord 17:568–573, 2003 [DOI] [PubMed] [Google Scholar]